Introduction
Sanguinarine, with a formula of
13-methyl-[1,3]benzodioxolo[5,6-c]-1,3-dioxolo[4,5-i]phenanthridinium,
is an active ingredient derived from the roots of Sanguinaria
canadensis, the seeds of Argemone mexicana and from
various other poppy-fumaria species (1,2).
Sanguinarine is of great interest from a practical and research
perspective due to its widespread and evident biological activities
(3). It is used as a naturopathic
therapy for treating infections and managing pain, and as an
expectorant, sedative and emetic (3). Sanguinarine has been demonstrated to
exhibit anti-oxidant, anti-tumor, anti-inflammatory and
anti-microbial properties (1,4–7). However, the effect of sanguinarine on
neuroprotection has not been widely investigated.
Stroke or cerebral ischemia is one of the leading
causes of long-term disabilities and mortality worldwide. Ischemic
injury is caused by a permanent or transient reduction in cerebral
blood flow in the brain artery (8,9). As a
result of oxygen depletion, brain tissue is exposed to a dramatic
decline in blood flow, Ca2+ overload, mitochondrial and
DNA damage, excessive glutamate-receptor activation and oxygen
radical formation (8,9). Necrosis and apoptosis then occur in
brain cells, leading to eventual cell death. Various mechanisms of
cerebral ischemia have been identified in previous studies,
including excitotoxicity, peri-infarct depolarizations,
inflammation and programmed cell death (10,11).
Following ischemia, inflammatory cells (including microglia and
blood-derived leukocytes) are activated and accumulate in the brain
tissue, resulting in inflammatory injury.
During the processes of cerebral ischemia or stroke,
certain molecular factors are generated, which then activate
components of innate immunity, promote inflammatory signaling and
cause tissue damage (12). The most
extensively studied inflammatory cytokines associated with stroke
include interleukin (IL)-1β, IL-6, IL-10 and tumor necrosis
factor-α (TNF-α). These molecules gather more leukocytes to the
site of ischemia, resulting in further loss of nerve cells,
increased apoptosis or necrosis in cerebral tissue, and an
increased area of cerebral infarction (13). All these functions are considered to
induce apoptosis. Members of the B-cell lymphoma 2 (Bcl-2) family
serve an important role in cerebral ischemia. In particular, Bcl-2
(which is an anti-apoptotic protein) and Bcl-2-associated X protein
(Bax; which is a pro-apoptotic protein) regulate apoptosis by
mutual suppression (14). Shortly
following the beginning of ischemia, dephosphorylation and
translocation of Bax from the cytosol to the mitochondria, as well
as dimerization of Bax with antiapoptotic proteins, occur in the
brain (15,16). Bax is then oligomerized and
activated, eventually triggering the release of apoptotic proteins
stored in the mitochondrial intermembrane space, resulting in
neuronal apoptosis (17).
Considering that inflammatory changes occur during
the acute phase of ischemic stroke, and that inflammation serves a
central role in the disease outcome, the use of anti-inflammatory
treatment agents may benefit patients suffering an ischemic stroke.
Thus, the development of anti-inflammatory drugs is required for
the recovery from stroke. Sanguinarine is known to be an effective,
naturally active, anti-inflammatory agent. Therefore, the current
report investigated the in vivo effect of sanguinarine
treatment in an animal model of middle cerebral artery occlusion
(MCAO). The findings provide an insight into the
sanguinarine-dependent anti-inflammatory and anti-apoptotic
activities in brain injury.
Materials and methods
Animals
A total of 24 male adult Sprague-Dawley rats (age,
8–10 weeks; weight, 240–260 g) were provided by the Lab Animal
Center of The Fourth Military Medical University (Xi'an, China) and
housed in polypropylene cages in an air-conditioned room (24°C, 50%
humidity) with a 12-h dark:light cycle, allowing free access to
pelleted diet and water. There were three groups in total, each
with 8 rats. All experiments were performed in accordance with the
Guidelines for Animal Research of The Fourth Military Medical
University. The study was approved by the Ethics Committee of
Medical Ethics and the Human Clinical Trial Committee of Xijing
Hospital (approval no. XJYYLL-2015694).
Reagents
Sanguinarine was purchased from Shaanxi Huike
Botanical Development Co., Ltd (Xi'an, China). Triphenyl
tetrazolium chloride (TTC) was purchased from Amresco, LLC (Solon,
OH, USA) and was dissolved in phosphate buffered saline (PBS) at 1%
(m/v). All ELISA kits for IL-1β (cat no. CSB-E08055r), IL-6 (cat
no. CSB-E04640r) and TNF-α (cat no. CSB-E11987r) were purchased
from Cusabio Biotech Co., Ltd. (Wuhan, China). All antibodies were
purchased from Proteintech (Wuhan, China). The enhanced
chemiluminescence kit was purchased from EMD Millipore (cat no.
WBKLS0100; Billerica, MA, USA).
MCAO animal model
The MCAO model was established in male
Sprague-Dawley rats as previously described (18,19).
Rats were anesthetized using 10% chloral hydrate (Dalian Meilun
Biotech Co., Ltd., Dalian, China) throughout the surgery. MCAO was
maintained for 2 h, followed by reperfusion for 24 h (20). Sanguinarine was suspended in 0.5%
carboxymethyl cellulose (CMC)-Na (Tianguan, Guangzhou, China) and
rats were administered a dose of 15 mg/kg intragastrically. For the
vehicle-treated group, equal volumes of 0.5% CMC-Na were
administered. In the vehicle-treated group, the same volume of 0.5%
CMC-Na was administered 1 h prior to MCAO. Rats were anesthetized
with chloral hydrate and decapitated 24 h after MCAO.
Neurological evaluation
Modified neurological severity score (mNSS) was
determined 1 day after MCAO by two independent observers. All
assessments were performed in triplicate. This scoring included
evaluation of the balance, sensory, reflex and motor of rats, and
scores were graded on a scale of 0–18 (21). A higher score represents a more
severe injury (normal = 0; maximal deficit = 18).
Measurement of infarct volume
Rats were anesthetized with 10% chloral hydrate and
decapitated following reperfusion for 24 h. Brains were rapidly and
carefully removed, and sliced into 2-mm continuous slices using a
metallic brain matrix (Xinruan Informatlon Technology Co. Ltd.,
Shanghai, China). The slices were stained with 1% TTC at 37°C for
15 min in the dark, then fixed with 4% formaldehyde in PBS. The
unstained waxy area of the brain slice was defined as infarction,
and the infarct volume ratio was measured and calculated as
described previously (22).
Nissl stain of rat brain
The rats treated by ischemia reperfusion after MCAO
and sustained for 24 h, then anesthetized with 10% chloral hydrate,
and processed by transcardial perfusion with PBS and then with 10%
neutral-buffered formalin. Next, the brains were removed and
immersed in 10% fresh neutral-buffered formalin for 24 h and
embedded in paraffin. The brains were then cut into 2 mm thick
sections, dewaxed, rehydrated with xylene and ethanol and stained
with 0.5% (m/v) Toluidine Blue (Sigma-Aldrich, St. Louis, MO, USA).
Nissl bodies were visualized with an Eclipse Ti-U Inverted
Microscope System (Nikon Corporation, Tokyo, Japan) and counted
using Image-Pro Plus version 6.0 (Media Cybernetics, Inc.,
Rockville, MD, USA).
ELISA of TNF-α, IL-6 and IL-1β
The injured areas of the brain tissue were removed
24 h after ischemia/reperfusion (I/R) injury, washed in cold PBS
and placed into a homogenate tube. Appropriate volume of PBS were
added into the tubes at 4°C, to allow for the tissues to be ground
into 10% homogenate. The supernatant was collected following
centrifugation at 4,000 × g for 15 min. The protein levels
of TNF-α (cat no. CSB-E11987r), IL-6 (cat no. CSB-E04640r) and
IL-1β (cat no. CSB-E08055r) were determined using ELISA kits
(Cusabio Biotech Co., Ltd.) according to the manufacturer's
instructions, which included the addition of 100 µl of
appropriately diluted samples to each well. Standards (triplicates)
and blanks were run with each plate to ensure accuracy
Western blotting assay
The injured area of the brain tissue was homogenized
in cold radioimmunoprecipitation assay buffer (Sigma-Aldrich). The
concentrations of whole cell extracts were determined by
bicinchoninic acid assay (Thermo Fisher Scientific, Inc., Waltham,
MA, USA) and 20 µg total proteins were loaded into each well.
Protein extracts were subjected to electrophoresis on a 10%
Bis-Tris protein gel (Invitrogen; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA). The membranes were incubated with the following
primary antibodies: Rabbit anti-Bax polyclonal antibody (1:500; cat
no. 50599-2-Ig), rabbit anti-Bcl-2 polyclonal antibody (1:500; cat
no. 12789-1-AP), mouse anti-GAPDH monoclonal antibody (1:1,000; cat
no. 60004-1-Ig). The horseradish peroxidase-conjugated goat
anti-mouse/rabbit IgG were used to detect the primary antibodies.
Subsequently, enhanced chemiluminescence reagent was added. The
respective densities of western blots were analyzed using Quantity
One 1-D Analysis Software (version 4.4; Bio-Rad Laboratories, Inc.,
Hercules, CA, USA).
Statistical analysis
Data are expressed as the mean ± standard error.
Multiple group comparisons were performed using one-way analysis of
variance followed by Dunnett's test in order to detect inter-group
differences. The difference between the mean values of two groups
was assessed using a non-paired Student's t-test. SPSS version 12
(SPSS, Inc., Chicago, IL, USA) and GraphPad Prism (GraphPad
Software, Inc., La Jolla, CA, USA) were used to perform all
statistical analyses. All experiments were independently repeated
three times. P<0.05 were considered to indicate a statistically
significant difference.
Results
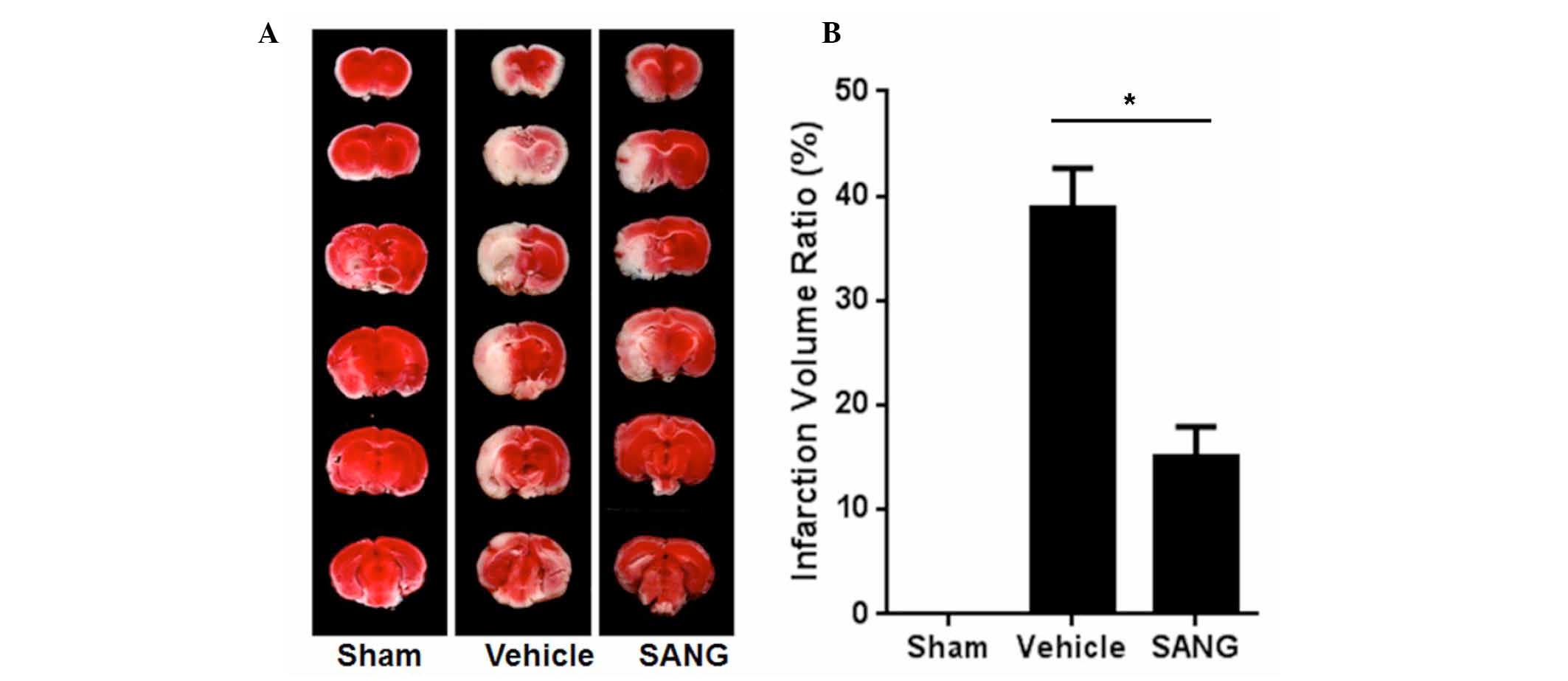
Sanguinarine reduced infarct injury in
MCAO rats
Fig. 1 presents
representative brain slices stained with TTC 24 h after reperfusion
in vehicle- and sanguinarine-treated rats. Infarct volumes were
expressed as a percentage of the intact contralateral hemisphere,
and were found to be significantly lower in sanguinarine-treated
rats (15.03%), when compared with the infarct volumes of
vehicle-treated animals (38.76%; P<0.05) in the transient
ischemic model of stroke.
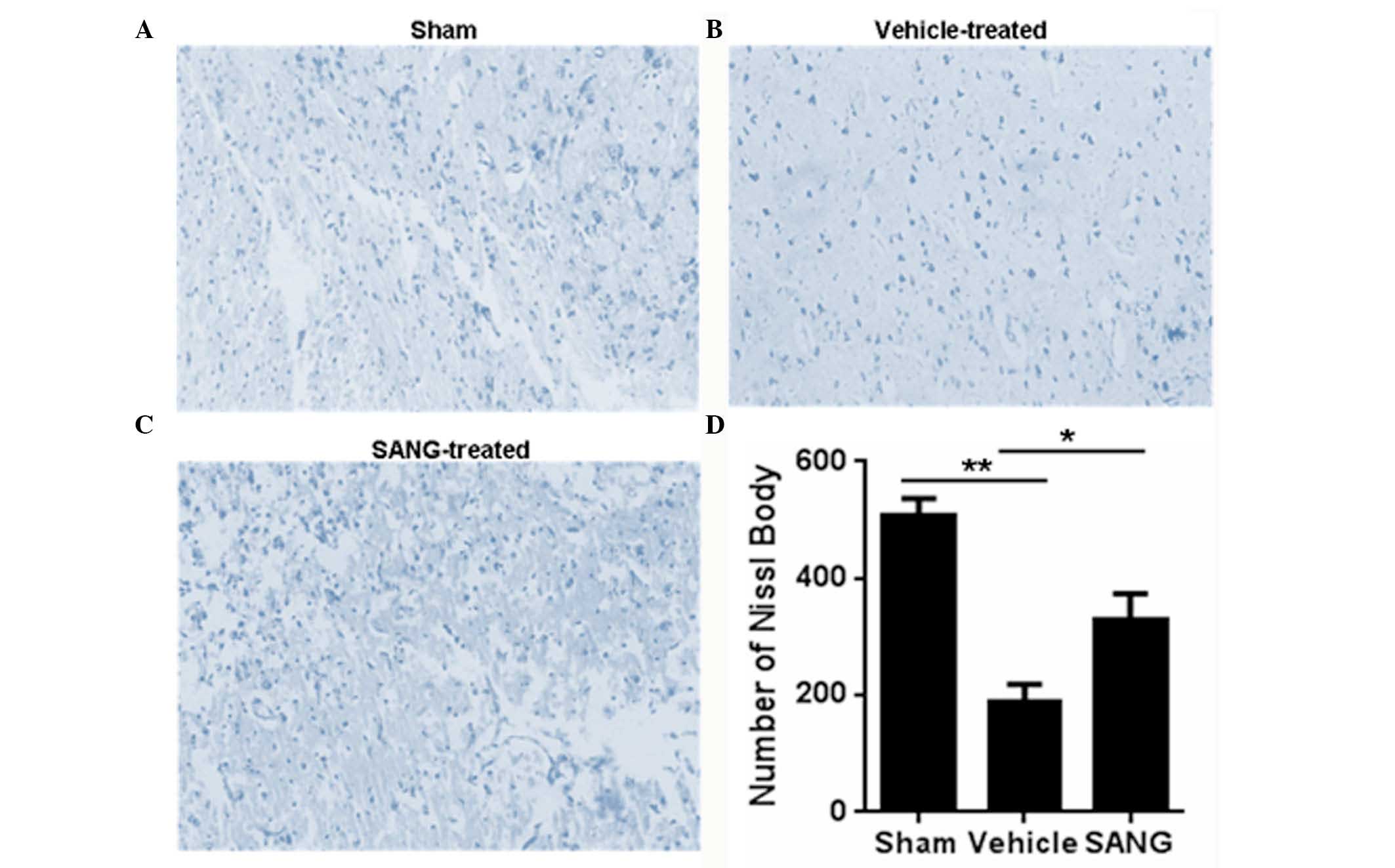
Nissl staining was also investigated in brain
samples from the three groups. The number of Nissl bodies was
significantly reduced following MCAO (vehicle group), when compared
with the sham group (189.33±29.41 vs. 506.00±30.83, respectively;
P<0.01; Fig. 2). Treatment with
sanguinarine significantly increased the number of Nissl bodies
(328.00±45.77) when compared with that in the vehicle-treated rats
(189.33±29.41; P<0.05).
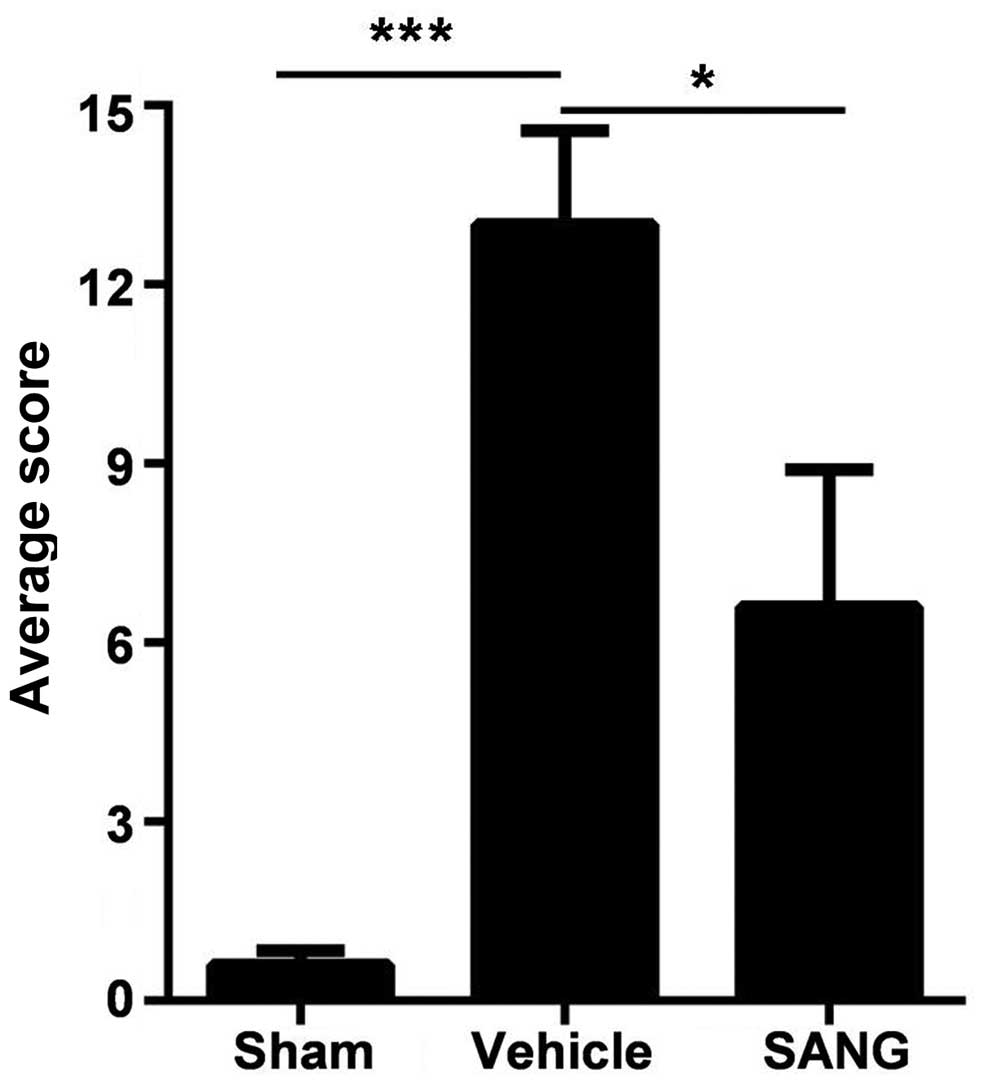
Sanguinarine improves functional
outcome following MCAO
Prior to MCAO, the neurologic scores were normal in
all animals (score = 0 in all groups). High-grade behavioral
deficits (scores >12) were recorded in all animals 60 min after
MCAO (Fig. 3). Vehicle-treated
animals exhibited severe behavioral impairments throughout the
survival period including circling to the right, and the inability
to balance and walk successfully on the beam. Treatment with
sanguinarine significantly improved the neurologic score in
comparison with the vehicle-treated rats 24 h after reperfusion
(P<0.05; Fig. 3).
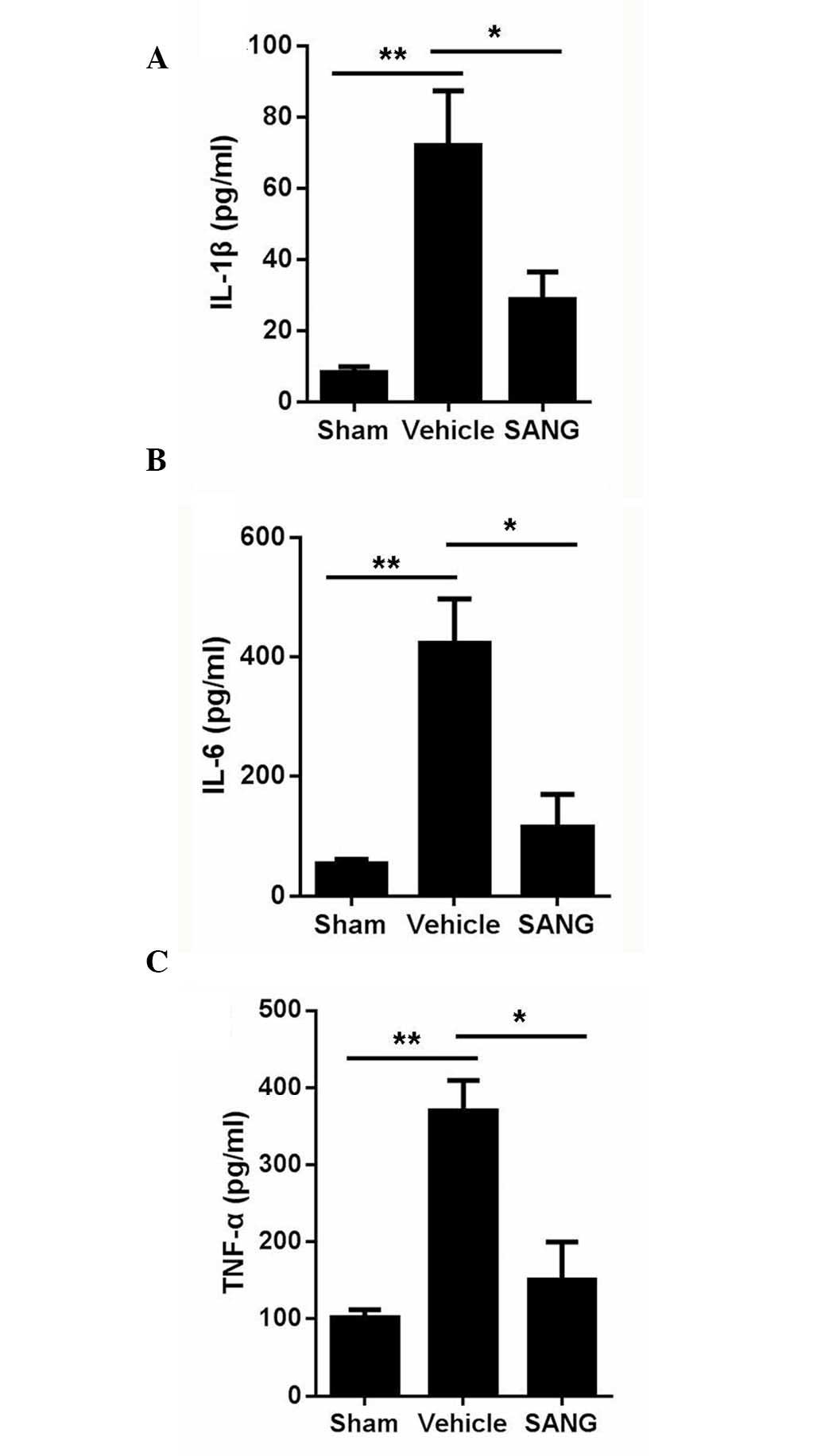
Sanguinarine suppresses the
inflammation caused by global cerebral I/R
ELISA was performed to detect the contents of TNF-α,
IL-6 and IL-1β in injured brain tissue. Compared with brain tissues
obtained from sham-operated animals, global cerebral I/R brains had
a significant higher expression level of TNF-α, IL-6 and IL-1β
proteins (Fig. 4). Pre-treatment
with sanguinarine significantly attenuated the increase in the
TNF-α, IL-6 and IL-1β protein expression levels following global
cerebral I/R (Fig. 4).
Sanguinarine reduces the activation of
apoptotic signaling caused by global cerebral I/R
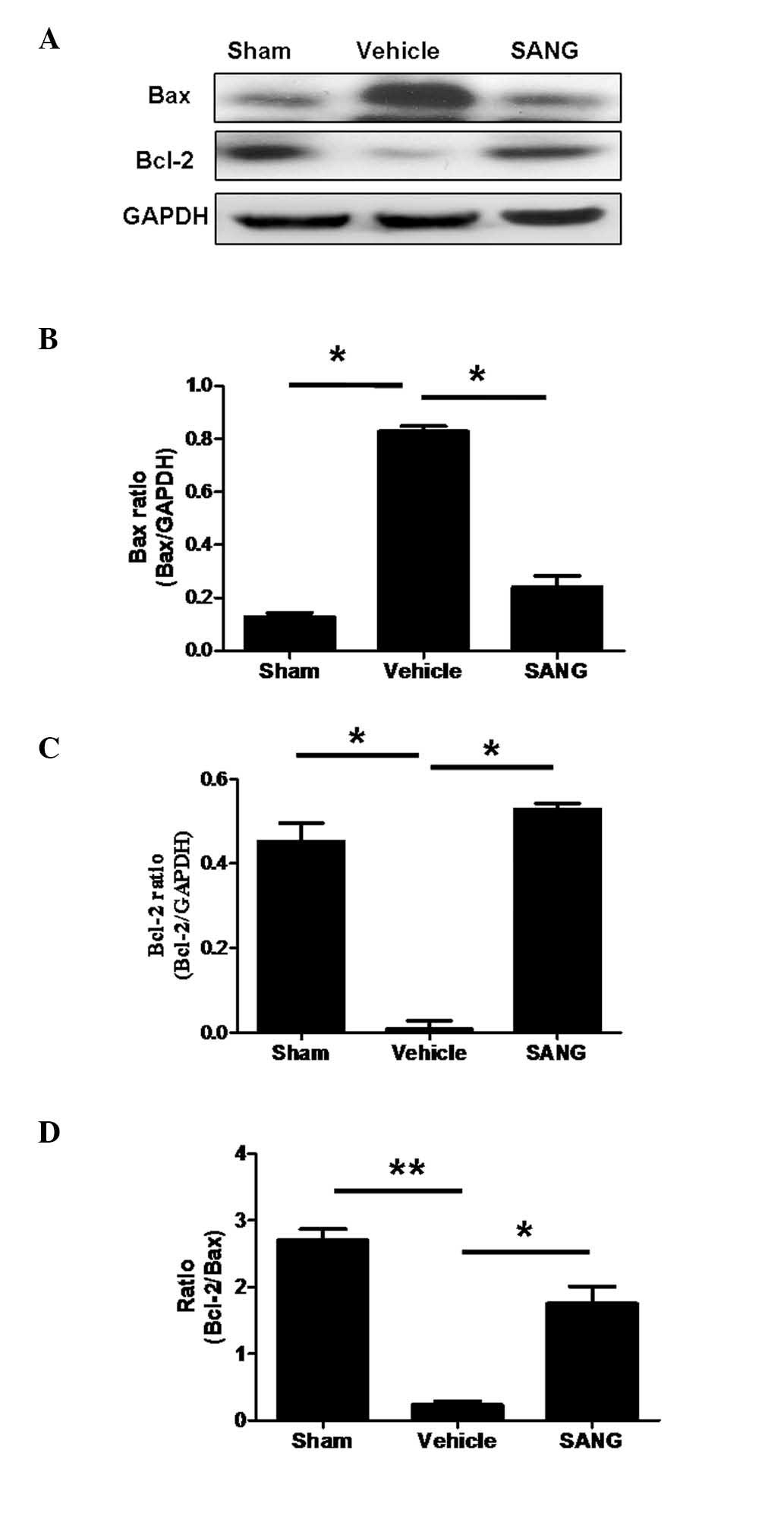
To investigate apoptotic signaling, the expression
of the anti-apoptotic protein Bcl-2 and the pro-apoptotic protein
Bax was investigated. The ratio of Bcl-2/Bax is presented in
Fig. 5. Global cerebral I/R injury
resulted in a significant reduction in Bcl-2 protein expression in
comparison with the sham-operated group. In addition, treatment of
sanguinarine significantly increased the reduced Bcl-2 expression
(P<0.05). By contrast, Bax protein expression following global
cerebral I/R was significantly increased in comparison with
sham-operated animals. This increase in Bax protein expression was
significantly ameliorated by pre-treatment with sanguinarine.
Discussion
Inflammation is a pathological marker of ischemic
stroke and results in cerebric lesion; however, the mechanisms
underlying this process are poorly understood (23). The central nervous and immune system
interact in complex ways. The destruction of neurons induced by
cerebral ischemia results in an immune response that is necessary
to remove cell debris and initiate the regenerative process;
however, this inflammatory response can aggravate cerebral damage
and cause secondary cerebral injuries (24,25).
Circulating inflammatory mediators can activate the cerebrovascular
endothelium and glial cells in the brain and affect ischemic brain
injury (26). Cytokines are
important inflammatory mediators (27,28) and
their role has been well established in previous in vivo and
in vitro investigations. Ischemic injury results in an
increase in the release of cytokines, which are involved in the
necrosis of neuronal cells (27,28).
Among the large number of cytokines, TNF-α, IL-1β and IL-6 modulate
tissue injury in stroke, and are therefore potential targets in
developing treatments for stroke (29). The effect of cytokines on the extent
of infarction depends on their viability in ischemic penumbra
during the early phase of stoke (28). Numerous neuroprotective agents have
been found to be effective in animal models of stroke; however, few
studies have translated these findings into clinical applications.
One reason for this may be the failure to consider clinical
co-morbidities and risk factors in experimental animal models
(27).
As an efficient anti-inflammatory agent,
sanguinarine has been used for centuries as a therapeutic agent for
the treatment of inflammatory diseases (1); however, the protective effect of
sanguinarine on cerebral ischemia is poorly reported. In the
present study, the effect of sanguinarine on MCAO rats was
examined, and its therapeutic action was investigated in a
well-controlled animal model of MCAO. The results demonstrated that
pre-treatment with sanguinarine prevents delayed neuronal death in
the MCAO model. In addition, it was observed that pre-treatment
with sanguinarine was neuroprotective in transient cerebral
ischemia in rats, as the infarct volume of MCAO rats was found to
be significantly reduced in the sanguinarine-treated group. The
injury of brain structure was also declined in the
sanguinarine-treated group.
The mechanism of action of sanguinarine was also
investigated in the present study. The results demonstrated that
treatment with 15 mg/kg sanguinarine resulted in a significant
reduction in cerebral infarction in MCAO-induced rats with
permanent focal cerebral ischemia. In addition, sanguinarine
exerted neuroprotective effects against histological injury and
neurological deficits following ischemia. The expression of Bcl-2
increased, while that of Bax was reduced, and the release of
inflammatory cytokines TNF-α, IL-1β and IL-6 was reduced following
pre-treatment with sanguinarine.
In conclusion, the present study demonstrated that
sanguinarine treatment mediated a significant protective effect
in vivo. The results suggested that sanguinarine effectively
reduced apoptosis in brain cells following sanguinarine treatment,
since the pro-apoptotic Bax was downregulated and the
anti-apoptotic Bcl-2 was upregulated. The current study contributes
towards the understanding of the protective properties of
sanguinarine in MCAO animal models and the molecular mechanisms
underlying this activity. Thus, to the best of our knowledge, this
study provided the first scientific support for the use of
sanguinarine for the treatment of human cerebral ischemia
disease.
References
|
1
|
Niu X, Fan T, Li W, Xing W and Huang H:
The anti-inflammatory effects of sanguinarine and its modulation of
inflammatory mediators from peritoneal macrophages. Eur J
Pharmacol. 689:262–269. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Li H, Zhai Z, Liu G, Tang T, Lin Z, Zheng
M, Qin A and Dai K: Sanguinarine inhibits osteoclast formation and
bone resorption via suppressing RANKL-induced activation of
NF-kappaB and ERK signaling pathways. Biochem Biophys Res Commun.
430:951–956. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mitscher LA, Drake S, Gollapudi SR and
Okwute SK: A modern look at folkloric use of anti-infective agents.
J Nat Prod. 50:1025–1040. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Obiang-Obounou BW, Kang OH, Choi JG, Keum
JH, Kim SB, Mun SH, Shin DW, Kim KW, Park CB, Kim YG, et al: The
mechanism of action of sanguinarine against methicillin-resistant
staphylococcus aureus. J Toxicol Sci. 36:277–283. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lee JS, Jung WK, Jeong MH, Yoon TR and Kim
HK: Sanguinarine induces apoptosis of HT-29 human colon cancer
cells via the regulation of Bax/Bcl-2 ratio and caspase-9-dependent
pathway. Int J Toxicol. 31:70–77. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sun M, Lou W, Chun JY, Cho DS, Nadiminty
N, Evans CP, Chen J, Yue J, Zhou Q and Gao AC: Sanguinarine
suppresses prostate tumor growth and inhibits survivin expression.
Genes Cancer. 1:283–292. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kim S, Lee TJ, Leem J, Choi KS, Park JW
and Kwon TK: Sanguinarine-induced apoptosis: Generation of ROS,
down-regulation of Bcl-2, c-FLIP and synergy with TRAIL. J Cell
Biochem. 104:895–907. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen Y, Zhang L, Ni J, Wang X, Cheng J, Li
Y, Zhen X, Cao T and Jia J: LLDT-8 protects against cerebral
ischemia/reperfusion injury by suppressing post-stroke
inflammation. J Pharmacol Sci. 131:131–137. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shim R and Wong CHY: Ischemia,
Immunosuppression and Infection--Tackling the Predicaments of
Post-Stroke Complications. Int J Mol Sci. 17:642016. View Article : Google Scholar
|
|
10
|
Broughton BR, Reutens DC and Sobey CG:
Apoptotic mechanisms after cerebral ischemia. Stroke. 40:e331–e339.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dirnagl U, Iadecola C and Moskowitz MA:
Pathobiology of ischaemic stroke: An integrated view. Trends
Neurosci. 22:391–397. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Murakami A, Nakamura Y, Tanaka T, Kawabata
K, Takahashi D, Koshimizu K and Ohigashi H: Suppression by citrus
auraptene of phorbol ester-and endotoxin-induced inflammatory
responses: Role of attenuation of leukocyte activation.
Carcinogenesis. 21:1843–1850. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Farhoudi M, Najafi-Nesheli M, Hashemilar
M, Mahmoodpoor A, Sharifipour E, Baradaran B, Taheraghdam A,
Savadi-Oskouei D, Sadeghi-Bazargani H, Sadeghi-Hokmabadi E, et al:
Effect of IMOD™ on the inflammatory process after acute ischemic
stroke: A randomized clinical trial. Daru. 21:262013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Niizuma K, Yoshioka H, Chen H, Kim GS,
Jung JE, Katsu M, Okami N and Chan PH: Mitochondrial and apoptotic
neuronal death signaling pathways in cerebral ischemia. Biochim
Biophys Acta. 1802:92–99. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Saito A, Hayashi T, Okuno S, Ferrand-Drake
M and Chan PH: Overexpression of copper/zinc superoxide dismutase
in transgenic mice protects against neuronal cell death after
transient focal ischemia by blocking activation of the bad cell
death signaling pathway. J Neurosci. 23:1710–1718. 2003.PubMed/NCBI
|
|
16
|
Kirkland RA, Windelborn JA, Kasprzak JM
and Franklin JL: A bax-induced pro-oxidant state is critical for
cytochrome c release during programmed neuronal death. J Neurosci.
22:6480–6490. 2002.PubMed/NCBI
|
|
17
|
Fiskum G, Murphy AN and Beal MF:
Mitochondria in neurodegeneration: Acute ischemia and chronic
neurodegenerative diseases. J Cereb Blood Flow Metab. 19:351–369.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Satoh T, Kosaka K, Itoh K, Kobayashi A,
Yamamoto M, Shimojo Y, Kitajima C, Cui J, Kamins J, Okamoto S, et
al: Carnosic acid, a catechol-type electrophilic compound, protects
neurons both in vitro and in vivo through activation of the
Keap1/Nrf2 pathway via S-alkylation of targeted cysteines on Keap1.
J Neurochem. 104:1116–1131. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wang N, Wu L, Cao Y, Wang Y and Zhang Y:
The protective activity of imperatorin in cultured neural cells
exposed to hypoxia re-oxygenation injury via anti-apoptosis.
Fitoterapia. 90:38–43. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hwang SY, Shin JH, Hwang JS, Kim SY, Shin
JA, Oh ES, Oh S, Kim JB, Lee JK and Han IO: Glucosamine exerts a
neuroprotective effect via suppression of inflammation in rat brain
ischemia/reperfusion injury. Glia. 58:1881–1892. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Wang C, Pei A, Chen J, Yu H, Sun ML, Liu
CF and Xu X: A natural coumarin derivative esculetin offers
neuroprotection on cerebral ischemia/reperfusion injury in mice. J
Neurochem. 121:1007–1013. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Denes A, Ferenczi S and Kovács KJ:
Systemic inflammatory challenges compromise survival after
experimental stroke via augmenting brain inflammation, blood- brain
barrier damage and brain oedema independently of infarct size. J
Neuroinflammation. 8:1642011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kamel H and Iadecola C: Brain-immune
interactions and ischemic stroke: Clinical implications. Arch
Neurol. 69:576–581. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Brea D, Sobrino T, Ramos-Cabrer P and
Castillo J: Inflammatory and neuroimmunomodulatory changes in acute
cerebral ischemia. Cerebrovasc Dis. 27:(Suppl 1). S48–S64. 2009.
View Article : Google Scholar
|
|
25
|
Benakis C, Vaslin A, Pasquali C and Hirt
L: Neuroprotection by inhibiting the c-Jun N-terminal kinase
pathway after cerebral ischemia occurs independently of
interleukin-6 and keratinocyte-derived chemokine (KC/CXCL1)
secretion. J Neuroinflammation. 9:762012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hamishehkar H, Beigmohammadi MT, Abdollahi
M, Ahmadi A, Mahmoodpour A, Mirjalili MR, Abrishami R, Khoshayand
MR, Eslami K, Kanani M, et al: Identification of enhanced cytokine
generation following sepsis. Dream of magic bullet for mortality
prediction and therapeutic evaluation. Daru. 18:155–162.
2010.PubMed/NCBI
|
|
27
|
Lambertsen KL, Biber K and Finsen B:
Inflammatory cytokines in experimental and human stroke. J Cereb
Blood Flow Metab. 32:1677–1698. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Pradillo JM, Denes A, Greenhalgh AD,
Boutin H, Drake C, McColl BW, Barton E, Proctor SD, Russell JC,
Rothwell NJ and Allan SM: Delayed administration of interleukin-1
receptor antagonist reduces ischemic brain damage and inflammation
in comorbid rats. J Cereb Blood Flow Metab. 32:1810–1819. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Xu Y, Wang JY, Song XH, Qu LD, Wei RL, He
FP, Wang K and Luo BY: RIP3 induces ischemic neuronal DNA
degradation and programmed necrosis in rat via AIF. Scientific
Reports. 6:293622016. View Article : Google Scholar : PubMed/NCBI
|