Introduction
Acute fibrinous and organizing pneumonia (AFOP) is a
rare lung disease that was first reported in the year 2002
(1). The distinctive
histopathological characteristics of AFOP are intra-alveolar fibrin
deposits and associated organizing pneumonia, but without the
classical hyaline membrane that is typically associated with
diffuse alveolar disease. As only a small number of cases of AFOP
have been reported to date, much ambiguity prevails over the
clinical features, radiographic characteristics and prognoses of
AFOP. In the present study, a patient diagnosed with AFOP, based on
histopathological examination of a lung biopsy, is described. Based
on a review of literature pertaining to documented AFOP cases, a
summary of the clinical features, radiological characteristics,
treatment outcomes and prognoses associated with AFOP is
presented.
Case report
A 39-year-old male presented with a 10-day history
of high fever and cough with expectoration that was unresponsive to
empirical treatment for pulmonary bacterial infection (moxifloxacin
0.4 g daily for 5 days; Bayer, Leverkusen, Germany) in January 2014
at Nanjing General Hospital of Nanjing Military Command (Nanjing,
China). Serial chest computed tomography (CT) scans performed prior
to hospitalization revealed enlarging bilateral lung lesions. There
was no history of poisoning, exposure to dusty environmental
conditions, smoking or alcohol intake. At the time of admission,
the patient was looking ill, with slight dyspnea and pyrexia
(39.2°C). Laboratory investigations revealed a white blood cell
count of 4.6×109 cells/l [normal range (NR),
4–10×109 cells/l], differential neutrophil count of
68.6% (NR, 40–70%) and a C-reactive protein (CRP) level of 39.2
mg/l (NR, <10 mg/l) in blood. The clotting parameters were
normal. The blood biochemical indices were as follows: Alanine
aminotransferase 124 U/l (NR, <50 U/l), aspartate
aminotransferase 124 U/l (NR, <50 U/l), gamma-glutamyl
transferase 72 U/l (NR, <50 U/l), lactate dehydrogenase 779 U/l
(NR, 90–250 U/l) and creatinine 36 µmol/l (NR, 40–110 µmol/l). The
patient tested negative for human immunodeficiency virus. Arterial
blood gas analysis revealed PaCO2 28 mmHg,
PaO2 59 mmHg and pH 7.48 (FiO2, 40%). Sputum
culture yield was negative. Tests for autoantibody and
anti-Epstein-Barr virus, anti-mycoplasma and anti-influenza virus A
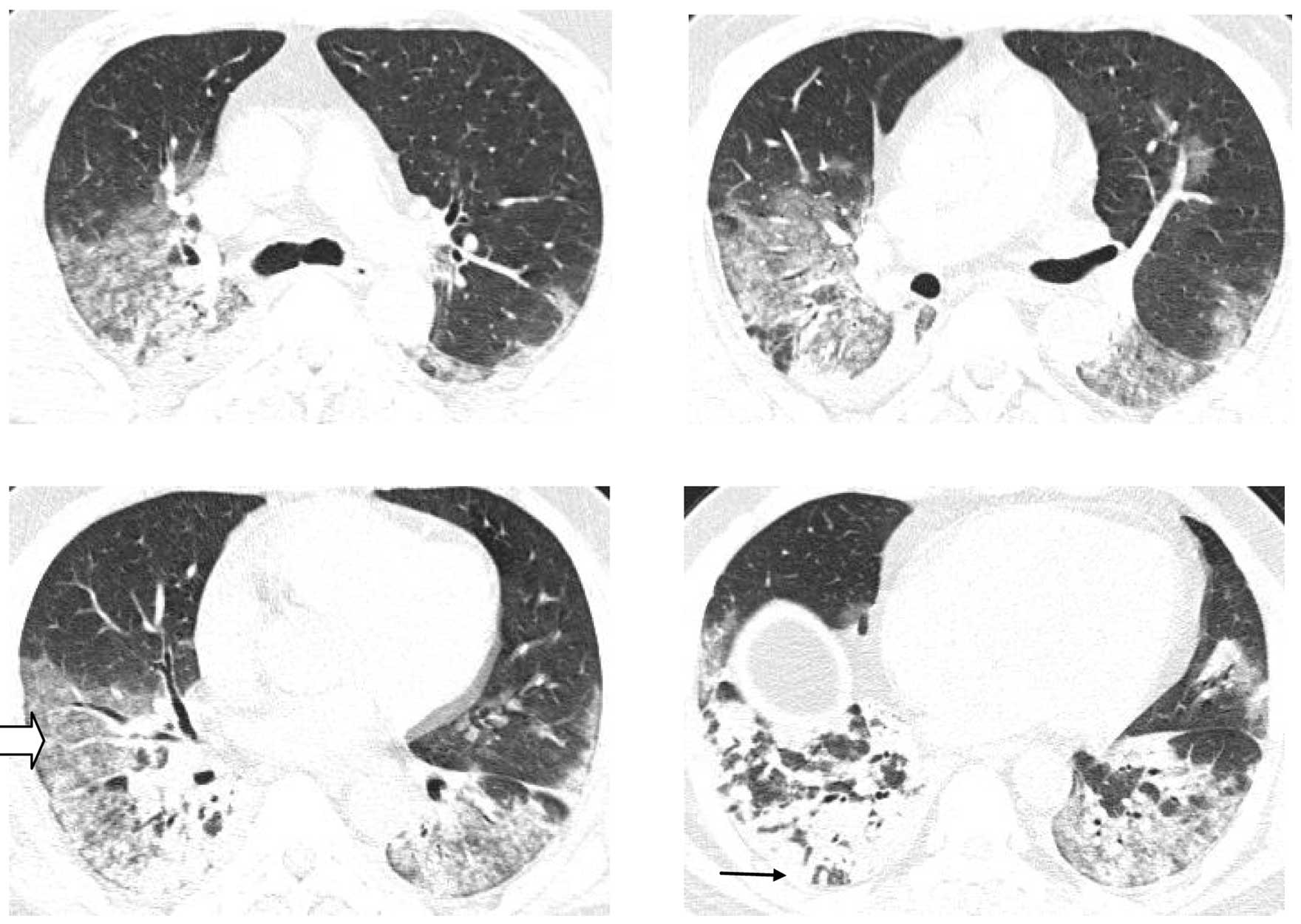
antibody were negative. Chest CT showed bilateral lung
consolidation, ground glass opacities and a small quantity of
bilateral pleural effusion (Fig. 1).
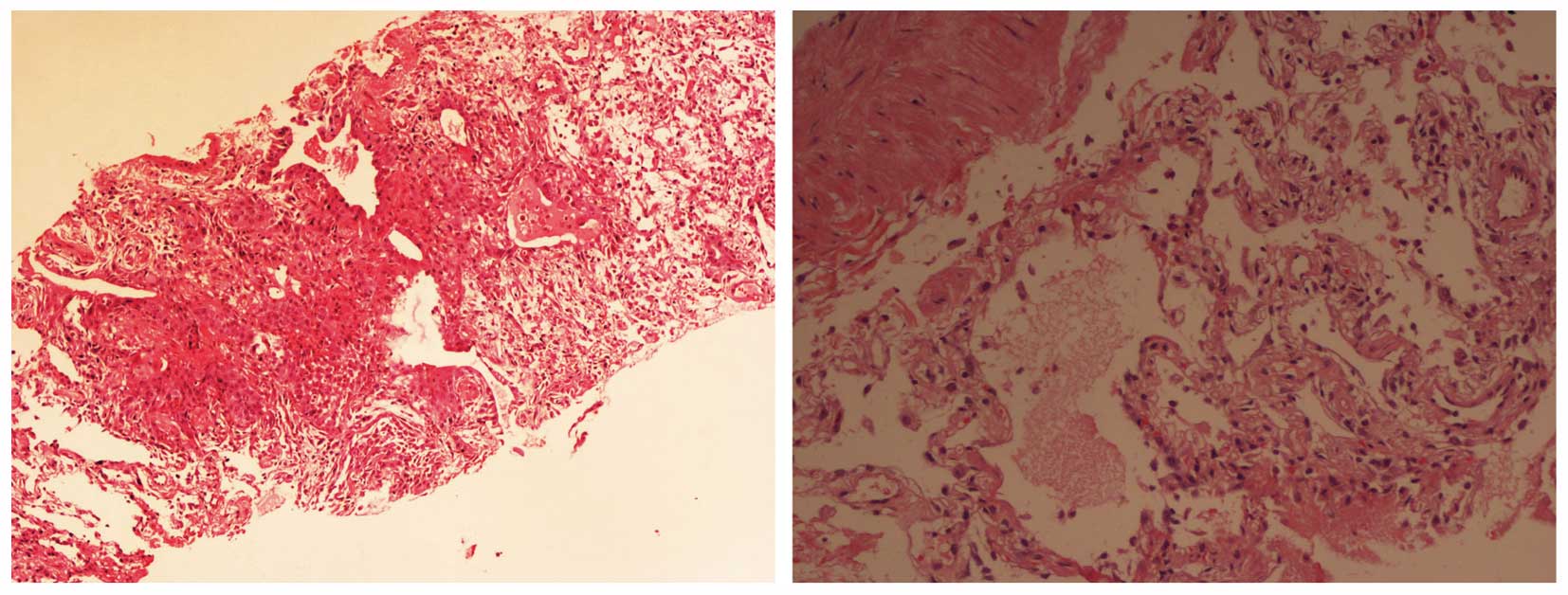
A pulmonary biopsy specimen from the lower lobe confirmed the
pathological diagnosis of AFOP (Fig.
2); histopathological examination of lung biopsy specimen with
hematoxylin and eosin stain (magnification, ×10) showed lymphocytic
inflammatory infiltrate and fibroblast proliferation. After
diagnosis, 500 mg methylprednisolone (Pfizer, Inc., New York, NY,
USA) was administered for 3 days followed by 80 mg for 1 week, but
the SpO2 of the patient could not be improved, and he
succumbed to mortality 14 days after admission. The patient's wife
provided written informed consent.
Literature review
General literature review
A literature search on PubMed (www.ncbi.nlm.nih.gov/pubmed) and Medline database
(www.embase.com) was performed between January
2015 and January 2016 using the key words ‘acute fibrinous’ and
‘organizing pneumonia’ or ‘AFOP’, and yielded a total of 42
articles. English language case reports were included, and
manuscripts without adequate details were excluded. Furthermore,
relevant Chinese language manuscripts were searched, and
duplication was eliminated by combining the reports that happened
to refer to the same patient. In addition, reports were removed
that lacked data on clinical manifestations, imaging findings,
treatment outcomes and prognosis. A total of 24 articles with
reference information on 29 patients (including the patient in the
present study) qualified for the literature review and served as
the study population for the purpose of this analysis (Table I) (2–25). Of 29
patients, 20 were male and 9 were female; the median age was 55
years (range, 10–73 years). There was a considerable variability in
the past medical history of AFOP cases and included hypertension,
chronic nephrosis, hypothyroidism, diabetes mellitus, hematological
disorders (leukemia and myelodysplastic syndrome), pulmonary
diseases (cystic fibrosis, asthma and amiodarone-induced
interstitial pneumonia), post-lung transplantation for cystic
fibrosis, interstitial pneumonia and autoimmune diseases, such as
systemic lupus erythematosus (SLE). Smoking appeared not to be a
risk factor, since only 5 of the 29 patients had a history of
smoking. In addition, 12 patients had no past medical history and
were apparently healthy prior to the present illness.
 | Table I.Summary of literature reports on acute
fibrinous and organizing pneumonia. |
Table I.
Summary of literature reports on acute
fibrinous and organizing pneumonia.
| Author | No. reported
patients | Ref. |
|---|
| Guimarães et
al, 2012 | 1 | 2 |
| Kobayashi et
al, 2005 | 1 | 3 |
| Heo et al,
2010 | 1 | 4 |
| Damas et al,
2006 | 1 | 5 |
| Valim et al,
2012 | 1 | 6 |
| Lee et al,
2009 | 1 | 7 |
| Hariri et al,
2010 | 1 | 8 |
| Otto et al,
2013 | 1 | 9 |
| Feng et al,
2014 | 1 | 10 |
| Labarinas et
al, 2013 | 1 | 11 |
| Rapaka et al,
2011 | 1 | 12 |
| Bhatti et al,
2009 | 1 | 13 |
| Renaud-Picard et
al, 2015 | 1 | 14 |
| Xu et al,
2014 | 1 | 15 |
| Miao et al,
2010 | 1 | 16 |
| Gui et al,
2012 | 2 | 17 |
| Zhang et al,
2010 | 1 | 18 |
| Qiu et al,
2013 | 5 | 19 |
| Garcia et al,
2015 | 1 | 20 |
| Piciucchi et
al, 2015 | 1 | 21 |
| Sauter and Butnor,
2014 | 1 | 22 |
| Prahalad et
al, 2005 | 1 | 23 |
| Vasu et al,
2009 | 1 | 24 |
| Yokogawa and Alcid,
2007 | 1 | 25 |
| Present case,
2014 | 1 |
|
Clinical manifestation of AFOP
Clinical manifestation of AFOP appeared to lack
specificity with patients presenting with pulmonary and/or
extra-pulmonary symptoms. The most common pulmonary symptom was a
cough (21/29 patients); 9 patients had a non-productive (dry)
cough. Other less common symptoms included progressive dyspnea,
cough with expectoration, chest pain and hemoptysis (2/29)
(Table II). Vomiting was reported
in 3 patients, indicating the probability of bacterial
infection.
 | Table II.Main pulmonary and extrapulmonary
symptoms of acute fibrinous and organizing pneumonia (AFOP). |
Table II.
Main pulmonary and extrapulmonary
symptoms of acute fibrinous and organizing pneumonia (AFOP).
| Symptoms | No. patients
(n=29) |
|---|
| Cough | 21 |
| Expectoration | 12 |
| Dyspnea | 15 |
| Hemoptysis | 2 |
| Chest pain | 4 |
| Fever | 16 |
| Fatigue | 1 |
| Anorexia | 2 |
| Loss of weight | 1 |
| Night sweat | 3 |
Fever was the other predominant manifestation, with
16 out of 29 patients having fever as their first symptom at the
time of onset. The highest temperature recorded was 39.8°C, and
rarely was it associated with chills and rigors. Most common
extra-pulmonary symptoms included fatigue, anorexia, loss of weight
and night sweats. However, these symptoms were not common.
The clinical presentation of AFOP in the present
study included acute and sub-acute onset. The reported etiology was
idiopathic, secondary to pulmonary infection, connective tissue
disorders or adverse drug reactions. The onset of illness tended to
vary with the etiology with apparently no predictable pattern being
discernible. It was typically difficult to ascertain the exact time
of onset. The time span from disease onset to initiation of medical
treatment ranged between three days and eight months. A number of
patients showed signs of infection, such as upper respiratory tract
signs and symptoms, along with fever. The most important pulmonary
sign was the presence of moist rales in both lower lobes of the
lung (14/29 patients), but in 3 patients the abnormal pulmonary
signs were confined to a unilateral lobe.
Laboratory tests demonstrated that a small number of
patients (4/14) had elevated white blood cells, but the majority of
patients (8/11) had elevated CRP. Immunologic tests and
anti-neutrophil cytoplasmic antibodies were normal except in one
patient with SLE. The various pathological investigations performed
included transbronchial lung biopsy (TBLB) in one patient,
thoracoscopic lung biopsy in three patients, open-lung biopsy in
two patients and pulmonary puncture in 23 patients. All cases were
diagnosed as AFOP on the basis of histopathological evidence.
Chest imaging
A number of patients had multiple bilateral lung
infiltrative shadows at onset; in these patients, the diagnosis was
first suspected on the basis of chest radiography signs. Chest CT
was more informative in delineating the pathological chest signs
(Table III).
 | Table III.Primary imaging findings in acute
fibrinous and organizing pneumonia. |
Table III.
Primary imaging findings in acute
fibrinous and organizing pneumonia.
| Imaging findings | No. patients
(n=28)a |
|---|
| Ground-glass
opacity | 13 |
| Consolidation | 24 |
| Nodular shadows | 8 |
| Strip/net shadow | 5 |
| Interlobular septal
thickening | 1 |
| Unilateral lung | 2 |
| Distribution in both
lower lobes | 7 |
| Distribution near the
pleura | 5 |
| Distribution in
bronchial vascular bundles | 7 |
| Low density
shadow | 0 |
| Halo sign | 3 |
| Reserved halo
sign | 1 |
| Hydrothorax | 6 |
| Pneumothorax | 0 |
Treatment and prognosis
Hormone therapy was the mainstay of treatment in
these patients, with initial dosage varying from prednisone 0.5
mg/kg/day to methylprednisolone 240 mg/day. The treatment regimen
tended to vary among the patients. Likewise, there was a wide
variability in treatment outcomes; ranging between complete
resolution and partial resolution, and in case of four patients,
deterioration leading to mortality.
Discussion
AFOP is a rare pathological entity first described
by Beasley et al (1).
Following this, additional cases of AFOP have been reported. In
2013, the American Thoracic Society/European Respiratory Society
statement defined AFOP as a subgroup of idiopathic interstitial
lung disease with acute lung injury that is characterized by fibrin
deposition in pulmonary alveoli and organization of loose
connective tissue (26). The other
characteristic feature is the absence of diffuse pulmonary alveolar
injury, hyaline membrane formation and no eosinophil infiltration
or granuloma formation (26).
Although all cases were diagnosed on the basis of histopathological
evidence, there were marked differences in clinical manifestations,
treatment and prognosis.
AFOP is a group of illnesses marked by a
considerable heterogeneity with respect to clinical and
pathological changes. The disease etiology is idiopathic or
secondary to other diseases, such as viral infection, connective
tissue disorders and adverse drug reactions. Furthermore, owing to
the heterogenous clinical presentation, the cause of AFOP is
typically ambiguous.
The most common symptoms of AFOP identified in
previous literature were cough, fever and dyspnea, while chest pain
and hemoptysis were relatively less frequent. The clinical picture
appears to be similar to that in other forms of idiopathic
interstitial pneumonia; however, fever that is more common in AFOP
as compared with other forms of interstitial pneumonia.
Radiographic chest findings included consolidation
and bilateral ground-glass shadows with no low-density shadows. The
clinical manifestations of AFOP have been summarized in a number of
reports (8,10,15,17). As
per these reports, the majority of patients had presented with
organizing pneumonia along with multiple plaques, and diffuse
increase in dense shadows in pulmonary alveoli distributed in outer
zone and bilateral boundaries (15).
However, a small number of the patients presented with randomly
distributed nodular shadows. The etiology as well as the
pathological basis of AFOP requires further research in order to
facilitate its distinction from tuberculosis and tumors.
Out of the four mortalities on record among the
study population in the current report, there were 3 males and 1
female. The key distinguishing factors in this study was a higher
proportion of cases with dyspnea and lack of nodular shadows on
chest radiographs, while there was no significant difference in the
proportion of patients manifesting fever. In addition, it was
identified that the development of hydrothorax in AFOP was a poor
prognostic indicator (Table IV).
However, findings from the present study require further evaluation
and validation in larger series.
 | Table IV.Analysis of patients with poor
prognosis. |
Table IV.
Analysis of patients with poor
prognosis.
| Grouping | Mortality at
post-treatment visit | Survival at
post-treatment visit |
|---|
| Age (±SD) | 39.3±19.0 | 54.5±16.5 |
| Gender
(male:female) | 3:1 | 17:8 |
| Symptoms (n=29),
n |
|
|
|
Dyspnea | 3/4 | 12/25 |
|
Fever | 2/4 | 14/25 |
| Computed tomography
(n=28), n |
|
|
|
Ground-glass opacity | 2/4 | 11/24 |
|
Consolidation | 4/4 | 20/24 |
| Nodular
shadows | 1/4 | 7/24 |
|
Hydrothorax | 3/4 | 3/24 |
In conclusion, the current report presents a case of
AFOP that has a rapid onset and progress, is not secondary to other
diseases, shows no improvement in response to glucocorticoid
hormone treatment and has a poor prognosis, and summarizes the key
aspects of this rare disease based on a review of available
published literature. Given the ambiguous etiology and heterogenous
clinical presentation, there is likely to be a significant
under-reporting of AFOP. In other words, the incidence rate of AFOP
could be much higher than what has so far been reported in the
literature. Therefore, the key clinical aspects underlined in this
report should pave the way for further research on AFOP.
References
|
1
|
Beasley MB, Franks TJ, Galvin JR, Gochuico
B and Travis WD: Acute fibrinous and organizing pneumonia: A
histological pattern of lung injury and possible variant of diffuse
alveolar damage. Arch Pathol Lab Med. 126:1064–1070.
2002.PubMed/NCBI
|
|
2
|
Guimarães C, Sanches I and Ferreira C:
Acute fibrinous and organising pneumonia. BMJ Case Rep.
2012:bcr01201136892012.PubMed/NCBI
|
|
3
|
Kobayashi H, Sugimoto C, Kanoh S,
Motoyoshi K and Aida S: Acute fibrinous and organizing pneumonia:
Initial presentation as a solitary nodule. J Thorac Imaging.
20:291–293. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Heo JY, Song JY, Noh JY, Yong HS, Cheong
HJ and Kim WJ: Acute fibrinous and organizing pneumonia in a
patient with HIV infection and Pneumocystis jiroveci pneumonia.
Respirology. 15:1259–1261. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Damas C, Morais A, Moura CS and Marques A:
Acute fibrinous and organizing pneumonia. Rev Port Pneumol.
12:615–620. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Valim V, Rocha RH, Couto RB, Paixão TS and
Serrano EV: Acute fibrinous and organizing pneumonia and
undifferentiated connective tissue disease: A case report. Case Rep
Rheumatol. 2012:5492982012.PubMed/NCBI
|
|
7
|
Lee SM, Park JJ, Sung SH, Kim Y, Lee KE,
Mun YC, Lee SN and Seong CM: Acute fibrinous and organizing
pneumonia following hematopoietic stem cell transplantation. Korean
J Intern Med. 24:156–159. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hariri LP, Unizony S, Stone J,
Mino-Kenudson M, Sharma A, Matsubara O and Mark EJ: Acute fibrinous
and organizing pneumonia in systemic lupus erythematosus: A case
report and review of the literature. Pathol Int. 60:755–759. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Otto C, Huzly D, Kemna L, Hüttel A, Benk
C, Rieg S, Ploenes T, Werner M and Kayser G: Acute fibrinous and
organizing pneumonia associated with influenza A/H1N1 pneumonia
after lung transplantation. BMC Pulm Med. 13:302013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Feng AN, Cai HR, Zhou Q, Zhang YF and Meng
FQ: Diagnostic problems related to acute fibrinous and organizing
pneumonia: Misdiagnosis in 2 cases of lung consolidation and
occupying lesions. Int J Clin Exp Pathol. 7:4493–4497.
2014.PubMed/NCBI
|
|
11
|
Labarinas S, Gumy-Pause F, Rougemont AL,
Baerlocher G, Leibundgut EO, Porret N, Schäppi MG,
Barazzone-Argiroffo C, Passweg J, Merlini L, et al: Is acute
fibrinous and organizing pneumonia the expression of immune
dysregulation? J Pediatr Hematol Oncol. 35:139–143. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rapaka V, Hussain MA, Niazi M and
Diaz-Fuentes G: Severe acute fibrinous and organizing pneumonia
causing acute respiratory distress syndrome and shock. J
Bronchology Interv Pulmonol. 18:269–273. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bhatti S, Hakeem A, Torrealba J, McMahon
JP and Meyer KC: Severe acute fibrinous and organizing pneumonia
(AFOP) causing ventilatory failure: Successful treatment with
mycophenolate mofetil and corticosteroids. Respir Med.
103:1764–1767. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Renaud-Picard B, Dégot T, Biondini D,
Weingertner N, Reeb J, Chenard MP and Kessler R: Successful lung
retransplantation in a patient with acute fibrinous and organizing
pneumonia: A case report. Transplant Proc. 47:182–185. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Xu Y, Ding Hz, Hu T and Qh W: Acute
fibrinous and organizing pneumonia: A case report and review of the
literature. Lin Chuang Fei Ke Za Zhi. 1:186–189. 2014.(in
Chinese).
|
|
16
|
Miao LY, Dai JH, Gui XH, Zhang DP and FQ
M: The clinical pathological features of acute fibrinous and
organizing pneumonia. Lin Chuang Fei Ke Za Zhi. 9:1260–1262.
2010.(in Chinese).
|
|
17
|
Gui XH, Zhang YW, Dai JH, Cai HR, Xiao YL,
Meng FQ and Chen B: Acute Fibrinous and Organizing Pneumonia: Two
case reports and literature review. Chinese Journal of Respiratory
and Critical Care Medicine. 6:558–561. 2012.
|
|
18
|
Zhang J, Fang QH, Feng RE, Ma YM, Cao Y
and Wang RG: Acute fibrinous and organizing pneumonia: A case
report and review of the literature. Zhonghua Jie He He Hu Xi Za
Zhi. 33:892–895. 2010.(In Chinese). PubMed/NCBI
|
|
19
|
Qiu YY, Miao LY, Cai HR, Xiao YL, Ye Q,
Meng FQ and Feng AN: The clinicopathological features of acute
fibrinous and organizing pneumonia. Zhonghua Jie He He Hu Xi Za
Zhi. 36:425–430. 2013.(In Chinese). PubMed/NCBI
|
|
20
|
Garcia BA, Goede T and Mohammed TL: Acute
fibrinous organizing pneumonia: A case report and literature
review. Curr Probl Diagn Radiol. 44:469–471. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Piciucchi S, Dubini A, Tomassetti S,
Casoni G, Ravaglia C and Poletti V: A case of amiodarone-induced
acute fibrinous and organizing pneumonia mimicking mesothelioma. Am
J Respir Crit Care Med. 191:104–106. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sauter JL and Butnor KJ: Expanding the
spectrum of pulmonary histopathological manifestations of
anti-synthetase syndrome: Anti-EJ-associated acute fibrinous and
organizing pneumonia. Histopathology. 65:581–582. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Prahalad S, Bohnsack JF, Maloney CG and
Leslie KO: Fatal acute fibrinous and organizing pneumonia in a
child with juvenile dermatomyositis. J Pediatr. 146:289–292. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Vasu TS, Cavallazzi R, Hirani A and Marik
PE: A 64-year-old male with fever and persistent lung infiltrate.
Respir Care. 54:1263–1265. 2009.PubMed/NCBI
|
|
25
|
Yokogawa N and Alcid DV: Acute fibrinous
and organizing pneumonia as a rare presentation of abacavir
hypersensitivity reaction. AIDS. 21:2116–2117. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Travis WD, Costabel U, Hansell DM, King TE
Jr, Lynch DA, Nicholson AG, Ryerson CJ, Ryu JH, Selman M, Wells AU,
et al: ATS/ERS Committee on Idiopathic Interstitial Pneumonias: An
official American thoracic society/European respiratory society
statement: Update of the international multidisciplinary
classification of the idiopathic interstitial pneumonias. Am J
Respir Crit Care Med. 188:733–748. 2013. View Article : Google Scholar : PubMed/NCBI
|