Introduction
Rheumatoid arthritis (RA) is a chronic and common
inflammatory disease affecting as much as 1% of the population
worldwide (1). It is a destructive
and progressive joint disease characterized by synovial membrane
inflammation and joint cartilage destruction, which results in
joint deformity and disability, and an impaired quality of life
(2). The occurrence of RA is more
common in females compared with males (1). Previous studies have indicated that
patients with RA are likely to experience irreversible joint damage
1 year after its onset (3). Thus,
the early diagnosis and treatment of RA are important for improved
outcomes of RA.
Magnetic resonance imaging (MRI) and ultrasound (US)
techniques, which provide the satisfactory visualization of joint
structures coupled with high sensitivity and specificity, are
commonly used in the clinical examination and radiographic
assessment of RA (4). MRI allows
direct visualization of synovitis, together with prognostic
information of neighboring bones and bone marrow, which provides
crucial evidence of bone erosion and bone marrow edema (5). Accumulating evidence has indicated that
MRI is more sensitive than conventional radiography in identifying
bone erosion and edema (6,7). Døhn et al (8) indicated that MRI was ~5 times more
sensitive than X-ray in the detection of bone erosion by comparing
MRI and X-ray of the second-to-fifth metacarpophalangeal (MCP)
joints of one hand in 17 patients with RA. In addition, a previous
report demonstrated that MRI scan images could predict the onset of
RA with high sensitivity (100%) and specificity (78%) in 31/33
patients, and evaluate the synovitis with erosion and/or bone edema
in a previous similar group of patients with RA (9).
Although US can not detect bone marrow edema, it is
used frequently for the clinical assessment of synovitis with
effusion, power Doppler signal and synovial hypertrophy (10). In a previous study, Zheng et
al (11) confirmed that US
examination was feasible and capable of predicting RA disease, as
measured by the disease activity score in 28 joints for the
evaluation of joints. Furthermore, McQueen et al (12) have previously indicated that US is
able to detect bone erosion with 95% specificity and 78% predictive
accuracy, with a bone volume loss of >20% in US-accessible
areas, such as in the dorsal and palmar aspects of MCP joints.
These results indicate that MRI and US may be applicable in the
evaluation of RA activity, progression and treatment responses.
In the present study, the effectiveness of
high-frequency US is compared with MRI in the detection of early
RA, and the advantages of each method, with regards to joint
effusion, synovial proliferation and bone marrow edema, are
identified.
Materials and methods
Patients
A total of 39 patients (20 men and 19 women; mean
age, 50.2 years) diagnosed with early-stage RA between January and
December 2010 in Yantai Yuhuangding Hospital (Yantai, China) were
enrolled in the current study. The diagnosis of RA was based on the
1987 American College of Rheumatology classification criteria
(13). Patients who had experienced
symptoms of RA for >24 months were excluded from the study. The
median age of patients at the onset of the disease was 51.8±2.2
years (range, 22–75 years). The mean disease course was 8.8±2.5
months. Written informed consent was obtained from all the
participants. The study was conducted with approval from the Ethics
Committee of Yantai Yuhuangding Hospital.
US examination
Ultrasonographic evaluation was performed using
color US diagnostic apparatus (LOGIQ-10; General Electric Company,
Fairfield, CT, USA), equipped with a 12-MHz linear array probe. US
was conducted by an experienced radiologist blinded to the study.
The patients were examined while sitting upright, with the hand
placed on a cushion and the palm facing upward. A total of 1,248
joints were scanned, including bilateral wrist joints, and the
sagittal and coronal sections of the hand joints. All patients
underwent US assessment of the wrists, MCP joints, proximal
interphalangeal (PIP) joints for the presence of joint effusion
(defined by the compressible anechoic intracapsular region), bone
erosion (defined by bone cortex breakage in the joint area) and
synovial proliferation (defined by thickness >2 mm in wrist
joints, and >1 mm in MIP and PIP joints with a low echo)
(14,15). Lateral flexion of MCP joints 2–5 and
wrists were examined for the presence of tendinitis and tendon
sheath edema. In addition, synovial blood flow in each joint was
assessed with color Doppler flow imaging and high-resolution color
flow.
MRI evaluation
All patients underwent MRI evaluation of hands and
wrists using a 3.0T MR system (Signa EXCITE; General Electric
Company). Patients were placed in a prone position with the hand
above the head and the palm facing upward. Continuous coronal and
axial plane MRI without contrast were obtained using T1-weighted
spin-echo sequences, short inversion time inversion recovery (STIR)
gradient-echo sequences and T2-weighted turbo spin-echo sequences,
respectively. The presence of erosion, bone marrow edema, synovial
thickening and tendinitis were assessed according to the Outcome
Measures in Rheumatology RA MRI Scoring system (5). MRI images were evaluated by a doctor
who was experienced in joint MRI.
Statistical analysis
Data analysis was performed using SPSS version 16.0
software (SPSS, Inc., Chicago, IL, USA). Data are expressed as the
mean ± standard deviation and were analyzed using χ2
test. P<0.05 was considered to indicate a statistically
significant difference.
Results
High-frequency US is significantly
better at detecting synovial proliferation and joint effusion,
compared with MRI
US and MRI results obtained from 39 patients are
presented in Table I. A total of 858
joints were scanned by US and MRI for the detection of bone
erosion, bone marrow edema, synovial proliferation and joint
effusion, while the other 390 tendons were used for the evaluation
of tendinitis and tendon sheath edema. No statistically significant
sensitivities were observed between high-frequency US and MRI in
bone erosion [44 (5.1%) vs. 35 (4.1%), respectively; P>0.05],
tendinitis [18 (4.6%) vs. 14 (1.5%), respectively; P>0.05] and
tendon sheath edema [37 (9.5%) vs. 30 (7.7%), respectively;
P>0.05]. Significant differences were identified between
high-frequency US and MRI in synovial proliferation [132 (15.4%)
vs. 66 (7.7%), respectively; P<0.05] and joint effusion [89
(10.4%) vs. 52 (6.1%), respectively; P<0.05]. Significantly
higher sensitivity (P<0.05) was identified in the detection of
bone marrow edema using MRI (5.5%) compared with high-frequency US
(0%).
 | Table I.Comparisons between high-frequency US-
and MRI-detected abnormalities in joints (n=858) in rheumatoid
arthritis. |
Table I.
Comparisons between high-frequency US-
and MRI-detected abnormalities in joints (n=858) in rheumatoid
arthritis.
| Item | No. joints | US (% total
joints) | MRI (% total
joints) | P-value | χ2 |
|---|
| Bone erosion | 858 | 44 (5.1%) | 35 (4.1%) | 0.300 | 1.075 |
| Bone marrow
edema | 858 | 0 (0.0%) | 47 (5.5%) | <0.001 | 48.324 |
| Synovial
proliferation | 858 | 132 (15.4%) | 66 (7.7%) | <0.001 | 24.870 |
| Joint effusion | 858 | 89 (10.4%) | 52 (6.1%) | 0.001 | 10.578 |
| Tendinitis | 390 | 18 (4.6%) | 14 (1.5%) | 0.470 | 0.521 |
| Tendon sheath
edema | 390 | 37 (9.5%) | 30 (7.7%) | 0.371 | 0.800 |
MRI is suitable for visualization of
bone marrow edema in early RA, and US is sensitive to the detection
of joint effusion and synovial proliferation
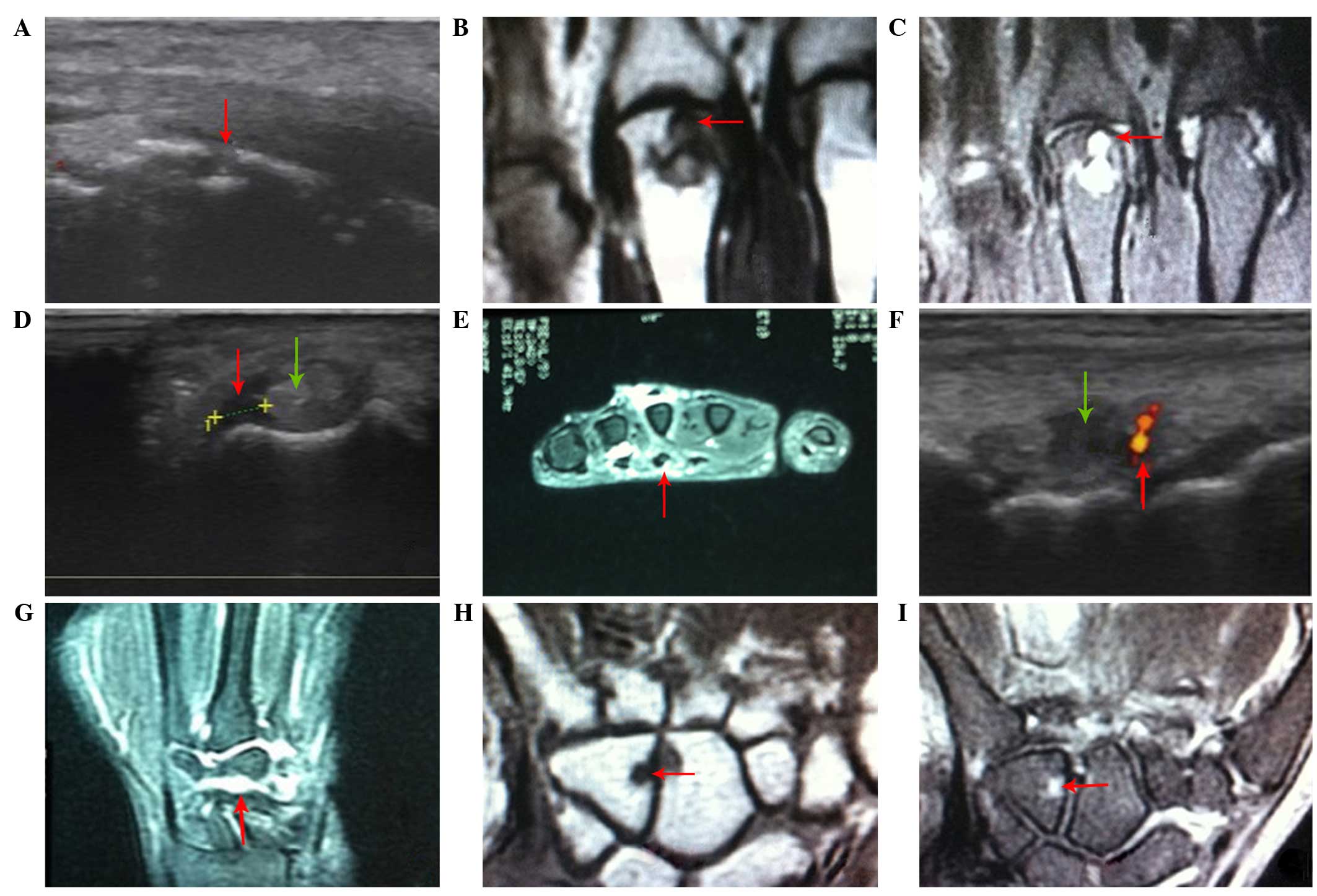
The symptoms of the above six abnormalities in RA
are presented in Fig. 1. The images
provide an insight into which types of imaging can provide the
required information in specific practice situations. Prominent
erosion in the distal third metacarpal bone with discontinuous bone
density (red arrow) was identified by US (Fig. 1A), while it was presented as moderate
hypointensity on a T1-weighted image (T1WI, red arrow) and
hyperintensity on a T2-weighted image (T2WI, red arrow) in the
coronal plane of the distal third metacarpal bone on MRI images
(Fig. 1B and C). Increased width in
the tendon (green arrow) with disturbance echo and a thin sheath
layer low echo (red arrow) were identified in the flexor tendon of
the left hand, which indicates tendinitis and tendon sheath edema
using high-frequency US (Fig. 1D).
Meanwhile, dilated tendon and high intensity on T2WI (red arrow) in
the surroundings of the tendon were observed in the sagittal planes
of the left-hand flexor tendon on the MRI images (Fig. 1E). Joint effusion with low echo,
synovial proliferation in a cotton-like shape and blood flow signal
in the synovium (red arrow) were identified in the bone gap of the
right wrist with US (Fig. 1F). Joint
effusion and synovial proliferation were presented as
hyperintensity on T2WI MRI images (red arrow) in the coronal
position of the bone gap of the right wrist (Fig. 1G). Bone marrow edema appeared as a
hyposignal on the T1-weighted sequence image, and hypersignal on
T2-weighted sequence image (red arrow), in the coronary carpal bone
of the left hand (Fig. 1H and I),
whereas bone marrow abnormality was not visualized using US. These
results suggest that MRI is ideally suited to visualizing bone
marrow edema in early RA, whereas US has high sensitivity and
diagnostic values in the detection of joint effusion and synovial
proliferation.
Discussion
RA is a form of autoimmune arthritis manifested with
persistent synovitis that most commonly involves the wrist and
finger joints (2). RA occurs across
all ethnic populations and ages, with a peak incidence between the
ages of 45 and 65 years (16).
Uncontrolled RA may result in permanent joint injury and other
extra-articular complications affecting normal activities and
quality of life (17). Aside from
genetic factors, environmental factors are prominent in the
development of RA (18). For
example, smoking is associated with a substantially increased risk
of RA (19), and patients
experiencing long-term stress are prone to developing RA (20). The early and accurate diagnosis of RA
serves an important role in the assessment of disease progression
and the early introduction of effective treatment options (21). Accumulating evidence indicates that
the early diagnosis of RA contributes towards the improved outcome
of RA, particularly within the first three months of the onset of
RA (22). Therefore, the
identification of changes associated with early RA using imaging
techniques is important in clinical practice.
To date, imaging techniques have served a focal role
in the evaluation of disease progression and the response to
therapy in RA (4). Plain radiography
has been traditionally used to detect and quantify RA, including
the detection of joint space loss, soft-tissue swelling and
marginal erosion (23). However, the
obtained information from X-ray analysis relies on relatively late
disease features, and is unsatisfactory with regards to current
demands, validity and accuracy.
Currently, US and MRI are commonly used in the
diagnosis and management of rheumatic disease (4). MRI provides a more global view of the
articular surfaces and internal bone structure of joints compared
with US. MRI enables the direct visualization of numerous bone and
soft tissue changes involving the synovial membrane, bone erosion
and cartilage thinning (24).
Additionally, MRI has a unique capacity to detect inflammation
within bone in the form of bone marrow edema, and this provides
important diagnostic and prognostic information in patients with
RA. US is widely used in the early diagnosis of RA, particularly in
the introduction and application of high frequency color Doppler
US, which can monitor joint effusion, blood flow change in the
synovium and synovial thickening (25). Furthermore, US may be used to monitor
disease status and predict disease recurrence, providing an
effective and valuable evaluation of treatments (26). Furthermore, US is more acceptable for
patients, as it is relatively simple, cheap and does not use
radiation (4). The combination of US
and MRI for the diagnosis of early RA has been validated (27). Szkudlarek et al (28) reported that the sensitivity and
specificity of Doppler US were 88.8 and 97.9%, respectively, which
is as effective as dynamic MRI for the evaluation of synovitis in
MCP joints. Rahmani et al (29) demonstrated that the overall
sensitivity and specificity of US in detecting bone erosion were 63
and 98%, respectively. Importantly, MRI and US have been described
as indispensable diagnostic tools to evaluate disease progression
and the response of disease, including RA, to various types of
treatments.
The decision of which modality should be used in
clinical diagnosis should be taken into consideration due to the
coexistence of the strengths and weaknesses of US and MRI. It is
important to understand the specific performance of US and MRI with
regards to imaging joint abnormalities. Bone marrow edema is
understood to be a marker for early inflammatory changes resulting
from cellular infiltration into bone marrow (30). The visualization of bone marrow edema
(BME) is clinically important in RA as it is the strongest
predictive factor in the progression of bone erosion (31). BME on MRI images is identified as a
lesion with intact trabecular structures and ill-defined margins
(32). It presents high signal
intensity on STIR or T2-weighted sequences, and presents low signal
intensity on T1-weighted MRI images (5). The ability of MRI to detect BME is
important since the pathologies of BME can not be visualized by
US.
Bone erosion, a central feature and common finding
in RA, is associated with disease severity and poor functional
outcome (33). The presence of
erosion detected by MRI is identified by direct contact with
cortical bone with sharp margins and obvious destruction of the
cortical bone barrier (34). Erosion
presents as hyperintensity on STIR or T2-weighted sequences and
hypointensity on T1-weighted sequences (34). In addition, it is described as an
intra-articular discontinuity of the bone surface that is visible
in two perpendicular planes on US images (15). It is controversial with regards to
which image modality has superior sensitivity in the detection of
bone erosion. Magnani et al (35) suggested that US was at least as
sensitive as MRI in detecting bone erosion in wrist and MCP joints,
while other evidence indicated that MRI had significantly increased
sensitivity compared with US for the evaluation of erosion in the
wrist and hand (36). Consistent
with the previous report (34), the
present study observed no significant difference between
high-frequency US and MRI with regards to the detection of bone
erosion. Soft tissues are often present in joint surroundings, such
as in the tendon and tendon sheath, resulting in tendinitis and
tendon sheath edema, which are common complications of RA that
typically occur in the hands and wrists (37). The abnormalities typically present as
dilated tendons with irregular margins, accompanied with a
disturbed fibrous-like echo (38).
In the present study, although high-frequency US demonstrated
slightly increased sensitivities with regards to detecting
tendinitis and tendon sheath edema, no statistically significant
differences were identified compared with MRI results.
Proliferative synovitis is the earliest and most
important pathological change observed in RA, and it is associated
with the quantity of joint fluid present (39). The presence of proliferative
synovitis on MRI is identified by a thickened area of synovial
compartment that presents as hypointensity on T1-weighted sequences
and hyperintensity on T2-weighted sequences (40). Although it is often less bright on
fluid-sensitive sequences in comparison with joint fluid, it can
not be easily differentiated from joint fluid based on the presence
of similar weighted sequences. Proliferative synovitis detected by
US presents as abnormal hypoechoic intra-articular tissue that is
poorly compressible and non-displaceable with Doppler signal
exhibition (15). The
non-displaceable nature of proliferative synovitis enables US to
distinguish between joint fluid and synovial thickening. Kasukawa
et al (41) indicated that US
was easy to use and effective in estimating the degree and pattern
of synovial proliferation and synovial effusion in the knee joints
of patients with RA. In the current study, it was demonstrated that
US was significantly more sensitive in detecting synovial
proliferation and joint effusion compared with MRI.
Providing effective treatments for RA following the
onset of the disease is essential in order to avoid the risk of
long-term structural and functional damage. To date, therapies used
to treat RA include non-steroidal anti-inflammatory drugs, which
are used for the treatment of pain and inflammation, and
disease-modifying antirheumatic drugs, which are commonly used as
first-line therapy for all newly diagnosed cases of RA (42). In addition, glucocorticoids and other
biological agents are used as a treatment strategy for RA (43,44).
Furthermore, non-pharmacological and non-surgical interventions are
increasingly optimized in patients with RA, including comprehensive
occupational therapy, wrist working splints and finger splints
(45).
In conclusion, the results in the present study
indicated that high-frequency US and MRI are both effective in
detecting bone erosion, tendinitis and tendon sheath edema in
patients with early RA. MRI was demonstrated to be superior in the
evaluation of bone marrow edema, while high-frequency US
demonstrated an increased sensitivity for detecting early joint
effusion and synovial proliferation in comparison with MRI. As
further evidence becomes available, US and MRI will become
increasingly important in the diagnosis and management of early RA.
High-frequency US may be considered as a valuable modality for the
detection of early RA, particularly when MRI is not accessible. The
decision of which tool should be used in a given trial should rely
on the clinical output requirement in order to minimize patient
discomfort.
References
|
1
|
Gibofsky A: Overview of epidemiology,
pathophysiology and diagnosis of rheumatoid arthritis. Am J Manag
Care. 18(Suppl 13): S295–S302. 2012.PubMed/NCBI
|
|
2
|
Apfelberg D, Maser R, Lash H, Kaye R,
Britton M and Bobrove A: Rheumatoid hand deformities:
Pathophysiology and treatment. West J Med. 129:267–272.
1978.PubMed/NCBI
|
|
3
|
Machold KP, Stamm TA, Nell VP, Pflugbeil
S, Aletaha D, Steiner G, Uffmann M and Smolen JS: Very recent onset
rheumatoid arthritis: Clinical and serological patient
characteristics associated with radiographic progression over the
first years of disease. Rheumatology (Oxford). 46:342–349. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Khan KM, Forster BB, Robinson J, Cheong Y,
Louis L, Maclean L and Taunton JE: Are ultrasound and magnetic
resonance imaging of value in assessment of Achilles tendon
disorders? A two year prospective study. Br J Sports Med.
37:149–153. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Østergaard M, Peterfy C, Conaghan P,
McQueen F, Bird P, Ejbjerg B, Shnier R, O'Connor P, Klarlund M,
Emery P, et al: OMERACT rheumatoid arthritis magnetic resonance
imaging studies. Core set of MRI acquisitions, joint pathology
definitions and the OMERACT RA-MRI scoring system. J Rheumatol.
30:1385–1386. 2003.PubMed/NCBI
|
|
6
|
Ostendorf B, Scherer A, Mödder U and
Schneider M: Diagnostic value of magnetic resonance imaging of the
forefeet in early rheumatoid arthritis when findings on imaging of
the metacarpophalangeal joints of the hands remain normal.
Arthritis Rheum. 50:2094–2102. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Suter L, Fraenkel L and Braithwaite R: The
role of magnetic resonance imaging in the diagnosis and prognosis
of rheumatoid arthritis. Arthritis Care Res (Hoboken). 63:675–688.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Døhn UM, Ejbjerg BJ, Hasselquist M,
Narvestad E, Court-Payen M, Szkudlarek M, Møller J, Thomsen HS and
Ostergaard M: Rheumatoid arthritis bone erosion volumes on CT and
MRI: Reliability and correlations with erosion scores on CT, MRI
and radiography. Ann Rheum Dis. 66:1388–1392. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Narváez J, Sirvent E, Narváez JA, Bas J,
Gómez-Vaquero C, Reina D, Nolla JM and Valverde J: Usefulness of
magnetic resonance imaging of the hand versus anticyclic
citrullinated peptide antibody testing to confirm the diagnosis of
clinically suspected early rheumatoid arthritis in the absence of
rheumatoid factor and radiographic erosion. Semin Arthritis Rheum.
38:101–109. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Backhaus M, Burmester G, Sandrock D,
Loreck D, Hess D, Scholz A, Blind S, Hamm B and Bollow M:
Prospective two year follow up study comparing novel and
conventional imaging procedures in patients with arthritic finger
joints. Ann Rheum Dis. 61:895–904. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zheng G, Wang L, Jia X, Li F, Yan Y, Yu Z,
Li L, Wei Q and Zhang F: Application of high frequency color
doppler ultrasound in the monitoring of rheumatoid arthritis
treatment. Exp Ther Med. 8:1807–1812. 2014.PubMed/NCBI
|
|
12
|
McQueen FM: Imaging in early rheumatoid
arthritis. Best Pract Res Clin Rheumatol. 27:499–522. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Arnett FC, Edworthy SM, Bloch DA, McShane
DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH and Luthra
HS: The American rheumatism association 1987 revised criteria for
the classification of rheumatoid arthritis. Arthritis Rheum.
31:315–324. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Schmidt W, Schmidt H, Schicke B and
Gromnica-Ihle E: Standard reference values for musculoskeletal
ultrasonography. Ann Rheum Dis. 63:988–994. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wakefield RJ, Balint PV, Szkudlarek M,
Filippucci E, Backhaus M, D'Agostino MA, Sanchez EN, Iagnocco A,
Schmidt WA, Bruyn GA, et al: Musculoskeletal ultrasound including
definitions for ultrasonographic pathology. J Rheumatol.
32:2485–2487. 2005.PubMed/NCBI
|
|
16
|
Gabriel SE: The epidemiology of rheumatoid
arthritis. Rheum Dis Clin North Am. 27:269–281. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cooles FA and Isaacs JD: Pathophysiology
of rheumatoid arthritis. Curr Opin Rheumatol. 23:233–240. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Scott IC, Steer S, Lewis CM and Cope AP:
Precipitating and perpetuating factors of rheumatoid arthritis
immunopathology: Linking the triad of genetic predisposition,
environmental risk factors and autoimmunity to disease
pathogenesis. Best Pract Res Clin Rheumatol. 25:447–468. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hutchinson D, Shepstone L, Moots R, Lear J
and Lynch M: Heavy cigarette smoking is strongly associated with
rheumatoid arthritis (RA), particularly in patients without a
family history of RA. Ann Rheum Dis. 60:223–227. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Cutolo M and Straub RH: Stress as a risk
factor in the pathogenesis of rheumatoid arthritis.
Neuroimmunomodulation. 13:277–282. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kahlenberg J and Fox D: Advances in the
medical treatment of rheumatoid arthritis. Hand Clin. 27:11–20.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nell V, Machold K, Eberl G, Stamm T,
Uffmann M and Smolen J: Benefit of very early referral and very
early therapy with disease-modifying anti-rheumatic drugs in
patients with early rheumatoid arthritis. Rheumatology (Oxford).
43:906–914. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Guillemin F, Billot L, Boini S, Gerard N,
Ødegaard S and Kvien TK: Reproducibility and sensitivity to change
of 5 methods for scoring hand radiographic damage in patients with
rheumatoid arthritis. J Rheumatol. 32:778–786. 2005.PubMed/NCBI
|
|
24
|
Hodgson RJ, O'Connor P and Moots R: MRI of
rheumatoid arthritis image quantitation for the assessment of
disease activity, progression and response to therapy.
Rheumatology. 47:13–21. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Patil P and Dasgupta B: Role of diagnostic
ultrasound in the assessment of musculoskeletal diseases. Ther Adv
Musculoskelet Dis. 4:341–355. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Foltz V, Gandjbakhch F, Etchepare F,
Rosenberg C, Tanguy ML, Rozenberg S, Bourgeois P and Fautrel B:
Power doppler ultrasound, but not low-field magnetic resonance
imaging, predicts relapse and radiographic disease progression in
rheumatoid arthritis patients with low levels of disease activity.
Arthritis Rheum. 64:67–76. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Amin MF, Ismail FM and El Shereef RR: The
role of ultrasonography in early detection and monitoring of
shoulder erosion and disease activity in rheumatoid arthritis
patients; comparison with MRI examination. Acad Radiol. 19:693–700.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Szkudlarek M, Court-Payen M, Strandberg C,
Klarlund M, Klausen T and Østergaard M: Power doppler
ultrasonography for assessment of synovitis in the
metacarpophalangeal joints of patients with rheumatoid arthritis: A
comparison with dynamic magnetic resonance imaging. Arthritis
Rheum. 44:2018–2023. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Rahmani M, Chegini H, Najafizadeh SR,
Azimi M, Habibollahi P and Shakiba M: Detection of bone erosion in
early rheumatoid arthritis: Ultrasonography and conventional
radiography versus non-contrast magnetic resonance imaging. Clin
Rheumatol. 29:883–891. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Orr JD, Sabesan V, Major N and Nunley J:
Painful bone marrow edema syndrome of the foot and ankle. Foot
Ankle Int. 31:949–953. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
McQueen FM and Ostendorf B: What is MRI
bone oedema in rheumatoid arthritis and why does it matter?
Arthritis Res Ther. 8:2222006. View
Article : Google Scholar : PubMed/NCBI
|
|
32
|
Szopińska I, Kontny E, Maśliński W,
Sobieszek M, Warczyńska A and Kwiatkowska B: Significance of bone
marrow edema in pathogenesis of rheumatoid arthritis. Pol J Radiol.
78:57–63. 2013. View Article : Google Scholar
|
|
33
|
Schett G and Gravallese E: Bone erosion in
rheumatoid arthritis: mechanisms, diagnosis and treatment. Nat Rev
Rheumatol. 8:656–664. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Jimenez-Boj E, Nöbauer-Huhmann I,
Hanslik-Schnabel B, Dorotka R, Wanivenhaus AH, Kainberger F,
Trattnig S, Axmann R, Tsuji W, Hermann S, et al: Bone erosion and
bone marrow edema as defined by magnetic resonance imaging reflect
true bone marrow inflammation in rheumatoid arthritis. Arthritis
Rheum. 56:1118–1124. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Magnani M, Salizzoni E, Mulè R, Fusconi M,
Meliconi R and Galletti S: Ultrasonography detection of early bone
erosion in the metacarpophalangeal joints of patients with
rheumatoid arthritis. Clin Exp Rheumatol. 22:743–748.
2004.PubMed/NCBI
|
|
36
|
Hoving JL, Buchbinder R, Hall S, Lawler G,
Coombs P, McNealy S, Bird P and Connell D: A comparison of magnetic
resonance imaging, sonography and radiography of the hand in
patients with early rheumatoid arthritis. J Rheumatol. 31:663–675.
2004.PubMed/NCBI
|
|
37
|
Alvarez-Nemegyei J and Canoso JJ:
Evidence-based soft tissue rheumatology: III: Trochanteric
bursitis. J Clin Rheumatol. 10:123–124. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Harcke HT, Grissom LE and Finkelstein MS:
Evaluation of the musculoskeletal system with sonography. AJR Am J
Roentgenol. 150:1253–1261. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Kannegieter NJ: Chronic proliferative
synovitis of the equine metacarpophalangeal joint. Vet Rec.
127:8–10. 1990.PubMed/NCBI
|
|
40
|
Barile A, Sabatini M, Iannessi F, Di
Cesare E, Splendiani A, Calvisi V and Masciocchi C: Pigmented
villonodular synovitis (PVNS) of the knee joint: magnetic resonance
imaging (MRI) using standard and dynamic paramagnetic contrast
media. Report of 52 cases surgically and histologically controlled.
Radiol Med. 107:356–366. 2004.PubMed/NCBI
|
|
41
|
Kasukawa R, Takeda I, Iwadate H and Kanno
T: Ultrasonographic evaluation of synovial effusion and synovial
proliferation pattern in the knee joints of patients with
rheumatoid arthritis. Mod Rheumatol. 12:64–68. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Ong CK, Lirk P, Tan CH and Seymour RA: An
evidence-based update on nonsteroidal anti-inflammatory drugs. Clin
Med Res. 5:19–34. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Gaffo A, Saag KG and Curtis JR: Treatment
of rheumatoid arthritis. Am J Health Syst Pharm. 63:2451–2465.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Gorter SL, Bijlsma JW, Cutolo M,
Gomez-Reino J, Kouloumas M, Smolen JS and Landewé R: Current
evidence for the management of rheumatoid arthritis with
glucocorticoids: A systematic literature review informing the EULAR
recommendations for the management of rheumatoid arthritis. Ann
Rheum Dis. 69:1010–1014. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Vlieland TP and Van den Ende CH:
Nonpharmacological treatment of rheumatoid arthritis. Curr Opin
Rheumatol. 23:259–264. 2011. View Article : Google Scholar : PubMed/NCBI
|