Introduction
Subarachnoid hemorrhage (SAH) is one of the most
serious acute neurologic events. Computed tomography (CT) of the
brain is the first diagnostic imaging method performed in patients
suspected of having a SAH. However, in rare circumstance, a similar
appearance may occur in CT imaging in the absence of blood in the
subarachnoid space, which has been designated as
‘pseudo-subarachnoid hemorrhage, PSAH’ (1). Although the exact mechanisms remain
unknown, severe diffuse brain edema might be associated with PSAH,
and it is extremely important to increase the recognition of PSAH
and to distinguish it from true SAH.
PSAH has been observed in various severe clinical
events, including acute poisoning (2), cardiopulmonary arrest without trauma
(3,4)
and sudden unconscious and generalized convulsions (5). In these cases, it was reported that the
prognoses of patients were all poor and the common characteristics
of pathophysiology were internal medicine-refractory diffuse
cerebral edema due to anoxic encephalopathy. Recent clinical trials
have favored hyperbaric oxygen therapy (HBOT) as a promising
therapeutic strategy for adult patients with severe head injury
(6,7); however, clinical data on the safety and
efficacy of HBOT in the pediatric field, with the exception of
acute carbon monoxide poisoning (8),
remains scarce. The present case report describes a pediatric case
of diffuse brain edema characterized by a radiological appearance
of PSAH successfully treated with HBOT.
Case report
A 10 year-old previously healthy boy was admitted to
the Yuhuangding Hospital (Yantai, China) with a 2-day history of a
fever and headache. The patient experienced a 3–5-min long,
generalized tonic-clonic convulsion and became unconscious 2 h
prior to admission. On admission, he had a temperature of 39°C and
was comatose. Brain stem reflexes were preserved and deep tendon
reflexes were very brisk, with a Glasgow coma scale (GCS) score of
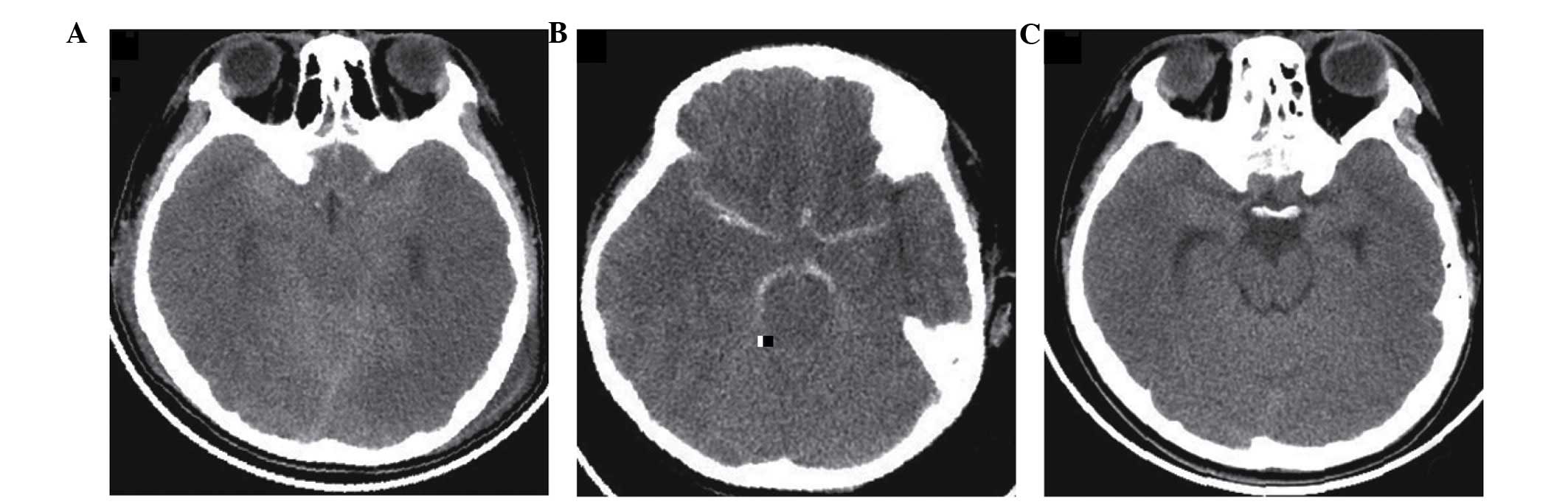
6 (E1V1M4). Brain CT (Fig. 1A)
revealed increased attenuation of the subarachnoid spaces in basal
cisterns, as well as signs of diffuse cerebral edema and was
interpreted as SAH by a radiologist. Lumbar puncture was performed
following treatment with mannitol (0.6 g/kg body weight infusion
over 30 min). Cerebrospinal fluid (CSF) examination revealed the
following results: Leukocytes, 180×106/l, with
lymphocytic predominance; no erythrocytes; normal protein, chloride
and glucose levels; and negative Gram stain. The lumbar puncture
showed no evidence of SAH while supporting viral encephalitis. CT
results were again considered and eventually interpreted as PASH.
The patient was treated with acyclovir (10 mg/kg body weight
repeated every 8 h for 10 days) and mannitol (0.6 g/kg body weight
repeated every 4–6 h for 72 h).
On day 2 of hospitalization, the mental status of
the patient was continuing to worsen, and intubation was required
for airway protection. The subsequent brain CT (Fig. 1B) continued to show signs of diffuse
cerebral edema and the attenuation values within the cisterns
ranged from 22 to 46 Hounsfield units (Hu), with a mean value 33
Hu. HBOT was administered at 72 h post admission. The protocol
consisted of 100% oxygen for 60 min at 2.0 absolute atmospheres.
Following the initial therapy, the GCS score of the patient
improved from 6 to 11 (E4V2M5), and he was successfully extubated
on day 4 of hospitalization.
On day 6 of hospitalization, following 3 days of
HBOT, the patient was able to eat, occasionally say words, follow
commands and display purposeful and spontaneous movements of his
arms and legs. Repeat brain CT (Fig.
1C) demonstrated that the basal cisterns had reopened and the
abnormal hyperdensity had disappeared. After 20 sessions of HBOT,
the patient was discharged with significant improvements in
ambulation, balance, speech and cognition. At the 1-year follow-up,
the patient had recovered completely and had resumed school without
apparent neurological sequelae. The present study was conducted in
accordance with the Declaration of Helsinki, and with approval from
the Ethics Committee of Yuhuangding Hospital. Written informed
consent was obtained from participant's guardians.
Discussion
A PSAH finding is a CT pseudo lesion that exhibits
characteristics similar to those of SAH, with a hyperattenuated
appearance of the cisterns and cerebral sulci relative to the brain
parenchyma (3). Although the exact
mechanisms causing the appearance of SAH remain unclear, cerebral
edema may be associated with PSAH (9). The dural sinuses are compressed by
severe brain edema, which compromises the venous drainage from the
brain and results in the cerebral veins becoming engorged; they
thus stand out against the edematous low attenuated cerebral
parenchyma, mimicking an SAH (10).
Senthilkumaran et al proposed the application of the
attenuation values (in Hu) to assist emergency physicians in
distinguishing PSAH from SAH: In basal cisterns of PSAH the
attenuation coefficient was reported to be 21–44 Hu, with a mean of
29–33Hu (11). The present patient
had an attenuation coefficient in the basal cisterns of 22–46 Hu
(mean, 33Hu), which is consistent with a diagnosis of PSAH on CT
imaging.
Previous reports have indicated that patients with
PSAH have a poor prognosis, and that he main risk factors for poor
outcome were increased intracranial pressure (ICP), higher lactate
levels, a longer duration of secondary anoxia due to cerebral
edema, and lack of effective treatment using internal medicine
(9,10). As early as 1982, Sukoff and Ragatz
reported that hyperbaric oxygenation was able to treat acute
cerebral edema effectively by reducing intracranial pressure and
concomitantly increasing cerebral oxygenation (12). In adults, studies have revealed that
HBOT can decrease cerebral edema, maintain blood-brain barrier
integrity, improve regional oxygen metabolism, and lower ICP and
dialysate lactate levels (6,13). HBOT refers to the inhalation of 100%
oxygen inside a hyperbaric chamber pressurized to >1 atmosphere.
The mechanisms of HBOT include increasing the partial pressure of
oxygen within the blood and the subsequent improvement of
mitochondrial metabolism and tissue oxygenation (14).
To the best of our knowledge, the present case
report describes the first pediatric case of acute nontraumatic
cerebral edema successfully treated with HBOT. However, the optimal
regimen for treating acute brain edema, and the efficacy and safety
of HBOT in the pediatric field, particularly in neonates and
infants remains elusive.
References
|
1
|
Chute DJ and Smialek JE:
Pseudo-subarachnoid hemorrhage of the head diagnosed by
computerized axial tomography: A postmortem study of ten medical
examiner cases. J Forensic Sci. 47:360–365. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
al-Yamany M, Deck J and Bernstein M:
Pseudo-subarachnoid hemorrhage: A rare neuroimaging pitfall. Can J
Neurol Sci. 26:57–59. 1999.PubMed/NCBI
|
|
3
|
Agha A and Al-Hakami M: A case report of
pseudo-subarachnoid hemorrhage. Maedica (Buchar). 6:210–212.
2011.PubMed/NCBI
|
|
4
|
Given CA II, Burdette JH, Elster AD and
Williams DW III: Pseudo-subarachnoid hemorrhage: A potential
imaging pitfall associated with diffuse cerebral edema. AJNR Am J
Neuroradiol. 24:254–256. 2003.PubMed/NCBI
|
|
5
|
Cucchiara B, Sinson G, Kasner SE and
Chalela JA: Pseudo-subarachnoid hemorrhage: Report of three cases
and review of the literature. Neurocrit Care. 1:371–374. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rockswold SB, Rockswold GL, Zaun DA and
Liu J: A prospective, randomized Phase II clinical trial to
evaluate the effect of combined hyperbaric and normobaric hyperoxia
on cerebral metabolism, intracranial pressure, oxygen toxicity, and
clinical outcome in severe traumatic brain injury. J Neurosurg.
118:1317–1328. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wolf EG, Baugh LM, Kabban CM, Richards MF
and Prye J: Cognitive function in a traumatic brain injury
hyperbaric oxygen randomized trial. Undersea Hyperb Med.
42:313–332. 2015.PubMed/NCBI
|
|
8
|
Mitchell SJ and Bennett MH: Unestablished
indications for hyperbaric oxygen therapy. Diving Hyperb Med.
44:228–234. 2014.PubMed/NCBI
|
|
9
|
Ahn JH, Choi SC, Jung YS and Min YG:
Clinical characteristics of patients with pseudo-subarachnoid
haemorrhage who were successfully resuscitated from out-of-hospital
cardiopulmonary arrest. Hong Kong J Emerg Med. 19:85–91. 2012.
|
|
10
|
Yuzawa H, Higano S, Mugikura S, Umetsu A,
Murata T, Nakagawa A, Koyama A and Takahashi S: Pseudo-subarachnoid
hemorrhage found in patients with postresuscitation encephalopathy:
Characteristics of CT findings and clinical importance. AJNR Am J
Neuroradiol. 29:1544–1549. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Senthilkumaran S, Balamurugan N, Menezes
RG and Thirumalaikolundusubramanian P: Role of Hounsfield units to
distinguish pseudo-subarachnoid hemorrhage. Clin Toxicol (Phila).
49:9482011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sukoff MH and Ragatz RE: Hyperbaric
oxygenation for the treatment of acute cerebral edema.
Neurosurgery. 10:29–38. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bullock MR: Hyperbaric oxygen therapy. J
Neurosurg. 112:1078–1079. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Huang L and Obenaus A: Hyperbaric oxygen
therapy for traumatic brain injury. Med Gas Res. 1:212011.
View Article : Google Scholar : PubMed/NCBI
|