Introduction
Flexible bronchoscopy is commonly used for the
diagnosis and management of a variety of pulmonary diseases.
However, it is an invasive procedure that can induce coughing,
pain, dyspnea and other adverse effects (1,2). The use
of sedatives not only can increase patients' safety and comfort
(3) but also can make it easier for
the bronchoscopist to perform the procedure and thus avoid
extending its duration (4). In
addition to alleviating the physiological response to airway
irritation during the procedure (5),
the proper sedatives should have a rapid onset and a short duration
of action, in addition to allowing rapid recovery.
Propofol, a non-opioid and nonbarbiturate sedative
hypnotic agent, is frequently used in the induction and maintenance
of anesthesia. The properties of rapid onset and offset of action
and of smooth recovery (6) make
propofol an appealing agent alone or in combination with an opioid
for procedural sedation (7–10). However, dose-dependent respiratory
depression and hypoxemia are possible, owing to interactions and
synergism between sedatives and opioids (11–13).
Dexmedetomidine, a highly selective
α2-adrenoceptor agonist, has an affinity for
α2-adrenoceptors that is 8-fold greater than that of
clonidine (14). In addition to
providing sedative and analgesic effects (15), dexmedetomidine can be applied
generally during fiberoptic intubation or other difficult airway
procedures without respiratory depression (16–18).
Research has revealed that dexmedetomidine alone is inferior to a
combination of propofol and fentanyl for maintaining hemodynamic
stability during endoscopic retrograde cholangiopancreatography
(19). However, few data are
available regarding the effectiveness of a combination of
dexmedetomidine and fentanyl for bronchoscopy. Therefore, the
present prospective, randomized study was conducted to test the
hypothesis that dexmedetomidine-fentanyl is as effective as
propofol-fentanyl for providing satisfactory peripheral oxygen
saturation (SpO2) and maintaining hemodynamic stability
in patients undergoing flexible bronchoscopy.
Materials and methods
Patients
The study protocol was approved by the ethics
committee of the Second Affiliated Hospital of Zhengzhou University
(Zhengzhou, China), and it adhered to the principles of the
Declaration of Helsinki. This study (registration number:
ChiCTR-TRC-13003904) enrolled 100 patients undergoing flexible
bronchoscopic procedures (for example, bronchoalveolar lavage or
transbronchial biopsy) who provided written evidence of informed
consent. The patients, whose ages ranged from 20 to 75 years (mean,
60.11 years) and who had an American Society of Anesthesiologists
(ASA) physical status of I–III, received treatment at the Second
Affiliated Hospital of Zhengzhou University at some point between
December 2013 and May 2014. They were initially randomized to
either of two groups, namely a propofol-fentanyl group (PF group;
n=50) or a dexmedetomidine-fentanyl group (DF group; n=50), on the
basis of a computer-generated randomization list. Exclusion
criteria included the following items: Psychological disorders,
hypersensitivity or allergy to the study drugs, uncontrolled
hypertension (uncontrolled blood pressure >140/90 mmHg), major
abnormalities of liver function, ischemic heart disease and severe
respiratory disease.
When patients arrived in the operating room, they
underwent insertion of a peripheral intravenous cannula for fluid
and drug administration. Their electrocardiograms and
SpO2 were monitored continuously during the procedure,
and blood pressure was automatically and noninvasively measured
every 5 min. At least 5 min prior to the initiation of fentanyl
administration and during the entire bronchoscopic procedure, each
patient received supplemental oxygen at a rate of 4 l/min via nasal
cannula. When SpO2 was <90% for >30 sec, which was
defined as oxygen desaturation or hypoxemia, oxygen delivery was
increased to 6 l/min (20) and
airway assistance maneuvers or devices were used, including verbal
and tactile stimulation, chin lifts, jaw thrusts, a face mask and
manual ventilation.
Flexible bronchoscopy
Any one of four experienced bronchoscopists used a
bronchoscope of the same diameter to perform transnasal
bronchoscopy in all patients, who were placed in a semi-recumbent
position. Topical anesthesia was provided by spraying 2% lidocaine
into the nasopharynx and oropharynx. In addition, 3-ml aliquots of
1% lidocaine were sprayed over the vocal cords, onto the trachea,
and onto the right and left main bronchi. Supplemental local
anesthesia was given as deemed necessary by the bronchoscopist. No
inhaled lidocaine was administered prior to the procedure (21).
Propofol was infused in a target-controlled manner.
However, to guarantee the patients' safety, a dose of 1 µg/kg
dexmedetomidine was used for at least the initial 10 min, and then
a continuous intravenous infusion rate of 0.2–0.7 µg/kg/h was used,
which is in line with the guidelines set forth in 1999 by the US
Food and Drug Administration (22).
Before starting sedation, patients in both groups
received an infusion dose of 1 µg/kg fentanyl (batch no. 1130506;
Yichang Humanwell Pharmaceutical Co., Ltd., Yichang, China).
Thereafter, the patients in the DF group received a loading dose of
1 µg/kg dexmedetomidine (batch no. 13031516: Jiangsu Hengrui
Medicine Co., Ltd., Jiangsu, China), infused continuously for ~12
min, and the loading dose was followed by a continuous intravenous
infusion at a rate of 0.5 µg/kg/h (23). The three-compartment pharmacokinetic
model was used, with the infusion of propofol administered via a
target-controlled syringe infusion pump (Injectomat TIVA Agilia;
Fresenius Kabi, Paris, France), according to each patient's age and
weight. The initial effect-site target for propofol (batch no.
JV642; AstraZeneca, Basiglio, Italy) concentration was 4 µg/ml in
the PF group. Subsequently, the concentration of propofol was
maintained at a level between 2 and 4 µg/ml (24) during the 12-min infusion period.
Loading doses of dexmedetomidine or propofol were observed to
achieve adequate conscious sedation, indicated by the onset of
ptosis. Whenever indications of insufficient sedation were
observed, including signs of pain or discomfort, agitation, a
persistent cough, and inadequate motor or verbal response to
manipulation, an additional 2 ml of 2% lidocaine was administered
into the trachea through the side hole of a flexible bronchoscope.
The number of times that additional lidocaine was administered was
recorded.
Outcome variables
The primary study objectives were the mean
SpO2 and hemodynamic variables. During the procedure,
the SpO2 and hemodynamic variables, including heart rate
(HR), systolic blood pressure (SBP) and diastolic blood pressure
(DBP), were recorded for both groups at the following time points:
1 min before initiation of fentanyl administration (T1),
at the initiation of flexible bronchoscopy (T2), 1 min
after initiation of bronchoscopy (T3), 5 min after
initiation of bronchoscopy (T4) and at the end of
bronchoscopy (T5).
Secondary objectives were cough scores and
discomfort scores as assessed by the patients themselves and also
by the bronchoscopists. At the end of the procedure,
bronchoscopists were asked to record their perception of the
patient's cough during the procedure, using a 10-point visual
analog scale (VAS) on which 0 represented no cough and 10
represented incessant coughing. Two hours after bronchoscopy,
patients were asked to record their perception of their own
coughing associated with the procedure, using the same 10-point
VAS. Patients and bronchoscopists were asked to use a 10-point VAS
to rate patients' discomfort associated with the procedure, where 0
represented no discomfort and 10 represented the greatest possible
discomfort. Willingness to undergo repeat bronchoscopy was also
recorded.
The level of sedation was assessed at T2
and T4 using the Modified Observer's Assessment of
Alertness/Sedation (MOAA/S) scale, detailed in Table I (25). Indications for flexible bronchoscopy,
type of bronchoscopy, duration of procedure, and elapsed time until
recovery were recorded for all patients. Recovery time was defined
as the time (min) elapsed between withdrawal of a flexible
bronchoscope and the moment that the patient was fully awake and
conversant.
 | Table I.Modified Observer's Assessment of
Alertness/Sedation scale (MOAA/S). |
Table I.
Modified Observer's Assessment of
Alertness/Sedation scale (MOAA/S).
| Responsiveness | Score |
|---|
| Agitated | 6 |
| Responds readily to
name spoken in normal tone | 5 |
| Lethargic response
to name spoken in normal tone | 4 |
| Responds only after
name is called loudly and/or repeatedly | 3 |
| Responds only after
mild prodding or shaking | 2 |
| Does not respond to
mild prodding or shaking | 1 |
| Does not respond to
deep stimulus | 0 |
Adverse events
Hypotension (SBP <90 mmHg or mean arterial
pressure <60 mmHg) was treated with an infusion of 10 mg
ephedrine. Bradycardia (HR <60 beats/min) was treated with an
infusion of 0.3 mg atropine. Hypertension (SBP >180 mm Hg or DBP
>100 mm Hg) and tachycardia (HR >100 beats/min and/or
variation of >20% from baseline value) were treated by
administering an additional 2 ml of 2% lidocaine into the
trachea.
Statistical analysis
In a large study, Grendelmeier et al
investigated the safety of sedation with propofol in flexible
bronchoscopy and reported a mean SpO2 of 93% [standard
deviation (SD), 4.3%] in their propofol group (26). For the present smaller study, it was
determined that a sample size of 44 participants per group was
necessary for a two-sided significance level (α) of 0.05 and a
power of 0.9 to detect a 3% difference in the mean SpO2
between the two groups. Assuming a 10% dropout rate, the actual
size needed for each group was 50 participants. The formula used to
calculate the sample size that was required was the following: n=2
[(µα/2+µβ) σ/δ]2, in which δ=3, σ=4.3, α=0.05 and β=0.1.
According to the µ value table, µ0.05/2=1.96 and
µ0.1=1.282, which were added into the formula
(n=44).
The data are presented as mean ± SD, or as number
with the percentage of patients in parentheses. Repeated-measures
analysis of variance was used to test between-group differences in
SpO2, HR, SBP and DBP over time. Continuous outcomes
were analyzed with the Student's t-test or the Mann-Whitney U test
as appropriate in terms of data distribution. Categorical data were
examined with the χ2 test, Fisher's exact test, or
Mann-Whitney U test as appropriate. Statistical analyses were
performed using the Statistical Package for Social Sciences (SPSS
for Windows, version 18.0; SPSS, Inc., Chicago, IL, USA). A P-value
of <0.05 was considered statistically significant.
Results
Comparison of basic patient
characteristics, indications for flexible bronchoscopy, and type or
duration of procedure in the two groups
There were no significant differences between the DF
and PF groups in terms of age, presence of comorbidities, or ASA
physical status (Table II). There
were also no statistically significant differences between the two
groups regarding the indications for bronchoscopy, type of
bronchoscopy, and procedure duration (Table III).
 | Table II.Demographic and baseline
characteristics of patients undergoing flexible bronchoscopy. |
Table II.
Demographic and baseline
characteristics of patients undergoing flexible bronchoscopy.
| Characteristic | DF group
(n=50) | PF group
(n=50) |
|---|
| Age, years | 59.76±7.61 | 60.46±6.93 |
| Male/female
(%) | 27/23 (54/46) | 22/28 (44/56) |
| Body mass index,
kg/m2 | 22.20±3.06 | 21.69±3.16 |
| ASA class |
|
|
| I | 22 (44) | 20 (40) |
| II | 13 (26) | 16 (32) |
|
III | 15 (30) | 14 (28) |
| Comorbidities |
|
|
| Chronic
obstructive pulmonary disease | 7
(14) | 9
(18) |
|
Coronary artery disease | 10 (20) | 8
(16) |
|
Diabetes | 12 (24) | 10 (20) |
 | Table III.Indications for flexible bronchoscopy
and type and duration of procedure. |
Table III.
Indications for flexible bronchoscopy
and type and duration of procedure.
| Bronchoscopy
parameter | DF group
(n=50) | PF group
(n=50) |
|---|
| Indication for
bronchoscopy |
|
|
|
Infection | 13 (26) | 11 (22) |
|
Hemoptysis | 9
(18) | 11 (22) |
|
Suspicion of malignancy | 20 (40) | 18 (36) |
|
Others | 8
(16) | 10 (20) |
| Type of
bronchoscopy |
|
|
|
Inspection | 15 (30) | 17 (34) |
|
Bronchoalveolar lavage | 10 (20) | 9
(18) |
|
Transbronchial biopsy | 18 (36) | 16 (32) |
|
Others | 7
(14) | 8
(16) |
| Duration of
procedure, min | 20.64±2.08 | 21.14±1.87 |
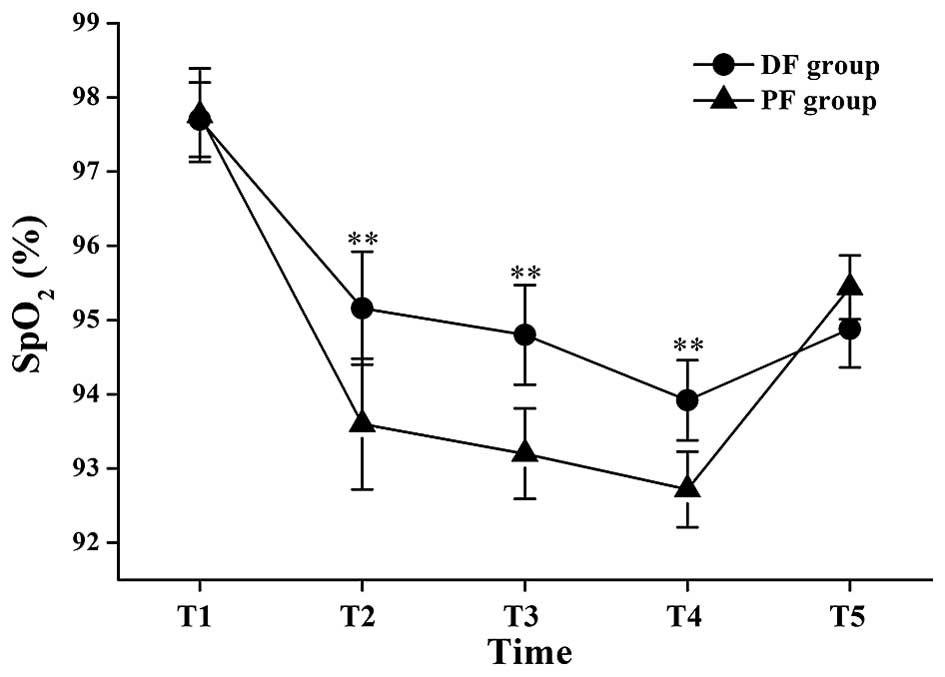
Changes in SpO2
There were no significant differences in
SpO2 values between the two groups at T1 and T5;
however, the mean SpO2 values at the T2, T3 and T4 time
points in the DF group were significantly higher than those in the
PF group (95.16±2.38 vs. 93.6±2.63% at T2: P<0.01; 94.8±2.05 vs.
93.2±1.83% at T3: P<0.01; 93.92±1.64 vs. 92.72±1.6% at T4:
P<0.01; Fig. 1).
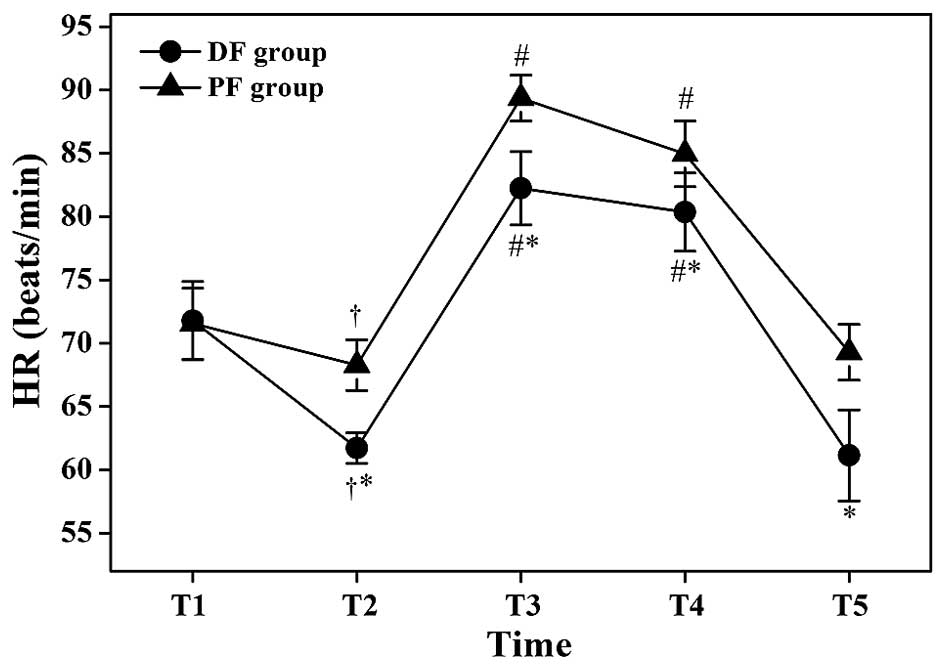
Changes in hemodynamic variables
The HR values at T2 were significantly lower
compared with those at T1 in the same group (P<0.05; Fig. 2), but the HR values at T3 and T4 were
significantly higher compared with those at T2 in the same group
(P<0.05; Fig. 2). The HR values
of the DF group at T2, T3, T4 and T5 were significantly lower
compared with those of the PF group (61.72±3.6 vs. 68.28±5.94
beats/min at T2: P<0.05; 82.24±8.7 vs. 89.36±5.68 beats/min at
T3: P<0.05; 80.36±9.26 vs. 84.96±8.06 beats/min at T4:
P<0.05; 61.14±11.06 vs. 69.28±6.53 beats/min at T5: P<0.05;
Fig. 2).
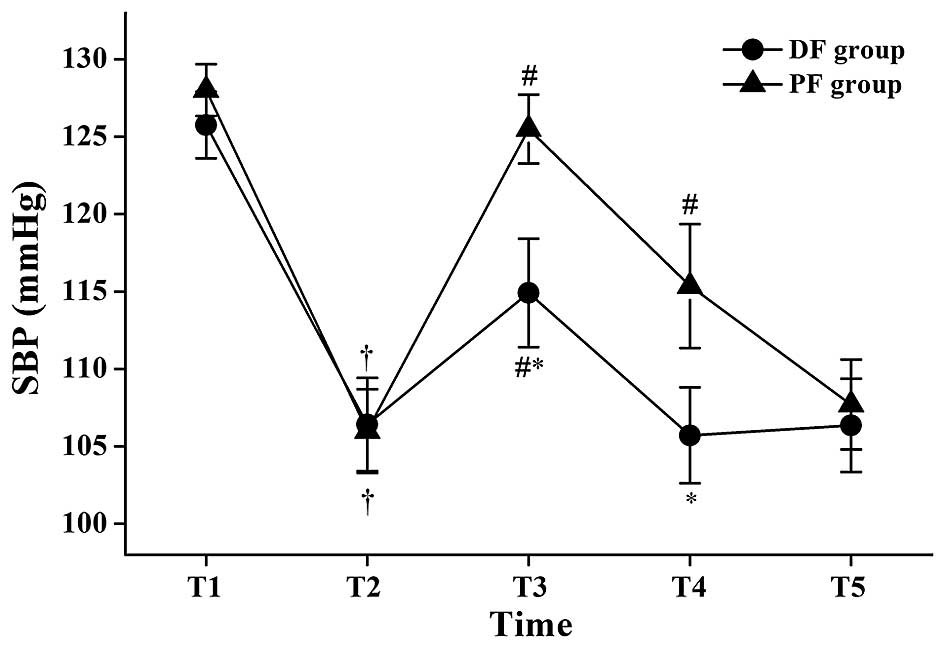
The SBP values at T2 were significantly lower
compared with those at T1 in the same group (P<0.05; Fig. 3), and the SBP values at T3 were
significantly higher compared with those at T2 in the same group
(P<0.05; Fig. 3). In the PF
group, the SBP values at T4 were significantly higher compared with
those at T2 (P<0.05; Fig. 3). The
SBP values of the DF group were significantly lower compared with
those of the PF group at T3 and T4 (114.92±10.66 vs. 125.52±6.65
mmHg at T3: P<0.05; 105.72±9.29 vs. 115.36±11.9 mmHg at T4:
P<0.05, Fig. 3).
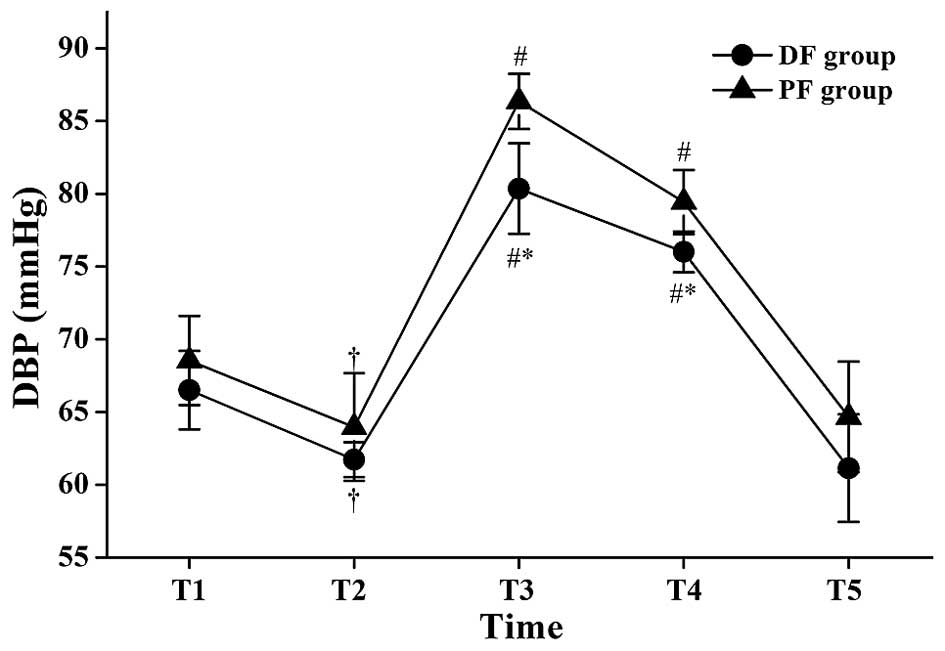
The DBP values at T2 were significantly lower
compared with those at T1 in the same group (P<0.05; Fig. 4), and the DBP values at T3 and T4
were significantly higher compared with those at T2 in the same
group (P<0.05; Fig. 4). The DBP
values of the DF group at T3 and T4 compared with those of the PF
group were statistically lower (80.36±9.26 vs. 86.36±5.77 mmHg at
T3: P<0.05; 75.98±5.27 vs. 79.44±6.64 mmHg at T4: P<0.05;
Fig. 4).
VAS scores, additional lidocaine
administration, MOAA/S scores and recovery times
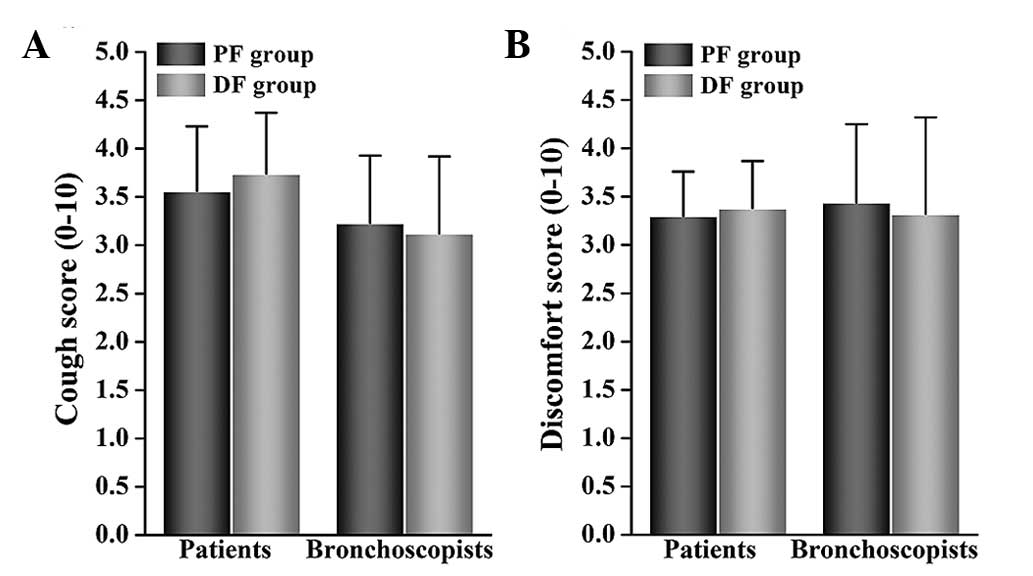
There were no significant differences in VAS scores
for coughing and discomfort between the two groups as rated by
patients or by bronchoscopists (Fig.
5). There was also no significant difference between groups
regarding the number of times that additional lidocaine was
necessary. There was no significant difference between groups
regarding MOAA/S scores at T2 and T4. The recovery times for the DF
group were significantly longer than those for the PF group
(13.1±1.68 vs. 11.91±2.14 min: P<0.05; Table IV).
 | Table IV.Outcome parameters in patients
randomized to dexmedetomidine-fentanyl or propofol-fentanyl. |
Table IV.
Outcome parameters in patients
randomized to dexmedetomidine-fentanyl or propofol-fentanyl.
| Outcome
parameter | DF group
(n=50) | PF group
(n=50) | P-value |
|---|
| No. of times
additional lidocaine was required |
|
| 0.802 |
| 0 | 22 | 20 |
|
| 1 | 13 | 16 |
|
|
>2 | 15 | 14 |
|
| MOAA/S score
5/4/3/2/1/0 |
|
|
|
T2 | 0/5/10/35/0/0 | 0/7/6/37/0/0 | 0.499 |
|
T4 | 15/24/6/5/0/0 | 12/23/8/7/0/0 | 0.808 |
| Recovery time,
min |
13.1±1.68a | 11.91±2.14 | 0.002 |
Adverse events
There were no significant differences in
hypotension, hypertension, tachycardia, or the proportions of
patients who would be willing to repeat the bronchoscopy procedure
between the two groups. However, there was a statistically
significant difference in the number of cases of hypoxemia between
the DF and PF groups (1 and 7 cases, respectively: P<0.05;
Table V). Furthermore, there was a
significant difference in bradycardia between the DF and PF groups
(13 and 5 cases, respectively: P<0.05; Table V).
 | Table V.Adverse events during the
procedure. |
Table V.
Adverse events during the
procedure.
| Adverse event or
parameter | DF group
(n=50) | PF group
(n=50) | P-value |
|---|
| Bradycardia | 13
(26)a | 5
(10) | 0.037 |
| Tachycardia | 6
(12) | 8
(16) | 0.564 |
| Hypotension | 8
(16) | 5
(10) | 0.372 |
| Hypertension | 5
(10) | 7
(14) | 0.538 |
| Hypoxemia | 1
(2)a | 7
(14) | 0.027 |
| Willingness for
repeat of bronchoscopy | 38 (76) | 33 (66) | 0.271 |
Discussion
The results of the present study show that a
combination of dexmedetomidine and fentanyl is superior to a
combination of propofol and fentanyl, the reasons for which are
discussed below.
A variety of sedatives, including benzodiazepines,
opioids and propofol, have been used for bronchoscopy. However,
certain studies have shown that following the use of sedatives,
recovery times are longer and more desaturations occur (27,28).
Although dexmedetomidine produces sedative, analgesic and hypnotic
affects, unlike other sedatives it provides respiratory stability
and does not cause any clinically relevant respiratory depression
(29). This finding has also been
confirmed by further research, which showed that dexmedetomidine
safely produces satisfactory sedation during fiberoptic intubation
or other difficult airway procedures (16–18,30).
Moreover, dexmedetomidine has no effect on end-tidal carbon dioxide
(31), preserves better arterial
saturation (32) and improves
oxygenation (33).
In the present study, the incidence of hypoxemia in
the patients treated with dexmedetomidine was much lower than in
the patients treated with propofol. This is in agreement with the
results of a study by Liao et al (34). This trend has previously been
explained as being due to the addition of an opioid to propofol
resulting in oxygen desaturation in patients undergoing
bronchoscopic procedures (35).
According to a study by Adachi et al,
hemodynamic responses during flexible bronchoscopy reflect an
increase in HR and blood pressure (36). In the present study, a greater
increase in HR and blood pressure at initiation of bronchoscopy
were observed among patients who were given propofol compared with
those who were given dexmedetomidine. These findings show that a
combination of dexmedetomidine and fentanyl is superior to a
combination of propofol and fentanyl in attenuating hemodynamic
responses during flexible bronchoscopy and that specifically, the
former combination maintained hemodynamic stability in the early
stage of the procedure. This was a better result than that reported
by Ryu et al for a dexmedetomidine group compared with a
remifentanil group during flexible bronchoscopy (37); they found no differences between
outcomes for those two sedatives.
Notably, VAS scores for patients' coughing and
discomfort, as recorded by patients and bronchoscopists were no
different between the dexmedetomidine and propofol groups. These
results differed from those of He et al (38) and Hendrickx et al (39) who found that dexmedetomidine had a
less pronounced amnesic effect, which might have occurred because
dexmedetomidine interacted synergistically with fentanyl to produce
deep hypnosis (38,39). This might also explain why
dexmedetomidine was associated with a longer recovery time.
However, on the basis of the present research methodology, the
current study focused on numbers of patients who were given
additional lidocaine two or more times. The exact amount of
lidocaine administered was not recorded. As a result, whether the
total amount of additional lidocaine correlated with the effects of
propofol or dexmedetomidine administration was not determined;
thus, it is not possible to directly draw conclusions regarding the
influence of propofol compared with dexmedetomidine on cough and
discomfort scores. Therefore, the amount of lidocaine spray used
should be recorded in future investigations.
The main adverse effects of dexmedetomidine include
bradycardia, hypotension, and hypertension (40). Bradycardia was observed more often in
the dexmedetomidine group than in the propofol group. Although the
two groups displayed both hypotension and hypertension, the
incidence of these conditions did not differ between groups.
The present study had the following limitations.
First, it was not a blinded study. Patients' level of sedation was
assessed by MOAA/S at only two time points during flexible
bronchoscopy. That might have influenced the results. To remove
sedation level as a confounding factor in future studies, depth of
anesthesia should be assessed by monitoring equipment at additional
time points, along with mean SpO2 values and hemodynamic
variables. Second, aside from bradycardia, hypotension and
hypertension, other adverse effects of dexmedetomidine that have
been observed in other studies, such as delirium, nausea, vomiting,
and shivering, were not recorded. Future studies must address those
additional effects.
In conclusion, with the exception of a longer
recovery time and higher incidence of bradycardia, the present
study found that dexmedetomidine-fentanyl was superior to
propofol-fentanyl in providing satisfactory sedation and peripheral
oxygen saturation during flexible bronchoscopy. Furthermore,
dexmedetomidine-fentanyl attenuated hemodynamic responses and
maintained hemodynamic stability in the early stage of
bronchoscopy.
Acknowledgements
Katharine O'Moore-Klopf, ELS (East Setauket, NY,
USA) provided professional English-language editing of this
article.
References
|
1
|
Poi PJ, Chuah SY, Srinivas P and Liam CK:
Common fears of patients undergoing bronchoscopy. Eur Respir J.
11:1147–1149. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Xavier Scheuermeyer F, Andolfatto G, Qian
H and Grafstein E: Does the sedation regimen affect adverse events
during procedural sedation and analgesia in injection drug users?
CJEM. 15:279–288. 2013.PubMed/NCBI
|
|
3
|
Putinati S, Ballerin L, Corbetta L,
Trevisani L and Potena A: Patient satisfaction with conscious
sedation for bronchoscopy. Chest. 115:1437–1440. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Du Rand IA, Blaikley J, Booton R,
Chaudhuri N, Gupta V, Khalid S, Mandal S, Martin J, Mills J, Navani
N, et al: British Thoracic Society guideline for diagnostic
flexible bronchoscopy in adults. Thorax. 68(Suppl 1): i1–i44. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Davies L, Mister R, Spence DP, Calverley
PM, Earis JE and Pearson MG: Cardiovascular consequences of
fibreoptic bronchoscopy. Eur Respir J. 10:695–698. 1997.PubMed/NCBI
|
|
6
|
Alletag MJ, Auerbach MA and Baum CR:
Ketamine, propofol and ketofol use for pediatric sedation. Pediatr
Emerg Care. 28:1391–1395. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Berkenbosch JW, Graff GR, Stark JM, Ner Z
and Tobias JD: Use of a remifentanil-propofol mixture for pediatric
flexible fiberoptic bronchoscopy sedation. Pediatric Anesthesia.
14:941–946. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Clark G, Licker M, Younossian AB, Soccal
PM, Frey JG, Rochat T, Diaper J, Bridevaux PO and Tschopp JM:
Titrated sedation with propofol or midazolam for flexible
bronchoscopy: A randomised trial. Eur Respir J. 34:1277–1283. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Reyle-Hahn M, Niggemann B, Max M, Streich
R and Rossaint R: Remifentanil and propofol for sedation in
children and young adolescents undergoing diagnostic flexible
bronchoscopy. Paediatr Anaesth. 10:59–63. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Stolz D, Kurer G, Meyer A, Chhajed PN,
Pflimlin E, Strobel W and Tamm M: Propofol vs. combined sedation in
flexible bronchoscopy: A randomised non-inferiority trial. Eur
Respir J. 34:1024–1030. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kodaka M, Okamoto Y, Handa F, Kawasaki J
and Miyao H: Relation between fentanyl dose and predicted
EC50 of propofol for laryngeal mask insertion. Br J
Anaesth. 92:238–241. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Peacock JE, Luntley JB, O'Connor B, Reilly
CS, Ogg TW, Watson BJ and Shaikh S: Remifentanil in combination
with propofol for spontaneous ventilation anaesthesia. Br J
Anaesth. 80:509–511. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Xu J, Yao Z, Li S and Chen L: A
non-tracheal intubation (tubeless) anesthetic technique with
spontaneous respiration for upper airway surgery. Clin Invest Med.
36:E151–E157. 2013.PubMed/NCBI
|
|
14
|
Hammer GB, Drover DR, Cao H, Jackson E,
Williams GD, Ramamoorthy C, Van Hare GF, Niksch A and Dubin AM: The
effects of dexmedetomidine on cardiac electrophysiology in
children. Anesth Analg. 106:79–83. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tan JA and Ho KM: Use of dexmedetomidine
as a sedative and analgesic agent in critically ill adult patients:
A meta-analysis. Intensive Care Med. 36:926–939. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bergese SD, Khabiri B, Roberts WD, Howie
MB, McSweeney TD and Gerhardt MA: Dexmedetomidine for conscious
sedation in difficult awake fiberoptic intubation cases. J Clin
Anesth. 19:141–144. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ramsay MA and Luterman DL: Dexmedetomidine
as a total intravenous anesthetic agent. Anesthesiology.
101:787–790. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Stamenkovic DM and Hassid M:
Dexmedetomidine for fiberoptic intubation of a patient with severe
mental retardation and atlantoaxial instability. Acta Anaesthesiol
Scand. 50:1314–1315. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Muller S, Borowics SM, Fortis EA, Stefani
LC, Soares G, Maguilnik I, Breyer HP, Hidalgo MP and Caumo W:
Clinical efficacy of dexmedetomidine alone is less than propofol
for conscious sedation during ERCP. Gastrointest Endosc.
67:651–659. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chhajed PN and Glanville AR: Management of
hypoxemia during flexible bronchoscopy. Clin Chest Med. 24:511–516.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wahidi MM, Jain P, Jantz M, Lee P,
Mackensen GB, Barbour SY, Lamb C and Silvestri GA: American College
of Chest Physicians consensus statement on the use of topical
anesthesia, analgesia and sedation during flexible bronchoscopy in
adult patients. Chest. 140:1342–1350. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Panzer O, Moitra V and Sladen RN:
Pharmacology of sedative-analgesic agents: Dexmedetomidine,
remifentanil, ketamine, volatile anesthetics and the role of
peripheral mu antagonists. Crit Care Clin. 25:451–469. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gerlach AT and Dasta JF: Dexmedetomidine:
An updated review. Ann Pharmacother. 41:245–254. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhang X, He W, Wu X, Zhou X, Huang W and
Feng X: TCI remifentanil vs. TCI propofol for awake fiber-optic
intubation with limited topical anesthesia. Int J Clin Pharmacol
Ther. 50:10–16. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
25
|
Drake LM, Chen SC and Rex DK: Efficacy of
bispectral monitoring as an adjunct to nurse-administered propofol
sedation for colonoscopy: A randomized controlled trial. Am J
Gastroenterol. 101:2003–2007. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Grendelmeier P, Kurer G, Pflimlin E, Tamm
M and Stolz D: Feasibility and safety of propofol sedation in
flexible bronchoscopy. Swiss Med Wkly. 141:w132482011.PubMed/NCBI
|
|
27
|
Gasparini S: It is time for patients to
undergo bronchoscopy without discomfort. Eur Respir J. 38:507–509.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Jantz MA: The old and the new of sedation
for bronchoscopy. Chest. 135:4–6. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ebert TJ, Hall JE, Barney JA, Uhrich TD
and Colinco MD: The effects of increasing plasma concentrations of
dexmedetomidine in humans. Anesthesiology. 93:382–394. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Grant SA, Breslin DS, MacLeod DB, Gleason
D and Martin G: Dexmedetomidine infusion for sedation during
fiberoptic intubation: A report of three cases. J Clin Anesth.
16:124–126. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Deutsch E and Tobias JD: Hemodynamic and
respiratory changes following dexmedetomidine administration during
general anesthesia: Sevoflurane vs desflurane. Pediatr Anesth.
17:438–444. 2007. View Article : Google Scholar
|
|
32
|
Koroglu A, Teksan H, Sagir O, Yucel A,
Toprak HI and Ersoy OM: A comparison of the sedative, hemodynamic
and respiratory effects of dexmedetomidine and propofol in children
undergoing magnetic resonance imaging. Anesth Analg. 103:63–67.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Venn RM, Hell J and Grounds RM:
Respiratory effects of dexmedetomidine in the surgical patient
requiring intensive care. Crit Care. 4:302–308. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Liao W, Ma G, Su QG, Fang Y, Gu BC and Zou
XM: Dexmedetomidine vs. midazolam for conscious sedation in
postoperative patients undergoing flexible bronchoscopy: A
randomized study. J Int Med Res. 40:1371–1380. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Yoon HI, Kim JH, Lee JH, Park S, Lee CT,
Hwang JY, Nahm SF and Han S: Comparison of propofol and the
combination of propofol and alfentanil during bronchoscopy: A
randomized study. Acta Anaesthesiol Scand. 55:104–109. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Adachi YU, Suzuki K, Obata Y, Doi M and
Sato S: Is the hemodynamic response to nasotracheal fiberoptic
bronchoscopy less than that following orotracheal bronchoscopy?
Anesth Analg. 105:5432007. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Ryu JH, Lee SW, Lee JH, Lee EH, Do SH and
Kim CS: Randomized double-blind study of remifentanil and
dexmedetomidine for flexible bronchoscopy. Br J Anaesth.
108:503–511. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
He XY, Cao JP, Shi XY and Zhang H:
Dexmedetomidine vs. morphine or fentanyl in the management of
children after tonsillectomy and adenoidectomy: A meta-analysis of
randomized controlled trials. Ann Otol Rhinoly Laryngol.
122:114–120. 2013. View Article : Google Scholar
|
|
39
|
Hendrickx JF, Eger EI II, Sonner JM and
Shafer SL: Is synergy the rule? A review of anesthetic interactions
producing hypnosis and immobility. Anesth Analg. 107:494–506. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Piao G and Wu J: Systematic assessment of
dexmedetomidine as an anesthetic agent: A meta-analysis of
randomized controlled trials. Arch Med Sci. 10:19–24. 2014.
View Article : Google Scholar : PubMed/NCBI
|