Introduction
Chronic heart failure (CHF) is the last stage for
the majority of cardiovascular diseases, and is a leading cause of
mortality (1). Its prognosis is
worse than many malignant tumors. Excessive enhancement of
sympathetic nerve excitability is the important pathological and
physiological ground for the development and progression of CHF
(1). β-adrenergic receptor (AR) is a
major receptor of the sympathetic nerve system, and
βl-AR, β2-AR and β3-AR of β-AR
exist on myocardial cells, with βl-AR and
β2-AR being the most frequent. In HF, due to the
selective reduction of βl-AR, the physiological effects
of β2-AR were significantly improved (2).
Experimental results showed that in ischemic
myocardial cells of domestic rabbits, the enhancement of
β2-AR gene expression can improve the myocardial
contractility and cell survival rate (3). By contrast, an increasing number of
experimental studies demonstrated that immune activation and
inflammatory reaction, with the increase of inflammatory factors as
their symbols, also play an important role in the process of CHF.
Interleukin (IL)-10 is one of the most important anti-inflammatory
cytokines that has been identified, and which plays a role in
lowering the levels of pro-inflammatory factors such as tumor
necrosis factor α (TNF-α), IL-1 and IL-6, and has protective
effects on the heart (4). It has
been reported that the application of immunoregulation to increase
IL-10 can improve the symptoms of HF (5). Previous findings showed that agonist
β2-AR is capable of inhibiting the generation of
multiple pro-inflammatory factors. However, currently there are no
literature reports on the overexpression of β2-AR to
clarify whether gene transfection in HF can influence the release
of anti-inflammatory cytokine IL-10 of myocardial cells (6,7).
The present study examined the effect of
β2-adrenergic receptor (AR) overexpression on interleukin (IL)-10
content secreted by cardiomyocytes of heart failure (HF) rats. The
results showed that the concentration of IL-10 secreted by
cardiomyocytes of HF rats was increased. The overexpression of
β2-AR in the cardiomyocytes of HF rats was able to
enhance the secretion of IL-10.
Materials and methods
Experimental animals
Healthy male Sprague-Dawley (SD) rats (n=100),
weighing 180–220 g, were provided by the Experimental Animal Center
of Xuzhou Medical College (Jiangsu, China). Animal experiments were
approved by the ethics committee of Xuzhou Medical College
Experimental reagents
Recombinant adenovirus with target gene
β2-AR [adenovirus type 5 (Ad5)-ADRβ2-enhanced
green fluorescent protein (EGFP)] and recombinant adenovirus only
with EGFP (Ad5-EGFP) were structured by Vector Gene Technology Co.,
Ltd. (Beijing, China). Collagenase type II was purchased from
Worthington Biochemical Co. (Freehold, NJ, USA). M199 culture
medium, carnitine, taurine and double antibody were purchased from
Sigma (St. Louis, MO, USA), and bovine serum albumin (BSA) was
purchased from Sunshine Biotechnology Co., Ltd. (Shanghai, China).
Anti-β2-AR (H-20): sc-569 was obtained from Santa Cruz
Biotechnology, Inc. (Dallas, TX, USA), and anti-β-actin was
purchased from Cell Signaling Technology, Inc. (Danvers, MA, USA).
The NBT/BCIP kit was purchased from Promega Corp. (Madison, WI,
USA), and the rats IL-10 ELISA kit was obtained from eBioscience,
Inc. (San Diego, CA, USA).
Methods
Establishment of a rat model with CHF
Abdominal aortic banding was used for the rat model
of CHF, and abdominal aortas were isolated without banding for rats
in the sham-operated group. Color Doppler imaging (GE Healthcare,
Piscataway, NJ, USA; Vivid7, provided by the Xuzhou Central
Hospital) and 10S probe (probe frequency: 11.0 MHz) were used to
detect cardiac structure and function 12 weeks after the operation.
Left ventricular end diastolic diameter (LVEDD), left ventricular
end systolic diameter (LVESD), LVE shortening fraction (FS) and
ejection fraction (EF) were measured, respectively. Five cardiac
cycles were selected to calculate the mean value of each ultrasound
measurement value. The screening criteria included: rats with poor
appetite, no gain in weight, low spirit, low activities, fluffy and
lackluster coat of fur, and tachypnea, and cardiac color Doppler
ultrasound index EF <60%. Rats conforming to the above criteria
were included into the HF group. Rats in the HF group were randomly
divided into the HF control group (HF), EGFP-transfected group
(HF+EGFP) and β2-AR-EGFP-transfected group
(HF+β2). Rats in the sham-operated group were also
randomly divided into the control group (sham), EGFP-transfected
group (sham+EGFP) and β2-AR-EGFP-transfected group
(sham+β2).
Isolation and culture of myocardial cells of
rats
Collagenase type II dissociation method was used for
the isolation of myocardial cells of rats. Abdomens of rats were
injected with heparin sodium (1,500 U/150 g) 30 min prior to
anesthesia. Thoracotomy was immediately employed to obtain hearts
after anesthesia, the hearts were placed in cold 1 mmol/l
calciferous KH solution to cease beating, and were immediately hung
on the Langendorff perfusion apparatus (ADInstrument, Colorado
Springs, CO, USA). After 5 min retrograde perfusion through aorta
with 1 mmol/l calciferous KH solution, the calciferous KH solution
was replaced by low-calcium KH solution for another 5 min
perfusion, and then converting enzyme solution circulatory
perfusion was used for 10–15 min. The temperature of the whole
perfusion process was kept at 37°C, and the flow rate was kept at
8–10 ml/min. Once the textures of hearts softened, the myocardium
was dissected and cultured in the culture dish. Myocardium was cut
into pieces, oscillated and incubated in enzyme solution for 5 min.
A nylon net (300 µm) was used for filtration, the filter solution
was centrifuged at 16 × g (400 rpm) for 1 min, the supernatant was
discarded and naturally settled in 1 mmol/l calciferous KH solution
after re-suspension and repeated three times. The visual counting
method was utilized to calculate the density of myocardial cells,
and cells were cultured using M199 culture solution with 0.2% BSA
in the living cell density of 1×105/ml.
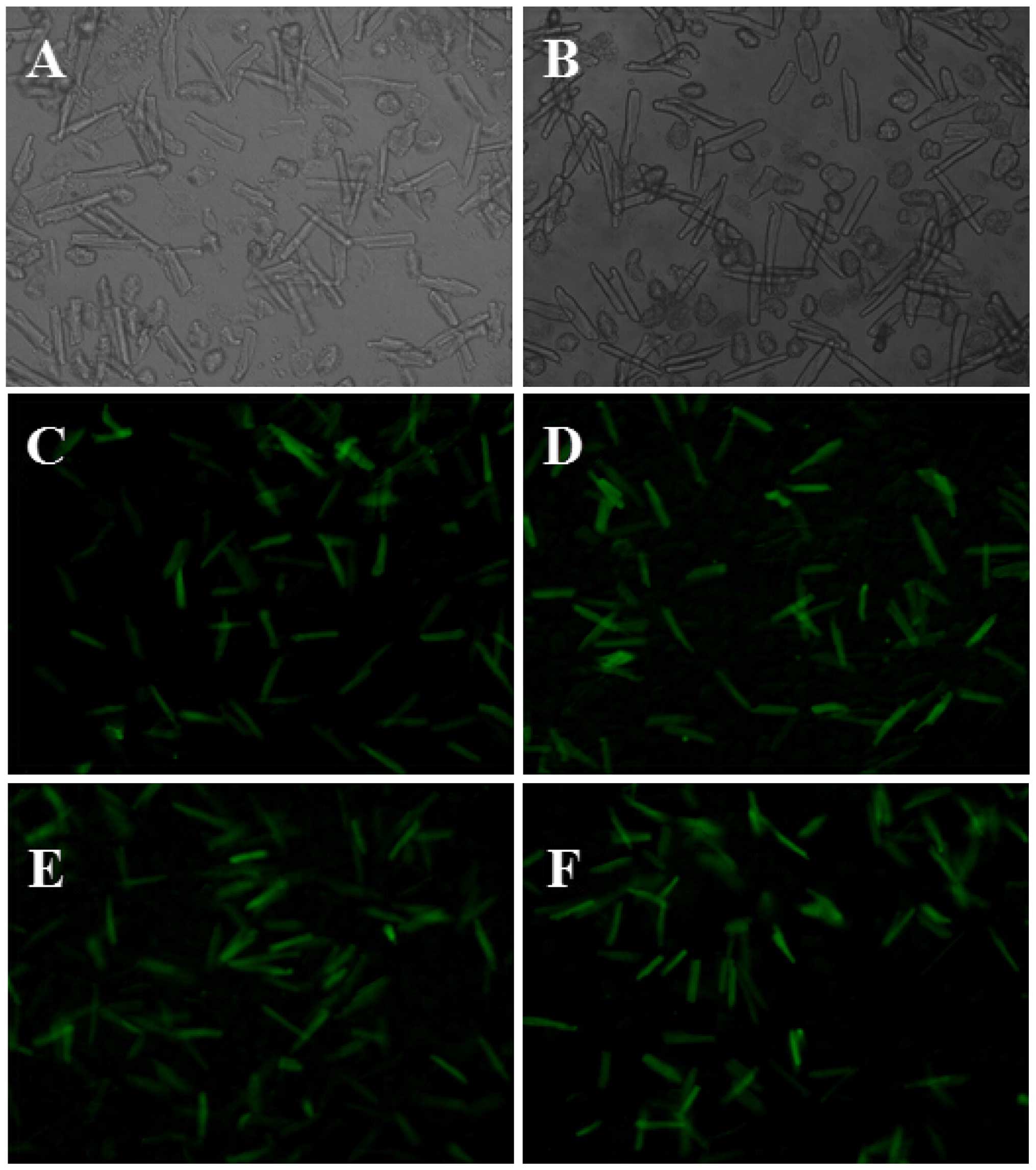
Gene transfection of myocardial cells of
rats
Recombinant adenovirus with β2-AR or EGFP
genes were used to transfect myocardial cells of rats, at a
multiplicity of infection of 100. At 48 h after transfection, the
myocardial cells were removed from the incubator, observed and
photographed under a fluorescence microscope (AF6000, Leica
(Wetzlar, Germany). Five views were randomly selected and
transfection efficiencies, as the number/total number of stab cells
with the expression of green fluorescence under the same view, were
calculated, respectively.
Detection of β2-AR protein expression
by western blotting
At 48 h after transfection, adenovirus-transfected
myocardial cells were collected, cleaned in culture medium twice,
centrifuged 16 × g (400 rpm) for 1 min and the supernatant was
discarded, and homogenate with protease inhibitor cocktail was
added. The cells were broken by ultrasound, after measuring its
protein concentration by the Lowry method, 4 × Laemmli
SDS-polyacrylamide gel (PAGE) loading buffer of the same volume was
added to the sample with the same protein content, and was placed
in a boiling water bath for 5 min. Denatured protein sample (100
µg) of the same volume was loaded on SDS-PAGE for ionophoretic
separation. Subsequently, separated proteins were transferred to a
nitrocellulose (NC) membrane using the semi-dry transferring
method. The NC membrane was incubated for 3 h at room temperature
with primary mouse monoclonal anti-β2 AR antibody at a dilution of
1:1000 (Sigma-Aldrich, St. Louis, MO, USA, catalog no.: SAB4504272)
and then transferred to 4°C for overnight incubation. TBST was used
for washing the membrane three times, followed by incubation with
polyclonal goat-anti-mouse secondary antibody (Sigma-Aldrich,
catalog no.: A6715) for 2 h at room temperature. TBST buffer was
used to wash the membrane for 5 min, three times. For the
chemiluminescent reaction, the NBT/BCIP kit was used for coloration
in newly prepared AP coloring solution. Images were captured and
data analysed using software such as Image J, Sigmastat and
Sigmaplot (7). Optical density of
the control group was set at 1, and other groups were represented
by its multiple.
Detection of IL-10 content by ELISA
After 48 h of incubation, myocardial cells in each
group were centrifuged at 389 × g for 20 min. The culture
supernatants were collected, and preserved at −80°C. ELISA was used
to detect the content of IL-10 released by myocardial cells, and
the procedures were in accordance with the instructions of the kit
(eBioscience, San Diego, CA, USA).
Statistical analysis
SPSS 16.0 (SPSS, Inc., Chicago, IL, USA) was used
for the statistical analysis. Measurement data were presented as
mean ± standard deviation. Double independent sample t-test was
employed for the treatment of results of the ultrasound cardiac
function measuring of rats. After homogeneity test of variances,
western blot data and ELISA detection results were statistically
analyzed by one-way analysis of variance. As for variance
comparison among groups, the LSD test was used for homogeneity,
while Dunnett's T3 test was used for heterogeneity. P<0.05 was
considered to indicate a statistically significant difference.
Results
Identification of the model of rats
with CHF
Partial abdominal aortic constriction was employed
for 70 male SD rats to establish the HF model, and abdominal aortas
were isolated without banding for 30 rats in the sham-operated
group. Post-operation, 18 rats in the model group died, and the
mortality rate was 26%; and 1 rat in the sham-operated group died,
and the mortality rate was 3%. The rats in the HF model group had
symptoms of loss of appetite and weight, low spirit, low activity,
fluffy and lackluster coat of hair, tachypnea after surgery, and
the 27 rats conforming to the criteria of HF in color Doppler
ultrasonography after 12 weeks, were randomly divided into groups.
No symptoms were identified in the sham-operated group, and 27 of
29 rats were randomly selected for ultrasonography, and randomly
divided into groups. The results of color Doppler ultrasonography
after 12 weeks showed that compared with the sham-operated group,
LVEDD and LVESD of rats in the HF group significantly increased
(P<0.05), while FS and EF significantly decreased (P<0.05;
Table I).
 | Table I.Comparison of cardiac ultrasound
indexes between heart failure and sham-operated rats, 12 weeks
after operation. |
Table I.
Comparison of cardiac ultrasound
indexes between heart failure and sham-operated rats, 12 weeks
after operation.
| Groups | Cases | LVEDD, mm | LVESD, mm | FS, % | EF, % |
|---|
| Sham | 27 | 5.93±0.68 | 3.25±0.72 | 46.22±6.28 | 81.59±5.20 |
| HF | 27 |
8.78±0.80a |
6.15±0.95a |
26.30±3.17a |
55.96±5.05a |
Results of myocardial cell survival
rate
In total, 27 rats conformed to the criteria of HF.
Following myocardial cell isolation, the rats were randomly divided
into the HF control group (HF), EGFP-transfected group (HF+EGFP)
and β2-AR-EGFP-transfected group (HF+β2),
with 9 cases in each group. Similarly, after myocardial cell
isolation, 27 rats in the sham-operated group were randomly divided
into the control group (sham), EGFP-transfected group (sham+EGFP)
and β2-AR-EGFP-transfected group (sham+β2), with 9 cases
in each group. In addition, 9 normal rats were selected for
myocardial cell isolation as the normal control group
(control).
In comparison to the control group, after 48 h of
incubation the myocardial cell survival rates in the HF, HF+EGFP
and HF+β2 groups significantly decreased (P<0.05).
Compared with the sham group, after 48 h the myocardial cell
survival rates in the sham+EGFP and sham+β2 groups did
not show any significance. Compared with the HF group, the 48-h
myocardial cell survival rates in the HF+EGFP and HF+β2
groups had no significant difference (Table II).
 | Table II.Comparison of 48 h myocardial cell
survival rates of rats in each group. |
Table II.
Comparison of 48 h myocardial cell
survival rates of rats in each group.
| Groups | Cases | 48-h survival
rates, % |
|---|
| Control | 9 | 63.93±4.82 |
| Sham | 9 | 63.45±5.76 |
| Sham+EGFP | 9 | 62.15±4.59 |
|
Sham+β2 | 9 | 62.68±7.55 |
| HF | 9 |
54.48±7.70a |
| HF+EGFP | 9 |
52.33±7.22a |
|
HF+β2 | 9 |
52.79±7.90a |
Myocardial cells transfected with
adenovirus with β2-AR or EGFP genes
At 48 h after myocardial cells of rats were
transfected with adenovirus with β2-AR or EGFP genes,
green fluorescence was observed under an inverted fluorescence
microscope, and the transfection efficiency was calculated as 80%
(Fig. 1).
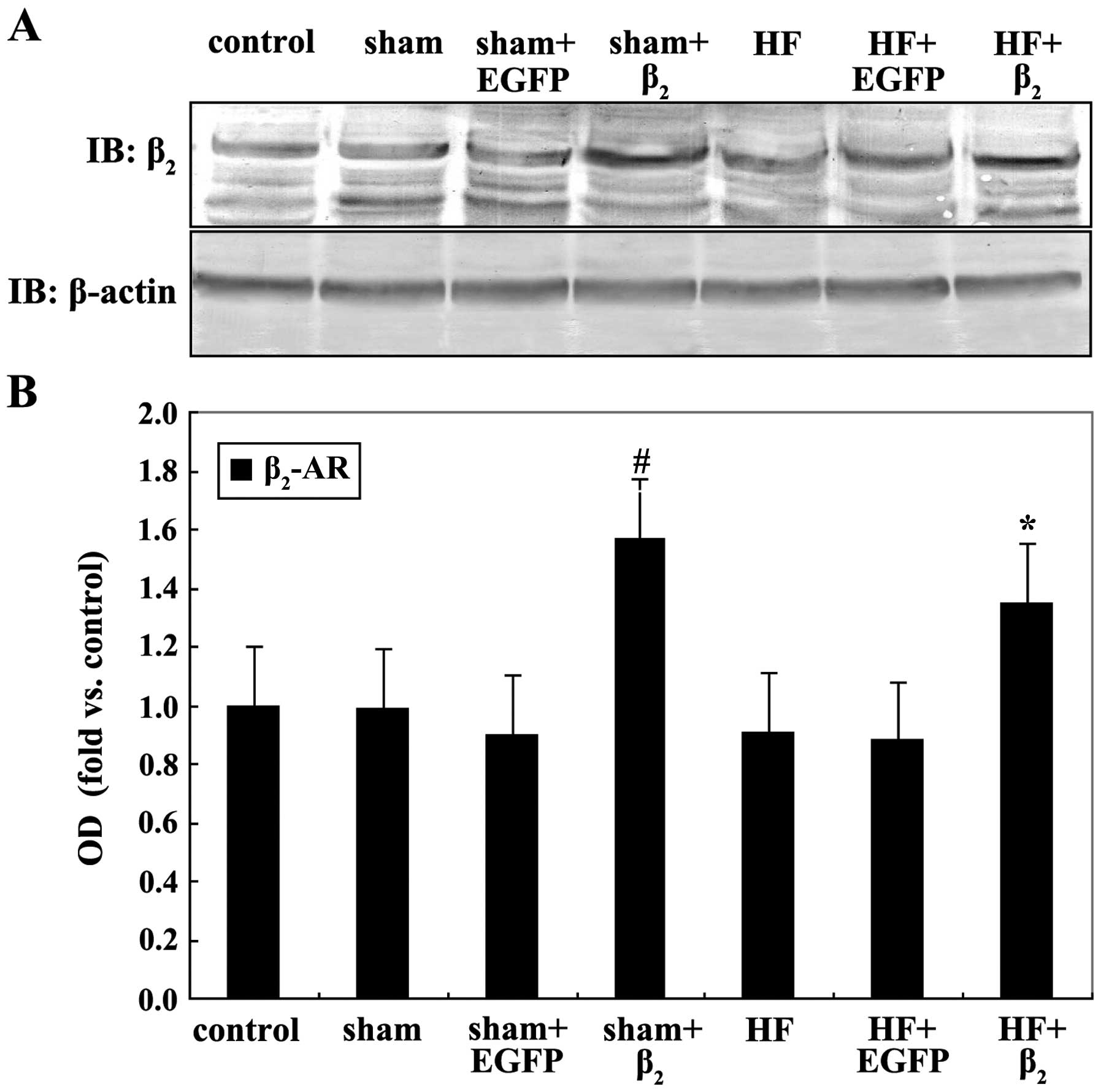
β2-AR expression of
myocardial cells of rats transfected with adenovirus with
β2-AR or EGFP genes
Compared with the control or sham group,
β2-AR expression in the HF group had no significant
difference. The content of β2-AR of myocardial cells in
the HF+β2 group was significantly higher than that of
the HF+EGFP and HF groups (P<0.05), and the β2-AR
expression content of the sham+β2 group was higher than
that of the sham+EGFP and sham groups (P<0.05; Fig. 2).
Results of myocardial cell IL-10
level
Compared with the control and sham group, IL-10
content in the HF group was slightly higher (P<0.05). The IL-10
content in the HF+β2 group was significantly higher than
that of the HF+EGFP and HF groups (in both conditions, P<0.05),
while the differences between IL-10 content in the
sham+β2 group and that of the sham+EGFP and sham groups
are of no statistical significance (in either condition, P>0.05;
Table III).
 | Table III.Comparison of IL-10 content in each
group released by myocardial cells of rats. |
Table III.
Comparison of IL-10 content in each
group released by myocardial cells of rats.
| Groups | Cases | IL-10, pg/ml |
|---|
| Control | 9 | 18.91±5.87 |
| Sham | 9 | 21.60±5.89 |
| Sham+EGFP | 9 | 21.05±3.76 |
|
Sham+β2 | 9 | 22.51±5.67 |
| HF | 9 |
39.84±5.96a |
| HF+EGFP | 9 |
42.23±4.74a |
|
HF+β2 | 9 |
63.11±5.62a,b |
Discussion
Heart failure (HF) is a complex clinical syndrome,
its basic process is myocardial remodeling, and its performance
includes hypertrophy and apoptosis of myocardial cells and fibrosis
of mesenchyme (1). Recent findings
have shown that inflammatory cytokines participate in the
development and progression of HF. According to its biological
effects, multiple cytokines that are involved in CHF can be
generally divided into (8,9): The pro-inflammatory cytokines,
including IL-1, IL-6, TNF-α and CRP, the most reported in
literature (10–12); and the anti-inflammatory cytokines,
such as IL-10, IL-4 and transforming growth factor-β (8–12).
IL-10 is one of the most important anti-inflammatory
cytokines which is mainly generated by B cells,
monocytes/macrophages and Th2 cells (13). In addition, other types of cells
including CD8+ cells, keratinocytes, mastocytes and
myocardial cells can also generate IL-10 (14). The main biological activity of IL-10
involves immunosuppressive effects, which can inhibit multiple
cytokines including interferon-γ, IL-2, IL-3, IL-1β, IL-6, and
TNF-α. IL-10 has been identified to have immunomodulatory effects,
which can facilitate cellular immunity, stimulate B cells to
activate hyperplasia and release antibodies, and facilitate the
proliferation and maturity of T cells (8,15). Based
on the biological characteristics of IL-10, it is believed that
IL-10 is a protective cytokine in CHF (16). Verma et al (17) reported that isoproterenol (ISO) was
utilized to induce the myocardial hypertrophy HF model of wild-type
and IL-10 gene knockout mice, and it was identified that the
myocardial hypertrophic remodeling and cardiac function conditions
of IL-10 gene knockout mice are more deteriorated than controls. In
spite of the introduction of IL-10 into IL-10 gene knockout mice
through genetic recombination, the results have shown that IL-10
inhibits or even reverses ISO-induced myocardial hypertrophic
remodeling and fibrosis, as well as improve cardiac function
(17). The results suggest that
IL-10 can inhibit myocardial remodeling and improve cardiac
function, and has protective effects on myocardium. However,
results of IL-10 level changes in CHF, are inconsistent. Changes in
the IL-10 level may increase significantly (18), increase insignificantly, while some
even slightly decrease (19). The
results of the present study showed that the IL-10 level of HF rats
was higher than the normal rats, and the probable causes were: i)
In HF, due to the increase and stimulation of multiple
pro-inflammatory cytokines, IL-10 increase is compensatory; and ii)
in HF, the level of TNF-α increases, which stimulates the
expression of IL-10 in the transcriptional level, and makes IL-10
composited and released by myocardial cell increase.
The decrease of number and function of selective
β1-AR is accompanied by HF, and an interesting
‘substitution effect’ phenomenon was generated between
β1-AR and β2-AR (20). Especially after the overexpression of
β2-AR, under the background of β1-AR loses
its power, the advantages of β2-AR gradually become
evident and it overtakes. Dorn et al (21) reported that the overexpression of
β2-AR in rats can improve cardiac contractile and
relaxant function and reverse myocardial hypertrophy. The results
of early laboratory investigations of the present study also show
that after the β2-AR overexpression of myocardial cells
of rats with HF, basic contractile function of myocardiac cells can
be improved (22). Previous findings
have shown that β2-AR mediates effects such as cardiac
contractile and relaxant function, and leads to many changes of
numerous inflammatory cytokines after the excitement of
β2-AR. Using lipopolysaccharide to induce inflammatory
reactions and excite β2-AR by specific β2-AR
agonist, it was identified that β2-AR can inhibit the
generation of IL-18 and IL-12 (23).
There are results of animal experiments showing that the changes of
β2-AR expression can adjust inflammatory reactions of
cytokines such as IL-12 (24).
HF itself is an inflammatory reaction, thus in this
study, we assessed whether the increase of β2-AR
expression of myocardial cells of HF have the effects of adjusting
inflammatory reactions by influencing the release of IL-10. We
found that in comparison to normal rats, β2-AR
expression on the surface of myocardial cells of rats with HF has
no significant changes, which concurs with earlier reports
(25). We transferred
β2-AR gene into the myocardial cells of rats with HF by
the carrier of recombinant adenovirus to overexpress
β2-AR, thus, the impact of β2-AR on
myocardial cells anti-inflammatory cytokine IL-10 can be studied,
and the relationship between β2-AR and HF inflammatory
reaction can be preliminarily studied. We identified that IL-10
level of myocardial cells of rats with HF was slightly higher than
that of normal rats. Through gene transfection technology, we
enhanced the myocardial cell surface expression of
β2-AR, and IL-10 level of myocardial cells of the
HF-transfected β2-AR group further increased in
comparison with the HF control group, and IL-10 level of myocardial
cells of the sham-operated-transfected β2-AR group has
no significant decrease compared with the sham-operated control
group. This result shows that the increase of β2-AR
expression can increase the IL-10 level of myocardial cells of rats
with HF, while it has no significant impact on IL-10 level of
myocardial cells of normal rats. It suggests that introducing
β2-AR into myocardial cells by gene transfection can
also be achieved by increasing the IL-10 level of myocardial cells
anti-inflammatory cytokine, which can play certain roles of
anti-inflammatory immunoregulation, and can become a new
therapeutic target for the treatment of HF.
The present study excluded the whole body influences
including nerve and body fluid, and the impact of β2-AR
overexpression on the IL-10 release of myocardial cells of rats
with HF was observed at the in vitro cellular level.
However, understanding the relationship between them with the
combination of the impact of in vivo level β2-AR
on cytokines would be beneficial. Currently, the mechanism of the
impact of β2-AR overexpression on HF myocardial cell
IL-10 release and molecular signaling pathways remain to be
determined and require further investigation. In addition, this
study selected pro-inflammatory factor IL-10 as the object of
investigation in order to understand its relationship with
β2-AR. Therefore, future studies should select other
inflammatory factors as the focus of study to more comprehensively
understand the relationship between β2-AR and
inflammatory reaction in HF.
Acknowledgements
The present study was partly financed by the Jiangsu
Provincial Special Program of Medical Science (no. BL2012019).
References
|
1
|
Khatibzadeh S, Farzadfar F, Oliver J,
Ezzati M and Moran A: Worldwide risk factors for heart failure: A
systematic review and pooled analysis. Int J Cardiol.
168:1186–1194. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nikolaev VO, Moshkov A, Lyon AR, Miragoli
M, Novak P, Paur H, Lohse MJ, Korchev YE, Harding SE and Gorelik J:
Beta2-adrenergic receptor redistribution in heart failure changes
cAMP compartmentation. Science. 327:1653–1657. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dong H, Chen Q, Sun S, Yu H and Zhang Z:
Overexpression of beta(2)AR improves contractile function and
cellular survival in rabbit cardiomyocytes under chronic hypoxia.
Biochem Biophys Res Commun. 398:383–388. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bolger AP, Sharma R, von Haehling S,
Doehner W, Oliver B, Rauchhaus M, Coats AJ, Adcock IM and Anker SD:
Effect of interleukin-10 on the production of tumor necrosis
factor-alpha by peripheral blood mononuclear cells from patients
with chronic heart failure. Am J Cardiol. 90:384–389. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gullestad L, Aass H, Fjeld JG, Wikeby L,
Andreassen AK, Ihlen H, Simonsen S, Kjekshus J, Nitter-Hauge S,
Ueland T, et al: Immunomodulating therapy with intravenous
immunoglobulin in patients with chronic heart failure. Circulation.
103:220–225. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bosmann M, Grailer JJ, Zhu K, Matthay MA,
Sarma JV, Zetoune FS and Ward PA: Anti-inflammatory effects of β2
adrenergic receptor agonists in experimental acute lung injury.
FASEB J. 26:2137–2144. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fragaki K, Kileztky C, Trentesaux C, Zahm
JM, Bajolet O, Johnson M and Puchelle E: Downregulation by a
long-acting beta2-adrenergic receptor agonist and corticosteroid of
Staphylococcus aureus-induced airway epithelial inflammatory
mediator production. Am J Physiol Lung Cell Mol Physiol.
291:L11–L18. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Padda RS, Gkouvatsos K, Guido M, Mui J,
Vali H and Pantopoulos K: A high-fat diet modulates iron metabolism
but does not promote liver fibrosis in hemochromatotic Hjv¯/¯ mice.
Am J Physiol Gastrointest Liver Physiol. 308:G251–G261. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Saghazadeh A, Gharedaghi M, Meysamie A,
Bauer S and Rezaei N: Proinflammatory and anti-inflammatory
cytokines in febrile seizures and epilepsy: Systematic review and
meta-analysis. Rev Neurosci. 25:281–305. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hirota H, Izumi M, Hamaguchi T, Sugiyama
S, Murakami E, Kunisada K, Fujio Y, Oshima Y, Nakaoka Y and
Yamauchi-Takihara K: Circulating interleukin-6 family cytokines and
their receptors in patients with congestive heart failure. Heart
Vessels. 19:237–241. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kurdi M and Booz GW: Can the protective
actions of JAK-STAT in the heart be exploited therapeutically?
Parsing the regulation of interleukin-6-type cytokine signaling. J
Cardiovasc Pharmacol. 50:126–141. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Padda RS, Shi Y, Lo CS, Zhang SL and Chan
JS: Angiotensin-(1-7): A novel peptide to treat hypertension and
nephropathy in diabetes? J Diabetes Metab. 6:1–6. 2015.
|
|
13
|
Fillatreau S, Sweenie CH, McGeachy MJ,
Gray D and Anderton SM: B cells regulate autoimmunity by provision
of IL-10. Nat Immunol. 3:944–950. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yoshida T, Hanawa H, Toba K, Watanabe H,
Watanabe R, Yoshida K, Abe S, Kato K, Kodama M and Aizawa Y:
Expression of immunological molecules by cardiomyocytes and
inflammatory and interstitial cells in rat autoimmune myocarditis.
Cardiovasc Res. 68:278–288. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Asadullah K, Sterry W and Volk HD:
Interleukin-10 therapy - review of a new approach. Pharmacol Rev.
55:241–269. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Domínguez Rodríguez A, Abreu González P,
García González MJ and Ferrer Hita J: Association between serum
interleukin 10 level and development of heart failure in acute
myocardial infarction patients treated by primary angioplasty. Rev
Esp Cardiol. 58:626–630. 2005.(In Spanish). PubMed/NCBI
|
|
17
|
Verma SK, Krishnamurthy P, Barefield D,
Singh N, Gupta R, Lambers E, Thal M, Mackie A, Hoxha E, Ramirez V,
et al: Interleukin-10 treatment attenuates pressure
overload-induced hypertrophic remodeling and improves heart
function via signal transducers and activators of transcription
3-dependent inhibition of nuclear factor-κB. Circulation.
126:418–429. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wykretowicz A, Furmaniuk J, Smielecki J,
Deskur-Smielecka E, Szczepanik A, Banaszak A and Wysocki H: The
oxygen stress index and levels of circulating interleukin-10 and
interleukin-6 in patients with chronic heart failure. Int J
Cardiol. 94:283–287. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Stumpf C, Lehner C, Yilmaz A, Daniel WG
and Garlichs CD: Decrease of serum levels of the anti-inflammatory
cytokine interleukin-10 in patients with advanced chronic heart
failure. Clin Sci (Lond). 105:45–50. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Lamba S and Abraham WT: Alterations in
adrenergic receptor signaling in heart failure. Heart Fail Rev.
5:7–16. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Dorn GW II, Tepe NM, Lorenz JN, Koch WJ
and Liggett SB: Low- and high-level transgenic expression of
beta2-adrenergic receptors differentially affect cardiac
hypertrophy and function in Galphaq-overexpressing mice. Proc Natl
Acad Sci USA. 96:6400–6405. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gong H, Lv Q and Lei W: The relationship
and mechanism between the expression of myocardial cells β2-AR of
rats with heart failure and cardiac function changes. Prog Mod
Biomed. 9:1024–1027. 2009.
|
|
23
|
Mizuno K, Takahashi HK, Iwagaki H, Katsuno
G, Kamurul HA, Ohtani S, Mori S, Yoshino T, Nishibori M and Tanaka
N: Beta2-adrenergic receptor stimulation inhibits LPS-induced IL-18
and IL-12 production in monocytes. Immunol Lett. 101:168–172. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Itoh CE, Kizaki T, Hitomi Y, Hanawa T,
Kamiya S, Ookawara T, Suzuki K, Izawa T, Saitoh D, Haga S, et al:
Down-regulation of beta2-adrenergic receptor expression by exercise
training increases IL-12 production by macrophages following LPS
stimulation. Biochem Biophys Res Commun. 322:979–984. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Shizukuda Y and Buttrick PM: Subtype
specific roles of beta-adrenergic receptors in apoptosis of adult
rat ventricular myocytes. J Mol Cell Cardiol. 34:823–831. 2002.
View Article : Google Scholar : PubMed/NCBI
|