Introduction
Acute encephalitis with refractory, repetitive
partial seizures (AERRPS) was first reported by the Japanese
scholar Sakuma et al (1) in
2001. As the clinical manifestations, neuroimaging findings and
prognosis of AERRPS are different from the known acute
encephalitis, the international medical community classified AERRPS
as a novel disease.
Primary clinical findings include the following:
Acute onset of seizures or consciousness impairment; frequent and
refractory partial seizures; the need for long-term anesthesia
(more than 2 weeks) with intravenous barbiturates or
benzodiazepines; a fever during the acute phase of illness;
cerebrospinal fluid (CSF) analysis revealing mild pleocytosis or
slight increase in protein; electroencephalogram (EEG) revealing
slow background during the acute phase and multifocal spikes during
the chronic phase; and magnetic resonance imaging (MRI) revealing
no specific abnormalities aside from occasional T2/fluid attenuated
inversion recovery hyperintense signals of the mesial temporal lobe
(1–7). To date, >200 cases have been
reported worldwide. AERRPS primarily affects school-age children
and adolescents (8). The present
study reports one case that was presented in 2008, and describes
the treatment that was provided.
Case report
The present study reports the case of a male 46
year-old patient with no history of head trauma, seizures and other
diseases, who smokes 20 cigarettes daily and has a long history of
alcohol consumption. The patient suffered a persistent headache
from December 14, 2008 after developing a cold. The headache
reportedly increased during exercise, and was accompanied with
general aches, fever, and a fluctuating body temperature between
38.5 and 39°C. At 7:00 am, December 17th during exercise at home,
the patient suddenly exhibited general convulsions,
unconsciousness, showed the whites of his eyes, and experienced
trismus, facial cyanosis, and limb stiffness followed by clonus,
which lasted ~2 min before the convulsions remitted. The patient
awoke a number of minutes later. The patient suffered from the
above convulsions at 8:00 a.m., December 17th in the emergency room
of Qinghai Provincial People's Hospital (Xingin, China), and was
fractionally intravenously injected 50 mg diazepam (Xudong Haipu
Pharmaceutical, Ltd., Shanghai, China). The convulsions arrested ~5
min following the injection; however, the patient still exhibited
dysphoria, despite the cranial computed tomography (CT) examination
detecting no abnormalities. The patient was, therefore, admitted
into the Emergency Intensive Care Unit (EICU) at Qinghai Provincial
People's Hospital on December 17th. The present study was conducted
in accordance with the declaration of Helsinki and was performed
with approval from the Ethics Committee of Qinghai Provincial
People's Hospital. Written informed consent was obtained from the
patient's family.
Examinations
On December 17th, the patient's body temperature was
38.4°C, pulse was 90 beats/min, breathing was 29 times/min and
blood pressure was 121/77 mmHg. The patient was in a light coma.
The bilateral pupils exhibited the same size and roundness (3.0
mm), and were sensitive to light. The cardiopulmonary abdominal
examination was normal. Neurological examination revealed cervical
resistance and a jaw-chest distance of three cross-fingers, and no
other positive signs were found in the nervous system.
Auxiliary examinations
On December 17th, the patient's cranial CT and chest
X-ray showed no abnormalities. White blood cell count was
12.46×109 cells/l (measured using an Automatic
Hematology Analyzer; cat. no. XT-1800i; Sysmex Corporation, Kobe,
Japan). A lumbar puncture was performed three times on the first,
fifth and sixteenth day, and the CSF pressures were 190 cm
H2O, 215 cm H2O and 175 cm H2O,
respectively; the cell counting (white blood cells in CSF) was 13
cells/mm, 8 cells/mm and 5 cells/mm, respectively; protein
concentration was 1.22 g/l, 1.14 g/l and 0.37 g/l, respectively
(cell counting and protein concentration measured using Cobas 8000
Modular Analyzer; Roche Diagnostics, Basel, Switzerland); and the
detection of cryptococcus was negative (identified using an India
Ink Staining kit; cat. no. BA4042; Beisuo Biological Technology,
Ltd., Zhuhai, China). Viral immunological analysis of blood and CSF
showed no abnormalities.
Clinical course
The patient was diagnosed with viral encephalitis,
and measurements of intracranial pressure reduction were performed,
and ribavirin and phenobarbital was administered. Every 8 h, 0.1 mg
phenobarbital (New Asia Pharmaceutical, Ltd., Shanghai, China) was
intravenously injected. Every 12 h, 0.5 g ribavirin was
intravenously injected (Romit Pharmaceutical Corporation, Xinghua,
China) The patient exhibited convulsions again on the second day,
which were the same as those experienced prior to hospitalization;
the convulsions lasted ~3 min and were accompanied with apnea,
therefore, the patient underwent trans-oral intubation for
mechanical ventilation and was administered an intravenous
injection of 800 mg sodium valproate (Nankai Yongong
Pharmaceutical, Ltd., Tongliao, China), which was then consistently
administered to the patient (1 mg/min/kg). However, the patient
continued to experience frequent convulsions, >10 times daily,
which alternated between general tonic-clonic seizures and focal
facial-finger twitching seizures. Combinations of anti-epileptic
drugs and powerful sedatives had no significant clinical effects
(sodium valproate 1 mg/min/kg via pump; phenobarbital 0.1 mg
intravenously injected every 8 h; midazolam 32 mg/h (Corden Pharma
S.P.A., Monza, Italy) via pump; propofol 320 mg/h (Jiangsu Nhwa
Pharmaceutical Co., Ltd., Xuzhou, China) via pump; phenytoin 0.2 g
(Zhejiang Million State Pharmaceutical, Ltd., Wenling, China) via
nasogastric intubation every 8 h; and lamotrigine 25 mg
(GlaxoSmithKline, Poznań, Poland) via nasogastric intubation every
12 h). The plasma concentrations of valproate, phenobarbital and
phenytoin were monitored and maintained within the effective
therapeutic concentration ranges. As a result of the poor effects
of the above drugs, the patient was administered the muscle
relaxant vecuronium (Zhejiang Xianju Pharmaceutical, Ltd.,
Hangzhou, China) after one week, intravenously infused 2–4 mg/h.
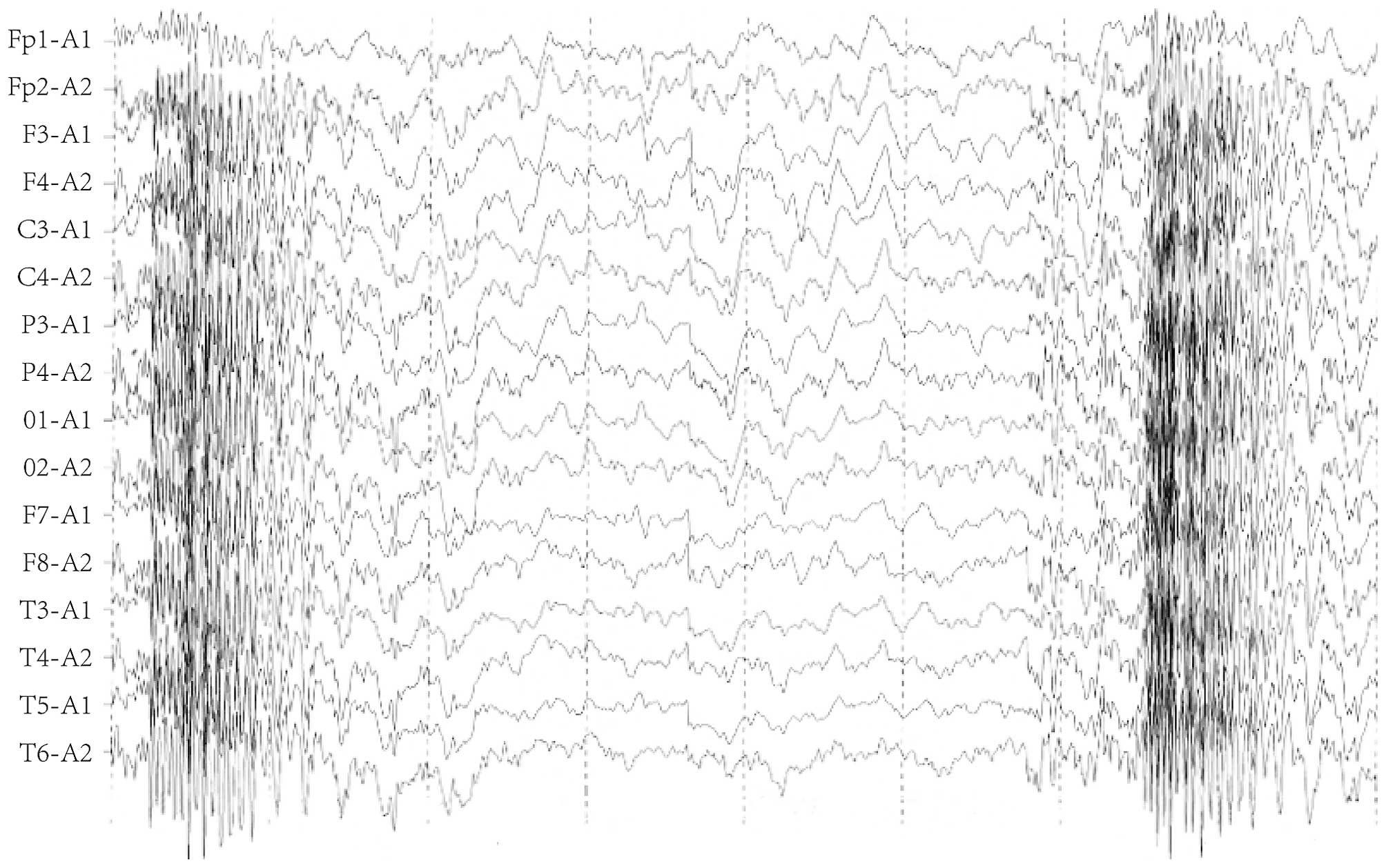
Although the systemic and local twitching was markedly reduced, EEG
monitoring demonstrated the persistent status of a large quantity
of high-amplitude sharp waves and spikes at all leads (Fig. 1).
After 5 days of the application of muscle relaxants,
the medication was withdrawn due to the absence of any effect. On
day 14 of hospitalization, the patient was diagnosed with AERRPS.
The administration of anti-epileptic drugs was arrested, and the
patient was administered an intravenous injection of 0.2 g
phenobarbital once every 2 h; the total daily quantity was 2.4 g,
and the plasma concentration was between 15 and 198 µg/ml. When the
plasma concentration was <100 µg/ml, no noticeable reduction of
seizures was observed. On day 19, the plasma concentration reached
137 µg/ml and general seizures were markedly reduced, although the
partial seizures remained frequent. On day 23, the plasma
concentration reached 198 µg/ml, and the general and partial
seizures were markedly decreased to 0–2 times daily (general
seizures) and 5–10 times daily (partial seizures). The dose of
phenobarbital was then gradually decreased, and when a large dose
of phenobarbital was administered on day 64 (0.2 g every 6 h), no
general convulsive seizures occurred. However, partial seizures
still occurred occasionally, therefore, the therapy was changed to
oral administration of 0.18 g phenobarbital three times per day.
Clinical characteristics of the patient included a long-term
lasting fever and a daily temperature fluctuating between 38.0 and
39.5°C. After day 29 when the convulsions became gradually
controlled, the body temperature gradually reduced to the normal
range. The patient became conscious on day 55, and although
language function, cognitive ability, capacity of calculation and
memory were impaired, the patient could walk under assistance. The
patient's intelligence was determined to be equivalent to that of
2–3 year-old child. Cranial MRI on day 56 and 217 after admission
showed no obvious abnormalities. The patient was transferred from
EICU to the Department of Neurology Rehabilitation of Qinghai
Provincial People's Hospital 93 days after admission, but succumbed
to suffocation on day 237.
Discussion
In 1986, Awaya and Fukuyama (2) first described a group of Japanese
children who suffered from acute encephalitis, with uncontrollable
partial and general seizures experienced during the acute and
convalescent phase throughout the whole course. In addition, the
children experienced various degrees of prolonged periods of fever;
the clinical course was not typical of general acute encephalitis,
the prognosis was poor, and the mortality and morbidity were high;
therefore, it was considered to be a novel disease (2). After 15 years, in 2001, Sakuma et
al (1) diagnosed and treated one
case, and retrospectively analyzed 21 cases reported in the
literature, and named the disease AERRPS. The following diagnostic
criteria were then proposed: i) The acute phase of encephalitis
lasts >2 weeks; ii) partial seizures accompanied with general
seizures occur throughout the acute and convalescent course; iii)
frequent seizures result in the sustained state, which is more
prominent in the acute phase; iv) the prominent clinical
manifestation of seizures is difficult to control; v) viral
encephalitis and systemic metabolic disorders are excluded. To
date, the English literature has reported >200 AERRPS cases,
including cases reported in Japan (3–12),
Chinese Taiwan (13,14), Italy (15), Australia (16) and the United Arab Emirates (17); other countries have reported a small
number of cases. The authors of the current study reported 4 cases
in 2009 in Chinese.
To date, the cause of AERRPS remains unclear,
although a previous report (2)
stated that it may be caused by a viral infection in the patients'
blood or CSF, no specific virus has been identified. Other previous
studies (7,10) reported evidence of immunological
abnormalities in the patients' blood or CSF, particularly in
glutamate receptor (GluR) antibodies. Wakamoto et al
(10) demonstrated that the GluR,
namely the ε2, ζ1 and δ2 subtype immunoglobulin G antibodies, exist
in the patient's blood and CSF, and that plasma interleukin (IL)-2,
IL-6, IL-10, tumor necrosis factor-α and interferon-γ were
significantly increased. Ito et al (4) used hormone impulse and high-dose
γ-globulin treatment and achieved positive results. An 11-year-old
male suffered from AERRPS, and was positive for autoantibodies to
the glutamate receptor Gluepsilon2 IgG or IgM in an examination of
blood and CSF. The patient was treated with artificial respiration,
thiamylal sodium, mild hypothermia therapy, steroid pulse therapy
and massive gamma-globulin therapy. Afterwards, the patient had
sequelae, such as post-encephalitic epilepsy (the same seizures
continued to recur), hyperkinesia, impairment of immediate memory,
a change in character (he became sunny and obstinate), dysgraphia,
and mild atrophy of the hippocampus, amygdala and cerebrum.
However, the patient could still attend school. These results
suggest that AERRPS may be immune-mediated autoimmune encephalitis.
In the present study, the patient experienced prodromal symptoms of
upper respiratory tract infections, such as fever, slight increase
of elevated CSF pressure and transient increase of cell count and
proteins. This suggests that AERRPS is caused by inflammatory
lesions of the central nervous system; however, the symptoms were
markedly different from the clinical course of general acute
encephalitis. It would have been beneficial to conduct
immunological tests of the CSF, but these were not performed. The
clinical course experienced by the patient in the current study
fully met the diagnostic criteria of AERRPS.
The neuroimaging of AERRPS exhibits no specificity
(2,18); the majority of patients exhibit
normal or non-specific changes with regards to cranial CT or MRI in
the acute phase, whereas various degrees of brain atrophy are
exhibited in their recovery phase and are associated with poor
prognosis. The two cranial MRIs performed on the patient in the
current study showed no cerebral atrophy, results which were not
concordant with previous studies. This may be related to the fact
that the central nervous system in a patient of school age has not
fully developed (8), thus cerebral
atrophy would be more likely to cause secondary damage in
children.
The most prominent feature of AERRPS that
distinguishes it from general acute encephalitis is its
uncontrollable epileptic seizures and poor prognosis. Almost every
patient in the acute and convalescent phase of AERRPS experiences
frequent complex partial seizures accompanied with or without
secondary general seizures (8). EEG
monitoring (5,13) demonstrated that the majority of
patients primarily exhibit slow-wave rhythm in intermittent
episodes, with sustained polymorphic δ activities, and focal or
fully explosive high-amplitude sharp rhythms at the onset of
complex partial and secondary general seizures. Although the
seizure frequency in the recovery phase is lower compared with the
acute phase, one previous study (18) reported that a 6-year-old patient
exhibited intermittent complex partial seizures for >3 years,
and eventually succumbed to the seizures. The clinical features and
EEG monitoring of the seizures in the patient in the present study
were consistent with those of previous studies (5,13). Two
weeks after the onset of the seizures, despite the administration
of combined various anti-epileptic drugs, including phenobarbital,
phenytoin, midazolam, sodium valproate, propofol and lamotrigine,
and muscle relaxants, the EEG monitoring and clinical onset showed
no improvement. The anti-epileptic drugs were withdrawn after two
weeks, and large doses of intravenous pentobarbital, 0.2 g/2 h,
were administered, reaching a daily dose of 2.4 g. When the plasma
concentration of pentobarbital achieved 137 µg/ml, the general
seizures were markedly reduced and EEG monitoring exhibited the
unique periodic outbreak-suppress form associated with a
phenobarbital-induced coma, namely the spike-explosive suppression
pattern (19). The highest blood
concentration reached 198 µg/ml, at which point the systemic and
local seizures were significantly reduced to 0–2 times daily
(general seizures) and 5–10 times daily (partial seizures).
Following this, the dosage of phenobarbital was gradually
decreased, until no general convulsive seizures occurred on day 64
of the application of large-dose phenobarbital. The patient
experienced occasional partial seizures with a plasma concentration
of phenobarbital maintained at ~50 µg/ml in the convalescent phase.
The intermittent episodes exhibited primarily slow-wave rhythms,
accompanied by polymorphous δ and β activities.
Since the cause of AERRPS is unknown, treatment
targeting uncontrollable recurrent epileptic seizures has become
the key to identifying the prognosis. Despite the option to
administer combined anti-epileptic drugs and strong anesthetic,
there lacks an effective means to fully control the seizures
(14). It was reported that the
intravenous injection of high-dose pentobarbital was effective in
the majority of patients (3,11), particularly in controlling general
seizures in the acute phase; the maximal dose used was >5
mg/kg/h, its effective blood concentration was >40 µg/ml and the
highest peak reached was 190 µg/ml.
Whether AERRPS is a novel disease and the
elucidation of its epidemiology and etiology remain the focus of
academic controversy. Although cases of AERRPS are rare, its unique
characteristics, different from general encephalitis, must be
recognized clinically. In the present study, although the patient
underwent long rehabilitation in his recovery phase, his
intelligence, language functions and motor functions were severely
impaired, and the patient ultimately succumbed to suffocation,
which was consistent with the poor prognosis reported.
The reported age distribution of patients with
AERRPS ranges between 5 months and 18 years; the disease primarily
affects school-age children and adolescents, with one case reported
of a 22 year old adult diagnosed with AERRPS (12). The patient in the present study was
46-years-old, inconsistent with the results of previous studies,
suggesting that children and young adults are the primary age
groups affected. However, the diagnostic criteria of AERRPS does
not emphasize age as a factor; when an adult patient meets the
diagnostic criteria, the possibility of AERRPS should be
considered, as the early application of large-dose phenobarbital to
control seizures may be the key towards improved prognosis.
References
|
1
|
Sakuma H, Fukumizu M and Kohyama J:
Efficacy of anticonvulsants on acute encephalitis with refractory,
repetitive partial seizures (AERRPS). No To Hattatsu. 33:385–390.
2001.(In Japanese). PubMed/NCBI
|
|
2
|
Awaya Y and Fukuyama Y: Epilepsy sequelae
of acute encephalitis: Encephalopathy (third report). Jpn J
Psychiatry Neurol. 40:385–387. 1986.
|
|
3
|
Hamano K, Watanabe A and Kohyama J: A case
of acute encephalitis with refractory, repetitive partial seizures
(AERRPS) showing transient disappearance of the seizure with
occurrence of choreo-ballistic movement. No To Hattatsu. 35:59–64.
2003.(In Japanese). PubMed/NCBI
|
|
4
|
Ito H, Mori K, Toda Y, Sugimoto M,
Takahashi Y and Kuroda Y: A case of acute encephalitis with
refractory, repetitive partial seizures, presenting autoantibody to
glutamate receptor Gluepsilon2. Brain Dev. 27:531–534. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Saito Y, Maegaki Y, Okamoto R, Ogura K,
Togawa M, Nanba Y, Inoue T, Takahashi Y and Ohno K: Acute
encephalitis with refractory, repetitive partial seizures: Case
reports of this unusual post-encephalitic epilepsy. Brain Dev.
29:147–156. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Maegaki Y, Kondo A, Okamoto R, Inoue T,
Konishi K, Hayashi A, Tsuji Y, Fujii S and Ohno K: Clinical
characteristics of acute encephalopathy of obscure origin: A
biphasic clinical course is a common feature. Neuropediatrics.
37:269–277. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Okanishi T, Mori Y, Kibe T, Takahashi Y,
Saito Y, Maegaki Y and Yokochi K: Refractory epilepsy accompanying
acute encephalitis with multifocal cortical lesions: Possible
autoimmune etiology. Brain Dev. 29:590–594. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sakuma H: Acute encephalitis with
refractory, repetitive partial seizures. Brain Dev. 31:510–514.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sakuma H, Awaya Y, Shiomi M, Yamanouchi H,
Takahashi Y, Saito Y, Sugai K and Sasaki M: Acute encephalitis with
refractory, repetitive partial seizures (AERRPS): A peculiar form
of childhood encephalitis. Acta Neurol Scand. 121:251–256. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wakamoto H, Takahashi Y, Ebihara T,
Okamoto K, Hayashi M, Ichiyama T and Ishii E: An immunologic case
study of acute encephalitis with refractory, repetitive partial
seizures. Brain Dev. 34:763–767. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Watanabe S, Okumura Y and Aiba H: A case
of acute encephalitis with refractory repetitive partial seizures
successfully controlled by very-high-dose phenobarbital therapy
found in a boy. No To Hattatsu. 46:443–446. 2014.(In Japanese).
PubMed/NCBI
|
|
12
|
Matsuzono K, Kurata T, Deguchi S,
Yamashita T, Deguchi K and Abe K: Ketogenic diet therapy is
effective in encephalitis with refractory seizures. Neurol Res.
36:906–910. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shyu CS, Lee HF, Chi CS and Chen CH: Acute
encephalitis with refractory, repetitive partial seizures. Brain
Dev. 30:356–361. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lin JJ, Lin KL, Wang HS, Hsia SH and Wu
CT: Effect of topiramate, in combination with lidocaine and
phenobarbital, in acute encephalitis with refractory repetitive
partial seizures. Brain Dev. 31:605–611. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Specchio N, Fusco L, Claps D and Vigevano
F: Epileptic encephalopathy in children possibly related to
immune-mediated pathogenesis. Brain Dev. 32:51–56. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Dahaba AA, Liu DW and Metzler H:
Bispectral index (BIS) monitoring of acute encephalitis with
refractory, repetitive partial seizures (AERRPS). Minerva
Anestesiol. 76:298–301. 2010.PubMed/NCBI
|
|
17
|
Ismail FY and Kossoff EH: AERRPS, DESC,
NORSE, FIRES: Multi-labeling or distinct epileptic entities?
Epilepsia. 52:e185–e189. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Fukuyama T, Inaba Y, Higuchi T, Sekiguchi
Y and Ishida S: A case of sudden unexpected death in epilepsy 3
years after the onset of acute encephalitis with refractory,
repetitive partial seizures. No To Hattatsu. 43:313–316. 2011.(In
Japanese). PubMed/NCBI
|
|
19
|
Hufnagel A, Burr W, Elger CE, Nadstawek J
and Hefner G: Localization of the epileptic focus during
methohexital induced anthesia. Epilepsia. 33:271–284. 1992.
View Article : Google Scholar : PubMed/NCBI
|