Introduction
Pupillary light reflex is an important indicator for
the determination of whether an unconscious patient's brain is
damaged (1,2). Pupillary light reflex should be
assessed to determine the therapy the patient is to receive, and to
evaluate the patient's status prior to and subsequent to treatment.
In addition, if medical disputes arise, obtaining objective data
regarding pupillary light reflex, which reflects intracranial
status that is directly connected to patient's life, is
necessary.
With the use of a pupillometer, a method by which to
measure pupillary light reflex, an accurate measurement of the size
of the pupil may be obtained. However, its use is accompanied by
constraints, such as a lack of portability and usability (3). The most common method for the
measurement of pupillary light reflex utilizes a penlight (PEN)
(4). PENs are cost-effective and
portable. However, by using a PEN, quantitative assessment is
difficult to achieve as a result of its dependence upon the
subjective judgment of a clinician and their level of
experience.
Smartphones have received attention due to their use
as an easy tool by which to produce and utilize information for the
development of applications (5), and
continuous development is possible by updating APPs. An APP was
developed in the current study by utilizing portable smartphones to
measure pupillary light reflex easily and conveniently. The
aforementioned APP was designed to obtain objective results and a
quantitative interpretation by measuring pupillary light reflex
using the camera and flash function available on smartphones. The
present study aimed to explore whether pupillary light reflex
measured by using two methods, a smartphone APP and PENs, displayed
significant differences, in addition to identifying the potential
for the use of an APP as a basis for further studies.
Materials and methods
Development of a smartphone
application
The Samsung Galaxy Series of smartphones were used
in the present study. The camera flash was utilized to provide
light stimulation to the pupil and acquire images to assess the
pupils' reaction to the stimulation. In the current study, a Galaxy
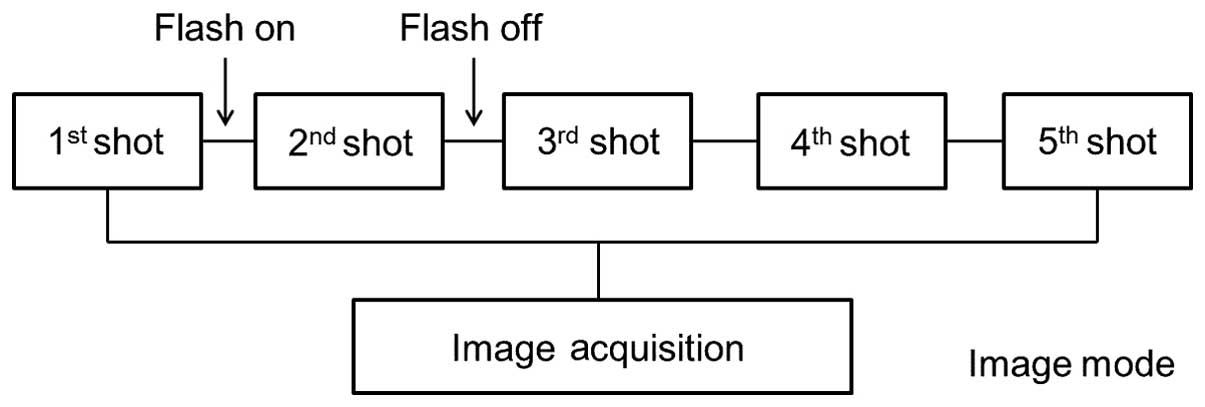
S4 (Samsung; Gyeonggi-do, South Korea) was used. As presented in
Fig. 1, the main interface opens
once the APP is run. The camera mode was activated using the touch
panel, and the ‘shot’ button was subsequently used to implement
pupillary light reflex examination. One image was captured prior to
light stimulation, another image was acquired during the light
stimulation, and several images were obtained at various time
intervals after the flash had been turned off (Fig. 2). During the development of this APP
protocol, the initial settings for acquiring images were set as 5
pictures in 6 sec, with focus set to ‘close-up’ and the optical
image stabilization function enabled. Exposure was set to the
maximum to ensure that the border between the iris and the pupil
could be clearly distinguished.
Captured images were sent to the touch panel through
a graphic processor (5.0-inch full HD super AMOLED display;
Samsung). Results were displayed on the screen. On the left hand
side, the initial image captured prior to light stimulation is
presented; whereas the four images obtained following the light
stimulation are displayed on the right hand side of the screen, to
enable comparison (Fig. 3). Images
were stored on the smartphone with the date and time so they could
be viewed again at a later time-point.
Subjects and methods
The present study was approved by the Institutional
Review Board of Chungbuk National University Hospital (approval no.
2014-10-003), and written informed consent was obtained from each
volunteer. Pupillary light reflex was measured using a PEN (3 M LED
FL-3000 Plus, 3 M Company, Maplewood MN, USA) and an APP on 30
healthy volunteers. Volunteers included 18 women and 12 men, aged
33.1±5.3 years (range, 24–49 years), of Korean descent. Assessment
was performed in a room with fluorescent light (illuminance,
200–230 lux). Volunteers sat on a chair with their upper body
tilted 30° and measurements commenced once the patient's pupils had
stabilized with their eyes closed for ~6 min. Assessors opened the
eyelids of volunteers; therefore, their eyes were opened passively.
Volunteers were instructed to look straight ahead rather than focus
on certain areas. When using the PEN, the eyelid of the volunteer
was opened with one hand and the penlight was held 10–15 cm away
from the eye with the assessor's other hand. When using the APP,
assessors held the camera lens in front of volunteers' eye at a
distance of 15 cm and the volunteers' eyelid was opened with the
remaining hand. The hand holding the camera was used to press the
‘shot’ button on the screen.
One doctor, who is familiar with measuring pupillary
light reflex, conducted pupillary light reflex examination with a
PEN, and pupil size and degree of response were recorded.
Volunteers were permitted to rest for 10 min with their eyes
closed. Following this, another tester used the APP to obtain
images. In the same manner, pupillary light reflex data for all 20
volunteers were gathered using the two respective methods. After
all data were obtained, the doctor who previously used the PEN
recorded the pupil size and degree of response using only the
images from the APP. During this period, the doctor did not receive
any data retrieved from the PEN method. Upon completion of these
processes, a comparative analysis of the data retrieved from the
PEN and the APP was performed.
Pupil size (in mm) and degree of response were
assessed on the checklist. Initial pupil size was recorded prior to
light stimulation and minimum pupil size was recorded following
light stimulation. A pupil size scale diagram was provided to
ensure that assessors were able to measure the size objectively
(4). For degree of response,
recorders selected from the following subjective indicators: Prompt
(++); sluggish (+); and no response (−). Value of κ was also
determined, and was categorized as follows: <0.20, poor;
0.21–0.40, fair; 0.41–0.60, moderate; 0.61–0.80, good; and
0.81–1.00, very good.
Statistical analysis
Statistical analyses were performed using SPSS
software, (version 12.0; SPSS, Inc., Chicago, IL, USA). Paired
t-test was used to compare initial pupil size measured by the two
methods, and to compare pupil size following light stimulation
measured by the two methods. Paired t-test and the Bland-Altman
method were used to estimate the bias and limits of agreement
between the two techniques for the estimation of pupil size.
Agreement was measured using the intraclass correlation (ICC)
coefficient. In addition, degree of response measured by the two
techniques yielded a discontinuous value, and cross tabulation was
used to assess concordance. A κ-value >0.8 was considered to
indicate good consistency. P<0.05 was considered to indicate a
statistically significant difference.
Results
Pupil size
From the subjects of the current study (n=30), 60
paired comparisons were obtained. Images of pupillary light reflex
acquired from the APP are presented in Fig. 3. Initial pupil size was 6.0±1.9 mm
when measured using a PEN, and 5.8±1.8 mm when measured by the APP.
There was no significant difference between the two methods
regarding initial pupil size. However, on average, initial pupil
size was greater when measured by the PEN, as compared with the
APP. Furthermore, pupil size following light stimulation was
2.9±1.1 mm for the PEN and 2.8±1.0 mm for the APP, with no
significant difference detected (Table
I).
 | Table I.Comparison of pupil size prior to and
following light stimulus. |
Table I.
Comparison of pupil size prior to and
following light stimulus.
| Variable | Stimulus tool | Pre-light stimulus
(mm) | Post-light stimulus
(mm) |
|---|
| Pupil size (mm) | Pen light | 6.0±1.9 | 2.9±1.1 |
|
| Smartphone
application | 5.8±1.8 | 2.8±1.0 |
| P-value |
| 0.083 | 0.293 |
Bias and limits of agreement
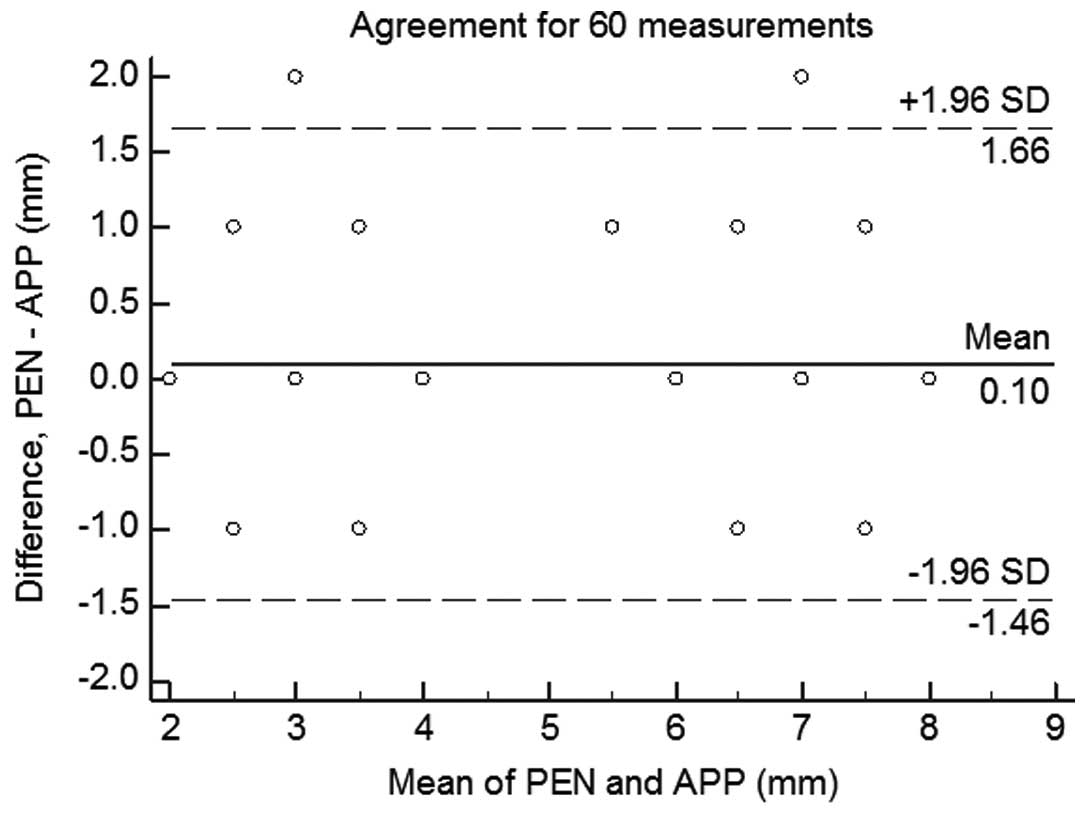
The Bland-Altman method was used to estimate the
bias and limits of agreement between the two techniques for
measuring pupil size (Fig. 4). Bias
was 0.1 mm and limits of agreement were ±1.5 mm when the APP was
compared with the PEN. ICC was 0.93 (95% confidence interval,
0.89–0.96) (Table II). Degree of
response of pupillary light reflex between the two methods
indicated a high consistency, with a κ-value of 1.00 (Table III).
 | Table II.Bland-Altman analysis and interclass
correlation coefficient. |
Table II.
Bland-Altman analysis and interclass
correlation coefficient.
| Variable | Bias (mm) | Limits of agreement
(mm) | Intraclass
correlation coefficient |
|---|
| 60 comparisons | 0.1 (P=0.33) | ±1.5 | 0.93 (95% CI
0.89–0.96) |
 | Table III.Cross-tabulation of pupillary light
reflex. |
Table III.
Cross-tabulation of pupillary light
reflex.
|
| Smartphone
application |
|
|---|
|
|
|
|
|---|
|
| Prompt | Sluggish | No response | Total |
|---|
| Pen light |
|
|
|
|
|
Prompt | 30 | 0 | 0 | 30 |
|
Sluggish | 0 | 0 | 0 | 0 |
| No
response | 0 | 0 | 0 | 0 |
| Total | 30 | 0 | 0 | 30 |
| Value of κ | 1.00 |
|
|
Discussion
Assessment of pupillary light reflex should be
performed under as follows: In a slightly dark environment, with
patients looking far away, and assessors should observe the
contraction of each pupil by flashing light onto one eye. In order
to avoid a miosis effect due to the near reflex, pupillary light
reflex should be assessed by instructing patients to fix their
focus upon a particular object some distance away (6). However, as the current experiment aimed
to compare the use of the two techniques in emergency situations
involving unconscious patients, a similar situation as observed
when examining patients in the emergency room or intensive care
unit, was simulated. This was conducted by instructing volunteers
to lay down under fluorescent light. If patients were to open and
close their eyes constantly, their pupils may have constricted in
response to the fluorescent light. Also, near reflex may occur when
patients consciously stare at the camera flash or the tip of the
PEN. To avoid these two phenomena, the patients' eyes were held
open. In the current study, no significant difference in initial
pupil size was detected between the two methods; however, on
average, initial pupil size was greater when measured by the PEN,
as compared with the APP. We hypothesize that this is because pupil
size was assessed immediately after the patients' eyes were opened
when the PEN was used. In contrast, when the APP was used, during
the time taken to open the patient's eyes, operate camera, and
capture the images, the patient's pupil may have contracted in
response to the lights. A 10-min rest was employed between the two
techniques due to the consideration of re-expansion time of the
pupil following the execution of pupillary light reflex. In a study
concerning pupil re-expansion conducted by Léon et al
(7), 14 healthy subjects were
treated with red and blue light stimulation. Upon the
administration of red light stimulation, it took 11 sec on average
for the patients' pupil to return to 90% of the initial size, and
after undergoing blue light stimulation, it took 16 sec on average.
In addition, it took 17 and 22 sec for the patients' pupil to
return to 95% of their initial size following stimulation with red
and blue light, respectively. From the results of this previous
study (7), we hypothesize that 10
min after pupillary light reflex assessments, pupil size would have
returned to the initial size. In the present study, a pupil size
scale diagram was used to improve objectivity when completing a
checklist after measuring pupil size. When using the PEN, the
checklist was primarily conducted from memory. By contrast, when
using the APP, details were assessed more objectively due to the
ability to compare images and pupil size with the scale diagram.
However, in the images obtained by a smartphone, pupil size could
be exaggerated as a result of close-up filming. To adjust for this,
pupil size was determined by comparing it with the size of the
entire eye, and the pupil size scale diagram was used for reference
alone. Due to the aforementioned reasons, we suggest that some
error in size may have arisen.
Following the administration of light stimulation,
pupil contraction occurs after a pupil incubation period due to the
slow action of the iris muscle (8).
The range of pupil incubation period is 180–500 msec, which
decreases with increasing light intensity. Furthermore, in normal
cases, the range increases by 1 msec with age; 235 msec at the age
of 20 years old and 280 msec when one is 70 years old (9,10). As
pupil incubation occurs within 300 msec, and the speed of pupil
contraction is most rapid at the beginning, the minimal pupil size
after pupillary light reflex was determined from the second image
captured after the flash is enabled. When the flash is enabled,
miosis is maintained and immediately after the light is turned off,
the pupil begins to return to the initial pupil state. Pupil
expansion speed is fastest the moment the light is removed
(8). Therefore, from the third
image, the image captured after the flash is turned off, an image
of the expanded pupil size was obtained. In this manner, as five
consecutive images were compared, the aspect of transition was
obtained in a stream of time, and pupillary light reflex response
was accurately determined.
The major limitation of the APP in the present study
was obtaining a clear image. When capturing an image using a
smartphone, the same subject may appear differently according to
light surroundings. Particularly, it is difficult to classify the
pupil from the iris as Asians typically have a dark iris color. For
accurate measurement, researchers have previously used continuous
infrared illumination and an infrared-sensitive camera (10). As this method could not be applied on
smartphones due to its complexity and the substantial costs
involved, the current study upgraded the application setting to
adjust the exposure in order to expose the boundary of the pupil as
clearly as possible. Once exposure was set to the maximum, allowing
the subjects to be clearly visualized in good light, satisfactory
images were obtained.
The current study investigated pupillary light
reflex measured by a PEN and an APP, and the results indicated that
pupil size had no significant difference and pupil degree of
response was high in consistency between the two methods. However,
there were a number of limitations to the present study. Research
was conducted on a limited patient group as the current study was
unable to recruit patients who displayed a sluggish pupil response.
In addition, the sample size was small and was not divided into
age, gender or profession. With the use of various patient groups
and upgrading the APP to ensure it was easier to use, the present
application may be useful in measuring pupillary light reflex. In
addition, if more objective data could be obtained by developing an
application that was able to automatically measure pupil size or
determine pupil contraction degree, this would have substantial
benefits. The APP could be used for tracking observations during
the patient treatment process, obtaining objective medical
evidence, constructing a report structure among medical personnel,
and aiding telemedicine systems as a form of supplementary data.
The aforementioned benefits will contribute to changes and
developments within the field.
Acknowledgements
The current study was supported by a research grant
from Chungbuk National University in 2013.
References
|
1
|
Santhanam R, Pillai SV, Kolluri SV and Rao
UM: Intensive care management of head injury patients without
routine intracranial pressure monitoring. Neurol India. 55:349–354.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Meyer S, Gibb T and Jurkovich GJ:
Evaluation and significance of the pupillary light reflex in trauma
patients. Ann Emerg Med. 22:1052–1057. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Matouskova O, Slanar O, Chytil L and
Perilk F: Pupillometry in healthy volunteers as a biomarker of
tramadol efficacy. J Clin Pharm Ther. 36:513–517. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jonathan CH: Disorders of the eye In:
Harrison's Principles of Internal Medicine. Longo DL, Fauci AS,
Kasper DL, Hauser SL, Jameson JL and Loscalzo J: I:(18th).
McGraw-Hill. New York: 224–225. 2012.
|
|
5
|
Zvornicanin E, Zvornicanin J and
Hadziefendic B: The use of smart phones in opthalmology. Acta
Inform Med. 22:206–209. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jonathan CH: Disturbances in vision and
ocular movements. Harrison's Principles of Internal Medicine. Longo
DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL and Loscalzo J:
I:(13th). McGraw-Hill. (New York). 1011994.
|
|
7
|
Léon L, Crippa SV, Borruat FX and Kawasaki
A: Differential effect of long versus short wavelenghth light
exposure on pupillary re-dilation in patients with outer retinal
disease. Clin Experiment Ophthalmol. 40:e16–e24. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ellis CJ: The pupillary light reflex in
normal subjects. Br J Ophthalmol. 65:754–759. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bergamin O and Kardon RH: Latency of the
pupil light reflex. Sample rate, stimulus intensity and variation
in normal subjects. Invest Ophthalmol Vis Sci. 44:1546–1554. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Whiting RE, Yao G, Narfström K, Pearce JW,
Coates JR, Dodam JR, Castaner LJ and Katz ML: Quantitative
assessment of the canine pupillary light reflex. Invest Ophthalmol
Vis Sci. 54:5432–5440. 2013. View Article : Google Scholar : PubMed/NCBI
|