Introduction
Double gallbladder is a biliary anomaly with an
incidence of 1 case per 3,800–4,000 patients (1). It is typically not diagnosed
preoperatively, but is incidentally identified intraoperatively
(2). However, this condition may be
missed during the surgery and diagnosed during a postoperative
endoscopic retrograde cholangio-pancreatography examination
performed for persistent biliary symptoms (3,4). In
order to avoid intraoperative injury, open-surgery is a common
treatment strategy. Gorecki et al (5) reported a case of double gallbladder
originating from the left hepatic duct during a laparoscopic
surgery, which was then converted to an open procedure due to the
absence of the accessory cystic duct. However, this surgical
procedure results in several risks. Therefore, the present study
suggests the importance of double gallbladder diagnosis to avoid
complications and careful surgery to complete the laparoscopic
surgery.
The current study describes a case of a manifestly
complex inflammatory double gallbladder in a 66-year-old woman with
secondary common bile duct (CBD) stones. A laparoscopic
choledochoscopy were performed to explore and remove a common bile
duct stone through the cystic duct without using a T-tube, and the
gallbladder was surgically removed. To the best of our knowledge,
this is the first of such cases to be reported in the English
language. It is safe and feasible to identify the anatomical
association, move the gallbladder and explore the entire biliary
duct through the use of laparoscopic choledochoscopy without
postoperative complications.
Case report
The patient was a 66-year-old woman with whose
primary complaint was intermittent epigastric and right upper
quadrant pain, which she had experienced for ~3 years. The episodes
did not involve fever or jaundice and relieved by anti-inflammatory
treatment with ceftazilime (Hainan HaiLing Chemical Pharmaceutical
Co., Ltd., Hainan, China; 2 g twice a day, by intravenous drip).
The episodes were frequent, with the pain experienced by the
patient upon admission to hospital presenting in the upper abdomen
and right upper quadrant for >1 month without fever or jaundice.
The patient presented with physical weakness and a lack of
appetite, and brown feces and pale yellow urine were observed. Upon
admission to the Beijing Tiantan Hospital (Beijing, China) in April
2014, the patient had a body temperature of 36.5°C and a heart rate
of 70 bpm without systemic lymph node enlargement or jaundice of
the skin or sclera. There was no evidence of anemia. Her abdomen
was flat, and the right upper quadrant showed mild tenderness with
no rebound tenderness or muscle tension. Murphy's sign and liver
percussion pain assessments were negative. Laboratory tests
revealed a normal white blood cell (WBC) count. The amylase, urea,
electrolyte and liver function assessments were normal; the total
bilirubin level was 12.5 µmol/l (normal range, 5.1–19.0 µmol/l),
and the direct bilirubin level was 3.2 µmol/l, indicating that
neither level was elevated. An abdominal B-scan ultrasound revealed
a double cavity in the gallbladder region with a thickened wall
with a rough surface. A 1.7 cm hyperechoic mass was observed in one
capsule and had an acoustic shadow behind it, which was removable.
The extrahepatic bile duct was widened, and the diameter at the
widest point was ~1.2 cm. In addition, a stone was present in the
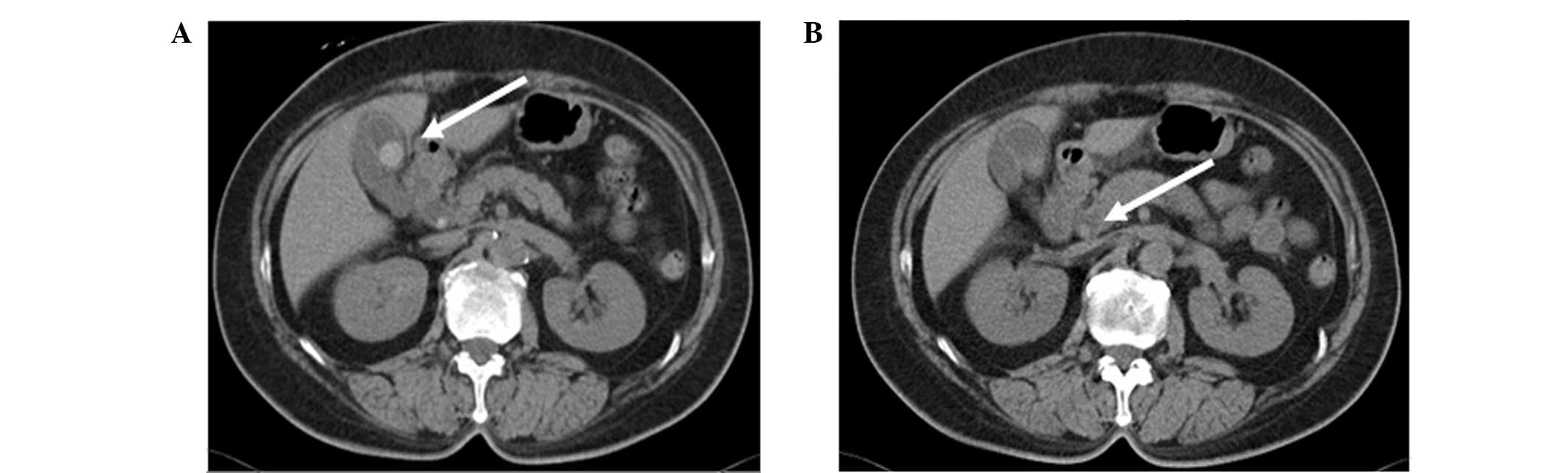
CBD. An abdominal computed tomography scan revealed that the double
gallbladder walls were thickened, and a stone with clear boundaries
was observed. The choledochectasia had a diameter of 1.4 cm, and a
stone with a diameter of 0.4 cm was detected in the CBD (Fig. 1). The magnetic resonance
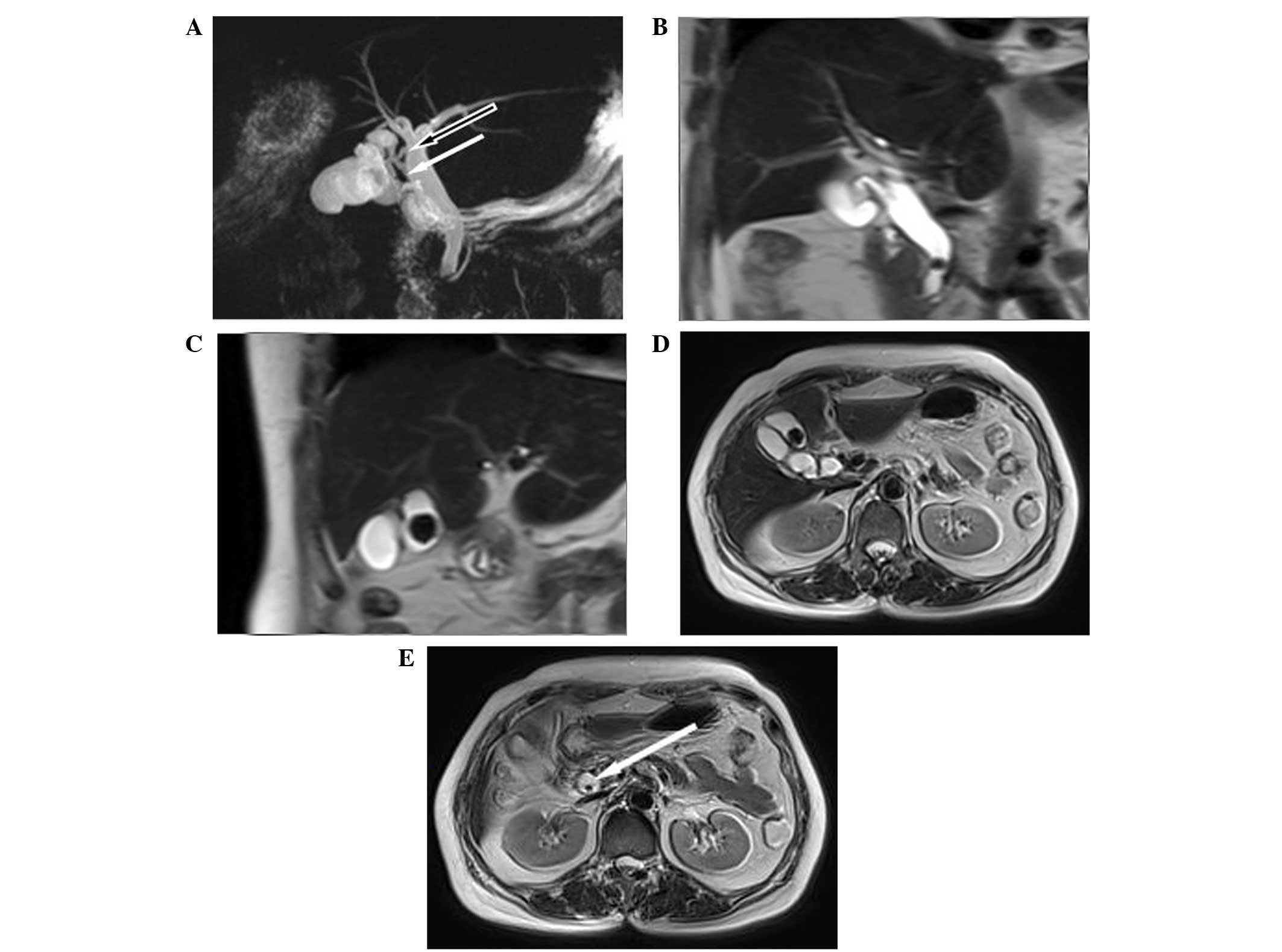
cholangiopancreatography (MRCP) findings were as follows: A
dual-chamber gallbladder; choledochectasia; gallstones with
cholecystitis; and common bile duct stones (Fig. 2). A laparoscopic cholecystectomy (LC)
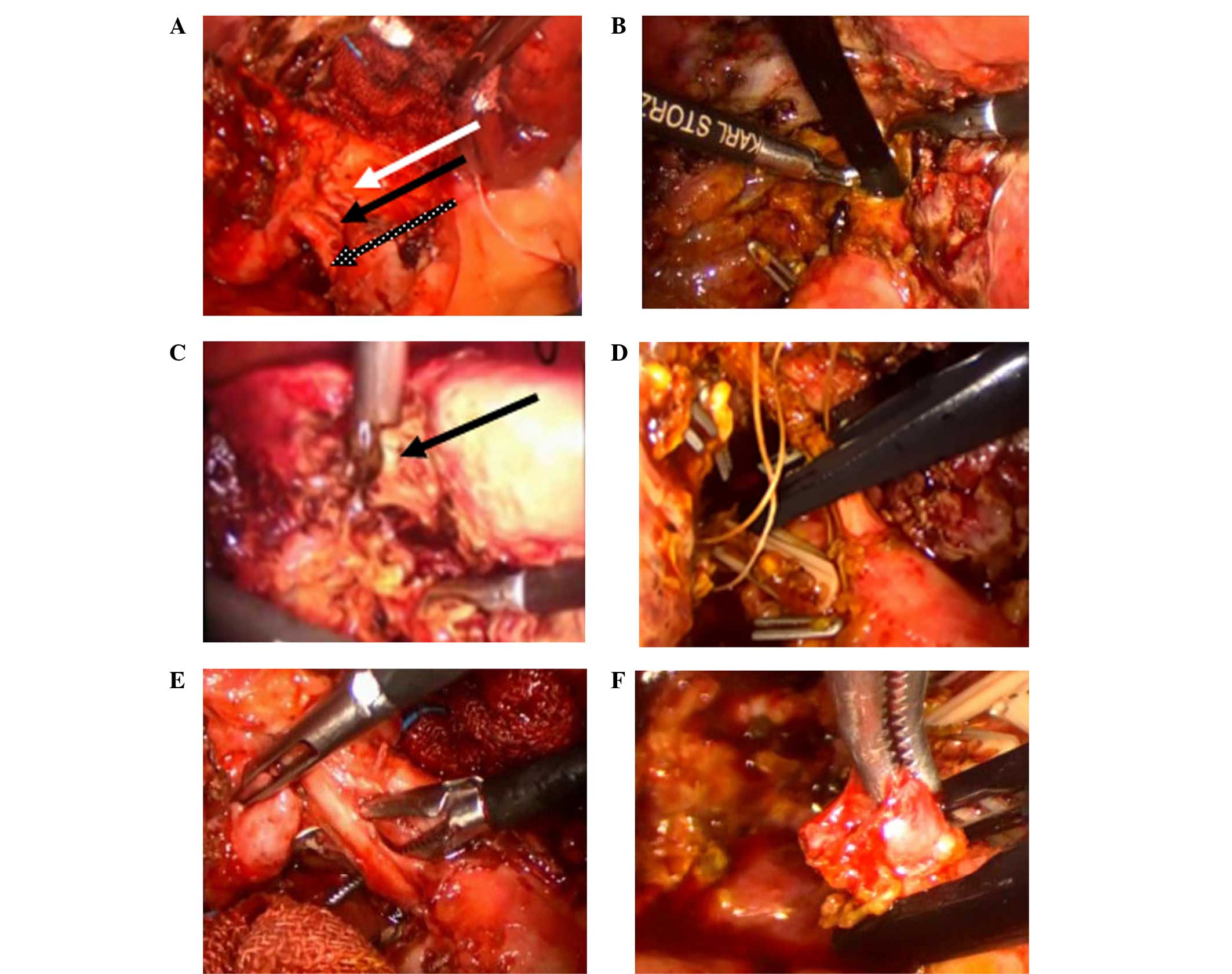
was performed in April 2014. Fibrosis from chronic inflammation
caused surgical difficulties. A retrograde resection was performed.
Dissection of Calot's triangle was carefully performed, and two
cystic ducts and one cystic artery were readily distinguished. Two
cystic ducts were separately connected to the CBD (Fig. 3). A micro-incision was performed
through the anterior wall of the second cystic duct and the point
of connection to the CBD, and the choledochoscope was inserted and
the stone was removed (Fig. 3). The
second cystic duct was sutured without the use of a T-tube, and
Tyco (Medtronic Inc., Minneapolis, MN, USA) absorbable clips were
fixed upon it. The cystic artery and the first cystic duct were set
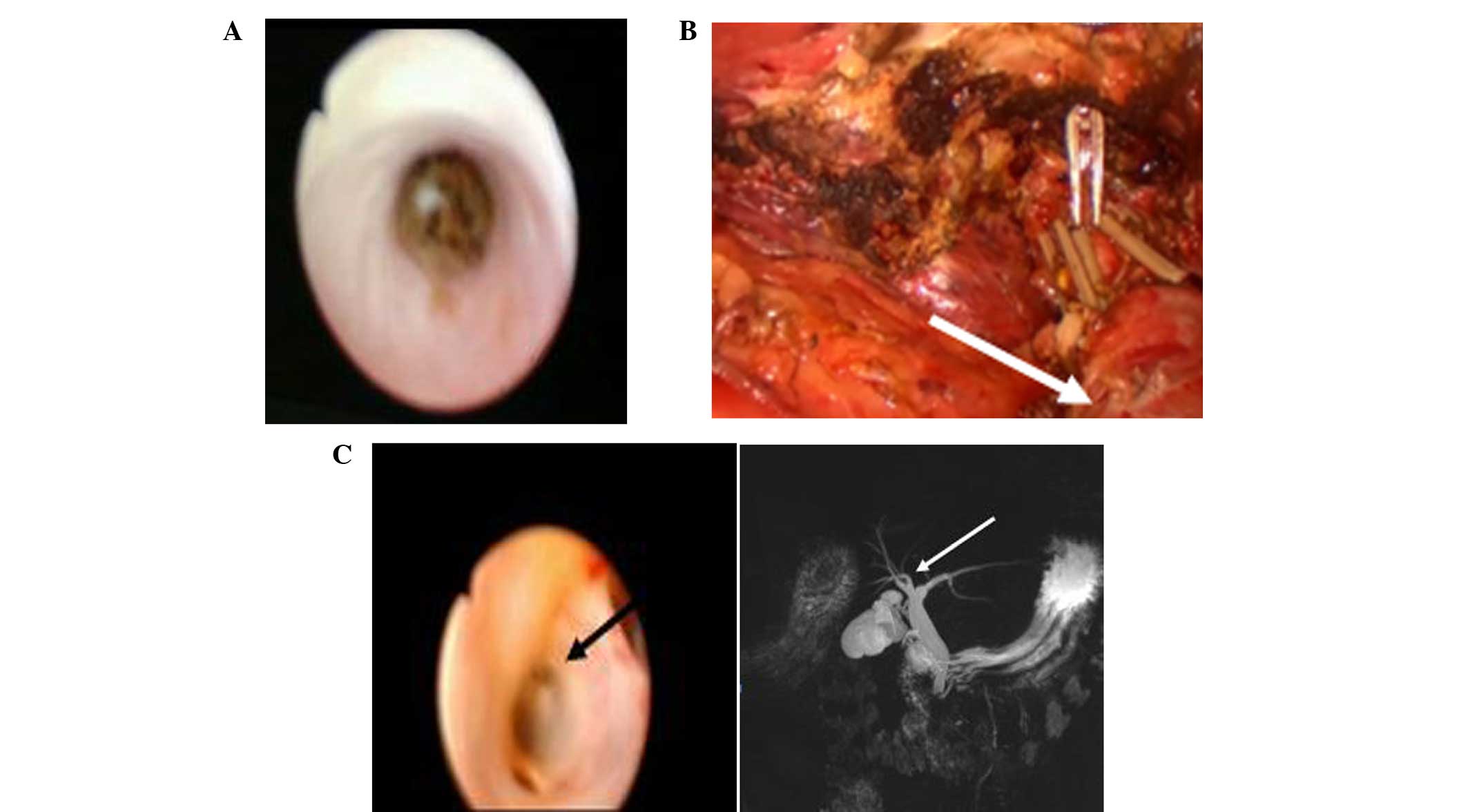
on Tyco absorbable clips separately (Fig. 3). Exploration by choledochoscopy
during LC surgery confirmed that the lumen structure was consistent
with the results of MRCP. No residual stones were identified and
the cystic structure remained unchanged (Fig. 4).
A number of postoperative conditions were noted.
There was 50 ml peritoneal drainage from the gallbladder fossa
after 16 h on the first day, and the drainage fluid was pale and
contained blood. No bile was observed. The drainage fluid during
the subsequent 24 h amounted to 20 ml. The patient did not
experience any pain, and her body temperature remained normal. The
laboratory test results 16 h post-surgery showed that the WBC count
was 18.61×109/l, which decreased to normal levels
without the administration of anti-inflammatory therapies. The
alanine transaminase (normal range, 0.0–41.0 IU/l) and aspartate
aminotransferase (normal range, 0.0–42.0 IU/l) levels were 99.5
IU/l and 127 IU/l, respectively. Glutathione (Shandong Green Leaf
Pharmaceutical Co., Ltd., Yantai, China) was administered once
postoperatively (1.2 g; intravenous drip) to preserve the function
of the liver, which recovered rapidly. The total bilirubin and
direct bilirubin levels were 16.5 µmol/l and 5.3 µmol/l,
respectively. Two days post-surgery, the patient began a liquid
diet and was discharged the following day.
The microscopic image of the double gallbladder
showed chronic cholecystitis. Previous studies concerning double
gallbladder cases associated with conditions other than
cholecystitis and gallstones have shown laparoscopic surgery
results (Table I) (5–16).
 | Table I.Cases of laparoscopic surgery of
double gallbladder associated with circumstances other than
cholecystitis and gallstones. |
Table I.
Cases of laparoscopic surgery of
double gallbladder associated with circumstances other than
cholecystitis and gallstones.
| First author | Year | Associated
circumstance | Preoperative
diagnosis | Second surgery
required | Intraoperative
complications | Ref. |
|---|
| Gorecki | 1998 | Originated from the
left hepatic duct | Y | N | Conversion to OC | (5) |
| Weibel | 2001 | Originated from the
right hepatic duct | Y | Y | Conversion to OC | (6) |
| Schroeder | 2003 | Triple
gallbladder | Y | N | N | (7) |
| Ohtani | 2003 | Cholelithiasis
adenomyomatosis | Y | N | N | (8) |
| Papaziogas | 2005 | Two separate cystic
ducts connected through an ostium | N | N | Conversion to OC | (9) |
| Sasaki | 2005 | Double gallbladder
(duodenal type) | Y | N | N | (10) |
| Vijayaraghavan | 2006 | Pyocoele acute
cholecystitis and cystadenoma | N | N | N | (11) |
| Singh | 2006 | Accompanied by
jaundice | Y | Y | N | (12) |
| Lefemire | 2009 | Neuroma of a double
gallbladder | Y | Y | N | (13) |
| Walbolt | 2011 | Accompanied by
gallstone pancreatitis | Y | N | N | (14) |
| Ghosh | 2014 | Accompanied by dual
pathology | Y | N | N | (15) |
| Giakoustidis | 2014 | Ciliated foregut cyst
of the gallbladder | Y | N | N | (16) |
| Present case | 2014 | Common duct
stones | Y | N | N | – |
Written informed consent was obtained from this
patient prior to participation into the present study.
Discussion
Two cases of double gallbladders have been reported
among 9,921 autopsy cases (0.02%), and 3 cases have been reported
out of a total of 9,970 cases (0.03%) in a radiographic survey
(1). Double gallbladders are
classified according to Boyden's classification (1), which is the most widely used. The two
primary duplication types consist of bi-lobed gallbladders and true
duplications, the latter of which involves two separate cystic
ducts. The true duplication type is subclassified into H- and
Y-shaped types. The H-shaped subtype involves two separate cystic
ducts that separately enter into the CBD, whereas the Y-shaped type
describes two cystic ducts that are adjoined prior entering the
CBD. The reconstruction image obtained by MRCP indicated a complete
(true) duplication of the gallbladder of the H-shaped type. The
technology currently available facilitates the generation of clear
preoperative anatomical images that provide anatomical details
during surgery that could enable the prevention of intraoperative
damage to the biliary duct, otherwise the double gallbladder may be
missed (17).
Double gallbladder abnormalities are typically
associated with gallstones and cholecystis, with sporadic reports
of other anomalies. Kawanishi et al (18) reported a double gallbladder with an
adenocarcinoma originating in the left hepatic duct. Nayak et
al (17) reported a case
concerning a double gallbladder completely enclosed in a
cystogastric peritoneum fold. In addition, Ghosh (15) reported the case of a laparoscopic
cholecystectomy of a double gallbladder with dual pathology, whilst
Vijayaraghavan and Belagavi (11)
reported a double gallbladder with different disease entities.
Lefemine and Lazim (13) reported a
double gallbladder neuroma. Papaziogas et al (9) reported a gallbladder with two chambers
with separate cystic ducts, which communicated through an ostium,
with both chambers containing multiple gallstones. However, a
double gallbladder associated with CBD stones, particularly a case
treated by laparoscopic surgery, has rarely been reported in
previous studies (Table I) (5–16). The
authors of the present study hypothesize that the H-shaped subtype
(according to Boyden's classification) double gallbladders are more
likely to form common bile duct stones. The possibility of
gallstones migrating into the biliary tract would increase, and the
hydrodynamics within the bile duct may have changed, leading to the
formation of a vortex, and a minimal bile duct obstruction could
result in a mild infection. Subsequently, the infection would then
accelerate the formation of primary or secondary bile pigment
stones as well as cholesterol-mixed stone pieces.
Double gallbladders associated with other anomalies
present increased difficulties in cholecystectomies, and involve
postoperative complications. A review of the studies published in
English identified 13 laparoscopically-managed cases (13). The majority of cases did not require
conversion to an open cholecystectomy (Table I). Goel et al (19) and Ozmen et al (20) have reported the use of laparoscopic
treatment for a double gallbladder. For such rare variants, a
complete analysis of the imaging data and patient intraoperative
separation are necessary prior to the removal of any pipeline
during LC surgery. In cases with the H-shaped subtype, the
possibility of injury to the bile duct and hepatic artery is high
(21). In the present case, the LC
was successfully completed, despite the coexistence of acute and
chronic cholecystitis. Thus, the present results indicate that the
laparoscopic surgeon may not need to convert these cases to open
procedures, and that the standard 4-port technique may suffice.
Laparoscopic magnification provided a clear image of the details of
Calot's triangle, and by performing a detailed blunt dissection of
Calot's triangle with a layer-by-layer thinning procedure, the
pipeline structure was able to be clearly separated (Fig. 3). Therefore, as in the present study,
a retrograde resection should be applied and the gallbladder should
be opened, when necessary, to confirm the location of the cystic
duct from the cavity.
Choledochoscopy in LC surgery for a double
gallbladder associated with CBD stones has unique advantages. In
the current study, the second cystic duct (the upper branch) was
utilized during surgery. The choledochoscope is inserted into the
CBD at an almost right angle through the cystic duct, particularly
in the upper part of the CBD. It is easier to directly enter and
observe the intrahepatic bile duct branches and proximal residual
stones than the lower cystic duct (Fig.
3), followed by removal of the remote stones (Fig. 4). The first cystic duct (the lower
branch) is a reserve pathway. Choledochoscopy confirmed that the
cavity structure in the proximal biliary was in complete accordance
with that of the preoperative MRCP image (Fig. 4). In the present study, it was
evident that there was no residual cystic structure on the right
side of the CBD following the removal of the double gallbladder
(Fig. 4). Thus, choledochoscopy is
able to serve the same role as the operative cholangiography.
In conclusion, a double gallbladder associated with
common duct stones is highly rare. It is safe and feasible to
perform a meticulous laparoscopic dissection and removal of a
double gallbladder, in addition to an exploration of the common
duct for the removal of choledochoscopic stones following a
micro-incision at the anterior wall of the cystic duct, with a
primary suture of the cystic duct.
References
|
1
|
Boyden EA: The accessory gallbladder-an
embryological and comparative study of aberrant biliary vesicles
occurring inman and domestic mammals. Am J Anast. 38:177–231. 1926.
View Article : Google Scholar
|
|
2
|
García J Cueto, Weber A, Serrano Berry F
and Tanur Tatz B: Double gallbladder treated successfully by
laparoscopy. J Laparoendosc Surg. 3:153–155. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Heinerman M, Lexer G, Sungler P, Mayer F
and Boeckl O: Endoscopic retrograde cholangiographic demonstration
of a double gallbladder following laparoscopic cholecystectomy.
Surg Endosc. 9:61–62. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Silvis R, van Wieringen AJ and van der
Werken CH: Reoperation for a symptomatic double gallbladder. Surg
Endosc. 10:336–337. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Gorecki PJ, Andrei VE, Musacchio T and
Schein M: Double gallbladder originating from left hepatic duct: a
case report and review of literature. JSLS. 2:337–339.
1998.PubMed/NCBI
|
|
6
|
Weibel D, Kaufmann M and Riedtmann-Klee
HJ: Accessory gallbladder originating from the right hepatic duct.
Surg Endosc. 15:5192001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Schroeder C and Draper KR: Laparoscopic
cholecystectomy for triple gallbladder. Surg Endosc. 17:13222003.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ohtani Y, Tobita K, Dowaki S, Sugio Y,
Kashiwagi H, Tucker A and Makuuchi H: Duplicate gallbladder
diagnosed with endoscopic retrograde cholangiopancreatography and
treated with laparoscopic cholecystectomy. Dig Endosc. 15:69–71.
2003. View Article : Google Scholar
|
|
9
|
Papaziogas B, Lazaridis C, Paraskevas G,
Koutelidakis J, Katsinelos P, Oikonomou B, Chatzimavroudis G,
Grigoriou M and Atmatzidis K: A variant of the double gallbladder.
A possible cause of cholelithiasis? Folia Morphol (Warsz).
64:229–232. 2005.
|
|
10
|
Sasaki A, Yoshida T, Kakisako K, Ohta M,
Shimoda K and Kitano S: Laparoscopic cholecystectomy for a double
gallbladder of the duodenal type. Surg Laparosc Endosc Percutan
Tech. 15:355–358. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Vijayaraghavan R and Belagavi CS: Double
gallbladder with different disease entities: A case report. J Minim
Access Surg. 2:23–26. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Singh B, Ramsaroop L, Allopi L, Moodley J
and Satyapal KS: Duplicate gallbladder: An unusual case report.
Surg Radiol Anat. 28:654–657. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lefemine V and Lazim TR: Neuroma of a
double gallbladder: A case report. Cases J. 2:112009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Walbolt TD and Lalezarzadeh F:
Laparoscopic management of a duplicated gallbladder: A case study
and anatomic history. Surg Laparosc Endosc Percutan Tech.
21:e156–e158. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ghosh SK: Laparoscopic cholecystectomy in
double gallbladder with dual pathology. J Minim Access Surg.
10:93–96. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Giakoustidis A, Morrison D, Thillainayagam
A, Stamp G, Mahadevan V and Mudan S: Ciliated foregut cyst of the
gallbladder. A diagnostic challenge and management quandary. J
Gastrointestin Liver Dis. 23:207–210. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nayak SB, Shetty SD, Surendran S, Jetti R,
Kumar N and Sirasanagandla SR: Double gallbladder completely
enclosed in a cystogastric fold of peritoneum. Anat Cell Biol.
47:132–134. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kawanishi M, Kuwada Y, Mitsuoka Y, Sasao
S, Mouri T, Takesaki E, Takahashi T, Toyota K and Nakatani T: A
case of double gallbladder with adenocarcinoma arising from the
left hepatic duct: A case report and review of the literature.
Gastroenterol Res Pract. 2010:pii:7219462010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Goel A, Srivastava KN and Rana AK: Double
gallbladder-a laparoscopic management. Surg Laparosc Endosc
Percutan Tech. 13:348–349. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ozmen V, Gorgun E, Unal ES, Polat C and
Ozmen T: Laparoscopic treatment of a bilobed gallbladder: A case
report and review of the literature. Surg Laparosc Endosc Percutan
Tech. 13:345–347. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hishinuma M, Isogai Y, Matsuura Y, Kodaira
M, Oi S, Ichikawa N, Kosukegawa M and Kuriki K: Double gallbladder.
J Gastroenterol Hepatol. 19:233–235. 2004. View Article : Google Scholar : PubMed/NCBI
|