Introduction
Surgery is currently the most commonly used
treatment method for vocal cord polyps; however, the self-retaining
laryngoscope used during surgery can cause severe cardiovascular
reactions and stress responses, resulting in a series of changes in
the nervous, endocrine and metabolic systems (1). This surgical procedure is delicate,
with a high requirement for anesthesia; during the surgery, the
vocal cord is required to remain stationary, as this should reduce
the stress response and throat reflex, and fully relax the muscles,
and also enable recovery and rehabilitation from the surgery as
quickly as possible to avoid the aspiration of blood and
oropharyngeal secretions (2).
Therefore, it is vitally important to establish a scientifically
confirmed and reasonable amount of anesthetic for use during the
surgery.
A combination of the ultra-short-action opioid
remifentanil (Rem) and ultra-short-action intravenous anesthetic
propofol (Pro) is currently considered the best combination for
total intravenous anesthesia (TIVA) (3). Rem has very short half-life, and so the
continuous intravenous administration of Rem should not produce
cumulative effects (4). In
particular, its infusion time-related half-life is only 3–5 min; it
is not notably decomposed by plasma cholinesterase; repeated or
high-dose application does not affect the recovery time for
spontaneous breathing and extubation after its discontinuation; and
it can inhibit the decomposition of norepinephrine and
corticosteroids (5). Pro is rapidly
effective, with a short duration of action and rapid recovery, and
it makes sedation easy to control (6–8). These
two drugs are suitable for target-controlled infusion (TCI) in a
short surgical procedure.
However, at present there have been no definitive
studies concerning the dosage of Rem for use in surgery involving a
self-retaining laryngoscope. Thus, the aim of the present study was
to use the median effective concentration (EC50)
sequential test method to calculate the EC50 and 95%
confidence interval (95% CI) of the Rem-Pro combination for the
inhibition of self-retaining laryngoscope-caused cardiovascular
responses (SRLCCRs). Through observing changes of heart rate, mean
arterial pressure, auditory evoked potential (AEP) index, cortisol,
interleukin (IL)-6 and blood glucose prior to and following the
induction of anesthesia, as well as prior to and following the
self-retaining laryngoscope insertion, this study aimed to observe
the inhibitory effects of Rem towards the cardiovascular system and
SRLCCRs, aiming to provide a reference for its clinical use.
Materials and methods
General information
A total of 20 patients, who were subjected to vocal
cord polyp resection under general anesthesia in Weifang People's
Hospital (Weifang, China) from June 2009 to December 2012, were
randomly selected for inclusion in the present study. The exclusion
criteria were as follows: Circulation, glucose metabolism and
nervous system dysfunctions; preoperative history of long-term
application of analgesic or sedative drugs, with medication history
that would interfere with glucose metabolism, adrenal function or
the sympathetic system, with long-term history of alcohol abuse,
long-term application of opioids or allergic response to opioids;
endotracheal intubation could not be completed within 1 min;
serious cardiovascular reactions occurring during endotracheal
intubation and laryngoscope insertion that prevented the surgery
from proceeding. This study was approved by the ethics committee of
Weifang People's Hospital. Written informed consent was obtained
from the patients.
Anesthesia
All study subjects were set up for intravenous
access after entry into the surgery room, and connected to a
PM-6000 multi-parameter monitor (Mindray Bio-Medical Electronics
Co., Shenzhen, China) to show electrocardiogram (ECG), heart rate
(HR), pulse oxygen saturation (SpO2), non-invasive
arterial pressure (BP) and Alaris AEP Index (AAI) values. Rem
(batch no. 070904; Yichang Humanwell Pharmaceutical Co., Ltd.,
Yichang, China) and Pro (batch ET763; AstraZeneca SpA, Basiglio,
Italy) were infused through a TCI–I type infusion pump (Slgo
Medical Technology Co., Ltd., Beijing, China) for TCI. Rem was
infused with the plasma target-controlled concentration in
accordance with the EC50 sequential method; when the
plasma concentration and effect-site concentration were in
equilibrium [the half-life for equilibration (T1/2 Keo)
of Rem was 1.32 min (9), with
equilibrium of the two concentrations being reached 5–6 min later],
the TCI of Pro was initiated. When the patient lost consciousness
[Observer's Assessment of Alertness/Sedation (OAA/S) scale score
≤2], 0.1 mg/kg vecuronium (batch no. 070704.1; Xianju
Pharmaceutical Co., Ltd., Zhejiang, China) was intravenously
injected. Then, connection to the intubation and anesthesia
instrumentation was performed and the peak end tidal CO2
(PETCO2) level was maintained at 35–45 mmHg. After 3
min, the HS2301 self-retaining laryngoscope (Shanghai Hengsheng
Medical Instrument Co., Ltd., Shanghai, China) was inserted, and
the surgery was conducted. If a reduction in HR or systolic BP
occurred during the induction of anesthesia, cardiovascular drug
treatment was applied until the patient's HR or blood pressure was
stable (observed for 1 min). The laryngoscopic surgery was then
conducted, and the monitoring that was initiated prior to treatment
was continued, and values were recorded. If the HR or mean arterial
BP increased during laryngoscope insertion, the Rem target
concentration was adjusted to a higher level for completion of the
surgery (while the concentration for next patient was determined on
the basis of the initial concentration). The Pro plasma
concentration was controlled at 4 µg/ml (Marsh pharmacokinetic
parameters) (10). The Rem
target-controlled plasma concentration (Minto pharmacokinetic
parameters) (11) was determined
according to the EC50 sequential method, that is, the
patient's plasma target-controlled concentration was determined by
the previous patient's cardiovascular responses; if the previous
patient exhibited SRLCCRs, the next higher concentration level was
used; if there were no SRLCCRs, a lower-level concentration was
applied. The ratio of two adjacent concentrations was 1.2. The test
started from a Rem target-controlled plasma concentration of 5
ng/ml, and the concentration for each case was calculated from the
previous case on the basis of whether cardiovascular reactions were
exhibited.
Observation items and scoring
The values of HR, mean (arterial) blood pressure
(MBP) and the auditory evoked potential (AEP)-based A-line ARX
Index (AAI) were recorded. The data acquisition time points were:
Baseline value (T0), after anesthesia induction (T1), prior to
laryngoscope insertion (T2) and highest value within 3 min after
laryngoscope insertion (T3). Each value was recorded three times
and averaged. Changes of HR, MBP and/or AAI of >15% were
considered as positive cardiovascular responses.
Sedation scoring was initiated after the Pro
infusion, and the OAA/S scale score (12) was used to assess the patient's degree
of sedation. The scores were recorded at T1, T2 and T3,
respectively.
Arterial blood samples (5 ml) were drawn at T2 and
T3 for the measurement of stress indicators, namely cortisol and
the inflammatory marker interleukin (IL)-6 using radioimmunoassay
kits (Fuzhou Maixin Biotechnology Development Co., Ltd., Fuzhou,
China). Blood glucose levels were measured using a type II blood
glucose meter (Roche Diagnostics (Shanghai) Ltd., Shanghai, China)
at T2 and T3.
Statistical analysis
The EC50 sequential method was used
(13) to calculate the effective
plasma concentration of Rem that inhibited SRLCCR in 50% of
patients (the EC50). The valid number (r) and invalid
number (s) of SRLCCR inhibitions under a specific Rem plasma target
concentration were analyzed, and the logarithm of each plasma
target concentration (x), the total number of patients (n),
efficiency (p) of SRLCCR inhibition, and difference (d) of
logarithms of two adjacent concentrations were determined and used
to calculate the EC50 and 95% confidence interval (CI)
by the EC50 sequential method. The following formulae
were used: Logarithm of EC50 (lg EC50) =
∑nx/∑n; standard deviation of the logarithm of EC50 (S
lg EC50) = d√[p(1-p)/n-1]; and 95% CI for the overall
EC50 = (lg EC50 - 1.96 S lg EC50
to lg EC50 + 1.96 S lg EC50). The
EC50 and 95% CI values were reported as the
anti-logarithm of each logarithmic number. The average values of
cortisol, IL-6 and glucose under the Rem plasma target-controlled
concentration were determined, and intragroup comparisons were
conducted using paired t-tests. Measurement data are expressed as
mean ± standard deviation. SPSS software, version 11.5 (SPSS, Inc.,
Chicago, IL, USA) was used for statistical processing, with
P<0.05 considered to indicate a statistically significant
difference.
Results
General patient information and
grouping
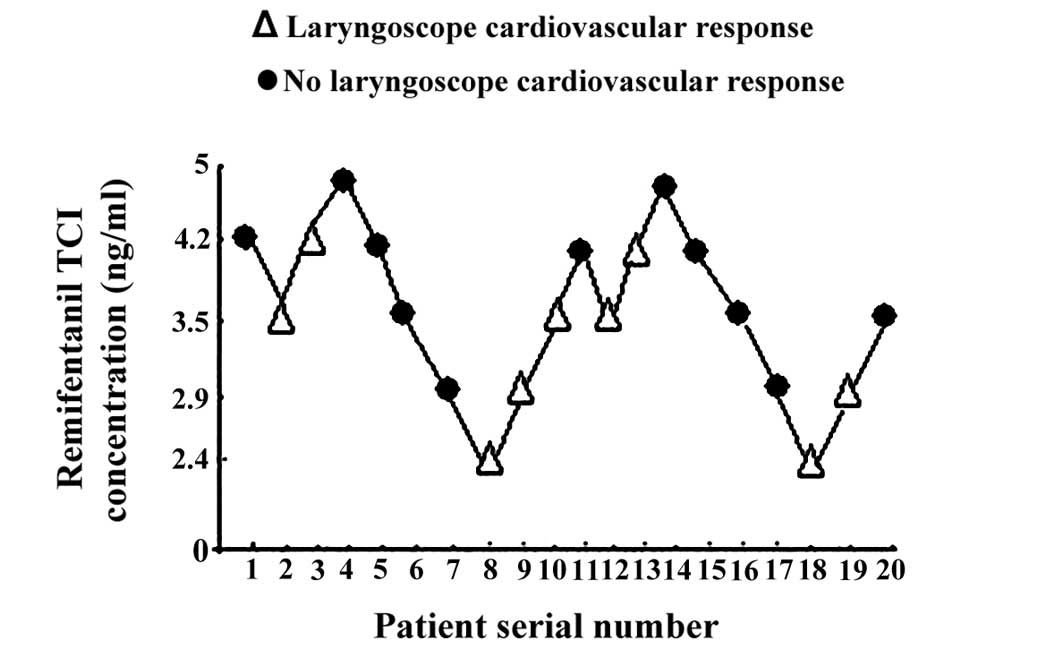
A total of 20 patients were enrolled in the present
study The Rem target concentrations of the selected patients were
set as follows: 2 cases at 5 ng/ml, 6 cases at 4.2 ng/ml, 6 cases
at 3.5 ng/ml, 4 cases at 2.9 ng/ml and 2 cases at 2.4 ng/ml. The 20
patients were then divided into five groups, for analysis according
to the different target concentrations of Rem; Group A, 5 ng/ml;
group B, 4.2 ng/ml; group C, 3.5 ng/ml; group D, 2.9 ng/ml; and
group E, 2.4 ng/ml. No statistically significant difference in age,
weight and gender was observed among the five groups (P>0.05;
Table I).
 | Table I.General information of the patients in
the five groups. |
Table I.
General information of the patients in
the five groups.
| Variable | Group A | Group B | Group C | Group D | Group E |
|---|
| Age (years) | 38 | 39.6±7.9 | 42.2±6.8 | 36.3±5.9 | 44 |
| Gender
(male/female) | 2/0 | 4/2 | 3/3 | 2/2 | 1/1 |
| Weight (kg) | 68.4 | 70.2±11.3 | 69.6±9.4 | 65.6±10.6 | 63.5 |
During testing, 1 patient was excluded due to the
occurrence of laryngoscope-induced bradycardia (HR, <50
beats/min), but none of the patients exhibited any chest wall
stiffness. Postoperative questioning confirmed that no patients
experienced intraoperative awareness.
Calculation of the
EC50
The valid number (r) and invalid number (s) of
SRLCCR inhibitions under each Rem plasma target concentration were
analyzed, and the logarithm of each plasma target concentration
(x), total number of patients (n), efficiency (p) of SRLCCR
inhibition and difference (d) of logarithms of two adjacent
concentrations were calculated, and the results are presented in
Table II. The EC50 value
calculated according to the EC50 sequential method was
3.5 ng/ml and the 95% CI was 3.47–3.60.
 | Table II.Remifentanil plasma target-controlled
concentration. |
Table II.
Remifentanil plasma target-controlled
concentration.
| Plasma
target-controlled concentration (ng/ml) | Log plasma
target-controlled concentration (x) | Total cases for each
plasma target-controlled concentration (n) | Valid cases of SRLCCR
inhibition (r) | Invalid cases of
SRLCCR inhibition (s) | Valid rate (%) of
SRLCCR inhibition (p) |
|---|
| 5 | 0.699 | 2 | 2 | 0 | 100 |
| 4.2 | 0.623 | 6 | 4 | 2 | 66.7 |
| 3.5 | 0.544 | 6 | 3 | 3 | 50.0 |
| 2.9 | 0.477 | 4 | 2 | 2 | 50.0 |
| 2.4 | 0.398 | 2 | 0 | 2 | 0 |
The Rem target-controlled plasma concentrations for
SRLCCR inhibition in each patient are shown in Fig. 1.
Changes of HR, MBP and AAI
With regard to HR, the HR at T1 was reduced compared
with that at T0 in group A (P<0.05) and group B (P<0.01). In
addition, the HRs at T3 were significantly increased compared with
those at T2 in groups D and E (P<0.05; Table III).
 | Table III.HR, MBP and AAI changes of the five
groups at different time points (mean ± standard deviation). |
Table III.
HR, MBP and AAI changes of the five
groups at different time points (mean ± standard deviation).
| Indices | Time point | Group A | Group B | Group C | Group D | Group E |
|---|
| HR (bpm) | T0 |
98.0±1.4 |
88.3±2.8 |
74.2±6.6 |
79.2±6.6 |
76.5±4.3 |
|
| T1 |
68.4±2.3a |
76.5±6.7b |
69.7±3.3 |
78.9±5.8 |
75.3±2.8 |
|
| T2 |
74.0±4.6 |
77.0±5.6 |
72.1±3.6 |
81.0±5.4 |
80.3±4.7 |
|
| T3 |
75.3±5.5 |
80.8±6.2 |
78.8±5.4 |
89.0±2.6c |
113.5±8.3c |
| MBP (mmHg) | T0 |
102.1±7.6 |
100.5±5.6 |
99.4±4.9 |
95.7±5.2 |
94.1±2.3 |
|
| T1 |
83.3±5.7a |
83.8±4.1b |
83.5±3.8b |
86.3±6.6a |
90.5±1.2 |
|
| T2 |
86.8±3.5 |
87.0±3.6 |
86.0±3.0 |
88.2±6.4 |
94.6±3.2 |
|
| T3 |
91.0±4.4 |
93.0±6.3 |
94.3±6.3 |
100.1±11.4c |
123.9±5.2c |
| AAI | T0 |
70.3±2.1 |
75.3±6.1 |
76.3±4.4 |
69.9±5.9 |
72.4±9.5 |
|
| T1 |
19.9±4.7a |
21.1±2.5b |
20.6±3.2b |
20.8±7.0b |
24.7±2.8 |
|
| T2 |
21.9±3.8 |
21.9±2.0 |
20.6±2.4 |
25.8±3.4 |
26.0±5.9 |
|
| T3 |
21.3±4.9 |
22.6±2.3 |
23.3±3.0 |
30.2±2.7c |
40.2±6.4c |
With regard to blood pressure, the MBP values for
groups A and D at T1 were reduced compared with those at T0
(P<0.05); the MBP values at T1 of groups B and C were also
reduced compared with those at T0, with a higher level of
significance (P<0.01). In groups D and E, the MBP values at T3
were significantly increased compared with those at T2 (P<0.05;
Table III).
The AAI value at T1 was reduced compared with that
at T0 in group A (P<0.05). In groups B, C and D, the AAI values
at T1 were also reduced compared with those at T0, with a higher
level of significance (P<0.01). Furthermore, the AAI values in
groups D and E at T3 were significantly increased compared with
those at T2 (P<0.05; Table
III).
Changes of cortisol, IL-6 and blood
sugar levels
When stress indicators were examined, it was
observed that the cortisol levels and blood sugar levels at T3 of
groups D and E were increased compared with those at T2, and the
differences were statistically significant (P<0.05; Table IV). In addition, in group D, the
IL-6 level at T3 was increased compared with that at T2 (P<0.05;
Table IV).
 | Table IV.Cortisol, IL-6 and blood glucose
levels in the five groups at different time points (mean ± standard
deviation). |
Table IV.
Cortisol, IL-6 and blood glucose
levels in the five groups at different time points (mean ± standard
deviation).
| Indices | Time point | Group A | Group B | Group C | Group D | Group E |
|---|
| Cortisol
(ng/ml) | T2 |
180.60±23.76 |
176.73±13.24 |
180.45±13.23 |
184.65±5.85 |
186.45±10.25 |
|
| T3 |
181.05±12.23 |
185.78±11.37 |
188.17±7.66 |
239.80±24.94a |
282.05±16.33a |
| IL-6 (ng/ml) | T2 |
0.71±0.06 |
0.72±0.06 |
0.73±0.07 |
0.86±0.05 |
0.87±0.06 |
|
| T3 |
0.74±0.08 |
0.78±0.06 |
0.79±0.08 |
0.95±0.07a |
1.62±0.18 |
| Blood glucose
(mmol/l) | T2 |
4.90±0.28 |
4.68±0.84 |
4.97±0.60 |
4.98±0.85 |
5.55±0.21 |
|
| T3 |
5.00±0.57 |
4.80±0.73 |
5.20±0.39 |
5.78±0.50a |
7.70±0.42a |
OAA/S scores
All patients exhibited no response towards the
deltoid extrusion pushing examination conducted at T1, T2 and T3,
and thus had a corresponding OAA/S score of 1. No significant
differences were observed.
Discussion
Vocal cord surgery using a self-retaining
laryngoscope involves a short operation with a strong stimulus;
although the duration of surgery is short, the requirements of
anesthesia are high, as it should not only reduce stress responses
and the throat reflex and fully relax the muscles, but also enable
the patient to recover and rehabilitate from the surgery as soon as
possible (2). Thus, the timely
mastering of the depth of anesthesia is very important, and the
scientific and rational determination of drug dosage during the
anesthesia is essential. The present study was conducted to
determine the drug dosage for Rem, and the results are analyzed as
follows.
Cortisol has been demonstrated to be a stress
indicator; for example, Haussmann et al studied healthy
human volunteers under three different stressful conditions, and
found that the salivary cortisol levels were significantly
increased following each type of stress (14). The present study showed that the
plasma cortisol values groups A, B and C at T3 were higher than
those at T2, but the difference was not significant (P>0.05).
However, it could be considered that the intubation affected
cortisol production, as the plasma cortisol levels of groups D and
E group increased significantly at T3 compared with T2 (P<0.05).
These results indicate that when Rem was ≤2.9 ng/ml, it could not
effectively inhibit the stress responses caused by the
laryngoscope.
IL-6 is an important type of inflammatory cytokine
that can mediate the pathophysiological process of stress; the
stimulus of surgical trauma could potentially induce the excessive
production of IL-6. It is considered that IL-6 is a particularly
sensitive inflammatory marker that can reflect tissue damage and
the degree of stress (15,16). A prior study suggested that changes
of IL-6 levels occur earlier and are more sensitive than those of
cortisol (17). In the present
study, the IL-6 values of all groups at T3 were higher than those
at T2. However, while the changes in groups A, B, C and E were not
significant (P>0.05), the plasma IL-6 level of group D was
significantly increased following insertion of the laryngoscope
(P<0.05). These results indicate that when the Rem concentration
was 2.9 ng/ml, it could not inhibit laryngoscope-induced IL-6
induction. The IL-6 levels of group E changed notably between T2
and T3, although not in a statistically significant manner, which
might be due to the small number of patients in this group.
A previous study has confirmed that glucose is an
effective indicator that can reflect the stress response (18). Testing has shown that following
laparoscopic surgery, blood glucose and cortisol values showed
significant differences from those preoperatively (19). The present study showed that there
was no significant change in the blood glucose values of groups A,
B and C before and after laryngoscope insertion (P>0.05), while
those of groups D and E at T3 were significantly increased compared
with those at T2 (P<0.05), indicating that when the Rem dosage
was <2.9 ng/ml, it could not effectively suppress the high
metabolic changes caused by laryngoscope insertion.
The results showed that HR at T1 was lower than that
at T0 for group A (P<0.05) and group B (P<0.01), and the HRs
of groups D and E at T3 were significantly increased compared with
those at T2 (P<0.05). One patient received emergency treatment
due to the rapid HR reduction during insertion of the laryngoscope
(<50 beats/min), and thus was excluded. One patient of group A
exhibited a decreased HR following the induction of anesthesia, and
thus required atropine treatment; 2 cases from groups D and E,
respectively, had an increased Rem target-controlled concentration
for the increased HR following laryngoscope insertion. This result
indicated that when the Rem plasma target-controlled concentrations
were 4.2 and 5 ng/ml, the patients might exhibit induced
cardiovascular responses, while at these concentrations, it would
be difficult to achieve effective inhibition of
laryngoscope-induced changes in HR. This result is essentially
consistent with the EC50, calculated by the
EC50 sequential method, and the above analysis.
Rem can expand the arteries to various degrees
(20), and excessive medication
could cause the lowering of blood pressure. The results of the
present study showed that the patients of each group exhibited a
reduction in MBP at T1 compared with that at T0, which might be
considered to be associated with the blood pressure-lowering
effects of Pro. However, the reduction of group E was not
significant (P>0.05), whereas the reductions at T1 compared with
those at T0 were significant for groups A and D (P<0.05) and
groups B and C (P<0.01). The MBPs of groups D and E at T3 were
significantly increased compared with those at T2 (P<0.05),
among which 1 case of groups A, B and C, respectively, received
ephedrine treatment because of blood pressure reduction at T1, and
1 case of group D and 2 cases of group E underwent adjustment of
the Rem target concentration at T3 due to the increase in blood
pressure. These results indicate that when the Rem target
concentrations were 2.9 and 2.4 ng/ml it was difficult to
effectively suppress the elevated blood pressure caused by the
insertion of the laryngoscope. This result is essentially
consistent with the above analysis. Whether Rem and Pro had a
synergistic effect in lowering the blood pressure requires further
investigation.
AAI is the AEP index derived from the usage of an
A-line monitoring instrument; AEP can accurately reflect the
situations of sedation and analgesia, as well as the prediction of
short-term body movements (21). AAI
values are normally in the range 0–100. Generally, it is considered
that AAI 60–100 represents the normal waking state, 40–60
represents the sleep state, 30–40 represents the light anesthesia
state, <30 represents the clinical anesthesia state and <10
represents the deep anesthesia state (22). It has been suggested that AAI can
much more sensitively reflect the depth of anesthesia than the
bispectral index in Pro-fentanyl anesthesia (23). The present study showed that the AAI
of group A at T1 was decreased compared with that at T0
(P<0.05), and those of groups B, C and D at T1 were
significantly lower than those at T0 (P<0.01); those of groups D
and E at T3 were significantly increased compared with those at T2
(P<0.05). Kreuer et al (24) studied the AAI changes during
anesthesia with Pro and Rem, and hypothesized that in Pro and Rem
anesthesia, a large variation in the AAI values might exist when
the patient is awake, which might explain the reduction of AAI
values of groups A, B and C after the induction of anesthesia.
In this study, sedation/alert scoring was performed
from the initiation of Pro TCI, and the results showed that the
OAA/S scores at three time points of all the patients were 1,
indicating that the patients were in the deep sleep state.
EC50 is a new concept for
target-controlled intravenous infusion drugs, with its meaning
equivalent to the minimum effective concentration of alveolar gas
in inhalation anesthesia. In this study, the EC50
sequential method was used to calculate the EC50 of
Rem-inhibited SRLCCR, so the patient selection was conducted in
accordance with the requirements of the EC50 sequential
method, with a total number of between 12 and 20.
It was calculated that the EC50 of Rem
for the inhibition of SRLCCRs was 3.5 ng/ml, with a 95% CI of
3.47–3.60 ng/ml. This study suggested that when the Pro
target-controlled concentration was 4 µg/ml and the concentration
of Rem was 5 or 4.2 ng/ml obvious inhibition of the cardiovascular
system could be achieved; while Rem target concentrations of 2.9
and 2.4 ng/ml may be insufficient to effectively inhibit SRLCCRs.
When all patients were anesthetized, the OAA/S scores prior to and
following laryngoscope insertion were 1, indicating that the
patients were in the deep sleep state. From the above analysis, it
could be concluded that a Pro concentration of 4 µg/ml could
maintain adequate sedation, and the increase of HR, MBP and AAI in
certain patients before the insertion was associated with the Rem
dose.
In conclusion, the EC50 sequential method
was used to calculate the EC50 (3.5 ng/ml) and 95% CI
(3.47–3.60 ng/ml) of Rem towards SRLCCR inhibition. The test
results showed that a Pro concentration of 4 µg/ml could maintain
adequate sedation. The dose of Rem that was able to effectively
inhibit SRLCCRs while not causing a serious Rem-induced inhibition
response was between 2.9 and 4.2 ng/ml. This result is consistent
with the results of calculation by the EC50 sequential
method.
References
|
1
|
Ghause MS, Singh V, Kumar A, Wahal R,
Bhatia VK and Agarwal J: A study of cardiovascular response during
laryngoscopy and intubation and their attenuation by ultra short
acting b-blocker esmolol. Indian J Anaesth. 46:104–106. 2002.
|
|
2
|
Yumoto E: Laryngeal surgery-vocal cord
polyp and anaesthesia. Nihon Jibiinkoka Gakkai Kaiho. 116:34–37.
2013.(In Japanese). View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yoo HS, Han JH, Park SW and Kim KS:
Comparison of surgical condition in endoscopic sinus surgery using
remifentanil combined with propofol, sevoflurane, or desflurane.
Korean J Anesthesiol. 59:377–382. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Egan TD: Remifentanil: An
esterase-metabolized opioid. West J Med. 166:2021997.PubMed/NCBI
|
|
5
|
Myre K, Raeder J, Rostrup M, Buanes T and
Stokland O: Catecholamine release during laparoscpic fundoplication
with high and low doses of remifentanil. Acta Anaesthesiol Scand.
47:267–273. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wu J, Mahmoud M, Schmitt M, Hossain M and
Kurth D: Comparison of propofol and dexmedetomedine techniques in
children undergoing magnetic resonance imaging. Paediatr Anaesth.
24:813–818. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sieg A bng-Study-Group, Beck S, Scholl SG,
Heil FJ, Gotthardt DN, Stremmel W, Rex DK and Friedrich K: Safety
analysis of endoscopist-directed propofol sedation: A prospective,
national multicenter study of 24441 patients in German outpatient
practices. J Gastroenterol Hepatol. 29:517–523. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Khan HA, Umar M, Tul-Bushra H, Nisar G,
Bilal M and Umar S: Safety of non-anaesthesiologist-administered
propofol sedation in ERCP. Arab J Gastroenterol. 15:32–35. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Minto CF, Schnider TW and Shafer SL:
Pharmacokinetics and pharmacodynamics of remifentanil. II. Model
application. Anesthesiology. 86:24–33. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Coetzee JF, Glen JB, Wium CA and Boshoff
L: Pharmacokinetic model selection for target controlled infusions
of propofol. Anesthesiol. 82:1328–1345. 1995. View Article : Google Scholar
|
|
11
|
Minto CF, Schnider TW and Shafer SL:
Pharmacokinetics and pharmacodynamics of remifentanil. II. Model
application. Anesthesiology. 86:24–33. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chernik DA, Gillings D, Laine H, Hendler
J, Silver JM, Davidson AB, Schwam EM and Siegel JL: Validity and
reliability of the Observers Assessment of Alertness/Sedation
scale: Study with intravenous midazolam. J Clin Psychopharmacol.
10:244–251. 1990.PubMed/NCBI
|
|
13
|
Yang SQ: China Medical Encyclopedia -
Medical Statistics (1st). Shanghai Science and Technology Press.
Shanghai: 203–204. 2011.
|
|
14
|
Haussmann MF, Vleck CM and Farrar ES: A
laboratory exercise to illustrate increased salivary cortisol in
response to three stressful conditions using competitive ELISA. Adv
Physiol Educ. 31:110–115. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Okholm C, Goetze JP, Svendsen LB and
Achiam MP: Inflammatory response in laparoscopic vs. open surgery
for gastric cancer. Scand J Gastroenterol. 49:1027–1034. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wang SZ, Chen Y, Lin HY and Chen LW:
Comparison of surgical stress response to laparoscopic and open
radical cystectomy. World J Urol. 28:451–455. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kristiansson M, Saraste L, Soop M,
Sundqvist KG and Thörne A: Diminished interleukin 6 and C reactive
protein response to laparoscopic versus open cholecystectomy. Acta
Anesthesiol Scand. 43:146–152. 1999. View Article : Google Scholar
|
|
18
|
Kehlet H: Multimodel approach to control
postoperative pathophysiology and rehabilitation. Br J Anaesth.
78:606–617. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cooper GM, Scoggins AM, Ward ID and Murphy
D: Laparoscopy - a stressful procedure. Anaesthesia. 37:266–269.
1982. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Unlügenç H, Itegin M, Ocal I, Ozalevli M,
Güler T and Işik G: Remifentanil produces vasorelaxation in
isolated rat thoracic aorta strips. Acta Anaesthesiol Scand.
48:7972004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Doi M, Gajraj RJ, Mantzaridis H and Kenny
GN: Prediction of movement at laryngeal mask airway insertion:
Comparison of auditory evoked potential index, bispectral index,
spectral edge frequency and median frequency. Br J Anaesth.
82:203–207. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Alpiger S, Helbo-Hansen HS, Vach W and
Ording H: Efficacy of A-line AEP Monitor as a tool for predicting
acceptable tracheal intubation conditions during sevoflurane
anaesthesia. Br J Anaesth. 94:601–606. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Nishiyama T and Hanaoka K: The A-line ARX
index may be a more sensitive detector of arousal than the
bispectral index during propofol-fentanyl-nitrous oxide anesthesia:
A preliminary investigation. Can J Anaesth. 51:539–544. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kreuer S, Bruhn J, Larsen R, Hoepstein M
and Wilhelm W: Comparison of Alaris AEP index and bispectral index
during propofol-remifentanil anaesthesia. Br J Anaesth. 91:336–340.
2003. View Article : Google Scholar : PubMed/NCBI
|