Introduction
Portopulmonary hypertension (POPH) is defined as
pulmonary arterial hypertension (PAH)-associated with portal
hypertension. The incidence of POPH in patients with liver
cirrhosis is 0.7%, which increases to 16% in patients with
refractory ascites (1). Patients
with POPH may exhibit only some of the symptoms associated with
PAH, including dyspnea, hepatic ascites and edema (1). At present, therapeutic strategies for
the treatment of POPH have yet to be assessed in randomized
controlled trials, such that no definitive treatment is currently
available.
Arterial underfilling secondary to systemic arterial
vasodilatation and hypoalbuminemia-associated low oncotic pressure
may lead to the activation of the renin-angiotensin-aldosterone
system (RAAS) and non-osmotic release of arginine vasopressin
(AVP). Activation of the RAAS and release of AVP has a major role
in the pathogenesis of fluid retention and contributes to
resistance to loop diuretics in patients with liver cirrhosis
(2). Coexistence of liver cirrhosis
with POPH may lead to elevated central venous pressure secondary to
right-sided heart failure, which, in turn, adversely affects
cardiorenal hemodynamics (3).
Therefore, patients with liver cirrhosis and POPH often require
treatment with high-dose loop diuretics that activate the RAAS and
the sympathetic nervous system, which then adversely affects the
cardiopulmonary circulation (2).
Tolvaptan is a selective vasopressin V2 receptor
antagonist that inhibits vasopressin-mediated water reabsorption in
the renal collecting ducts. It has recently been approved for the
treatment of liver cirrhosis with edema (4–6). The
inhibition of V2 receptor using tolvaptan is able to
effectively reduce excessive fluid overload and reduce the amount
of loop diuretics required, which can provide favorable
neurohumoral and hemodynamic effects. The present study reports a
case of POPH secondary to underlying liver cirrhosis in a
58-year-old woman, who was successfully treated with low-dose
tolvaptan.
Case report
A 58-year-old woman complained of leg edema and
exertional dyspnea, which was classified as World Health
Organization functional class II (7). The patient had been diagnosed with
hepatitis C virus-associated liver cirrhosis 9 years previously.
The patient had also been diagnosed with POPH 3 years previously
and had been treated with combination therapy of sildenafil (20 mg,
three times a day) and bosentan (62.5 mg, twice a day) for 2 years.
Subsequently, bosentan was changed to ambrisentan (5 mg, once a
day) due to hepatotoxicity 1 year prior to admission. The patient
suffered from leg edema and ascites despite combination therapy
with spironolactone (100 mg/day) and furosemide (80 mg/day). The
patient was admitted to the Mie University Hospital (Tsu, Japan) in
April 2012.
Upon hospital admission, the patient's blood
pressure was 105/58 mmHg with a slightly elevated pulse rate of 96
bpm [normal range (NR)=60–100 bpm] and 96% oxygen saturation. No
signs or symptoms of hepatic encephalopathy were observed, and a
physical examination showed bilateral leg edema. Cardiac
auscultation showed grade 2/6 pan-systolic murmur and a prominent
pulmonary component of the second heart sound. A chest X-ray scan
revealed pulmonary arterial dilatation and cardiomegaly, with a
cardiothoracic ratio of 0.57. Blood tests revealed pancytopenia
[white blood cell count, 2,650 cells/µl (NR=3500–9100 cells/µl);
hematocrit, 33.1% (NR=33.4–44.9%); platelet count,
3.7×104/µl (NR=13.0–36.9×104/µl)],
hypocoagulability [international normalized ratio of prothrombin
time, 1.62 (NR=0.85–1.15)], hyperbilirubinemia [total bilirubin,
5.5 mg/dl (NR=0.3–1.2 mg/dl)], and hypoalbuminemia [2.7 g/dl
(NR=3.8–5.2 g/dl)]; therefore, the patient was classified as having
Child-Pugh class C cirrhosis (score 10) (8). The hepatic aminotransferase
concentration was within the normal range and renal function was
not abnormal. Severe hypokalemia and mild-moderate hyponatremia
were detected, while the brain natriuretic peptide (BNP) and AVP
levels in the plasma were mildly elevated. Plasma renin activity
and plasma aldosterone concentration were also remarkably high.
Furthermore, transthoracic echocardiography showed right
ventricular and right atrial dilatation and severe tricuspid
insufficiency with normal left ventricular function. A computed
tomography scan showed no evidence of pulmonary embolism,
interstitial lung disease or adrenal tumor, but displayed abnormal
findings that suggested portal hypertension and liver cirrhosis.
The respiratory function of the patient was normal. Right heart
catheterization (RHC) revealed that the patient suffered from
moderate PAH. In addition, the cardiac index (CI) was higher than
normal, which was consistent with the diagnosis of POPH.
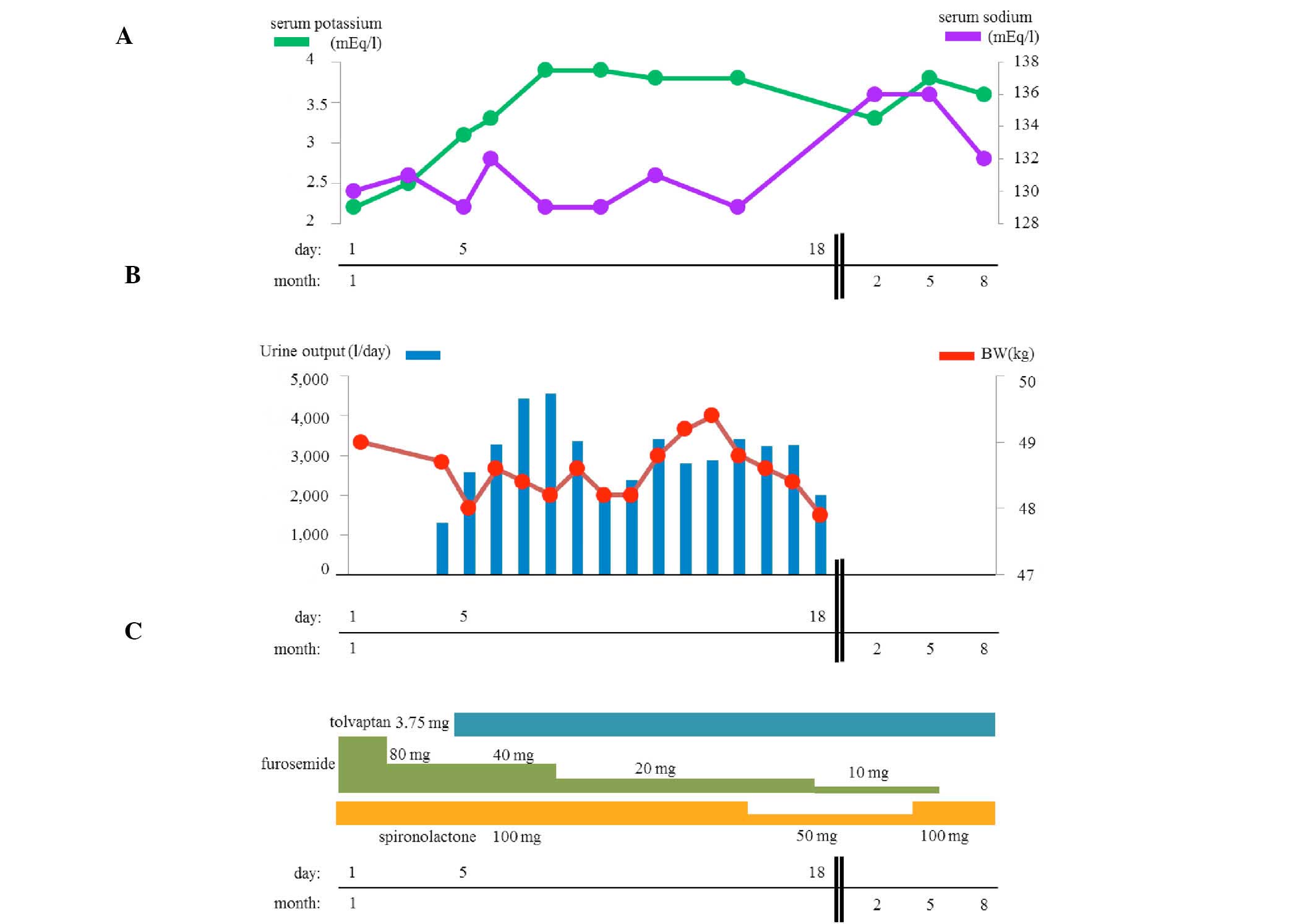
The patient was administered 80 mg/day oral
furosemide and 100 mg/day spironolactone, however the mean right
atrial pressure (RAP) and mean pulmonary capillary wedge pressure
values (4 mmHg and 8 mmHg, respectively) were not elevated. Since
the patient exhibited marked hypokalemia, the dose of furosemide
was decreased to 40 mg/day following admission. In addition, low
dose tolvaptan (3.75 mg/day) treatment was initiated in order to
treat liver cirrhosis-associated edema and diuretic-associated
adverse effects, including an electrolyte imbalance. As a result,
the urine output increased to >4,000 ml and the leg edema was
improved. Subsequently, the furosemide dose was tapered to 20
mg/day. The serum potassium level was increased from 2.2 to 3.8
mEq/dl, whereas the serum creatinine and blood urea nitrogen levels
were not altered within 1 week of treatment and no marked changes
in the patient's body weight were observed (Fig. 1 and Table
I). Notably, the levels of all neurohumoral markers, including
AVP, BNP, plasma renin activity (PRA), and plasma aldosterone
concentration (PAC) were decreased (Table I). Subsequently, spironolactone was
decreased to 50 mg/day on day 16 following hospitalization.
Repeated RHC was performed on day 17 following hospitalization (12
days after the initiation of tolvaptan treatment) and demonstrated
that the mean pulmonary arterial pressure (PAP) and pulmonary
vascular resistance (PVR) had decreased, although the systemic
arterial pressure, mean RAP and CI remained unchanged (Table II).
 | Table I.Pertinent laboratory variables pre-
and post-treatment. |
Table I.
Pertinent laboratory variables pre-
and post-treatment.
| Variables | Pre-treatment | Post-treatment | Normal |
|---|
| Serum sodium,
mEq/l | 130 | 131 | 135–145 |
| Serum potassium,
mEq/l | 2.2 | 3.8 | 3.6–4.9 |
| Serum urea nitrogen,
mg/dl | 15 | 12 | 8–20 |
| Serum creatinine,
mg/dl | 0.53 | 0.46 | 0.46–0.79 |
| AVP, pg/ml | 4.6 | 4.2 | <3.8 |
| BNP, pg/ml | 51.5 | 50 | <18.4 |
| Plasma renin
activity, ng/ml/h | 17 | 12 | 0.3–2.9 |
| Plasma aldosterone,
pg/ml | 463 | 391 | 29.9–159 |
 | Table II.Clinical, right heart catheterization
and blood gas variables pre- and post-treatment. |
Table II.
Clinical, right heart catheterization
and blood gas variables pre- and post-treatment.
| Variables | Pre-treatment | Post-treatment | Normal |
|---|
| Heart rate (bpm) | 96 | 84 | 60–100 |
| Blood pressure
(mmHg) | 105/58 | 107/66 | <120/80 |
| Mean PAP (mmHg) | 40 | 36 | 9–19 |
| PCWP (mmHg) | 8 | 11 | 4–12 |
| CI
(l/min/m2) | 4.61 | 4.5 | 2.5–4.0 |
| SVR (Wood unit) | 10.7 | 11.6 | 8.75–20 |
| PVR (Wood unit) | 4.89 | 3.91 | 1.25–3 |
| Mean RAP (mmHg) | 4 | 6 | 2~7 |
| PaO2
(mmHg) | 66.6 | 70.4 | >80 |
The patient was discharged on day 19 after
hospitalization, following a further decrease of the dose of
furosemide to 10 mg/day. The patient was successfully managed with
the combination of low-dose tolvaptan and spironolactone without
the need for furosemide administration 8 months after the induction
of tolvaptan therapy in an outpatient setting, and serum sodium was
increased (Fig. 1). The patient
unfortunately died due to hepatic failure 2 years and 5 months
following the induction of treatment. Written informed consent to
participate in the present study was obtained from the patient's
family.
Discussion
The present study reported a case of POPH that was
secondary to underlying liver cirrhosis. The patient was
successfully treated with low-dose tolvaptan. Tolvaptan therapy
ameliorated the signs and symptoms of liver cirrhosis-associated
edema, the electrolyte balance and the hemodynamic status
associated with a lower dose of loop diuretics.
Arterial underfilling that is secondary to systemic
arterial vasodilatation and low oncotic pressure leads to the
activation of RAAS and the non-osmotic release of AVP, which plays
a major role in the pathogenesis of fluid retention and contributes
to resistance to loop diuretics in patients with liver cirrhosis
(2). Fluid restriction in
combination with orally administered aldosterone antagonists and
loop diuretics has long been the primary approach used for the
treatment of fluid retention and edema (2). However, these therapies may be
ineffective in certain patients, and an escalating dose of
furosemide induces intravenous sodium loss that contributes to
decreased effective arterial blood volume, which in turn stimulates
the non-osmotic release of AVP, activating the V2
receptor and inducing water reabsorption in the distal nephron
(2). Free water reabsorption via AVP
stimulation can cause hypervolemic hyponatremia and hypokalemia in
cirrhosis (9,10). Therefore, the V2 receptor
is theoretically a therapeutic target. Sakaida et al
(4,5)
and Okita et al (6) reported
that add-on therapy of a low dose of tolvaptan to conventional
diuretics in patients with cirrhosis was effective in improving
hepatic edema with preferable tolerability. Although the
aforementioned studies did not assess whether V2
receptor blockade has favorable effects on the neurohumoral system,
the administration of tolvaptan was found to stabilize RAAS not
only by its aquaretic potency, but also by lowering the dose of
furosemide required (4–6). Indeed, PRA and PAC decreased after a
short time of treatment and low-dose tolvaptan therapy was applied
with concurrent de-escalation of the dose of furosemide to 20
mg/day in present case.
Notably, the mean PAP and PVR values decreased 12
days after the initiation of tolvaptan therapy in the present case.
Although no data have been previously reported regarding whether
V2 receptor blockade in the distal nephron can favorably
influence pulmonary circulation in patients with PAH in a clinical
setting, there is increasing evidence that the RAAS plays a
significant role in the development of PAH (11,12).
Maron et al (11) reported
that plasma aldosterone levels correlate positively with the PVR
and transpulmonary gradient in patients with PAH, and Preston et
al (12) reported that
mineralocorticoid receptor antagonism reduced the PVR in an
experimental pulmonary hypertension model. In the present case,
successful de-escalation of the furosemide dose rather than the
pharmacological effect of tolvaptan may have contributed to the PVR
reduction. Notably, chronic treatment combining spironolactone and
low-dose tolvaptan achieved optimal fluid control without
furosemide. From the neurohumoral perspective, dual blockade of the
RAAS and the V2 system can play a major role in
maintaining cardiopulmonary and renal hemodynamics in patients with
POPH secondary to liver cirrhosis.
In conclusion, the present study reported the use of
low-dose tolvaptan in a patient with POPH and electrolyte
disturbances associated with cirrhosis and conventional diuretics.
A low dose of tolvaptan is considered to be pharmaceutically
appropriate for such a condition, and may also provide beneficial
effects on pulmonary hemodynamics without deterioration of renal
and liver functions.
References
|
1
|
Hoeper MM, Krowka MJ and Strassburg CP:
Portopulmonary hypertension and hepatopulmonary syndrome. Lancet.
363:1461–1468. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Schrier RW: Use of diuretics in heart
failure and cirrhosis. Semin Nephrol. 31:503–512. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Golbin JM and Krowka MJ: Portopulmonary
hypertension. Clin Chest Med. 28:203–218. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sakaida I, Yanase M, Kobayashi Y, Yasutake
T, Okada M and Okita K: ASCITES Clinical Pharmacology Group: The
pharmacokinetics and pharmacodynamics of tolvaptan in patients with
liver cirrhosis with insufficient response to conventional
diuretics: A multicentre, double-blind, parallel-group, phase III
study. J Int Med Res. 40:2381–2393. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sakaida I, Kawazoe S, Kajimura K, Saito T,
Okuse C, Takaguchi K, Okada M and Okita K: Ascites-Doubleblind
Study Group: Tolvaptan for improvement of hepatic edema: A phase 3,
multicenter, randomized, double-blind, placebo-controlled trial.
Hepatol Res. 44:73–82. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Okita K, Kawazoe S, Hasebe C, Kajimura K,
Kaneko A, Okada M and Sakaida I: ASCITES Dose-Finding Trial Group:
Dose-finding trial of tolvaptan in liver cirrhosis patients with
hepatic edema: A randomized, double-blind, placebo-controlled
trial. Hepatol Res. 44:83–91. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Galiè N, Hoeper MM, Humbert M, Torbicki A,
Vachiery JL, Barbera JA, Beghetti M, Corris P, Gaine S, Gibbs JS,
et al: ESC Committee for Practice Guidelines (CPG): Guidelines for
the diagnosis and treatment of pulmonary hypertension: The Task
Force for the Diagnosis and Treatment of Pulmonary Hypertension of
the European Society of Cardiology (ESC) and the European
Respiratory Society (ERS), endorsed by the International Society of
Heart and Lung Transplantation (ISHLT). Eur Heart J. 30:2493–2537.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pugh RN, Murray-Lyon IM, Dawson JL,
Pietroni MC and Williams R: Transection of the oesophagus for
bleeding oesophageal varices. Br J Surg. 60:646–649. 1973.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ginés P, Berl T, Bernardi M, Bichet DG,
Hamon G, Jiménez W, Liard JF, Martin PY and Schrier RW:
Hyponatremia in cirrhosis: From pathogenesis to treatment.
Hepatology. 28:851–864. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pérez-Ayuso RM, Arroyo V, Planas R, et al:
Randomized comparative study of efficacy of furosemide versus
spironolactone in nonazotemic cirrhosis with ascites. Relationship
between the diuretic response and the activity of the
renin-aldosterone system. Gastroenterology. 84:961–968.
1983.PubMed/NCBI
|
|
11
|
Maron BA, Opotowsky AR, Landzberg MJ,
Loscalzo J, Waxman AB and Leopold JA: Plasma aldosterone levels are
elevated in patients with pulmonary arterial hypertension in the
absence of left ventricular heart failure: A pilot study. Eur J
Heart Fail. 15:277–283. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Preston IR, Sagliani KD, Warburton RR,
Hill NS, Fanburg BL and Jaffe IZ: Mineralocorticoid receptor
antagonism attenuates experimental pulmonary hypertension. Am J
Physiol Lung Cell Mol Physiol. 304:L678–L688. 2013. View Article : Google Scholar : PubMed/NCBI
|