Introduction
Varicocele (VC) is responsible for ~30–40% of
primary male infertility. It can be divided into the adult type and
juvenile type, and often occurs in the left side of testis (rate,
77–92%) (1). Several causes have
been identified for this disease including absence or dysfunction
of spermatic vein valve, weakness of vein wall and connective
tissues around the vein wall, cremaster hypoplasia and spermatic
vein return resulting from erect posture (2). The traditional operation, laparoscopy
and microtechnique are the main treatment methods used for
patients. However, the postoperative recurrence rate is relatively
high (20–30%) (3). Postoperative
recurrence can seriously reduce the patients quality of life and
adds difficulty to the second operation (4).
In the present study, the treatment effect of
transumbilical single-port laparoscopic varicocelectomy (TUSPLV) on
recurrent VC by comparing the surgical effects of TUSPLV with
traditional retroperitoneal ligation of the internal spermatic vein
was analyzed.
Materials and methods
Object information
From June, 2013 to January, 2015, a total of 64
patients diagnosed with recurrent VC and having suffered from
primary VC were enrolled. Patients with scrotal pain were evaluated
by the visual analogue scale (VAS). Color Doppler ultrasound was
used to evaluate: i) The varicosity degree (CDFI standard); ii) the
volume of testis [the calculation formula was volume (ml) = length
× width × thickness (mm) × 0.71]; the testicular atrophy index (AI)
[calculation formula was AI = (the right side - the left side)
volume of testis/volume of the right side of testis × 100%] and AI
>15% was considered testicular atrophy; and iii) the routine
analysis on the sperm quality including sperm volume, liquefaction
time, pH, sperm concentration, morphology and activity ratio.
The present study was approved by the Ethics
Committee of the Henan Provincial People's Hospital (Henan, China).
Written informed consent was obtained from the patients or their
families.
Patients were divided into the control group (n=30)
and the observation group (n=34) according to the surgical methods
they underwent. Patients in the observation group were treated with
TUSPLV and those in the control group were treated with traditional
retroperitoneal ligation of the internal spermatic vein. According
to the baseline data comparison between the two groups, the
differences had no statistical significance (P>0.05) (Table I).
 | Table I.Baseline data comparison between two
groups. |
Table I.
Baseline data comparison between two
groups.
| Groups | No. of cases | Age (years) | Left side | Infertility | Volume of testis
(ml) | Testicular
atrophy | Varicosity degree
II | Varicosity degree
III | No. of
recurrence | Mean time of
recurrence (months) | Traditional operation
of the previous operation types | Laparoscope |
|---|
| Control | 30 | 24.5±5.3 | 26 (86.7) | 20 (66.7) | 14.2±2.7 | 17 (56.7) | 14 | 16 | 1.2±0.3 | 8.2 | 16 | 14 |
| Observation | 34 | 24.3±5.5 | 27 (79.4) | 22 (64.7) | 14.5±2.8 | 19 (55.9) | 15 | 19 | 1.3±0.2 | 8.4 | 18 | 16 |
| t
(χ2) |
| 0.632 | 0.589 | 0.027 | 0.726 | 0.004 | 0.042 | 0.934 | 0.124 |
| 0.001 |
| P-value |
| 0.454 | 0.443 | 0.869 | 0.922 | 0.950 | 0.838 | 0.876 | 0.789 |
| 0.975 |
Surgical method
The control group surgeries were completed according
to the standard surgical process and the surgeries in the two
groups were completed by the same surgical and nursing team. For
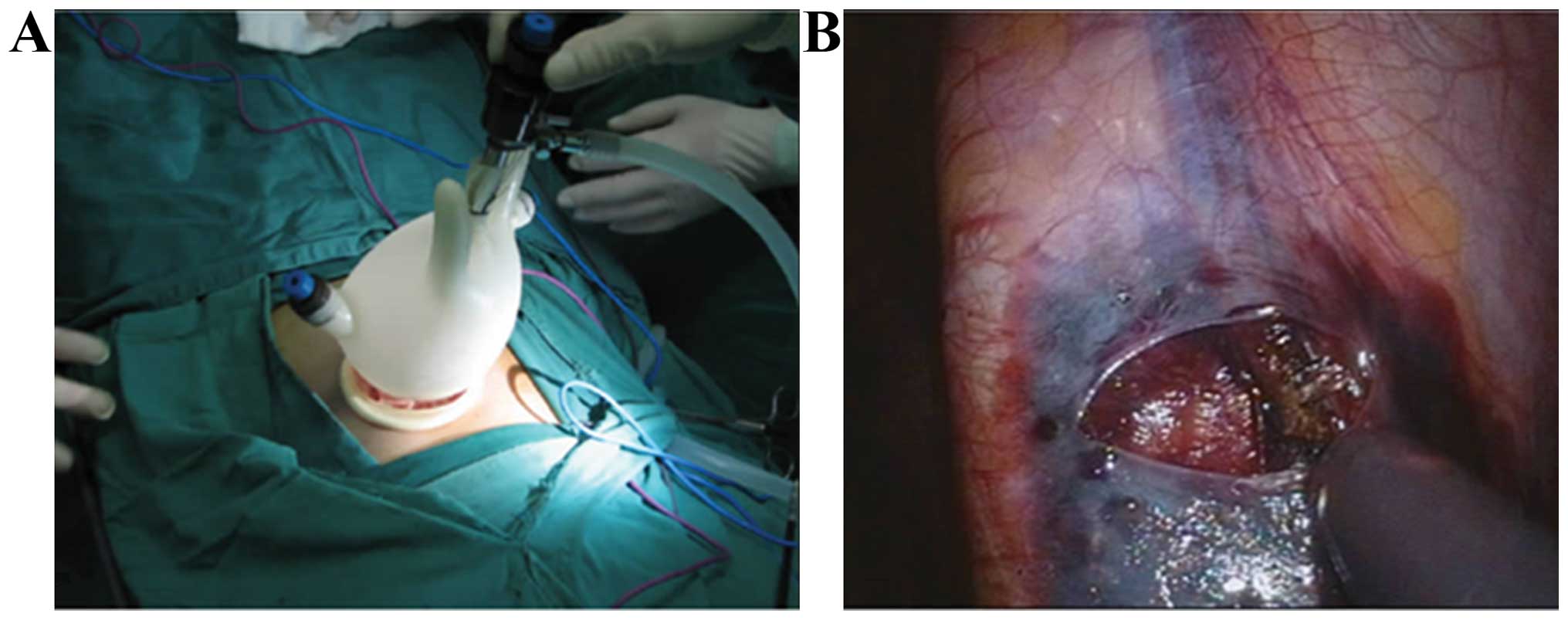
the TUSPLV, the single-port and multi-channel cannula were
self-made by using two elastic rubber rings and no. 7 gloves
(rubber ring with a diameter of 7 cm was used to cover the glove
cuff as an ‘outer ring’ and the other rubber ring with a diameter
of 3 cm was used to cover the middle part of the glove). The glove
was reversed in order that the rubber ring would turn to be the
inner ring and then the part of thumb, middle finger and little
finger tip on the glove were cut off so that the metal cannula
could be placed in the middle finger and the other two valve
circles placed in the thumb and the little finger. Finally they
were tied up and fixed by the suture lines. The incision with
length of 2 cm was made below the umbilicus and the single-port and
multi-channel cannula was placed inside the open abdomen. The
‘outer ring’ was placed in the incision while the ‘outer ring’ was
placed outside of the incision and CO2 was injected
through the metal cannula and the glove was pulled at the same time
to make the inner ring stick close to the inside of the incision.
The outer ring was kept close to the outside of the incision in a
way that the sealed incision would not leak and the
pneumoperitoneum pressure was maintained at 13 mmHg. The scope
entered the body through the metal cannula in the part of the
middle finger and surgical instruments entered the body through the
cannulas in the part of the little finger and the thumb. Through
the scope, we started by verifying any possible injuries in the
organs. We could see the spermaduct from ~1.5 cm above the inner
ring and observed that the A-shaped spermaduct was running
downward. For the patients who suffered from sigmoid colon and
peritoneal adhesion on the left side, we released the adhesion and
then found the spermatic vessels. Scissors were used to cut the
posterior peritoneum located in ~2 cm above the spermaduct to
separate and reveal the internal spermatic veins which generally
had 2–3 branches. We distinguished and reserved the testicular
artery, dissociated the internal spermatic veins and then
coagulated and cut the internal spermatic veins with ligasure
vessel sealing system (ligasure™) and checked whether there were
other venule branches. We used the same method to deal with the
other side of the testis. Subsequently, we reduced the abdominal
pressure and removed the pneumoperitoneum as well as cannulas once
we were confident that there was no hemorrhage. We then sewed up
the skin incision layer by layer (Fig.
1).
Observation target
Patients in the two groups were followed up for ~12
months to determine the differences regarding the time of
operation, bleeding volume during operation, perioperative
complications, recurrence rate and pregnancy rate.
Statistical analysis
SPSS 19.0 statistical software (Chicago, IL, USA)
was used for data analysis. Quantitative data were represented by
the mean ± standard deviation and the comparison between groups was
checked by t-test. Qualitative data were represented by the number
of cases or the percentage (%) and the comparison between groups
was verified using χ2 test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Comparison of operative time and
bleeding volume during operation
The operative time and bleeding volume in the
observation group were reduced significantly and the difference was
statistically significant (P<0.05) (Table II).
 | Table II.Comparison of operative time and
bleeding volume during operation. |
Table II.
Comparison of operative time and
bleeding volume during operation.
| Groups | Operative time
(min) | Bleeding volume
(ml) |
|---|
| Control | 63.5±10.5 | 167.8±24.5 |
| Observation | 46.2±7.5 | 125.4±21.3 |
| t-test | 4.628 | 4.795 |
| P-value | 0.041 | 0.039 |
Comparison of perioperative
complications, recurrence rate and pregnancy rate
The occurrence and recurrence rates of perioperative
complications in the observation group reduced significantly.
Differences were of statistical significance (P<0.05).
Comparison between the pregnancy rate between groups showed no
statistically significant difference (P>0.05) (Table III).
 | Table III.Comparison of perioperative
complications, recurrence rate and pregnancy rate cases, (%). |
Table III.
Comparison of perioperative
complications, recurrence rate and pregnancy rate cases, (%).
| Groups | No. of cases | Hydrocele of tunica
vaginalis | Testicular artery
injury | Injury of organs and
blood vessels in the pelvic cavity and abdominal cavity | Infection | Others | Occurrence rate of
total complications | Recurrence rate | Pregnancy rate |
|---|
| Control | 30 | 3 | 1 | 3 | 2 | 1 | 10 (33.3) | 12 (40.0) | 16 (53.3) |
| Observation | 34 | 1 | 1 | 1 | 1 | 0 | 4 (11.8) | 6 (17.6) | 20 (58.8) |
| χ2 |
|
|
|
|
|
| 4.338 | 3.939 | 0.195 |
| P-value |
|
|
|
|
|
| 0.037 | 0.047 | 0.659 |
Discussion
Complications and recurrence
reasons
Hydrocele of tunica vaginalis is the most common
complication after the spermatic vein ligation which mainly results
from the injury and faulty ligation of lymphatic vessels. The
occurrence rate is 3–39% (5). The
occurrence rate of postoperative testicular atrophy is ~0.2% and it
is mainly caused by the ligation or injury of testicular artery
(6). The recurrence rate after the
spermatic vein ligation usually range from 0.6 to 45% (7)and the reasons for recurrence mainly
include: i) Branches of spermatic vein fail to be ligated
completely and some scholars label the VC with collateral vein as
aberrantly fed VC (AFV). They believe that the postoperative
recurrence mainly results from AFV and missing ligation of lateral
vein (8). Currently, the spermatic
vein radiography is the most reliable method to diagnose primary
VC, among which the selective spermatic vein radiography has the
best result (9). ii) Inner spermatic
vein fails to be cut after ligation or the inner spermatic vein
becomes spasmodic and atrophic. It can be due to traction and
stimulation which makes it difficult to distinguish the inner
spermatic vein during the operation and causes missing ligation
(10). Therefore, when we are
separating and dealing with the spermatic cord we should
distinguish and push the spermaduct away (which is the hardest
tubular tissue in the spermatic cord) while cutting the cremasteric
fascia off. iii) Occurrence of the venous obstructive lesion.
Venous obstructive lesion usually occurs in the inferior vena,
common iliac artery, internal iliac artery and peripheral vein
after ligation of the inner spermatic vein which may result in the
recurrence of VC (11). iv) Faulty
ligation of inferior epigastric vein. The inferior epigastric vein
is in the deep inguinal ring and is close to the spermatic vein and
it runs through the inside of the spermatic vein, which may results
in the faulty ligation of inferior epigastric vein. Use of high
ligation may effectively avoid such faulty ligation. v) Ligation
position is extremely low. Results obtained from a prior study
showed (12,13) that in cases that testicular vein is
positioned lower, more branches of the vein are presented.
Testicular vein branches below the height of L 5 are usually 1–5.
The occurrence rate of testicular vein may reach 72% when the
branches of the testicular vein below the L 5 height are 2.
Advantages and disadvantages of
TUSPLV
TUSPLV can establish pneumoperitoneum by a
multi-channel canula and forms an operating space for flexible
laparoscopy instrument. This can increase the rate of success for
the operation (14). However, this
operation requires special instruments with complicated structure,
wide varieties and operational difficulties carry a high risk of
causing damage (15). We were
successful in completing this operation with minimal complications
by the using a self-made single-port and multi-channel cannula. We
used instruments such as cannulas, rubber rings and gloves that are
all common surgical instruments. Using common and inexpensive
materials makes the operation less complicated. We can also take
advantage of the existing traditional laparoscopy instruments
without any need to purchase expensive flexible instrument and
endoscope (16).
There are a few factors that should be considered
during the operation: i) Surgical instruments can be intersected
after entering the abdominal cavity through the single-port cannula
in the reverse direction of the multi-port laparoscope. Also, the
instruments on the left hand are shown as on the right hand after
they are placed in the body. Therefore, surgical team needs time to
adapt to this situation (17); and
ii) endoscope and surgical instruments enter the body from the same
port and collision between them may be unavoidable and the use of
traditional surgical instruments may cause more collision (18). We used high-definition endoscope and
the collision between the endoscope and surgical instruments was
reduced when the endoscope kept a far distance from the operation
site during the operation (19). The
cooperation between the endoscope operator and the doctor-in-charge
is essential and can reduce the probability of collision among
different instruments. In addition, the missing vein ligation and
faulty ligation of arterial lymph-vessel may be avoided when we
carry out the laparoscopic spermatic vein ligation. We should
carefully observe the vein branches with endoscope and then cut the
peritoneum with scissors to separate the vein. When separating the
vein, the testicular artery should be watched closely to avoid any
unwanted damage to this artery. By keeping the testicular artery
intact, complications caused by faulty ligation and missing
ligation resulting from blurred vision can be avoided (20).
Our results have shown that the time of operation
and bleeding volume in the observation group reduced significantly.
Moreover, the occurrence and recurrence rates of periprocedural
complications decreased significantly. We concluded that TUSPLV is
safe and effective in the treatment of recurrent VC.
References
|
1
|
Esteves SC and Agarwal A: Afterword to
varicocele and male infertility: current concepts and future
perspectives. Asian J Androl. 18:319–322. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pastuszak AW and Wang R: Varicocele and
testicular function. Asian J Androl. 17:659–667. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kim J, Shin JH, Yoon HK, Ko GY, Gwon DI,
Kim EY and Sung KB: Persistent or recurrent varicocoele after
failed varicoelectomy: outcome in patients treated using
percutaneous transcatheter embolization. Clin Radiol. 67:359–365.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kattan S: Incidence and pattern of
varicocele recurrence after laparoscopic ligation of the internal
spermatic vein with preservation of the testicular artery. Scand J
Urol Nephrol. 32:335–340. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kageyama Y, Horiuchi S, Yamada T, Kura N,
Negishi T and Yoshida K: Postoperative hydrocele testis as a
complication of high ligation of internal spermatic vein. Hinyokika
Kiyo. 34:851–854. 1988.(In Japanese). PubMed/NCBI
|
|
6
|
Lv JX, Wang LL, Wei XD, Zhang Z, Zheng TL,
Huang YH, Zhou J, Xia F and Pu JX: Comparison of treatment outcomes
of different spermatic vein ligation procedures in varicocele
treatment. Am J Ther. 12:13–14. 2015.
|
|
7
|
Grober ED, Chan PT, Zini A and Goldstein
M: Microsurgical treatment of persistent or recurrent varicocele.
Fertil Steril. 82:718–722. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Marsman JW: The aberrantly fed varicocele:
frequency, venographic appearance, and results of transcatheter
embolization. AJR Am J Roentgenol. 164:649–657. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Moon KH, Cho SJ, Kim KS and Park S and
Park S: Recurrent varicoceles: causes and treatment using
angiography and magnification assisted subinguinal varicocelectomy.
Yonsei Med J. 53:723–728. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Choi WS and Kim SW: Current issues in
varicocele management: a review. World J Mens Health. 31:12–20.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rotker K and Sigman M: Recurrent
varicocele. Asian J Androl. 18:229–233. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chen SS: Predictive factors of successful
redo varicocelectomy in infertile patients with recurrent
varicocele. Andrologia. 46:738–743. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Shabana W, Teleb M, Dawod T, Elsayed E,
Desoky E, Shahin A, Eladl M and Sorour W: Predictors of improvement
in semen parameters after varicocelectomy for male subfertility: a
prospective study. Can Urol Assoc J. 9:E579–E582. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Canes D, Desai MM, Aron M, Haber GP, Goel
RK, Stein RJ, Kaouk JH and Gill IS: Transumbilical single-port
surgery: evolution and current status. Eur Urol. 54:1020–1029.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kommu SS and Rané A: Devices for
laparoendoscopic single-site surgery in urology. Expert Rev Med
Devices. 6:95–103. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Rane A and Rao P and Rao P: Clinical
evaluation of a novel laparoscopic port (R-PORT™) in urology and
evolution of the single laparoscopic port procedure (SLIPP) and one
port umbilical surgery (OPUS). J Endourol. 21:22–23. 2007.
|
|
17
|
Sun YH, Wang LH, Yang B, Xu CL, Hou JG,
Xiao L and Liu B: Single-port transumbilical laparoscopic
nephrectomy: initial clinical experience of 3 cases. Zhonghua Wai
Ke Za Zhi. 47:1709–1711. 2009.(In Chinese). PubMed/NCBI
|
|
18
|
Kaouk JH and Palmer JS: Single-port
laparoscopic surgery: initial experience in children for
varicocelectomy. BJU Int. 102:97–99. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kang DH, Lee JY, Chung JH, Jo JK, Lee SH,
Ham WS, Cho KS, Lee KS, Kim TH and Lee SW: Laparoendoscopic single
site varicocele ligation: comparison of testicular artery and
lymphatic preservation versus complete testicular vessel ligation.
J Urol. 189:243–249. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Fu B, Wang GX, Sun T, Cui SP, Cao RF, Feng
L, Xi HB, Chen QK and Zhang X: Single-port transumbilical
laparoscopic surgery in urology with report of 18 cases. J Clin
Urol. 24:805–808. 2009.
|