Introduction
Intestinal pseudo-obstruction (IpsO) is defined as
ineffective intestinal propulsion which occurs in the absence of
mechanical or obstructive factors (1). Cases, in whom IpsO is the primary
clinical feature, are typically associated with connective tissue
diseases. However, IpsO presenting as the first manifestation in
systemic lupus erythematosus (SLE) is rare, and <30 cases of
IpsO in patients with SLE have been reported (1–4).
Clinical features generally include severe abdominal symptoms, such
as distension, pain, nausea and vomiting, while radiographic signs
show gaseous small bowel distension with air-fluid levels. Acute
lupus pneumonitis (ALP) is an uncommon pulmonary manifestation of
SLE, and lung involvement has only been reported in 3% of SLE
patients (5,6). ALP is an unusual but life threatening
complication of SLE, and usually presents with the acute onset of
fever, cough, tachypnea and hypoxia. The radiological sign of ALP
is consolidations in one or more areas, and is often associated
with pleural effusion and pulmonary arterial hypertension. The
majority of ALP responds to steroids and some requires treatment
with cyclophosphamide; however, the rate of mortality remains high
(5,7). IpsO and ALP occurring in a single
patient, described as co-manifestation with SLE, has not been
reported previously. Herein, we report a case in which IpsO was the
initial presentation of SLE, and secondary onset of ALP occurred
after emergency surgery.
Case report
A 26-year-old female, complaining of abdominal pain,
nausea, vomiting and constipation for 1 day, was admitted to the
emergency room of the Second Affiliated Hospital of Zhejiang
University (Hangzhou, China) in June 2013. Written informed consent
was obtained from the patient. Physical examinations showed
distress countenance, soft abdomen, absence of bowel sounds,
abdominal tenderness but no rebound tenderness. The auxiliary
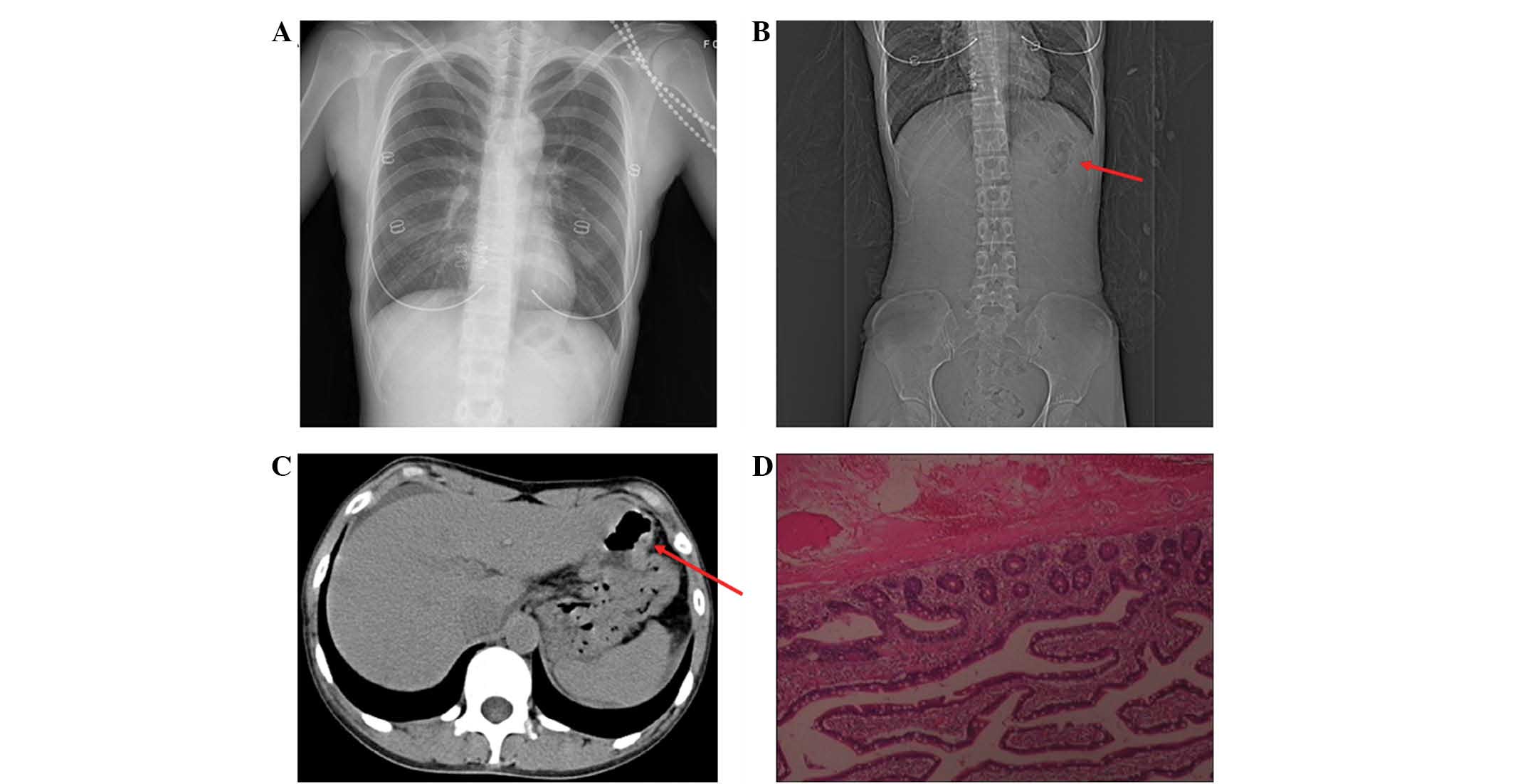
examinations of chest X-ray (Philips Medical Systems B.V.,
Eindhoven, The Netherlands) (Fig.
1A), white blood cell (WBC) count, hemoglobin (HGB),
erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and
urinalysis were normal. Computed tomography (CT) scanning showed
that the jejunal wall was thickened and streaky (Fig. 1B and C), and a small quantity of
ascites was observed. The patient denied any history of hereditary,
infectious or autoimmune diseases. The patient was thought to have
strangulated intestinal obstruction, and an emergency laparotomy
was performed. During the operation, ~80 cm of the jejunum showed
hyperemia and edema, with multiple petechiae on the serosal
surface, and lymph node enlargement in the mesentery. In addition,
~800 ml turbid peritoneal fluid was detected, but no bowel
perforation. Peritoneal lavage, segmental resection of the diseased
jejunum and placement of a jejunostomy fistula were performed.
Culture of the peritoneal fluid for bacteria and atypical bacteria
was negative. Pathological examination of the jejunum using
hematoxylin (Shanghai Bioscience & Technology Co., Ltd.,
Shanghai, China) and eosin (Shanghai SSS Reagent Co., Ltd.,
Shanghai, China) (H&E) staining showed chronic inflammation of
intestinal mucosa, with submucosal anapetia, congestion, hemorrhage
and interstitial edema. The muscle layer showed atrophy,
hemorrhage, serosal congestion and edema (Fig. 1D).
Post-operatively, intestinal peristalsis did not
recover, and a gastrointestinal decompression tube was placed in
the duodenum. Apart from the bowel problem, sporadic rashes and
mild fever without clear origin appeared. Following anti-infective
treatment (ceftazidimine, 2.5 g intravenous injection, q.8.h;
Hainan Haling Chemipharma Corporation, Ltd., Haikou, China) and
careful nursing with electrocardiograph monitoring (MP 30; Philips
Medical Systems B.V.) for 10 days, the patient demonstrated
clinical improvement (abdominal pain was relieved, and the patient
experienced no chills, nausea or vomiting, and vital signs were
stable) and was discharged.
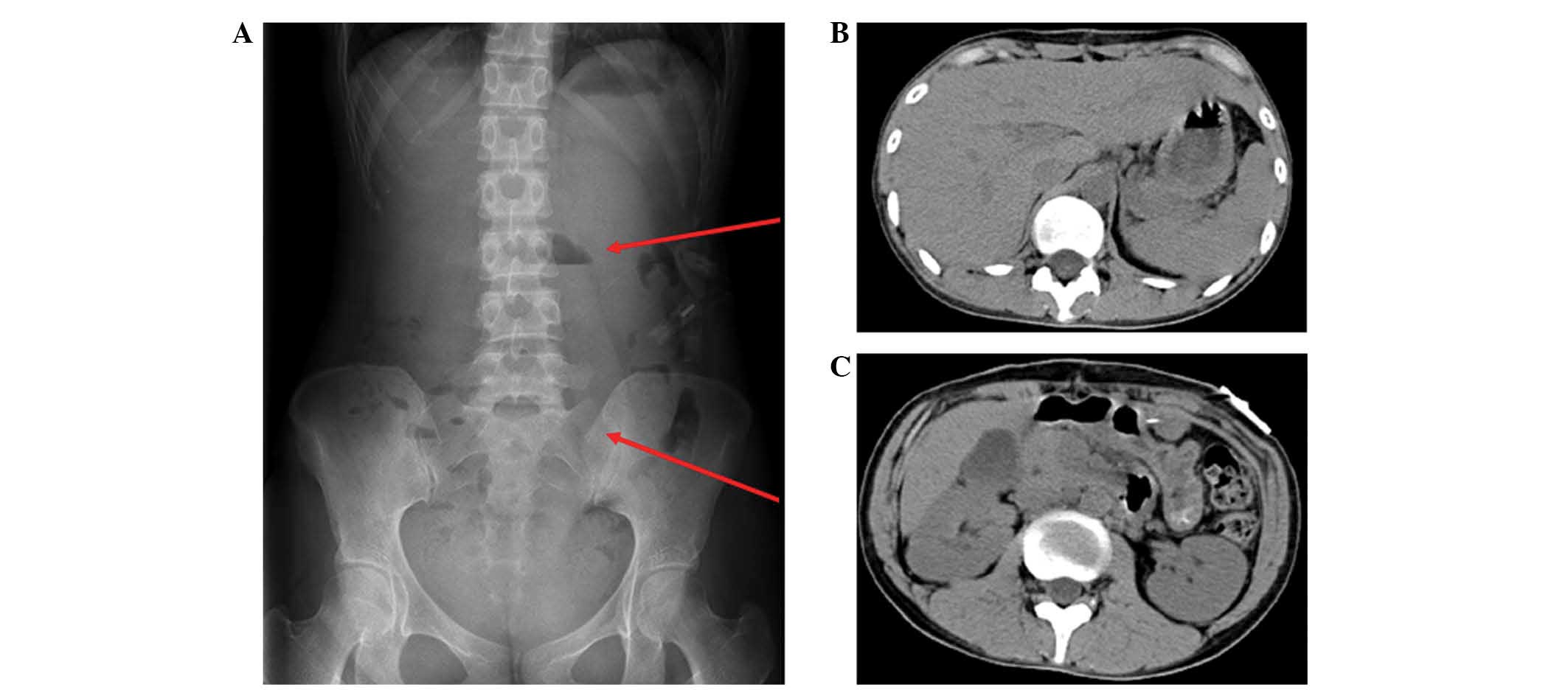
After 5 days, the patient was readmitted due to high
fever (39.2°C), upper abdominal pain, nausea and vomiting,
particularly after a fatty meal. Abdominal X-ray and CT scanning
(The Somatom Sensation 16; Siemens AG, Munich, Germany) revealed
sporadic air-fluid levels and intestinal wall thickness (Fig. 2). Anti-infective treatment
(cefoperazone and sulbactam, both 1.5 g intravenous infection,
q.12.h; Pfizer, Inc., New York, NY, USA) was administered, but was
ineffective. Multiple rashes on the lower extremities appeared on
the fourth day, and laboratory examinations showed a rheumatoid
factor of 20.4 IU/ml (increased), antinuclear antibody 1:320
(increased); ESR 26.00 mm/h (increased); anti-ribonucleoprotein
antibody +++ (strong), anti-Smith antibody +++ (strong), anti
Sjogren's syndrome A antibody +++ (strong) and anti-Sjogren's
syndrome B antibody + (weak). Antibodies against double
stranded-DNA was not detected; complement (C3), 0.39 g/l
(decreased); CRP, 7.0 mg/l (normal); WBC, 2.5×109/l
(decreased) and HGB, 89 g/l (decreased). Furthermore, the patient
had experienced hair loss and multiple red rashes in response to
strong sunlight the previous year. SLE and lupus-related IpsO were
then diagnosed according to American College of Rheumatology
criteria (1997) (8), and the
Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) score
was 10 (8). The patient was treated
with 2 mg/kg/day methylprednisolone (Pfizer, Inc.) and her general
condition improved after 2 days.
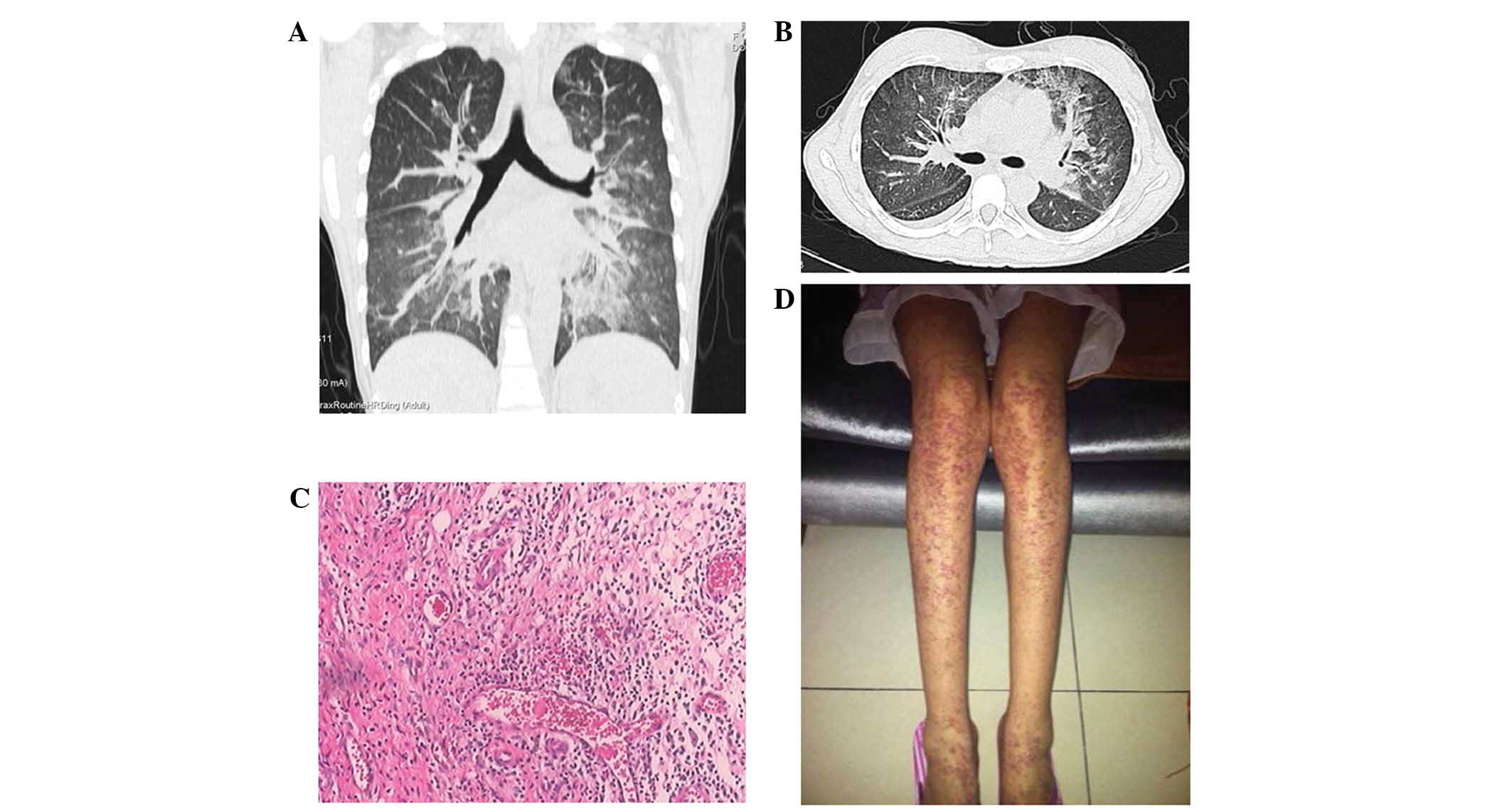
However, the patient had sudden onset of fever
(40.4°C) and dyspnea, oxygen saturation (SaO2) was 87%,
and arterial blood gas analysis revealed a pH of 7.409,
PCO2, 33.6 mmHg and PO2, 83.9 mmHg. Further
laboratory examination showed: Glutamic pyruvic transaminase, 436
U/l (increased); glutamic oxaloacetic transaminase, 740 U/l
(increased); K+, 3.36 mmol/l (decreased); and WBC, HGB,
CRP and urinalysis were normal. On chest CT, both lungs showed
ground-glass appearance, with uneven density, interlobular septal
thickening and bilateral hydrothorax (Fig. 3A and B). Anti-infective treatment
(imipenem and cilastatin, 0.5 g intravenous injection, q.8.h) was
administered for 3 days; however, fever and dyspnea were not
alleviated. A comprehensive infectious work-up (blood, sputum and
urine cultures) was negative. A bronchoalveolar lavage (BAL;
Olympus BX43; Olympus Corporation, Tokyo, Japan) examination from
the affected areas was also negative for gram positive/negative
bacteria, viral infections, fungal infections, acid fast bacilli or
hemosiderin-laden macrophage. The erythematous rash was
accentuated, and pathological biopsy results (using H&E
staining) showed subcutaneous fibrous tissue hyperplasia with
inflammatory cell infiltration (Fig. 3C
and D). ALP was finally diagnosed and high-dose (1 g/day)
methylprednisolone + gamma globulin therapy was administered. After
3 days treatment, the patient's temperature dropped to 37.0°C and
dyspnea was significantly ameliorated. This therapy was followed by
2 mg/kg/day methylprednisolone as maintenance treatment, and
glycyrrhizin (Minophagen Pharmaceutical Co., Ltd., Tokyo, Japan) to
improve liver function. Repeat chest CT scan showed significant
improvement.
During long-term tapering period or after stopping
corticosteroids (methylprednisolone, Pfizer, Inc.), the patient
recovered well with no relapse detected.
Discussion
The present study presents a rare case in which IpsO
was the initial presentation of SLE with secondary onset of ALP
after emergency surgery. To the best of our knowledge, there have
been no previous reports of IpsO and ALP occurring in a single
patient.
IpsO is defined as the presence of clinical features
suggesting intestinal obstruction, but without organic obstruction
(9). As in the present case, the
clinical manifestations of IpsO include abdominal pain, nausea,
vomiting, absence of bowel sounds and may include constipation and
fever (4). An X-ray and CT scan
frequently show air-fluid levels and thickening of the small and/or
large intestinal wall. IpsO may be the first manifestation of SLE
in some patients; however, it usually represents a complication,
with few case series described in the literature (1,2,10). IpsO is easily confused with
mechanical intestinal obstruction and represents a diagnostic
challenge for the surgeon. Ureterohydronephrosis is highly
associated with IpsO in SLE (1,4,10), as repeated urinalysis examination
results were negative, ureterohydronephrosis did not occur in this
patient.
The pathophysiology of IpsO secondary to SLE remains
unclear (9), although the hypotheses
have suggested dysmotility due to a primary myopathy or secondary
to an immune complex mediated vasculitis (11). The pathological characteristics of
the gastrointestinal tract in chronic intestinal pseudo-obstruction
(CIPO) patients include widespread myocyte necrosis, severe atrophy
and fibrosis in the muscularis layer; active serositis with serosal
thickening and fibrosis, with little or no evidence of vasculitis
or injury (11,12). In the present AIPO case, the
pathological results of the jejunum showed muscle layer atrophy,
with submucosal anapetia, congestion and hemorrhage. No evidence of
vasculitis or thromboembolism was detected. Therefore, the present
case supports the hypothesis that the clinical features of AIPO in
SLE patients appear to be the result of a primary intestinal smooth
muscle myopathy, similar to that in CIPO.
ALP is an uncommon (1–12%) manifestation, but may be
a life-threatening complication of SLE (12). The clinical features of ALP are
characterized by acute onset of fever, cough, pleurisy and dyspnea.
The key radiographic manifestation in the majority of cases is
pulmonary infiltration, which appears on CT scan as ground-glass or
honeycomb appearance (5,13). The diagnosis of ALP is essential to
exclude other causes of lung infiltration, particularly infective
pneumonia (7). In the present case
infective pneumonia was excluded, as a comprehensive infectious
work-up was negative and anti-infective treatment was ineffective.
Diffuse alveolar hemorrhage was excluded by the negative results of
hemosiderin-laden macrophage in BAL fluid. ALP was finally
diagnosed by the syndrome of acute reversible hypoxemia, the
abnormal results of CT scan, and the exclusion of other causes of
lung infiltration. The pathophysiology of ALP is based on an acute
injury to the alveolar capillary units in pulmonary vasculature
(7). ALP typically occurs during the
active stage of SLE, which may partially explain why mortality in
ALP is ~50% even when treated with large doses of steroids
(14). Emergency surgery has been
shown to be an independent risk factor for increasing the
complication rate and morbidity of SLE patients (15,16). In
the present case, although the SLEDAI score was 10, ALP occurred,
which may be explained by the emergency surgery performed for IpsO.
The trauma of abdominal operation enhances inflammatory function,
which may have promoted the activity of autoimmunity in SLE
patients and eventually caused the occurrence of ALP.
The recommended therapy for ALP is high-dose
methylprednisolone with gamma globulin supplementation. Early
treatment with corticosteroids may significantly attenuate vascular
injury. In the present case, the patient's clinical symptoms were
ameliorated and the radiographic results showed improvement
following high-dose methylprednisolone + gamma globulin supplement
therapy for 3 days followed by 2 mg/kg methylprednisolone as
maintenance treatment.
In conclusion, we report the first case of ALP and
IpsO co-existing in a patient with SLE. It remains a challenge for
the surgeon to establish the correct diagnosis and prevent
inappropriate surgical intervention when IpsO plays a role in the
initial presentation of SLE. ALP typically occurs during the active
stage of SLE, thus emergency surgery may increase the rate of this
complication. Early immunosuppressive therapy could be lifesaving
in these patients.
Acknowledgements
This study was supported by the Natural Science
Foundation of Zhejiang Province (grant. no. LY14H160033).
References
|
1
|
Kansal A, Jain A, Thenozhi S and Agarwal
V: Intestinal pseudo-obstruction associated with biliary tract
dilatation in a patient with systemic lupus erythematosus. Lupus.
22:87–91. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ceccato F, Salas A, Góngora V, Ruta S,
Roverano S, Marcos JC, Garcìa M and Paira S: Chronic intestinal
pseudo-obstruction in patients with systemic lupus erythematosus:
Report of four cases. Clin Rheumatol. 27:399–402. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Khairullah S, Jasmin R, Yahya F, Cheah TE,
Ng CT and Sockalingam S: Chronic intestinal pseudo-obstruction: A
rare first manifestation of systemic lupus erythematosus. Lupus.
22:957–960. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen YQ, Xue Q and Wang NS: Visceral
muscle dysmotility syndrome in systemic lupus erythematosus: Case
report and review of the literature. Rheumatol Int. 32:1701–1703.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chaiamnuay S, Heck LW, Bell WC and Bastian
HM: Acute granulomatous lupus pneumonitis: The first case report.
Lupus. 16:201–204. 2007.PubMed/NCBI
|
|
6
|
Cervera R, Khamashta MA, Font J,
Sebastiani GD, Gil A, Lavilla P, Doménech I, Aydintug AO,
Jedryka-Góral A, de Ramón E, et al: Systemic lupus erythematosus:
Clinical and immunologic patterns of disease expression in a cohort
of 1,000 patients. The European Working Party on Systemic Lupus
Erythematosus. Medicine (Baltimore). 72:113–124. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sarkar S and Saha K: Bilateral acute lupus
pneumonitis in a case of rhupus syndrome. Lung India. 29:280–282.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hochberg MC: Updating the American College
of Rheumatology revised criteria for the classification of systemic
lupus erythematosus. Arthritis Rheum. 40:17251997. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cacoub P, Benhamou Y, Barbet P, Piette JC,
Le Cae A, Chaussade S, Cadranel JF, Callard P, Opolon P and Godeau
P: Systemic lupus erythematosus and chronic intestinal
pseudoobstruction. J Rheumatol. 20:377–381. 1993.PubMed/NCBI
|
|
10
|
Mok MY, Wong RW and Lau CS: Intestinal
pseudo-obstruction in systemic lupus erythematosus: An uncommon but
important clinical manifestation. Lupus. 9:11–18. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Park FD, Lee JK, Madduri GD and Ghosh P:
Generalized megaviscera of lupus: Refractory intestinal
pseudo-obstruction, ureterohydronephrosis and megacholedochus.
World J Gastroenterol. 15:3555–3559. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hill PA, Dwyer KM and Power DA: Chronic
intestinal pseudo-obstruction in systemic lupus erythematosus due
to intestinal smooth muscle myopathy. Lupus. 9:458–463. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Matthay RA, Schwarz MI, Petty TL, Stanford
RE, Gupta RC, Sahn SA and Steigerwald JC: Pulmonary manifestations
of systemic lupus erythematosus: Review of twelve cases of acute
lupus pneumonitis. Medicine (Baltimore). 54:397–409. 1975.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Urowitz MB, Bookman AA, Koehler BE, Gordon
DA, Smythe HA and Ogryzlo MA: The bimodal mortality pattern of
systemic lupus erythematosus. Am J Med. 60:221–225. 1976.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Koh ET, Seow A, Leong KH and Chng HH: SLE
mortality in an oriental population. Lupus. 6:27–31. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Papa MZ, Shiloni E, Vetto JT, Kastner DL
and McDonald HD: Surgical morbidity in patients with systemic lupus
erythematosus. Am J Surg. 157:295–298. 1989. View Article : Google Scholar : PubMed/NCBI
|