Introduction
Paraneoplastic pemphigus, which was initially
described by Anhalt et al (1), is characterized by non-specific
pemphigus accompanying mucosal skin lesions showing erosion and
blisters, which occur as a result of the production of
autoantibodies against internal tumors. Skin lesions associated
with autoantibodies may not only be pemphigus lesions, but also
erythema multiforme-like lesions, graft-versus-host disease-like
lesions and lichen planus lesions (1,2). These
diseases may also cause mortality due to the infiltration of
autoantibodies into other organs, thus leading to the term
paraneoplastic autoimmune multiorgan syndrome (PAMS) (2).
Lymphoid hyperplasia is the rapid growth and
proliferation of normal cells that resemble lymph tissue, and the
majority of lymphoid hyperplasia cells are T lymphocytes (2,3).
Neoplasms associated with lymphoid hyperplasia include Castleman's
disease, non-Hodgkin's lymphoma and thymoma, and these tumors have
been frequently associated with PAMS (2). Conversely, sarcoma and malignant
melanoma have rarely been associated with PAMS (3). The most common symptoms of PAMS are
persistent oral lesions that are typically resistant to
pharmacological treatment (4–7).
Brachytherapy can be attempted when considering the accessibility
of the disease lesion, to minimize the side effects to the adjacent
organ and to increase the therapeutic radiation dose (8).
The present study is, to the best of our knowledge,
the first to report the results of intraluminal brachytherapy
application for the treatment of a persistent and
pharmacological-resistant oral erosive ulcer in a 42-year-old
female patient with giant lymph node hyperplasia (Castleman's
disease) and erosive skin lesions in the vaginal mucosa and trunk
region.
Case report
A 42-year-old female patient visited Chonbuk
National University Hospital (Jeonju, Republic of Korea) with an
8-month history of erosive skin lesions occurring in the trunk
region, oral mucosa and vaginal mucosa. The patient's medical
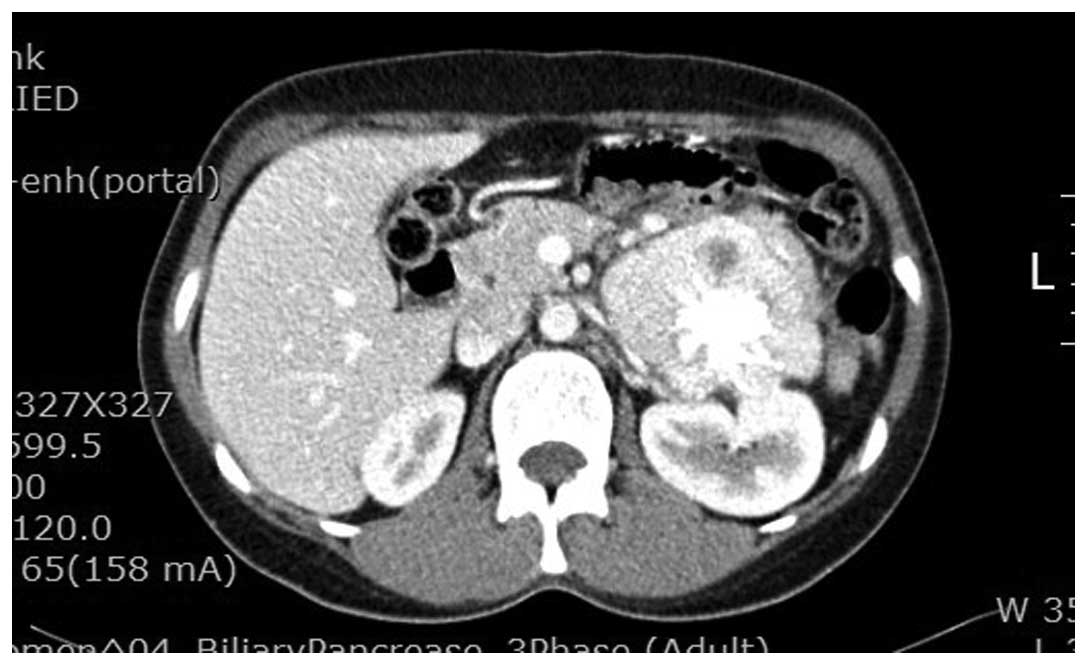
history and family history were normal. An abdominal computed
tomography (CT) scan (date, 18/6/2008) was performed following the
detection of elevated CA125 (86.4 U/ml; normal, 0–37 U/ml) and
CA19-9 (185.46 U/ml; normal, <37 U/ml) levels in a blood
examination. A retroperitoneal mass identified in the abdominal CT
scan was removed (date, 25/6/2008) and the patient was diagnosed
with Castleman's disease according to this biopsy (date, 30/6/2008)
(Fig. 1). The biopsy was a large
(12×6.5×6.8 cm) mass with multicentric, hyaline vasular lymph node
hyperplasia. The study was approved by the Institutional Review
Board of Chonbuk National University Hospital and was conducted
according to the Declaration of Helsinki regarding biomedical
research involving human subjects. A detailed explanation of the
study was provided to the patient, and written informed consent was
obtained from the patient.
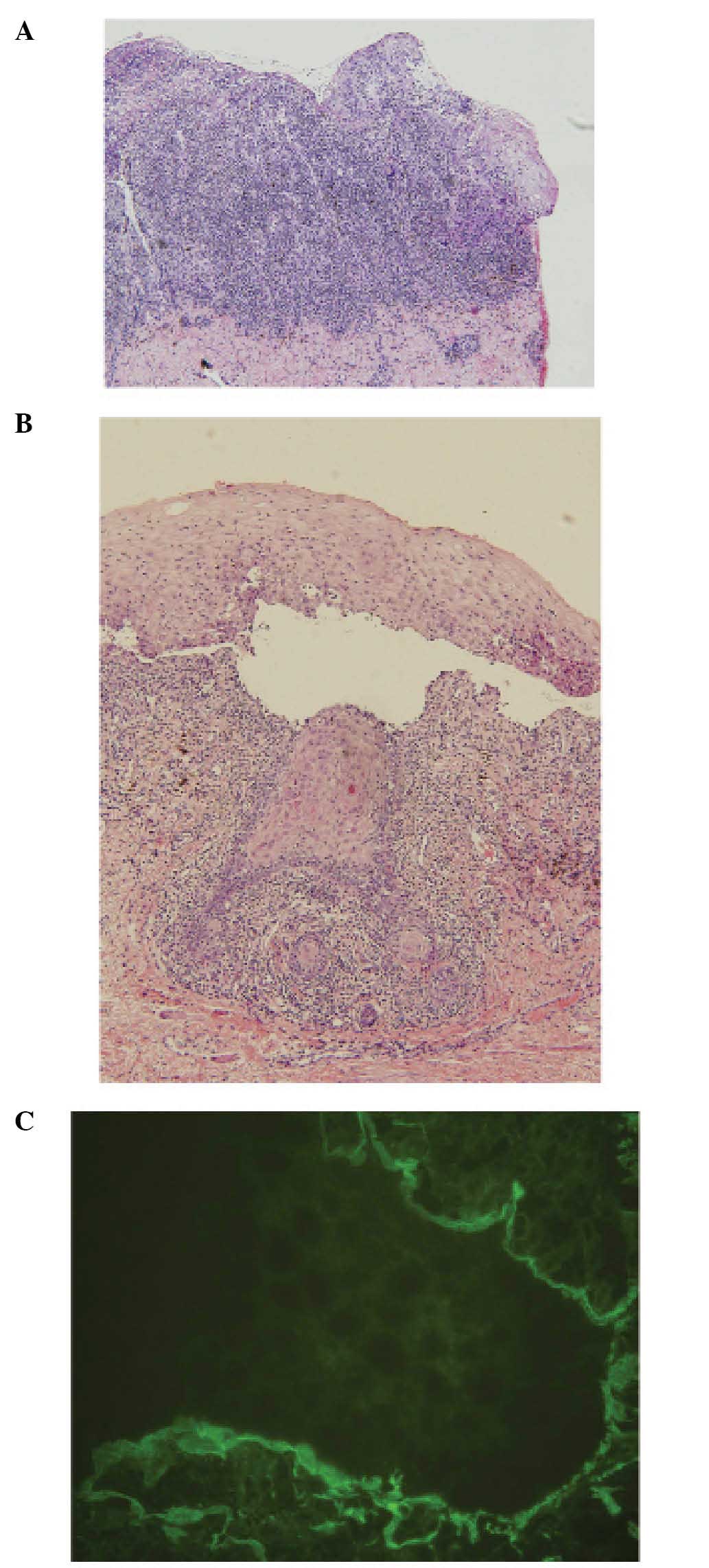
Biopsies of the skin lesions were performed, and
hematoxylin and eosin-stained pathology sections were classified
according to their histological features, analyzed under a
microscope (BX50; Olympus Corporation, Tokyo, Japan). The trunk
lesions showed non-caseating granulomous features and positive
lichen planus under low magnification, and chronic inflammatory
cell infiltration, numerous blood vessels, lymphohistiocytic
granuloma infiltrate and multicentric giant cells under high
magnification (Fig. 2A). In the skin
lesions from the vaginal mucosa, epidermal labia majora-acanthosis,
separation of the dermoepidermal junction, destruction of the basal
layer and deposition of lymphoid cells and neutrophils in the
dermis were observed under low magnification, and dyskeratosis,
exocytosis, acantholysis and squamous metaplasia of the epidermis
and keratinocytes were observed under high magnification (Fig. 2B). The tongue was ulcerated and
lacked the epithelium, and dense lymphoid cell infiltration into
the tongue was observed under low magnification. In addition,
acanthosis and dense lymphoid cell infiltration were observed under
high magnification. Immunofluorescence (date, 7/8/2008) revealed
fibrinogen deposition along the basement membrane (Fig. 2C). For the immunofluorescence assay,
the tissue specimen was incubated for 1 h at room temperature using
a human IgG fluorescence-labeled antibody (cat. no. 23310; Pierce
Biotechnology; Thermo Fisher Scientific, Inc., Waltham, MA, USA;
dilution, 1:200).
The patient was diagnosed with PAMS (7/8/2008)
following analyses of the tissue obtained from the retroperitoneal
mass and skin lesions. Following the diagnosis, retroperitoneal
mass resection was performed to alleviate pain caused by the mass
and pharmacological treatment was performed for skin and mucosal
lesions. Pharmacological treatment consisted of a 4-month treatment
regime of twice daily methotrexate (50 mg; JW Pharmaceutical,
Seoul, Republic of Korea) and thalidomide (200 mg; TayTech BioGen,
Seoul, Republic of Korea) administration, followed by a one-time
administration of azaprine (100 mg; Korean United Pharmaceutical,
Inc., Seoul, Republic of Korea), an immunosuppressive drug, and 10
mg/day prednisolone (Korea Pharma, Seoul, Republic of Korea) for 1
year. The majority of the skin lesions in the trunk and vaginal
mucosa were successfully treated, albeit the erosive lesion in the
tongue was non-responsive to systemic pharmacological treatment and
caused persistent pain. Therefore, AgNO3 (Gana Chem Co.,
Ltd., Ulsan, Republic of Korea) treatment and local injection of
Tamceton (40 mg; HanAll BioPharma Co., Ltd., Seoul, Republic of
Korea) were administered 20 and 15 times, respectively. However,
the tongue lesion was non-responsive to these treatments, and the
patient underwent intraluminal brachytherapy.
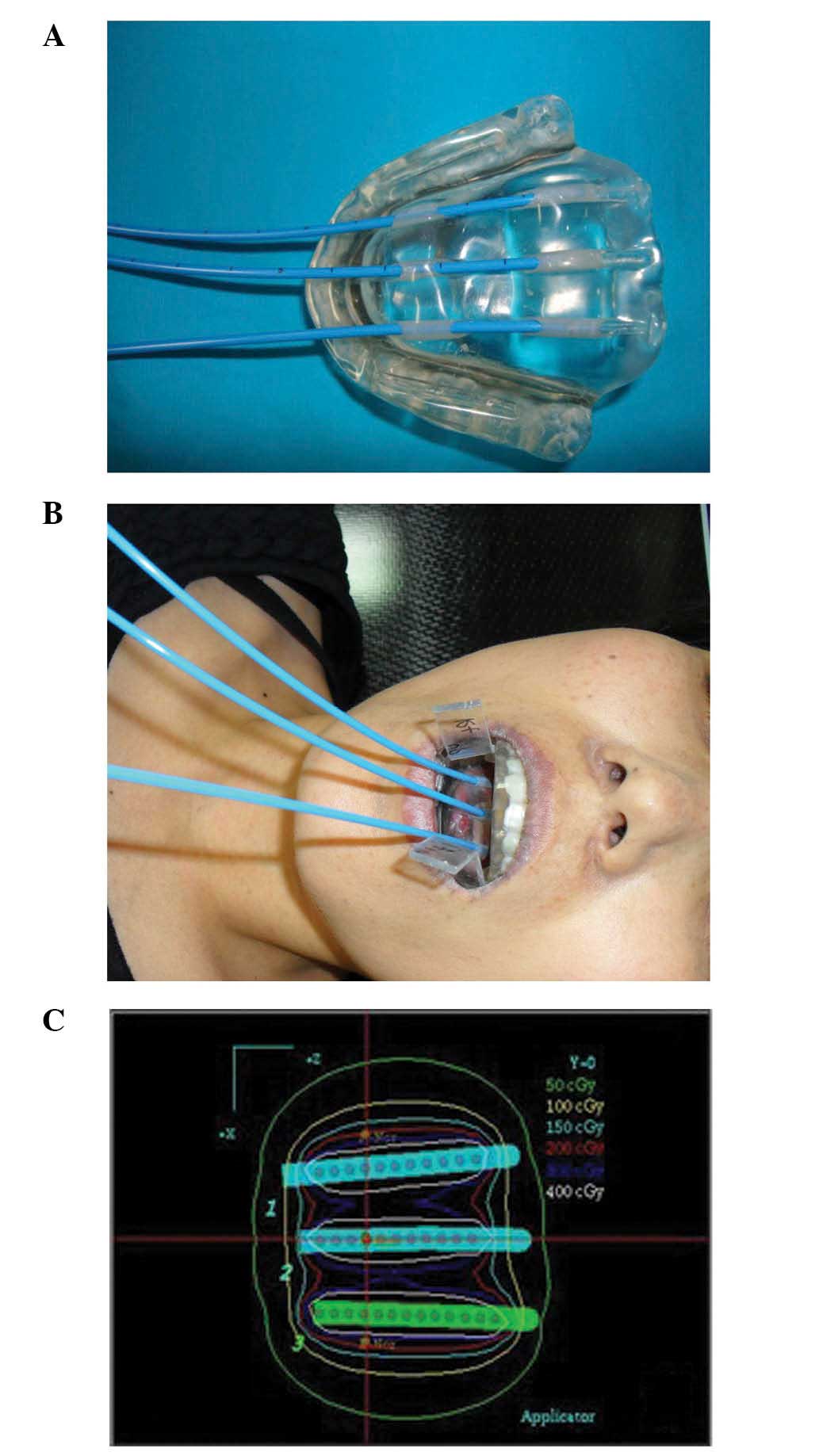
Oral lesions were limited to the anterior half of
the tongue, and no ulcerous lesions were observed in the buccal
mucosa or gingiva (Fig. 3).
Intraluminal brachytherapy was performed (date, 7/1/2010) to treat
locally-located lesions, prevent damage to the gingiva and enhance
the radiation dose effect. The device for oral brachytherapy was
designed using acrylic resin and consisted of separate molds for
the upper and lower jaws. The mold for the lower jaw consisted of
three 6F catheter holes with 1-cm intervals to insert the catheter
for brachytherapy (Fig. 4A). The
mold for the lower jaw constituted 2-mm lead plates to minimize the
radiation exposure to the gingiva and teeth during the therapy,
which were located adjacent to the tongue lesion. A 2-mm lead plate
was also inserted into the mold for the upper jaw during each
therapy to reduce the radiation exposure to the palate (Fig. 4B). The radiation dose for each
therapy was limited to ≤15 cGy. Treatment was performed using a
Lumencath® catheter (6F 150 cm; Elekta Instrument AB
Stockholm, Stockholm, Sweden) for brachytherapy. Radiation
treatment consisted of 2 Gy per session and two sessions per week,
using an Iridium-192 high-dose-rate brachytherapy system
(microSelectron HDR afterloader; Elekta Instrument AB Stockholm)
(Fig. 4C). The patient was exposed
to a total of 40 Gy radiation during 20 therapy sessions.
Grade 2 radiation-induced oral mucositis (9) was observed during the treatment.
Chronic side effects were not observed during the follow-up period
and the majority of the tongue lesions were successfully treated
following brachytherapy (Fig. 5). No
disease progression was observed during the 4-year follow-up
period; the patient's oral disease lesions completely healed.
Discussion
Pemphigus vulgaris is characterized by acantholysis
and intraepidermal blister formation, which are caused by the loss
of normal interactions between cells due to the production of
autoantibodies against the surface proteins of keratinocytes
(10). However, Anhalt et al
(1) examined a case of pemphigus
vulgaris showing non-specific clinical symptoms, including painful
erosive mucosal lesions and various skin rashes, that were
associated with the production of autoantibodies against a tumor,
which they termed paraneoplastic pemphigus. Subsequently, Nguyen
et al (11) suggested PAMS as
an alternative and more appropriate name for paraneoplastic
pemphigus for various reasons. First, the heterogeneity of clinical
characteristics can be expressed as clear rash without blisters
against the cross-section of the cells; second, autoimmune
multiorgan syndrome targeting epidermal cells and internal organs
is commonly observed in patients with paraneoplastic pemphigus; and
third, respiratory failure as a result of changes in bronchial
epithelial cells is observed, despite not typically being
associated with pemphigus.
Anhalt et al (1) suggested that paraneoplastic pemphigus
be diagnosed using the results of direct and indirect
immunofluorescence analyses, immunoprecipitation assays, an
analysis of clinical symptoms, including mucosal lesions with pain,
various systemic skin lesions and internal organ tumors, and
characteristic histological findings, including necrosis of
keratinocytes, disjunction of intraepidermal pickle cells,
vacuolization of the basal cell layer and dermatitis in the cell
junction area. However, Camisa and Helm (6) reported that PAMS could not be diagnosed
in some cases due to insufficient findings upon examination or a
condition that prohibited such examinations. Therefore, authors of
that study proposed novel criteria for the diagnosis of PAMS based
on distinguishing between major and minor findings (6). The major findings included various
types of skin rashes, associated internal tumors and characteristic
immunoprecipitation results, whereas the minor findings included
the confirmed disjunction of pickle cells via histological
analysis, precipitation of immunoreactants between the basal cell
layer and cells upon direct immunofluorescence and positive
findings in indirect immunofluorescence analyses using epithelial
cells from rat urinary bladders (6).
Using this method, PAMS may be diagnosed if all the three major
findings are identified or if any two of the major findings and any
two of the minor findings are observed (6). In the present study, the patient was
diagnosed with PAMS since she showed two of the major findings and
two of the minor findings identified previously (1,4,10).
PAMS has been rarely reported and its accurate
prevalence is not fully known. This may be because many cases of
PAMS are misdiagnosed as other diseases, including erythema
multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis,
lichen planus, pemphigus and graft-versus-host disease, due to its
diversity of clinical manifestations and histopathological findings
(11).
At present, PAMS is considered an autoimmune disease
and thus is treated with palliative treatments, including removal
of the symptom-causing mass or administration of immunosuppressive
drugs or adrenal cortical hormones (3–7).
However, a clear method for its treatment has yet to be established
(3–8).
Painful oral erosive ulcers and various forms of
skin rashes are typical skin lesions associated with PAMS (2). In particular, stomatitis is a common
clinical symptom in PAMS patients (1,9–11). Stomatitis is observed in the earliest
stage of the disease and shows the strongest resistance to
treatment, such that it is often the most persistent of the
associated symptoms. It typically occurs on the lateral side of the
tongue and extends towards the lip versmilion, thus causing pain.
Notably, PAMS has been shown to have more severe symptoms and a
wider range of clinical manifestations, as compared with normal
pemphigus (10,11).
In the present case, the first symptom experienced
by the patient was an erosive lesion in the oral mucosa and tongue,
which was associated with severe pain. Other symptoms experienced
by the patient, including skin lesions of the trunk and vaginal
mucosa, were improved following surgical resection of the mass from
the retroperitoneum, which was associated with the patient's
Castleman's disease, as well as treatment with an adrenal cortical
hormone, methotrexate, thalidomide and an immunosuppressive drug,
azaprine. However, the oral lesion was unresponsive to the
pharmacological treatment and surgical resection, and was the cause
of persistent severe pain.
Previous studies have reported that autoimmune
disorders may be sensitive to radiation (12,13).
Therefore, radiation therapy was considered for the present case.
In the present study, the patient underwent brachytherapy to
minimize radiation exposure to the surrounding organs. As a result
of brachytherapy, the lesions in the tongue were controlled without
causing serious acute or chronic side effects. In addition, neither
worsening nor progression of the lesion was observed during the
4-year follow-up period.
In conclusion, the present study has demonstrated
that brachytherapy is a promising therapeutic strategy for the
persistent and drug-resistant oral lesions that are often observed
in patients with PAMS. However, regular observation of the patient
may be required due to the slow response of PAMS to treatment and
the high rate of relapse of this disease.
Acknowledgements
The present study was supported by funds from the
Institute of Clinical Medicine of Chonbuk National University,
Biomedical Research Institute, Chonbuk National University
Hospital.
References
|
1
|
Anhalt GJ, Kim SC, Stanley JR, Korman NJ,
Jabs DA, Kory M, Izumi H, Ratrie H III, Mutasim D and Ariss-Abdo L:
Paraneoplastic pemphigus. An autoimmune mucocutaneous disease
associated with neoplasia. N Engl J Med. 323:1729–1735. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bystryn JC, Hodak E, Gao SQ, Chuba JV and
Amorosi EL: A paraneoplastic mixed bullous skin disease associated
with anti-skin antibodies and a B-cell lymphoma. Arch Dermatol.
129:870–875. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sehgal VN and Srivastava G: Paraneoplastic
pemphigus/paraneoplastic autoimmune multiorgan syndrome. Int J
Dermatol. 48:162–169. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Anhalt GJ and Nousari C: Paraneoplastic
Pemphigus. Fitzpatrick's Dermatology in General Medicine (7th).
Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS and Leffell
DJ: McGraw-Hill Education. (New York, NY). 468–474. 2008.
|
|
5
|
Lane JE, Woody C, Davis LS, Guill MF and
Jerath RS: Paraneoplastic autoimmune multiorgan syndrome
(paraneoplastic pemphigus) in a child: Case report and review of
the literature. Pediatrics. 114:e513–e516. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Camisa C and Helm TN: Paraneoplastic
pemphigus is a distinct neoplasia-induced autoimmune disease. Arch
Dermatol. 129:883–886. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wade MS and Black MM: Paraneoplastic
pemphigus: A brief update. Australas J Dermatol. 46:1–8. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Huang CJ, Hou MF, Luo KH, Wei SY, Huang
MY, Su SJ, Kuo HY, Yuan SS, Chen GS, Hu SC and Chuang HY: RTOG,
CTCAE and WHO criteria for acute radiation dermatitis correlate
with cutaneous blood flow measurements. Breast. 24:230–236. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Garran C, Montesdeoca N and Martinez MR:
Treatment of upper gum cercinima with high-dose-rate
customized-mold brachytherapy. Brachytherapy. 7:267–269. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Heymann WR: Paraneoplastic autoimmune
multiorgan syndrome. J Am Acad Dermatol. 51:631–632. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nguyen VT, Ndoye A, Bassler KD, Shultz LD,
Shields MC, Ruben BS, Webber RJ, Pittelkow MR, Lynch PJ and Grando
SA: Classification, clinical manifestations and immunopathological
mechanisms of the epithelial variant of paraneoplastic autoimmune
multiorgan syndrome: A reappraisal of paraneoplastic pemphigus.
Arch Dermatol. 137:193–206. 2001.PubMed/NCBI
|
|
12
|
Billet SE, Grando SA and Pittelkow MR:
Paraneoplastic autoimmune multiorgan syndrome: Review of the
literature and support for a cytotoxic role in pathogenesis.
Autoimmunity. 39:617–630. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Neuhof D and Debus J: Outcome and late
complications of radiotherapy in patients with unicentric Castleman
disease. Acta Oncol. 45:1126–1131. 2006. View Article : Google Scholar : PubMed/NCBI
|