Introduction
Hodgkin lymphoma (HL) is a malignant neoplasm of the
lymphatic tissue and one of the few adult malignancies that can be
successfully treated in the majority of cases (1). It is commonly found in the lymph nodes,
spleen, liver, bone marrow and other sites, with an incidence of
2–4 per 100,000 individuals annually (2). HLs predominantly involve the lymph
nodes and only ~5% arise in extranodal sites, in contrast to 30% of
non-HL cases presenting in extranodal sites (3). Primary extranodal lymphoma is less
common and is predominately non-HL (4–7).
Approximately 5% of all malignant neoplasms of the
head and neck are malignant lymphomas, which may include the
involvement of nodal or extranodal sites (8). The head and neck region is the second
most common anatomical site of extranodal lymphomas. In HL, the
development and spreading of extranodal lesions may occur in any
organ system, simulating other infectious or neoplastic diseases
(9). Extranodal involvement
constitutes an important pretreatment prognostic factor in patients
with lymphoma, and its incidence has increased in the last two
decades (10). Numerous studies have
indicated that extranodal disease involving >1 site presents a
worse outcome (11).
In non-HL, the second most common site of extranodal
involvement is the skin, with the gastrointestinal tract being the
first most common site (12). Unlike
non-HL, in which skin involvement is well-recognized, skin
infiltration of HL is extremely rare and is associated with poor
prognosis. The frequency of skin involvement is estimated to be
3.4% in HL, and its most common clinical presentation is a single
or multiple dermal or subcutaneous nodules (13).
Despite recent scientific progress, pathological
(immunohistochemical and morphological) examination is highly
beneficial in the diagnosis of HL (14). Morphologically, classical HL (cHL) is
characterized by neoplastic multinucleated mononuclear Hodgkin and
Reed-Sternberg (RS) cells, which typically account for 1–5% of all
cells in a cHL specimen (15). These
cells were associated with a microenvironment that consists of
abundant non-neoplastic cells, such as plasma cells, granulocytes,
histiocytes and lymphocytes, in varying proportions (16).
cHL has a bimodal age incidence, with the majority
of cases occurring between the ages of 15 and 35 years, and a
second peak incidence observed in older adults (11). No clearly defined risk factors have
been identified for the development of HL, and the cause of the
disease has yet to be elucidated. Certain factors demonstrated to
be associated with HL include immune suppression, viral exposures
and familial factors (12). Patients
with extranodal involvement were predominantly young males, and the
majority of the patients exhibited stage IV disease (13).
In the present case, a 25-year-old male, who
presented with a hard painless mass above the right superciliary
arch 2 months prior to admission, was subsequently diagnosed with
mixed cellularity cHL. To the best of our knowledge, this is the
first report of such a case. Written informed consent was obtained
from the patient.
Case report
A 25-year-old male, with a 2-month history of a
painless right frontal neoplasm with a similar hardness to that of
a bone fibroma, presented at the Department of Otolaryngology Head
and Neck Surgery (Shanghai First People's Hospital, Shanghai,
China) in April 2013 for diagnosis and surgical treatment. Soon
after the presentation of the first mass, the patient detected
another mass on the sternum, which had similar characteristics to
the initial mass. After ~1 month, the patient identified a 1×2-cm
sized mass in the left cervical lymph node, without pain or fever.
Prior to admission at the Shanghai First People's Hospital, a head
computed tomography (CT) scan had been performed at a different
hospital, and the imaging diagnosis indicated frontal fibroma;
however, the patient refused treatment and was subsequently
admitted to our hospital. In addition to the aforementioned
symptoms, the patient did not experience any discomfort, and his
daily life had not been affected significantly.
The involvement of forehead and cervical lymph node
rendered the presence of an otolaryngologist necessary to
participate in the detection and identification of the lesion.
Through a series of preoperative blood tests, the patient was
diagnosed with hepatitis B. Subsequent to the relevant
examinations, the patient underwent surgery performed at the
Department of Otolaryngology Head and Neck Surgery as his symptoms
were consistent with frontal fibroma. During surgery, the hard mass
on the right frontal area was found to be part of the subcutaneous
soft tissue, in proximity to the frontal bone surface but with a
relatively clear boundary. Therefore, the enlargement on the left
cervical lymph node was removed, in addition to the frontal
neoplasm, and both were subjected to pathological analysis. As the
surgery was performed by the Department of Otolaryngology Head and
Neck Surgery, the sternum mass was not removed.
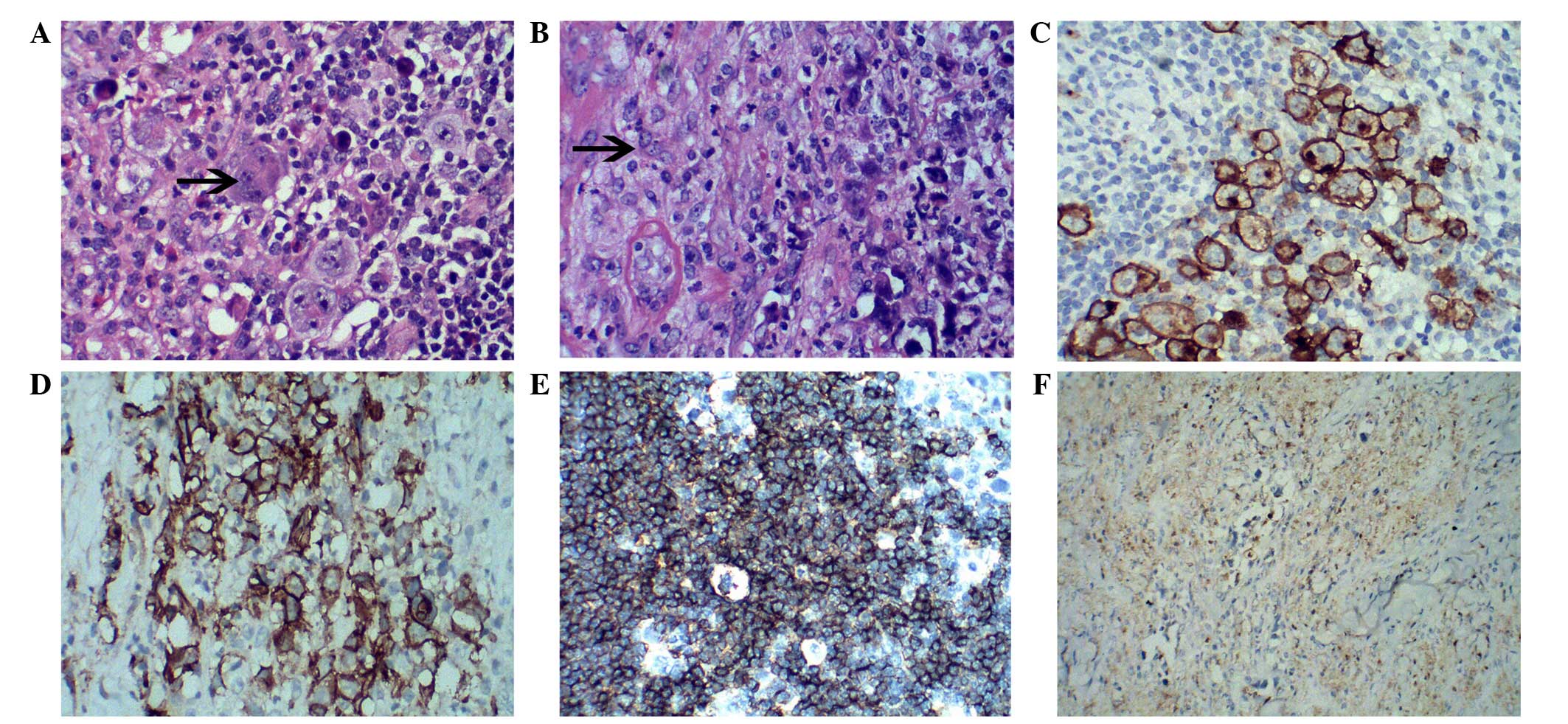
Postoperative pathology results were pathologically
atypical. Subsequent to a discussion of the case with clinicians
from Shanghai Ruijin Hospital and Zhongshan Hospital, a repeat
immunohistochemical staining was performed and the patient was
diagnosed with cHL of mixed cellularity with right frontal soft
tissue involvement. Samples from the patient were fixed in buffered
formalin, paraffin embedded and cut into 4-mm-thick sections prior
to staining with hematoxylin-eosin (HE). Histological analysis with
HE staining was performed on the mass of the left cervical lymph
nodes (Fig. 1A) and the right
frontal subcutaneous soft tissue (Fig.
1B). Immunohistochemical staining was conducted on fixed,
paraffin-embedded tissue sections using mouse anti-human CD30
(1:50; IS602), CD20 (1:200; IS604) and KP1 monoclonal antibodies
(1:4,000; IS609; all Dako North America, Inc., Carpinteria, CA,
USA). The results of immunohistochemical staining revealed that the
lymph node mass (Fig. 1C) and the
forehead subcutaneous soft tissue (Fig.
1D) were CD30-positive. In addition, the lymph node tissue was
also CD20-positive (Fig. 1E), and
the right frontal subcutaneous soft tissue was KP1-negative
(Fig. 1F). As some studies on cHL
cases have demonstrated that RS-H cells have a typical
immunophenotypic profile: CD15+, CD30+, while
high CD20+, dispersed cells exhibited a significant
correlation with longer overall survival and a trend toward
improved progression-free survival (17,18).
Kamper et al (18) showed
that high expression of CD68 (KP1) and CD163 in cHL cases
correlated with the presence of RS-H cells infected by EBV. Based
on the aforementioned findings, the patient was transferred to the
Department of Hematology for treatment. The progression of disease
and the effectiveness of the treatment was monitored by the present
authors. During the treatment, a biopsy of the sternum nodule was
performed, which was not found to be relevant to the disease.
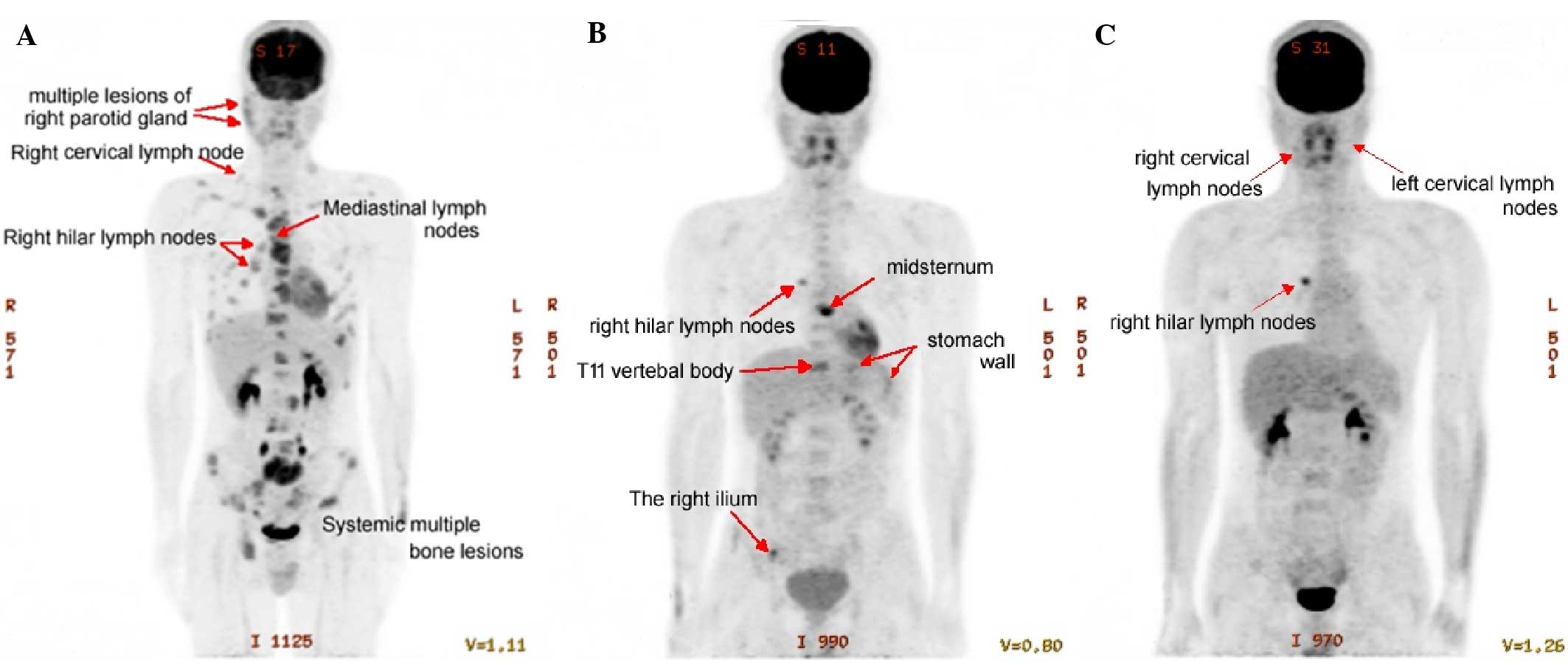
During the treatment course at the Department of
Hematology, the patient received positron emission tomography
(PET)-CT examination. The results indicated that the right
cervical, right supraclavicular, right hilar and mediastinal sites
presented multiple lymph node masses and systemic multiple bone
lesions (Fig. 2A). According to the
Cotswold staging system (19), the
patient was classified as stage IV B with soft tissue and bone
involvement. The patient was treated with six cycles of
conventional and two cycles of consolidation chemotherapy according
to the doxorubicin (Adriamycin), bleomycin, vindesine and
dacarbazine (ABVD) regimens, and obtained a satisfactory curative
effect. A total of 400 mg Adriamycin, 15 mg Bleomycin, 4 mg
Vindesine and 600 mg Dacarbazine was administered at day 1,
followed by a 15-day interval prior to the same treatment, which
composed a complete chemotherapy cycle. A one-month break was
included between each chemotherapy cycle. A second PET-CT was
performed in March 2014 following the eight cycles of chemotherapy
(Fig. 2B), and the results indicated
that the right hilar lymph node mass had increased in size, while
multiple bone lesions remained on the gladiolus, T11 vertebral body
and the right ilium. Compared with the initial PET-CT scan, the
tumors were significantly decreased, but several lesions remained.
Therefore, the hematologist at our hospital administered a further
six cycles of ifosfamide, gemcitabine, vinorelbine and prednisone
(IGEV regimen), and the patient exhibited a significant
improvement. The IGEV regimen included 1.4 g gemcitabine and 30 mg
vinorelbine at day 1, and 2 g ifosfamide and 100 mg prednisone at
days 1–4. Following the aforementioned therapy, a third PET-CT scan
was performed with a full-body PET scanner in 3-dimensional mode
(Fig. 2C). The scan revealed
multiple tumors invading the sternum, thoracic vertebra, ribs and
ilium. Compared with the former PET-CT scan (Fig. 2B), the glucose metabolism of the bone
lesions had recovered to a normal level, as it was no longer
aggregated, which indicated that the treatments were effective in
achieving a partial response.
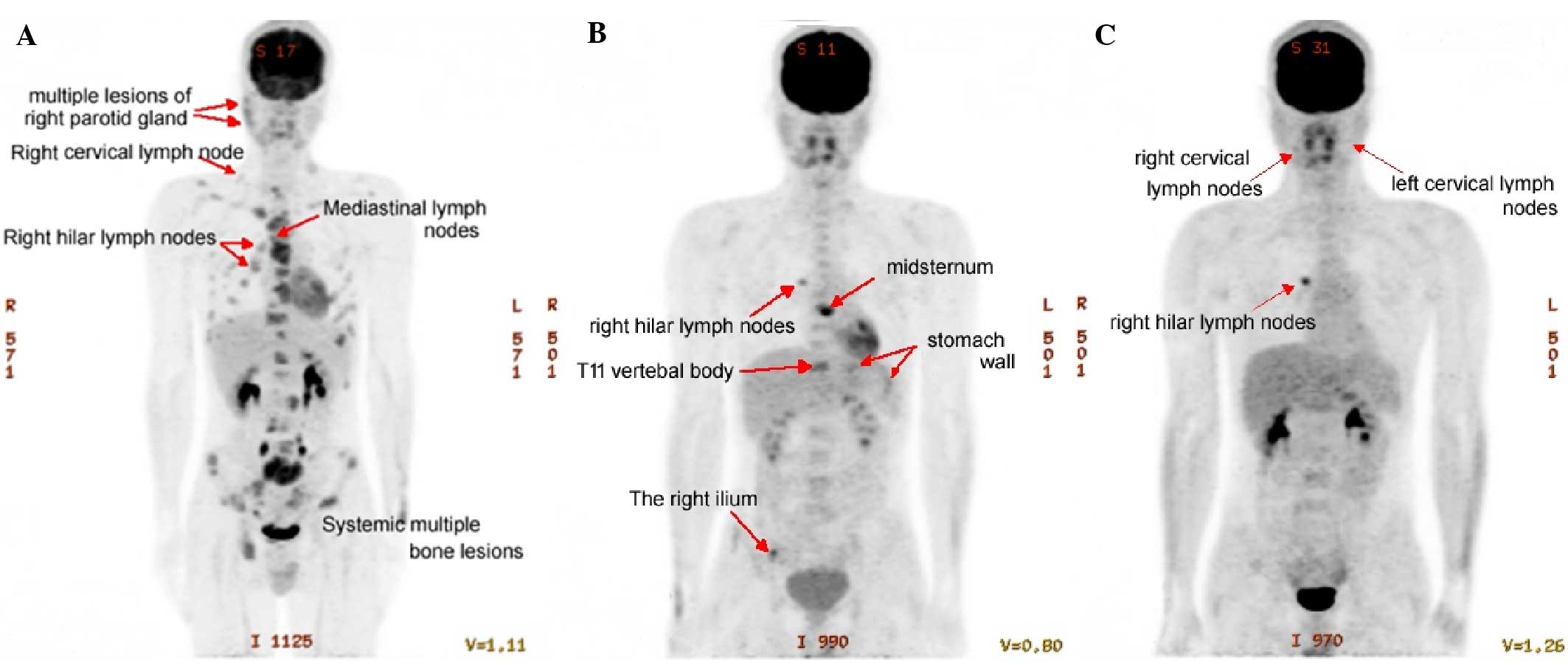 | Figure 2.PET-CT scanning image manifestations.
(A) PET-CT scan performed prior to ABVD chemotherapy. Multiple
lymph node masses were observed on the right of the neck, right
supraclavicular, right hilar and mediastinal sites, as well as
systemic multiple bone lesions. (B) PET-CT scan performed following
eight cycles of ABVD chemotherapy. (C) PET-CT scan performed
following six cycles of IGEV chemotherapy. PET-CT, positron
emission tomography-computed tomography; ABVD, doxorubicin
(Adriamycin), bleomycin, vindesine and dacarbazine; IGEV,
ifosfamide, gemcitabine, vinorelbine and prednisone. |
Discussion
The World Health Organization 2008 classification
recognizes two histological subtypes of HL, including the nodular
lymphocyte-predominant and the cHL subtypes. cHL includes the
following four entities: Nodular sclerosis, mixed cellularity,
lymphocyte-depleted and lymphocyte-rich cHL (20). The majority of HL patients present
with asymptomatic superficial lymphadenopathy. The predominant
sites of disease include the supraclavicular, mediastinal and
cervical lymph nodes, while hepatic or bone marrow involvement and
subdiaphragmatic presentation are less common (3,15). In
addition, extranodal presentations are considerably rare (1). Typically, HL presents with lymph node
involvement. Primary extranodal lymphoma is not commonly observed,
and the majority of such cases present non-HL disease (5).
In the present case, the patient initially
discovered a frontal subcutaneous nodule. This was followed by the
detection of a further nodule on the sternum, which demonstrated
similar characteristics to the former lesion. After ~1 month, the
patient noticed a mass of reasonable hardness on the left side of
the cervical spine. Following case discussion and repeated
immunohistochemical staining, the postoperative pathological
findings eventually resulted in a diagnosis of mixed cellularity
type cHL, involving the frontal subcutaneous soft tissue. Thus, the
current case cannot be considered as a primary skin lymphoma. The
most common skin involvement in lymphoma is adult T-cell lymphoma,
which is also associated with widespread lymphadenopathy, bone
marrow and blood involvement (21).
Skin involvement in HL is rare and also associated with poor
prognosis (22).
In mixed cellularity cHL, diffuse or vaguely nodular
infiltrate is observed, without band-forming sclerosis, although
fine interstitial fibrosis may be present. RS cells are more
typically detected in cHL, rather than in nodular sclerosis. Mixed
cellularity cHL presents predominately in adults and male patients,
and the stage upon diagnosis is frequently more advanced than in
nodular sclerosis or lymphocyte-predominant disease, with
involvement of lymph nodes, spleen, liver or bone marrow (1).
Primary lymphoma of the bone is rare, comprising ~5%
of all primary bone malignancies and ~5% of extranodal lymphomas
(16). Fluorodeoxyglucose-PET
scanning has emerged as an important tool in the staging of
patients with HL by significantly enhancing the staging information
obtained using other standard radiographic methods, such as X-ray
and CT (23). In the current study,
the patient was clinically diagnosed with stage IV disease, thus
the primary source of the lymphoma cannot be determined; however,
it is evident that the tumor involved the bones.
All types of cHL typically receive similar treatment
(20), based on the disease stage.
PET-CT has an important role in diagnosis and the evaluation of the
effects of chemotherapy (24). A
series of randomized trials in the past decades have established
ABVD as the gold standard on the basis of its efficacy and ability
to reduce the associated long-term toxic effects (25,26).
ABVD is also the standard chemotherapy treatment for patients with
advanced-stage disease (1). By
December 2013, the present patient had completed six cycles of ABVD
chemotherapy and two cycles of consolidation chemotherapy. The
patient exhibited a partial response to chemotherapy, with no
evident adverse effects. Following admission to the Shanghai First
People's Hospital, the patient underwent treatment with two
different chemotherapy regimes (ABVD and IGEV). At present, the
patient's general condition is stable and after accepting an
autologous bone marrow stem cell transplant in May 2014, the
patient received immunosuppressive therapy and attended outpatient
follow-ups every month. At the most recent follow-up in May 2016,
the patient was stable and did not report any discomfort. Clinical
follow-up will be continued.
In conclusion, extranodal cHL of the head and neck
is rare, while cHL with subcutaneous soft tissue involvement is
even rarer. In particular, primary HL of the skin is so rare that
several features have yet to be elucidated. Detailed physical
examination and medical history collection is necessary, and HL
should be considered in patient's with enlarged painless cervical
lymph nodes. Therefore, clinicians should pay attention to clinical
symptoms similar to bone fibroadenoma and share similar cases in
order to provide better diagnosis and treatment for cases of HL
with skin involvement.
References
|
1
|
Gobbi PG, Ferreri AJ, Ponzoni M and Levis
A: Hodgkin lymphoma. Crit Rev Oncol Hematol. 85:216–237. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cartwright R, Brincker H, Carli PM,
Clayden D, Coebergh JW, Jack A, McNally R, Morgan G, de Sanjose S,
Tumino R and Vornanen M: The rise in incidence of lymphomas in
Europe 1985–1992. Eur J Cancer. 35:627–633. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Weber AL, Rahemtullah A and Ferry JA:
Hodgkin and non-Hodgkin lymphoma of the head and neck: Clinical,
pathologic and imaging evaluation. Neuroimaging Clin N Am.
13:371–392. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dirim B, Karakas L, Oyar O, Bener S, Sener
M, Yagtu M, Erdogan N, Uluc E and Altay C: An unusual Hodgkin's
lymphoma case presenting with upper extremity multiple masses. Clin
Imaging. 36:873–876. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Travis WD, Banks PM and Reiman HM: Primary
extranodal soft tissue lymphoma of the extremities. Am J Surg
Pathol. 11:359–366. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Neskoromna-Jędrzejczak A, Tyndorf M,
Arkuszewski P and Kobos J: Head and neck lymphomas-diagnostic
difficulties. Pol Przegl Chir. 84:113–118. 2012.PubMed/NCBI
|
|
7
|
Kashyap R, Rai Mittal B, Manohar K,
Balasubramanian Harisankar CN, Bhattacharya A, Singh B, Malhotra P
and Varma S: Extranodal manifestations of lymphoma on
[18F]FDG-PET/CT: A pictorial essay. Cancer Imaging.
11:166–174. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Diehl V, Sextro M, Franklin J, Hansmann
ML, Harris N, Jaffe E, Poppema S, Harris M, Franssila K, van
Krieken J, et al: Clinical presentation, course, and prognostic
factors in lymphocyte-predominant Hodgkin's disease and
lymphocyte-rich classical Hodgkin's disease: Report from the
European Task Force on Lymphoma project on lymphocyte-predominant
Hodgkin's disease. J Clin Oncol. 17:776–783. 1999.PubMed/NCBI
|
|
9
|
Guermazi A, Brice P, de Kerviler EE, Fermé
C, Hennequin C, Meignin V and Frija J: Extranodal Hodgkin disease:
Spectrum of disease. Radiographics. 21:161–179. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ilica AT, Kocacelebi K, Savas R and Ayan
A: Imaging of extranodal lymphoma with PET/CT. Clin Nucl Med.
36:e127–e138. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Andjelic B, Antic D, Jakovic L, Todorovic
M, Bogdanovic A, Djurasinovic V, Bila J and Mihaljevic B: A single
institution experience on 314 newly diagnosed advanced Hodgkin
lymphoma patients: The role of ABVD in daily practice. Eur J
Haematol. 93:392–399. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Suárez AL, Pulitzer M, Horwitz S,
Moskowitz A, Querfeld C and Myskowski PL: Primary cutaneous B-cell
lymphomas: Part I. Clinical features, diagnosis and classification.
J Am Acad Dermatol. 69(329): e1–e13; quiz 341–342. 2013.
|
|
13
|
White RM and Patterson JW: Cutaneous
involvement in Hodgkin's disease. Cancer. 55:1136–1145. 1985.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tamaru J: Pathological diagnosis of
Hodgkin lymphoma. Nihon Rinsho. 72:450–455. 2014.(In Japanese).
PubMed/NCBI
|
|
15
|
Loo EY, Medeiros LJ, Aladily TN, Hoehn D,
Kanagal-Shamanna R, Young KH, Lin P, Bueso-Ramos CE, Manning JT Jr,
Patel K, et al: Classical Hodgkin lymphoma arising in the setting
of iatrogenic immunodeficiency: A clinicopathologic study of 10
cases. Am J Surg Pathol. 37:1290–1297. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Seymour JF: X. Extra-nodal lymphoma in
rare localisations: Bone, breast and testes. Hematol Oncol.
31(Suppl 1): S60–S63. 2013. View
Article : Google Scholar
|
|
17
|
Panico L, Tenneriello V, Ronconi F, Lepore
M, Cantore N, Dell'Angelo AC, Ferbo L and Ferrara F: High
CD20+ background cells predict a favorable outcome in
classical Hodgkin lymphoma and antagonize CD68+
macrophages. Leuk Lymphoma. 56:1636–1642. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kamper P, Bendix K, Hamilton-Dutoit S,
Honoré B, Nyengaard JR and d'Amore F: Tumor-infiltrating
macrophages correlate with adverse prognosis and Epstein-Barr virus
status in classical Hodgkin's lymphoma. Haematologica. 96:269–276.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lister TA, Crowther D, Sutcliffe SB,
Glatstein E, Canellos GP, Young RC, Rosenberg SA, Coltman CA and
Tubiana M: Report of a committee convened to discuss the evaluation
and staging of patients with Hodgkin's disease: Cotswolds meeting.
J Clin Oncol. 7:1630–1636. 1989.PubMed/NCBI
|
|
20
|
Yung L and Linch D: Hodgkin's lymphoma.
Lancet. 361:943–951. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Talpur R1, Venkatarajan S and Duvic M:
Mechlorethamine gel for the topical treatment of stage IA and IB
mycosis fungoides-type cutaneous T-cell lymphoma. Expert Rev Clin
Pharmacol. 7:591–597. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Möbs M, Cerroni L, Flaig MJ, Lenze D,
Hummel M and Assaf C: Molecular diagnostics in cutaneous lymphomas.
J Dtsch Dermatol Ges. 4:25–35. 2013. View Article : Google Scholar
|
|
23
|
Jerusalem G, Beguin Y, Fassotte MF, Najjar
F, Paulus P, Rigo P and Fillet G: Whole-body positron emission
tomography using 18F-fluorodeoxyglucose compared to
standard procedures for staging patients with Hodgkin's disease.
Haematologica. 86:266–273. 2001.PubMed/NCBI
|
|
24
|
Jhanwar YS and Straus DJ: The role of PET
in lymphoma. J Nucl Med. 47:1326–1334. 2006.PubMed/NCBI
|
|
25
|
Connors JM, Klimo P, Adams G, Burns BF,
Cooper I, Meyer RM, O'Reilly SE, Pater J, Quirt I, Sadura A, et al:
Treatment of advanced Hodgkin's disease with
chemotherapy-comparison of MOPP/ABV hybrid regimen with alternating
courses of MOPP and ABVD: A report from the National Cancer
Institute of Canada clinical trials group. J Clin Oncol.
15:1638–1645. 1997.PubMed/NCBI
|
|
26
|
Canellos GP, Anderson JR, Propert KJ,
Nissen N, Cooper MR, Henderson ES, Green MR, Gottlieb A and
Peterson BA: Chemotherapy of advanced Hodgkin's disease with MOPP,
ABVD, or MOPP alternating with ABVD. N Engl J Med. 327:1478–1484.
1992. View Article : Google Scholar : PubMed/NCBI
|