Introduction
Indirect inguinal hernia (IIH) is the most common
disease in pediatric surgery with an incidence ranging from 1 to 5%
(1,2). In all cases of indirect hernia in
children, the condition manifests itself mainly by incarceration in
approximately 1/6 of all indirect inguinal cases (3).
Incarcerated IIH is very common in pediatric
emergency surgery. In cases with shorter incarceration time, no
obvious abdominal distension and no red or swollen scrotum and
groin area, of manual reduction were used. In cases with longer
incarceration time with red and swollen scrotum and groin area or
conditions of low intestinal obstruction and presence of bloody
stools in local scrotum, children required emergency surgery
instead of manual reduction. Several studies on the application of
laparoscopic surgery of incarcerated abdominal external hernia is
available (4–6).
With the advancements of laparoscopy in Chinese
pediatric surgery, we treated 64 cases of incarcerated IIH with
laparoscopic surgery at the Xuzhou Children's Hospital (Jiangsu,
China), and obtained better clinical effects compared with
traditional methods.
Materials and methods
General information
From January, 2012 to December, 2014, 64 children
were enrolled into the present study. These patients received
laparoscopic surgery at the Department of Pediatric Surgery, and we
reviewed their perioperative and postoperative follow-up studies.
There were 43 males and 21 females, aged 3 months to 6 years
(average, 2.1 years). The time of finding the groin mass ranged
from 9 to 68 h (average, 20.8 h). We had 33 cases of right side, 15
cases of left side and 16 cases of bilateral inguinal indirect
hernia with only one side incarceration. Clinical manifestations
included vomiting, paroxysmal crying in infants and complaining
about lower abdominal pain in preschoolers. Before surgery, the
children were examined using abdomen standing film to exclude
gastrointestinal perforation and ultrasonography of groin area was
performed to further confirm hernia contents.
Selection criteria used for the laparoscopic group
were: i) no bloody stools; ii) no obvious abdominal distension;
iii) generally in good condition to tolerate pneumoperitoneum; iv)
little or no red and swollen groin area; and v) preoperative
abdomen standing film with no gastrointestinal perforation,
abdominal ultrasound without many ascites.
The control group comprised 60 cases of children
treated with traditional surgery. Table
I shows the comparison between the two groups.
 | Table I.Comparison of the general information
between the two groups of children. |
Table I.
Comparison of the general information
between the two groups of children.
| Groups | n | Age (years) | Right side (n) | Left side (n) | Bilateral (n) | Male (n) | Female (n) | Cases of intestinal
necrosis (n) |
|---|
| Laparoscopic
group | 64 | 2.10±0.18 | 33 | 15 | 16 | 42 | 22 | 9 |
| Control group | 60 | 1.90±0.16 | 36 | 12 | 12 | 45 | 15 | 12 |
| t (χ2)
value |
| t=0.805 |
|
χ2=0.907 |
|
χ2=1.300 |
χ2=0.776 |
| P-value |
| 0.423 |
| 0.635 |
| 0.254 | 0.378 |
Study approval was provided by the ethics committee
of Xuzhou Children's Hospital. Written informed consent was
provided by the children's family and/or guardians.
Methods
Patients were placed in a supine position, lower
limbs were slightly outreached, and general anaesthesia was
performed with tracheal intubation. Longitudinal incision was
performed on the skin around the navel area to widen the navel
ring. Peritoneal incision was performed and a 5-mm trocar was
placed under direct vision to establish pneumoperitoneum (8-10-mm
Hg pressure, placed 30° laparoscope). Then a 3-mm deep incision on
the left-mid abdomen was performed and 3 mm grasping forceps were
placed. The operating table was adjusted to lower head higher feet
posture and the patient's affected side was elevated. At that
moment we could see clearly the internal ring of the affected side
and the intestine or uterus in females, with attachment hernia.
During surgery, patients received muscle relaxant and offered
manual reduction under direct vision. Hernia contents were
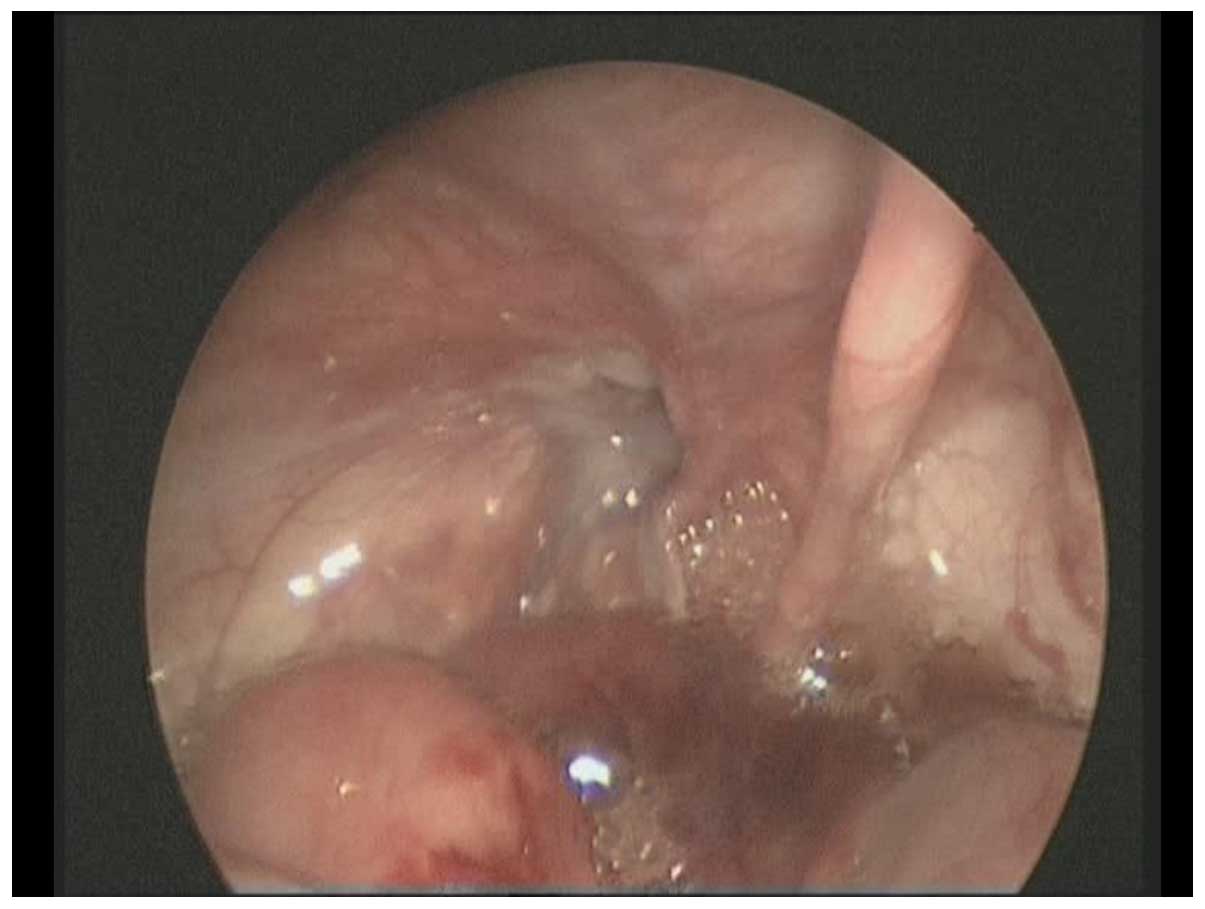
reconstructed in 44 cases successfully. In 13 cases we were not
able to put back the hernia contents. In those cases, at the
connection point of hernia blockage and abdominal wall, an incision
was performed at approximately 0.5 cm to the upper edge of the
hernia block. After mosquito vascular provoked anterior wall of the
inguinal canal, we incised approximately 0.2–0.4 cm. Consequently
we applied manual reduction under direct vision again and
reconstructed the intestine successfully (Fig. 1).
Internal ring closure method
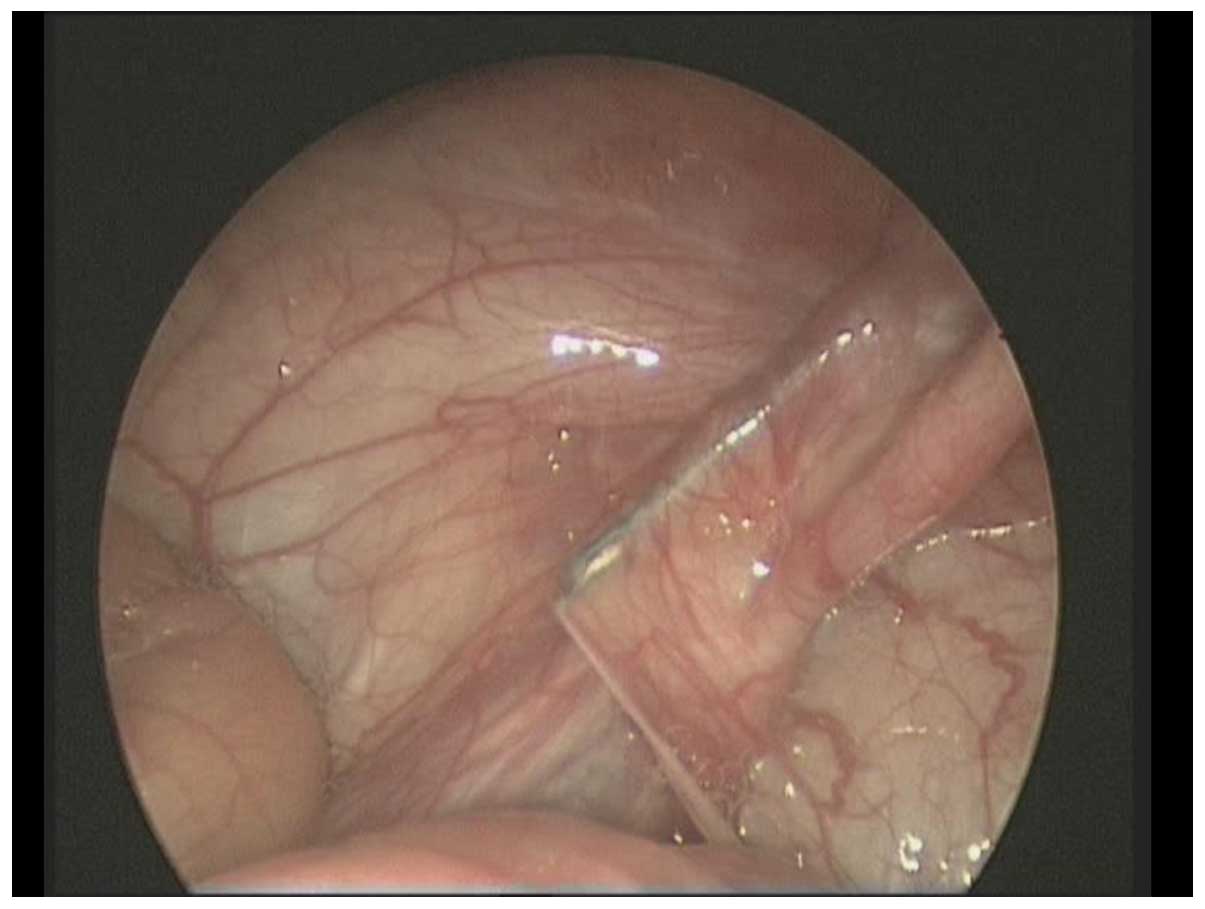
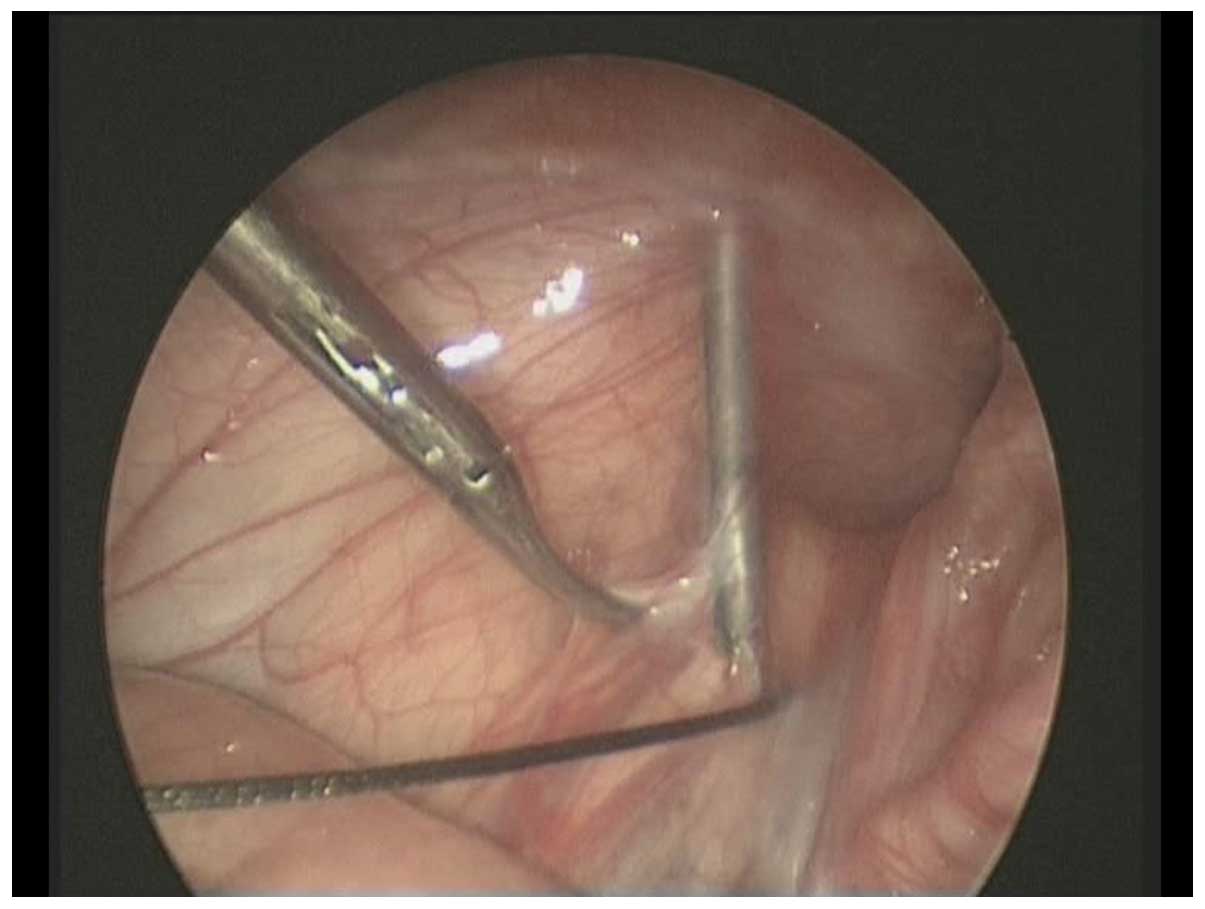
Percutaneous tissue was sutured with the epidural
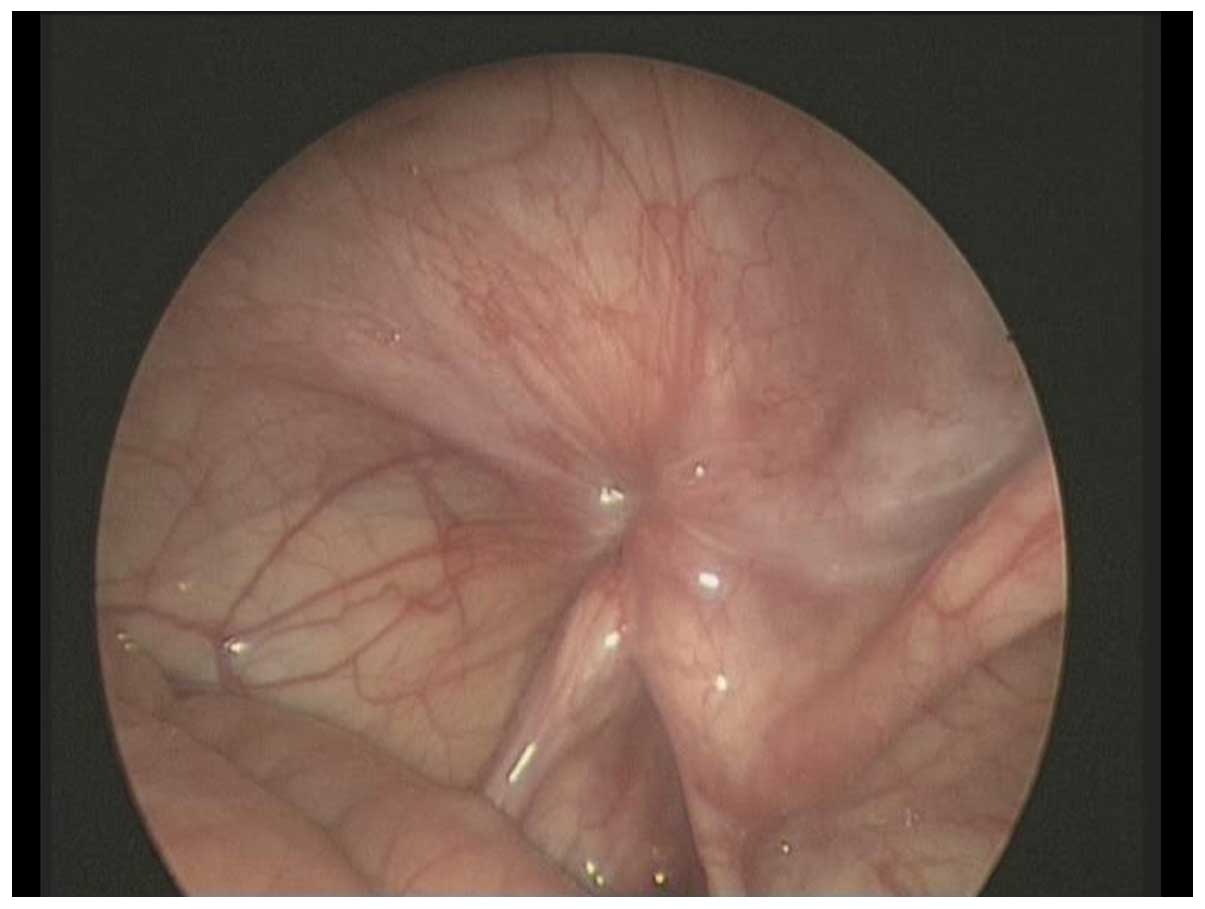
needle on both sides, inside (Fig.
2) and outside (Fig. 3) at the
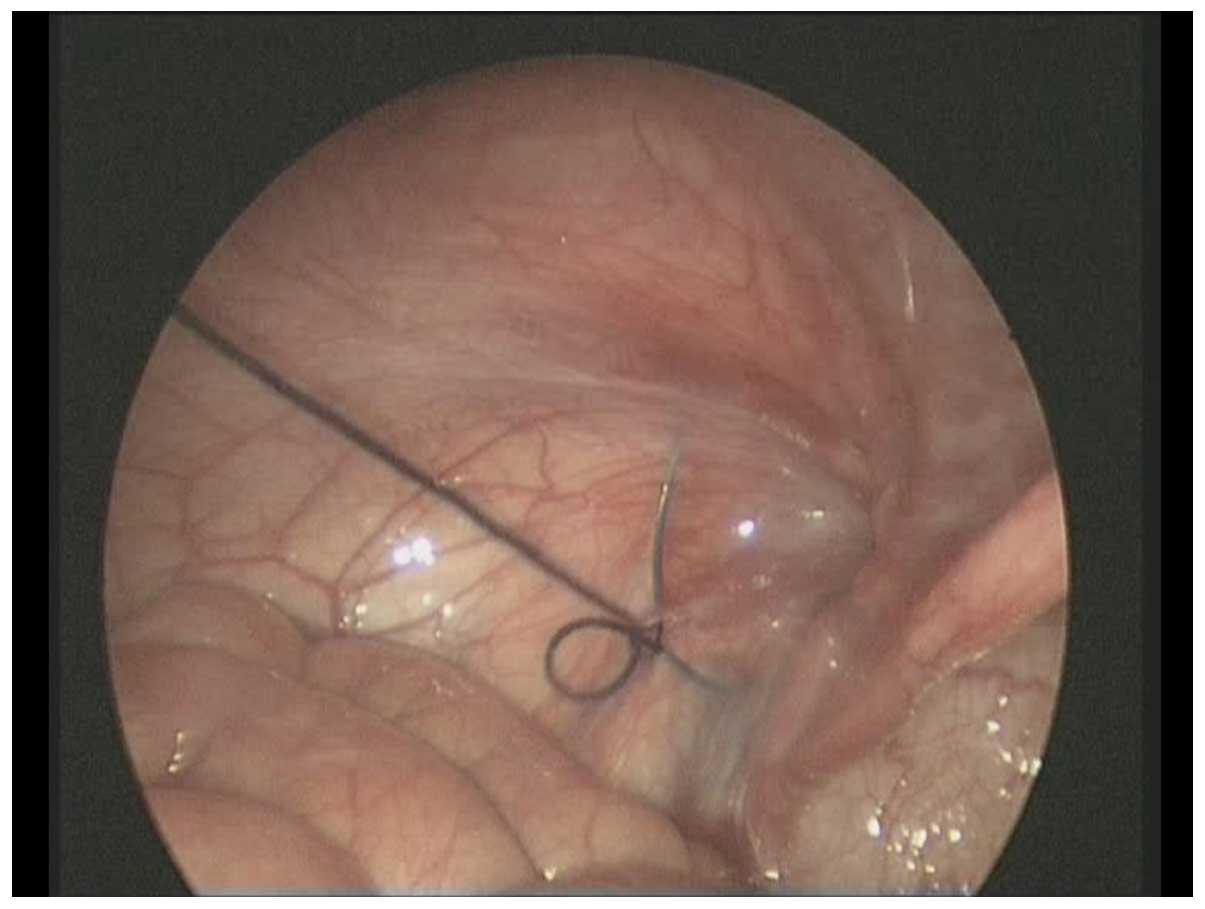
mouth of the inner ring and a single line and two-wire brought
through the pinhole. We used a two-wire loop to lead a single line
out of the body and ligated inner ring after making a knot
(Fig. 4). During the hernia ring
suturing process, we incised the inguinal canal's anterior wall and
passed two needles through the incised anterior wall of groin in
order to tighten the outer opening after making a knot (Fig. 5).
Small intestine necrosis processing
method
We expanded the navel incision and pulled the
necrotic bowel out of the abdominal cavity. Then we treated it with
resection and anastomosis after the closure of mesangial hole.
Intestine was then put back into abdominal cavity to re-establish
pneumoperitoneum (hernial sac ligation step was the same as
mentioned before). In the case of contralateral recessive hernia,
family members were consulted again during the operation in order
to obtain their consent for the surgery.
Postoperative treatment
Children without intestinal necrosis started
drinking small amounts of water 6 h after the operation. In the
absence of gastrointestinal reaction, children started liquid diet
and were discharged 1–3 days after operation. Children with chronic
intestinal necrosis fasted after operation and were treated with
gastrointestinal decompression for 3 days. They were fully
rehydrated at the same time. They gradually started liquid or
semliquid food after 3 days. They all received postoperative
anti-infection treatment for 3 to 5 days. Antibiotics were stopped
when no abnormal blood was observed and they were discharged 5–7
days after operation.
Statistical analysis
SPSS 13.0 statistical software (Chicago, IL, USA)
was used for statistical analyses. Data are presented as mean ± SD.
For comparison we used the t-test or χ2 test. P<0.05
showed statistically significant differences.
Results
The operation time in laparoscopic group ranged from
15 to 80 min (average, 41.5 min). Five cases suffered from mild
edema of scrotum after operation and 2 cases had inguinal
subcutaneous congestion. Symptoms disappeared after raising scrotum
and local physiotherapy. Postoperative length of stay ranged from 2
to 7 days (average, 3.2 days). All the patients were out-patients
and were followed up for 6 months to 1 year (average, 8.7 months),
there were no recurrence of indirect hernia in the group. No
concurrent hydrocele or testicular atrophy in male children was
observed.
The operation time of for control group ranged from
30 to 95 min (average, 53.9 min). After the operation, we had 38
cases with obvious edema of scrotum and three cases with wound
infection. Length of stay ranged from 4 to 7 days (average, 5.3
days) and they were followed-up to 6 months. We had 2 recurring
cases (males), who agreed to the second surgery, 3 and 6 months
after operation, respectively. For their second surgery we used the
laparoscopic hernia sac high ligation method. Sixty cases of
children were followed up from 6 months to 3 years (average, 1.5
years) and no secondary testicular atrophy or concurrent hydrocele
in male children was observed (Table
II).
 | Table II.Situation of perioperative period and
complications in the two groups. |
Table II.
Situation of perioperative period and
complications in the two groups.
|
|
|
|
| Postoperative
complications |
|---|
|
|
|
|
|
|
|---|
| Groups | n | Time of operation
(min) | Length of stay
(days) | Edema of scrotum
(n) | Recurrence (n) | Incision infection
(n) |
|---|
| Laparoscopic
group | 64 | 41.5±15.9 | 3.3±1.79 | 5 | 0 | 0 |
| Control group | 60 | 53.9±13.8 | 5.3±1.08 | 38 | 2 | 3 |
| t (χ2)
value |
| t=−4.630 | t=−7.892 |
|
χ2=17.086 |
|
| P-value |
| <0.001 | <0.001 |
| <0.001 |
|
Discussion
Pediatric incarcerated IIH is a common emergency
treatment in pediatric surgery (mostly in infants). Many children
have this condition for a long time before visiting a doctor. This
can reduce the chance of a successful manual reduction and leads
the medical team to opt for surgery. Traditional release of
incarcerated hernia surgery needs to dissect the inguinal canal
therefore the probability of postoperative complications, such as
edema of scrotum, hematoma, indirect hernia recurrence is high.
This method of surgery requires a 2-3-mm operation incision.
Laparoscopic surgery for inguinal hernia has been carried out for
many years. This method has several advantages compared with the
traditional method. Among the advantages are the small operation
incision, small intraoperative injury, fast procedure and
efficient, quick recovery with minimal impact on the patients'
reproductive system (7). There are
several studies (8–10) on performing laparoscopic technology
for pediatric incarcerated IIH. Since 2011, our hospital has
carried out two holes approach laparoscopic surgery treatment for
incarcerated IIH and obtained satisfactory results. In the
laparoscopic group we obtained better results compared to the
control group. In the observation group, the operation time and
length of stay was shorter while the incidence of postoperative
complications was much lower compared with the control group.
Laparoscopic surgery treatment for incarcerated IIH
offered several advantages: i) during the operation under
anesthesia we supplied muscle relaxants; ii) after the reduction
was carried out, we were able to directly observe the
revascularization of hernia contents; and iii) in the case of no
intestine necrosis, we obtained recovery almost as in the case of
ordinary laparoscopic inguinal hernia surgery. The recurrence rate
of laparoscopic incarcerated hernia surgery is usually lower than
that of traditional surgery (5), and
we obtained the same type of results in the present study. In
traditional surgery, under anesthesia, the return of hernia
contents can be a serious problem for the surgeon, because it is
difficult to explore the abdominal inner intestine through groin
incision. Some Chinese doctors have reported good results using
laparoscopic monitoring on children with failed manual reduction
surgeries. They used grasping forceps to lead downward or adopting
electric hook or scalpel to incise the inner mouth in the abdominal
cavity (11). This method had the
risk of avulsion of intestinal serosa or injury of edema intestinal
near the inner mouth. We used the approach of opening part of the
front wall of the inguinal canal through abdominal stripe incision,
which could turn back the intestine quickly and reduce the damage
for hernia contents because of reset force. For treating the inner
mouth after turning hernia contents were returned, we used epidural
needle with thread method. This was conducted easily and added no
extra financial burden on the families. This approach may be
appropriate for underdeveloped and poor regions. The results
revealed that our method did not increase the risk of postoperative
recurrence, and did not need any extra equipment.
In conclusion, compared with traditional surgery,
laparoscopic surgery in pediatric incarcerated IIH has numerous
advantages, such as fast reduction, small damage, short time of
operation and length of stay, and certain clinical application
value.
References
|
1
|
Wiener ES, Touloukian RJ, Rodgers BM,
Grosfeld JL, Smith EI, Ziegler MM and Coran AG: Hernia survey of
the Section on Surgery of the American Academy of Pediatrics. J
Pediatr Surg. 31:1166–1169. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kapur P, Caty MG and Glick PL: Paediatric
hernias and hydroceles. Pediatr Clin North Am. 45:773–789. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mackinnon AE: Hernia and
hydrocelePediatric Surgery. 32. Atwell JD: Arnold; London: pp.
309–312. 1998
|
|
4
|
Saggar VR and Sarangi R: Endoscopic
totally extraperitoneal repair of incarcerated inguinal hernia.
Hernia. 9:120–124. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hoffman A, Leshem E, Zmora O, Nachtomi O,
Shabtai M, Ayalon A and Rosin D: The combined laparoscopic approach
for the treatment of incarcerated inguinal hernia. Surg Endosc.
24:1815–1818. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ferzli G, Shapiro K, Chaudry G and Patel
S: Laparoscopic extraperitoneal approach to acutely incarcerated
inguinal hernia. Surg Endosc. 18:228–231. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Endo M, Watanabe T, Nakano M, Yoshida F
and Ukiyama E: Laparoscopic completely extraperitoneal repair of
inguinal hernia in children: a single-institute experience with
1,257 repairs compared with cut-down herniorrhaphy. Surg Endosc.
23:1706–1712. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tatli D and Numanoglu KV: Transverse
testicular ectopia associated with incarcerated inguinal hernia: a
case report. Cases J. 1:2002008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kaya M, Hückstedt T and Schier F:
Laparoscopic approach to incarcerated inguinal hernia in children.
J Pediatr Surg. 41:567–569. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nah SA, Giacomello L, Eaton S, de Coppi P,
Curry JI, Drake DP, Kiely EM and Pierro A: Surgical repair of
incarcerated inguinal hernia in children: laparoscopic or open? Eur
J Pediatr Surg. 21:8–11. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bin S, Hui W and Yang P: Laparoscopic high
ligation of hernial sac for the treatment of 18 cases with inguinal
incarcerated hernia in Chinese. J Minim Invasive Surg. 13:84–86.
2013.
|