Introduction
Osteochondral fractures of the patella may result in
premature osteoarthritis, chronic swelling, pain and subsequent
decreased physical activity. The fractures are usually associated
with acute patellar dislocation while such a fracture is observed
in 39–54% of the acute dislocations (1,2). The
estimated incidence of patellar dislocation in children is
43/100,000 yearly (1). Knee injuries
in children and adolescents are becoming more common and the main
reasons for this are participation in organized sports, increased
female participation in high risk sports, potentially decreased
motor skills in this population and the improved diagnostic skills
of the treating physicians (3,4). The
average age of patients with osteochondral fracture of the patella
following patellar dislocation is 14.6 years (5). Patellar injury is particularly
detrimental to children, who have long life expectancies, resulting
in morbidity being long-lasting. Numerous treatment methods exist
while non-operative care can be appropriate in stable, asymptomatic
cases (5). Fixation, excision of the
loose bony body, and marrow stimulating procedures such as donor
site microfracturing are other treatment options (6,7).
Fixation is the preferred treatment for unstable osteochondral
fractures, however, there are disadvantages to traditional metallic
implants and the less modern biodegradable implants: The metallic
implants require removal and the less modern biodegradable pins
exhibit an inflammatory reaction elicited from degradation products
(8–10). Biodegradable implants are not common
in injury-based patellar fractures in children, although they are a
widely accepted method of treatment in osteochondritis dissecans,
while both smooth pins and screws are commonly used (11,12).
The current report describes a novel operative
technique using headless poly-L-lactide-co-glycolide (PLGA) pins in
the treatment of a young child with such an injury-based fracture.
Written informed consent was obtained prior to this study.
Case report
The patient was an 11-year-old girl who did not have
any chronic disease. The patient fell whilst cycling and injured
her right knee. She was admitted to Oulu University Hospital (Oulu,
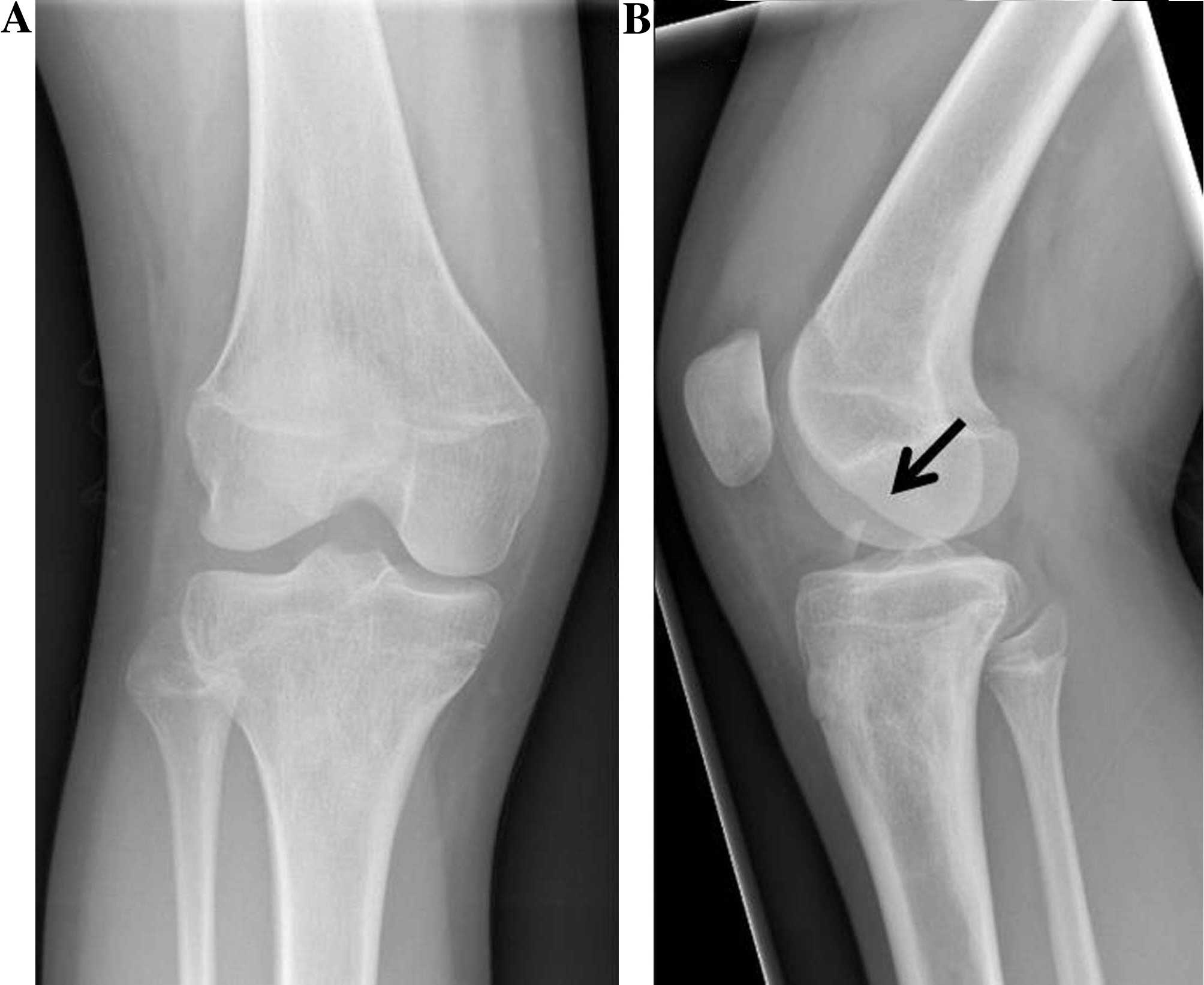
Finland) in November 2014. In the primary radiographs a loose bone
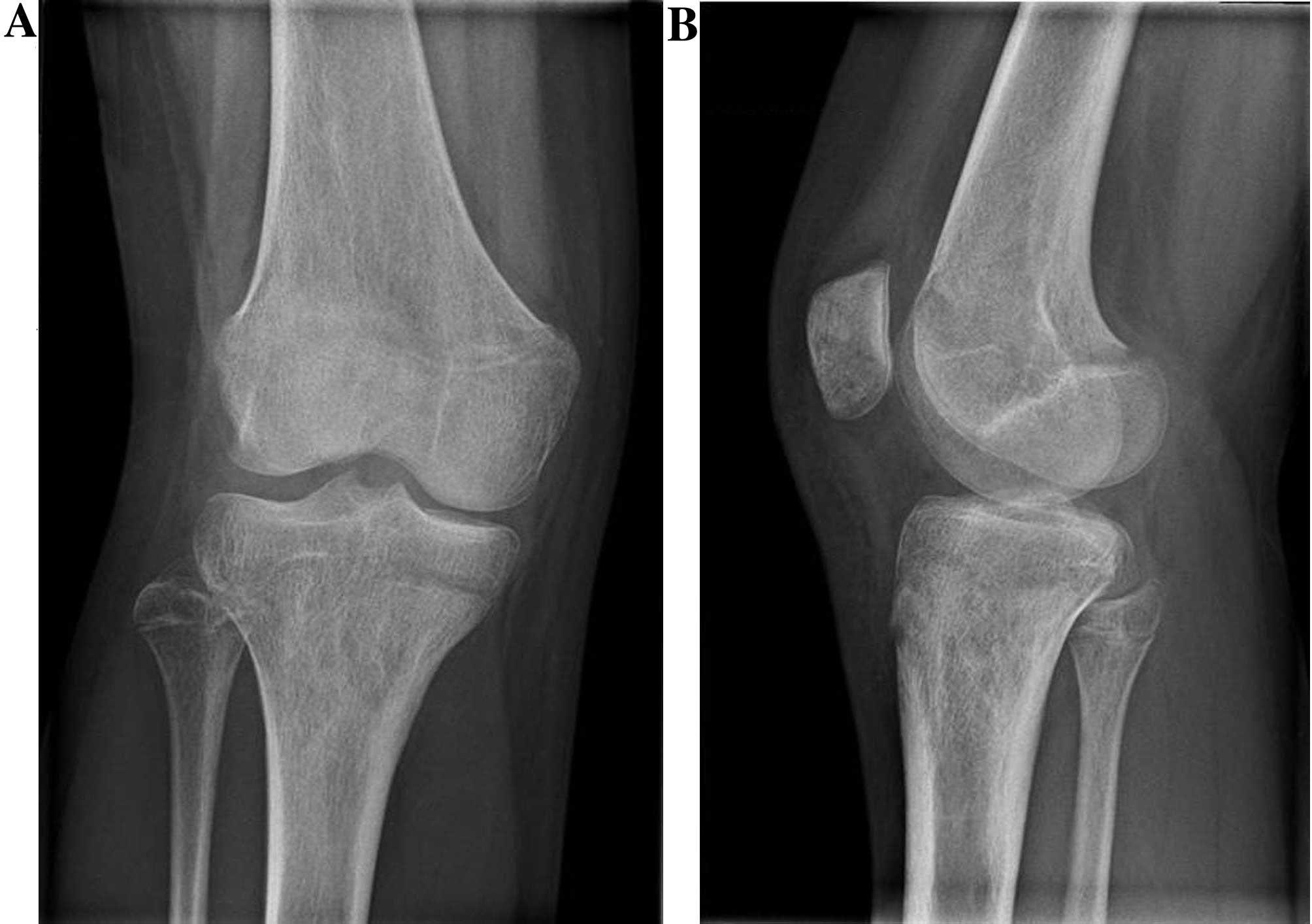
fragment was observed in the knee joint (Fig. 1). A computerized tomography (CT) scan
was then performed, which identified that the fragment originated
from a stress-bearing area of the distal apex of the patellae. The
fragment was ~10×10 mm in size and comprised the joint cartilage
surface and a thin layer of underlying bone tissue (Fig. 2). No other acute musculoskeletal
damage was observed in the CT scan.
Clinical investigation was repeated under general
anesthesia during surgery 5 days later and no patellar instability
was found. Lateral entry arthroscopy identified a large patellar
osteochondral fragment. Arthrotomy, instead of arthroscopy-guided
fixation, was necessary due to the small dimensions of the child
patient. The knee was drained and a vertical parapatellar technique
was used to dissect soft tissues in the approach to the patella,
which was laterally everted 90° using forceps, in order to gain
direct access to the lesion. The surface of the damaged area was
rasped and the fragment was adjusted into its original location.
The fragment was pressed against the patellar bone, followed by
fixation with two 1.4-mm and one 2.0-mm Kirschner wires.
Thereafter, the wires were replaced with two 1.5-mm and one 2.0-mm
PLGA (ActivaPin; Bioretec, Ltd., Tampere, Finland) pins. An
implant-specific ActivaPin-applicator (Bioretec, Ltd.) was used, so
that no notches or unevenness were left at the joint surface.
Postoperatively, an individual shell plaster using
flexible synthetic material was applied to the knee joint. No
weight bearing was allowed for 2 weeks following surgery, in order
to protect the patella from compression against the femoral
trochlear sulcus. Three weeks following the surgery, the patient
visited a surgeon at an outpatient clinic. Partial weight bearing
was allowed (~25 kg), a hinge joint orthosis was ordered to support
the knee and instructions on physical exercises were provided by a
physiotherapist familiar with pediatric trauma. Exercises were
introduced to be performed at home 2 or 3 times a day in order to
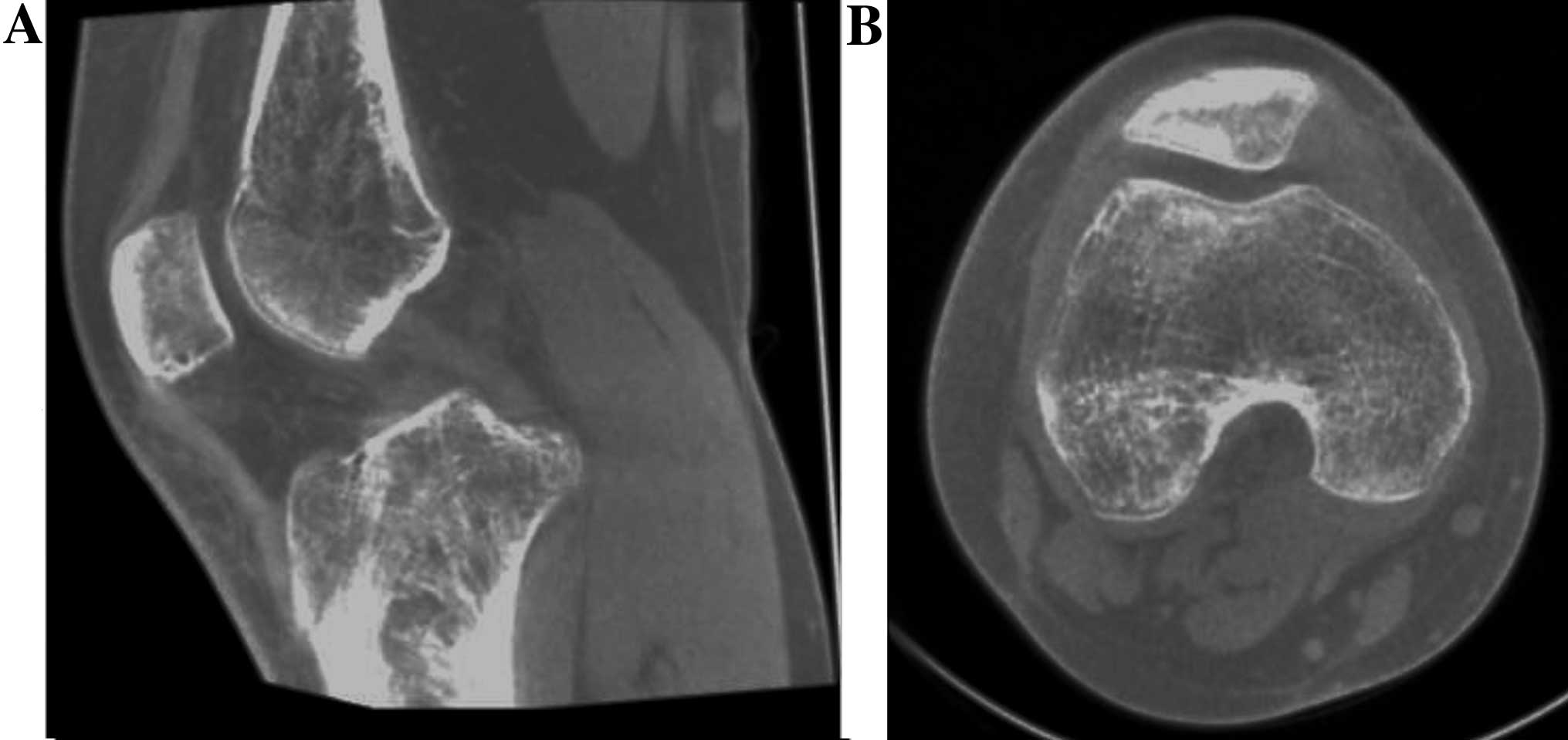
maintain muscle strength. Six weeks following the surgery, the
patellar bone appeared intact in radiographs (Fig. 3) and free movement was allowed. A CT
scan was performed eight weeks following the surgery, which
verified good bone healing (Fig. 4).
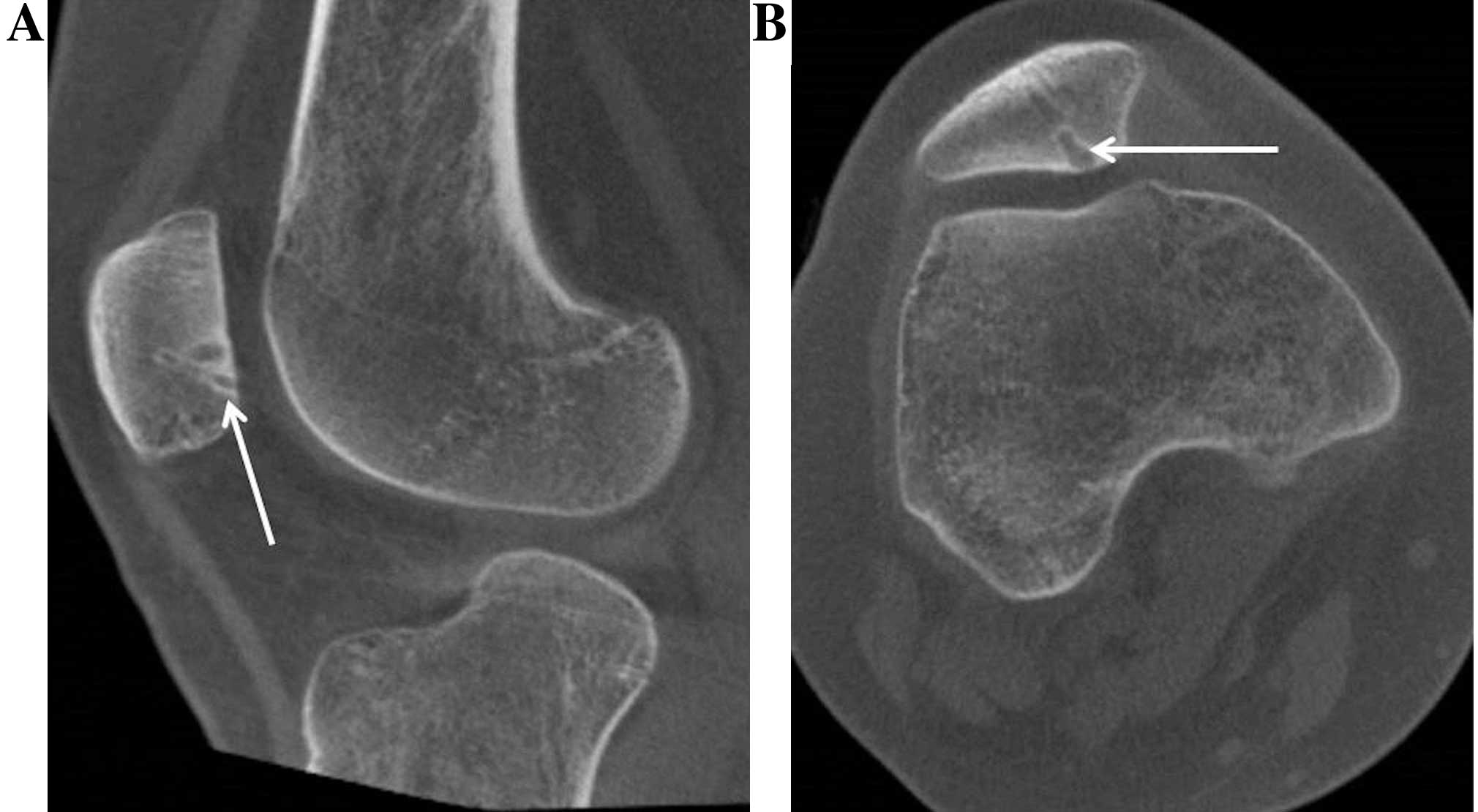
The femoral-patellar joint looked intact. The long-term result was
evaluated 13 months following the surgery. The patella was stable
and the knee had a full range of motion. The child had no
long-lasting symptoms and had returned to pre-injury activity
levels. A smooth joint surface and firm union was observed in cone
beam CT imaging. This imaging also showed edema in the outlines of
the implants, indicating that the degradation process of the
orthopedic implants was on-going, after which they were to be
replaced by bone tissue (Fig.
5).
Discussion
The present report describes an 11-year-old girl,
who was successfully operated on for traumatic patellar
osteochondral fracture by fixing the loose fragment with PLGA pins.
Bioabsorbable pins are typically used to treat osteochonditis
dissecans particles in juvenile skeletons (12). However, to best of our knowledge,
this method has not been widely reported previously in regards to
injury-based patellar fractures in children. In addition, the
material of the implants used in the current report is different
from the traditional absorbable materials previously reported to be
used in orthopedics; traditional absorbable materials have been
shown to affect the outcome, for example, there have been problems
with osteolysis when using polyglycolic acid pins in immature and
mature tissues (13–16).
The technique used in the current report was
straightforward, with excellent short- and long-term results. This
indicates that PLGA pins may be used to fix an intra-articular
fracture in an immature skeleton. In addition, this treatment was
advantageous as no further surgery was needed to remove the
biodegradable implants. The implants will degrade over time,
resulting in the patella being comprised and shaped like it was
prior to the injury.
The prevalence of osteochondral fractures in
children is unknown (17). However,
it has been suggested that knee injuries in children and
adolescents are increasing (3). In
cases of knee hemarthrosis, the incidence of patellar osteochondral
fractures is 5% (18). In addition,
the injury may be more common than previously suspected, as
patellar fractures may not be recognized in normal radiographs,
with magnetic resonance imaging needed to evaluate the
osteochondral damage (19).
In intra-articular osteochondral fractures of the
patella it is important to salvage the cartilage joint surface,
particularly in growing children, to prevent later symptoms and
early-onset osteoarthrosis (20).
Cartilage damage is a primary factor in long-term prognosis
following patellar injury (21).
Extirpation of loose fragments of joint surface results in
fibrocartilage tissue formation (22), thus removal is only acceptable for
small fragments not involved in the central part of the joint or
stress-bearing areas. Consequently, surgical repositioning and
fixation of fragments is the preferred method of treatment.
Numerous techniques have been described, with screw and pin
fixations being the most common (23–28).
However, traditional metallic implants can cause mechanical damage
of the joint if the surrounding bone collapses or cartilage wears
out and removal of the implants may be necessary (29). The primary advantage of absorbable
implants is that a second surgery for removal is not necessary
(17).
A previous study has determined that biodegradable
pin fixation is a feasible technique for the treatment of knee
injuries in adolescents (7). In
addition, other types of biodegradable implants, including screws
and nails, have been reported (30).
Despite the better compression provided by screws, the prominence
of the screw head may result in a more uneven joint surface
compared with pins (17,31). In the current report, satisfactory
compression was achieved with PLGA pins, where a tight ‘drill’ hole
was made using conventional Kirschner wire as a bore bit, instead
of a proper drilling. The stability of fixation was manually tested
during the surgery. Furthermore, the material of the implant used
in the current report swells between 1 and 2% when it comes into
contact with human tissue, further increasing the rigidity of the
fixation (32).
The technique described in the current report
resulted in an excellent recovery following PLGA pin fixation of an
adolescent traumatic patellar osteochondral fracture. Radiographic
imaging identified complete ossification of the loose fragment and
CT imaging demonstrated an intact knee joint surface. Bone healing
following treatment was fast, with osteosynthesis becoming stable
VI weeks postoperatively. Thirteen months postoperatively, the
outlines of the implants were partially recognized in CT imaging,
as a result of implant resolution, demonstrating on-going
replacement with human tissue. In conclusion, the novel surgical
approach to treating children with a traumatic patellar
osteochondral fracture by PLGA pins described in the current report
warrants future randomized clinical trials, in order to validate
the superiority of this technique over the traditional metallic
implants used in the pediatric population.
Acknowledgements
Dr Juha-Jaakko Sinikumpu received a grant supporting
the current report from Bioretec, Ltd. (Tampere, Finland).
References
|
1
|
Nietosvaara Y, Aalto K and Kallio PE:
Acute patellar dislocation in children: Incidence and associated
osteochondral fractures. J Pediatr Orthop. 14:513–515. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nomura E, Inoue M and Kurimura M: Chondral
and osteochondral injuries associated with acute patellar
dislocation. Arthroscopy. 19:717–721. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Seil R, Weitz FK and Pape D:
Surgical-experimental principles of anterior cruciate ligament
(ACL) reconstruction with open growth plates. J Exp Orthop.
2:112015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Aichroth PM, Patel DV and Zorrilla P: The
natural history and treatment of rupture of the anterior cruciate
ligament in children and adolescents. A prospective review. J Bone
Joint Surg Br. 84:38–41. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lee BJ, Christino MA, Daniels AH, Hulstyn
MJ and Eberson CP: Adolescent patellar osteochondral fracture
following patellar dislocation. Knee Surg Sports Traumatol
Arthrosc. 21:1856–1861. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gudas R, Kalesinskas RJ, Kimtys V,
Stankevicius E, Toliusis V, Bernotavicius G and Smailys A: A
prospective randomized clinical study of mosaic osteochondral
autologous transplantation versus microfracture for the treatment
of osteochondral defects in the knee joint in young athletes.
Arthroscopy. 21:1066–1075. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Matsusue Y, Nakamura T, Suzuki S and
Iwasaki R: Biodegradable pin fixation of osteochondral fragments of
the knee. Clin Orthop Relat Res. 166–173. 1996.PubMed/NCBI
|
|
8
|
Din R, Annear P and Scaddan J: Internal
fixation of undisplaced lesions of osteochondritis dissecans in the
knee. J Bone Joint Surg Br. 88:900–904. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nakagawa T, Kurosawa H, Ikeda H, Nozawa M
and Kawakami A: Internal fixation for osteochondritis dissecans of
the knee. Knee Surg Sports Traumatol Arthrosc. 13:317–322. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mainil-Varlet P, Rahn B and Gogolewski S:
Long-term in vivo degradation and bone reaction to various
polylactides. 1. One-year results. Biomaterials. 18:257–266. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rehm KE, Helling HJ and Gatzka C: New
developments in the application of resorbable implants. Orthopade.
26:489–497. 1997.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Adachi N, Deie M, Nakamae A, Okuhara A,
Kamei G and Ochi M: Functional and radiographic outcomes of
unstable juvenile osteochondritis dissecans of the knee treated
with lesion fixation using bioabsorbable pins. J Pediatr Orthop.
35:82–88. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fraser RK and Cole WG: Osteolysis after
biodegradable pin fixation of fractures in children. J Bone Joint
Surg Br. 74:929–930. 1992.PubMed/NCBI
|
|
14
|
Böstman O and Pihlajamäki H: Clinical
biocompatibility of biodegradable orthopaedic implants for internal
fixation: A review. Biomaterials. 21:2615–2621. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Rokkanen P, Böstman O, Hirvensalo E,
Partio EK, Mäkelä EA, Pätiälä H and Vihtonen K: Bioabsorbable
implants in orthopaedics. Curr Orthop. 13:223–228. 1999. View Article : Google Scholar
|
|
16
|
Rokkanen PU, Böstman O, Hirvensalo E,
Mäkelä EA, Partio EK, Pätiälä H, Vainionpää SI, Vihtonen K and
Törmälä P: Bioabsorbable fixation in orthopaedic surgery and
traumatology. Biomaterials. 21:2607–2613. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chotel F, Knorr G, Simian E, Dubrana F and
Versier G: French Arthroscopy Society: Knee osteochondral fractures
in skeletally immature patients: French multicenter study. Orthop
Traumatol Surg Res. 97(8): Suppl. S154–S159. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Vähäsarja V, Kinnuen P and Serlo W:
Arthroscopy of the acute traumatic knee in children. Prospective
study of 138 cases. Acta Orthop Scand. 64:580–582. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Vellet AD, Marks PH, Fowler PJ and Munro
TG: Occult posttraumatic osteochondral lesions of the knee:
Prevalence, classification, and short-term sequelae evaluated with
MR imaging. Radiology. 178:271–276. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kramer DE and Pace JL: Acute traumatic and
sports-related osteochondral injury of the pediatric knee. Orthop
Clin North Am. 43:227–236, vi. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Schmal H, Strohm PC, Niemeyer P, Reising
K, Kuminack K and Sudkamp NP: Fractures of the patella in children
and adolescents. Acta Orthop Belg. 76:644–650. 2010.PubMed/NCBI
|
|
22
|
Scopp JM and Mandelbaum BR: Cartilage
restoration: Overview of treatment options. J Knee Surg.
17:229–233. 2004.PubMed/NCBI
|
|
23
|
Sgaglione NA, Miniaci A, Gillogly SD and
Carter TR: Update on advanced surgical techniques in the treatment
of traumatic focal articular cartilage lesions in the knee.
Arthroscopy. 18(2): Suppl 1. S9–S32. 2002. View Article : Google Scholar
|
|
24
|
Beasley LS and Vidal AF: Traumatic
patellar dislocation in children and adolescents: Treatment update
and literature review. Curr Opin Pediatr. 16:29–36. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Jakob RP, Franz T, Gautier E and
Mainil-Varlet P: Autologous osteochondral grafting in the knee:
Indication, results, and reflections. Clin Orthop Relat Res.
170–184. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Cain EL and Clancy WG: Treatment algorithm
for osteochondral injuries of the knee. Clin Sports Med.
20:321–342. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Mandelbaum BR, Browne JE, Fu F, Micheli L,
Mosely JB Jr, Erggelet C, Minas T and Peterson L: Articular
cartilage lesions of the knee. Am J Sports Med. 26:853–861.
1998.PubMed/NCBI
|
|
28
|
Kish G, Módis L and Hangody L:
Osteochondral mosaicplasty for the treatment of focal chondral and
osteochondral lesions of the knee and talus in the athlete.
Rationale, indications, techniques, and results. Clin Sports Med.
18:45–66, vi. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Korhonen J, Sinikumpu JJ, Harmainen S,
Ryhänen J, Kallio P and Serlo W: Removal of osteosynthesis material
in children and young people. Duodecim. 130:689–695. 2014.(In
Finnish). PubMed/NCBI
|
|
30
|
Fuchs M, Vosshenrich R, Dumont C and
Stürmer KM: Refixation of osteochondral fragments using absorbable
implants. First results of a retrospective study. Chirurg.
74:554–561. 2003.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hirsch G and Boman A: Osteochondral
fractures of the knee in children and adolescents treatment with
open reduction and osteosynthesis using biodegradable pins.
Techniques in Orthopaedics. 13:139–142. 1998. View Article : Google Scholar
|
|
32
|
Sinikumpu JJ, Keränen J, Haltia AM, Serlo
W and Merikanto J: A new mini-invasive technique in treating
paediatric diaphyseal forearm fractures by bioabsorbable elastic
stable intramedullary nailing: A preliminary technical report.
Scand J Surg. 102:258–264. 2013. View Article : Google Scholar : PubMed/NCBI
|