Introduction
Since the 1950s, glucocorticoids had been widely
used in clinical practice as an effective means of treating
diseases such as systemic lupus erythematosus, severe acute
respiratory syndrome, and those caused by kidney transplantation,
resulting in an increase in the number of steroid-associated
necrosis of the femoral head (SANFH) cases (1–3). SANFH
is the most common cause of non-traumatic osteonecrosis (2). For the past 40 years, Chinese and
foreign researchers have investigated SANFH; however, its
pathogenesis remains unclear. There are a variety of theories as to
what is associated with the pathogenesis SANFH, including
dyslipidemia, intravascular coagulation, immune complex
deposition-induced arterial inflammation, osteoporosis, venous
stasis-induced intra-bone high pressure and hormonal toxicity of
bone cells. The above theories also did not clearly prove that the
bone cells exhibited necrosis, because no necrosis-specific
inflammatory responses cell swelling were found (4–8).
Therefore, SANFH lacks effective prevention and early treatment
strategies (9). Previous studies
have shown that hormones not only promote the apoptosis of bone
cells, osteoblasts and cartilage cells, but are involved in the
pathological process of femoral head necrosis (10,11). The
present study utilized single low-dose lipopolysaccharide (LPS)
plus methylprednisolone (MPS) to establish a rabbit model of SANFH.
The roles of levodopa (LEV) in cellular apoptosis were observed in
the rabbit model of SANFH, with the aim of providing a basis for
the prevention and early treatment of femoral head necrosis.
Materials and methods
Animals and grouping
A total of 44 healthy Chinese adult rabbits (age,
3.5±0.4 months; 2.5±0.5 kg; half male and half female; provided by
Animal Center of Medical College of Soochow University, Suzhou,
China) were bred in individual cages (20–30°C; 30–70% humidity, 12
h: 12-h light-dark cycle; free access to feed and water). The
present study was carried out in strict accordance with the
recommendations in the Guide for the Care and Use of Laboratory
Animals of the National Institutes of Health. The animal use
protocol was reviewed and approved by the Institutional Animal Care
and Use Committee (IACUC) of Soochow University (Suzhou,
China).
Rabbits were randomly divided into three groups.
Group A (n=15), the model group, was injected with 10 µg/kg LPS
(Escherichia coli serotype 0111:B4; 10 mg; Sigma-Aldrich;
Merck Millipore, Darmstadt, Germany) through the ear vein, and 20
mg/kg MPS (500 mg/bottle; H20060052; Pfizer, Inc., New York, NY,
USA) into the right gluteus 24 h later, for a total of three times
with a 24-h interval between injections. Group B (n=15), the
treatment group, was prepared using the same protocol as the model
group, followed by oral administration of LEV (0.4 g/kg/day;
Shanghai Fuda Pharmaceutical Co., Ltd., Shanghai, China)
immediately after modeling. Group C (n=14), the control group, was
injected with the same volume of normal saline in the same manner
and at the same time points as the above two groups. During the
experiment, all rabbits were injected with penicillin (800,000
U/per rabbit, twice per week; Harbin Pharmaceutical Group Co.,
Ltd., Harbin, China) in order to prevent infection. Following
imaging observation, seven rabbits from each group were sacrificed
via air embolism at the 6th- and 8th-week of the experiment for
subsequent analysis.
Imaging observation
Prior to sacrifice, 10% chloral hydrate (volume
fraction) anesthesia was intraperitoneally injected into the
rabbits, and dual-hip X-ray (V-5000; Phillips Healthcare, DA Best,
The Netherlands) and magnetic resonance imaging (MRI) (0.2T E-Scan;
Esaote Europe BV, Cambridge, UK) were performed to observe whether
there patchy density-reduced shadows were present in the X-ray
images of the rabbit femoral head area. During MRI examination,
rabbits were placed in the supine position, with their lower leg
flexed and fixed with tape. Using a knee coil, conventional SE
sequence T1-weighted imaging was performed [repetition time
(TR)/echo time (TE)=490/14 msec], in addition to T2-weighted
imaging (TR/TE=2632/96 msec), with no interval and the following
parameters: Matrix, 128×256; vision, 14×14 cm; thickness, 3 mm.
T1-weighted images demonstrated spotty, thin-thread and patchy low
signals, and T2-weighted images showed spotty, thin-thread or
patchy low or high signals, which were considered to indicate
femoral head necrosis.
Histopathologic examination
Six or eight weeks later, the rabbits of the three
groups were sacrificed via air embolism, then their bilateral
femoral heads were harvested, split in half along the central
coronal plane, placed in 10% neutral formalin solution for 24-h
fixation and decalcified in 5% dilute nitric acid for one week.
Following dehydration in an alcohol series the femoral heads were
embedded in paraffin, cut into 4-µm-thick slices, dewaxed and
hydrated prior to staining with hematoxylin for 5 min. Following
staining, the slices were hydrated for 10 min, eosin-stained for 2
min, dehydrated, hyalinized and turpentine-mounted before the bone
trabecular structure and changes in the bone cells and bone marrow
fats were observed under a light microscope. Femoral head necrosis
was determined according to the pathological features of empty bone
lacuna numbers and surrounding necrotic bone marrow tissues. Any
region in the slice that was found to exhibit one sign of
osteonecrosis was considered to be positive for SANFH. Pathological
changes in bone cellular necrosis were expressed as the percentage
of empty bone lacunae. At ×100 magnification in 10 randomly
selected high-power fields, the number of empty bone lacunae out of
50 bone lacunae in each field were counted to calculate the
percentage of empty bone lacunae.
Detection of cellular apoptosis
Paraffinized sections of the femoral head were used
to study cellular apoptosis using a terminal deoxynucleotidyl
transferase dUTP nick-end labeling (TUNEL) kit (KGA703; KGI
Biological Technology Development Co., Ltd., Nanjing, China), with
3,3′-daminobenzidine staining. Observed under the microscope, the
nucleus was stained as tan or brown and set as the positive result.
Five fields were randomly selected under ×400 magnification for
observation, the proportion of apoptotic cells in 50% of the vision
field were counted and indicated as the apoptosis index (AI).
Detection of serum insulin-like growth
factor-1 (IGF-1)
Prior to sacrificing the rabbits at the 8th week, 2
ml of blood was harvested from the central ear artery of each
rabbit in each group between 9:00 a.m. and 10:00 a.m. Blood samples
were immediately centrifuged at 4°C (3,600 r/min; 20 min) to
isolate the serum and were stored at −20°C. The serum IGF-1 level
was determined by radioimmunoassay using IGF-1 RIA kits (Shanghai
Sangon Biological Engineering Technology And Service Co., Ltd.,
Shanghai, China) according to manufacturer's instructions.
Statistical analysis
Data were processed using SPSS 13.0 statistical
software (SPSS Inc., Chicago, IL, USA), and expressed as mean ±
standard deviation (x ± s). Analysis of variance was performed, as
was Pearson's correlation analysis and linear regression. P<0.05
was considered to indicate a statistically significant
difference.
Results
General observation
One week after MPS was injected, the rabbits in
groups A and B exhibited gradually increased food intake and
general motor activity. Three weeks after MPS was injected, 50% of
the rabbits in group A exhibited reduced motor activity and
significant weight loss (P<0.05), whereas the rabbits in group B
exhibited normal motor activity without any significant changes in
body weight. One rabbit in groups A and B, respectively, succumbed
to anaphylactic shock 48 h after LPS injection. No mortality was
observed in group C, and the rabbits exhibited good spirits, normal
appetite, shiny fur and normal weight gain.
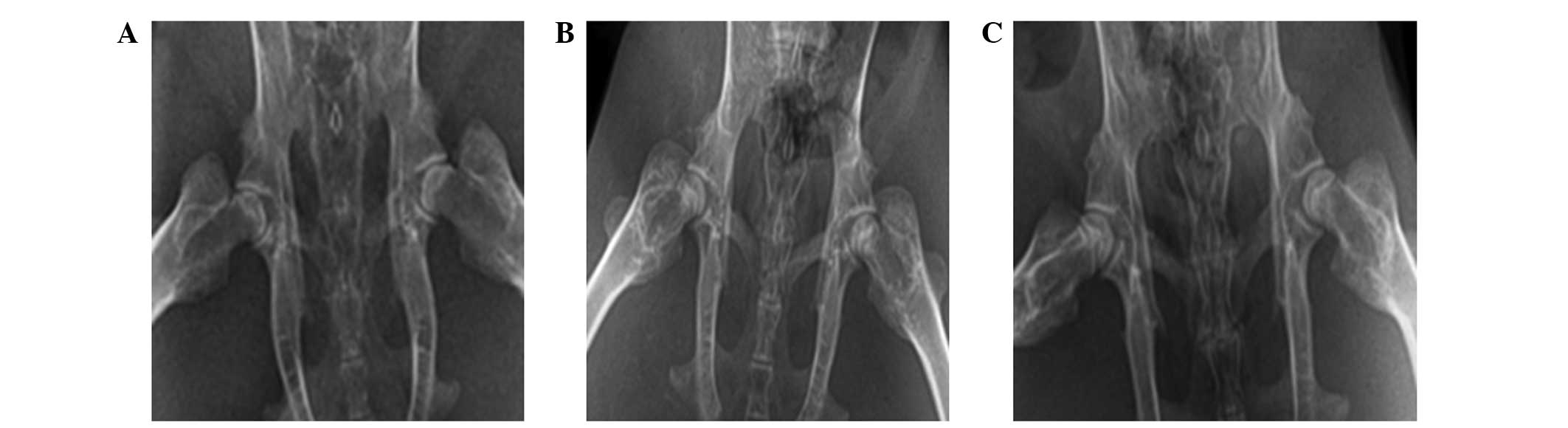
X-ray examination
In group A at the 6th week, dual-hip X-ray
demonstrated a normal femoral head, whereas the bone density was
less uniform, with cystic degeneration. At the 8th week, the
femoral head exhibited partial collapse, the density of the
majority of the femoral bone was uneven, with visible cystic
degeneration or sclerotic bone, or ‘crescent sign’. The joint space
was normal or slightly narrowed, and the bone trabeculae was
partially disrupted. In group B at the 6th week, dual-hip X-ray
demonstrated a normal femoral head with uniform bone density,
without sclerotic bone or cystic degeneration. At the 8th week, the
majority of femoral heads exhibited a normal appearance without
collapse; the bone density was evenly increased without cystic
degeneration or ‘crescent sign’, and the joint space was normal.
Group C exhibited a normal appearance (Fig. 1).
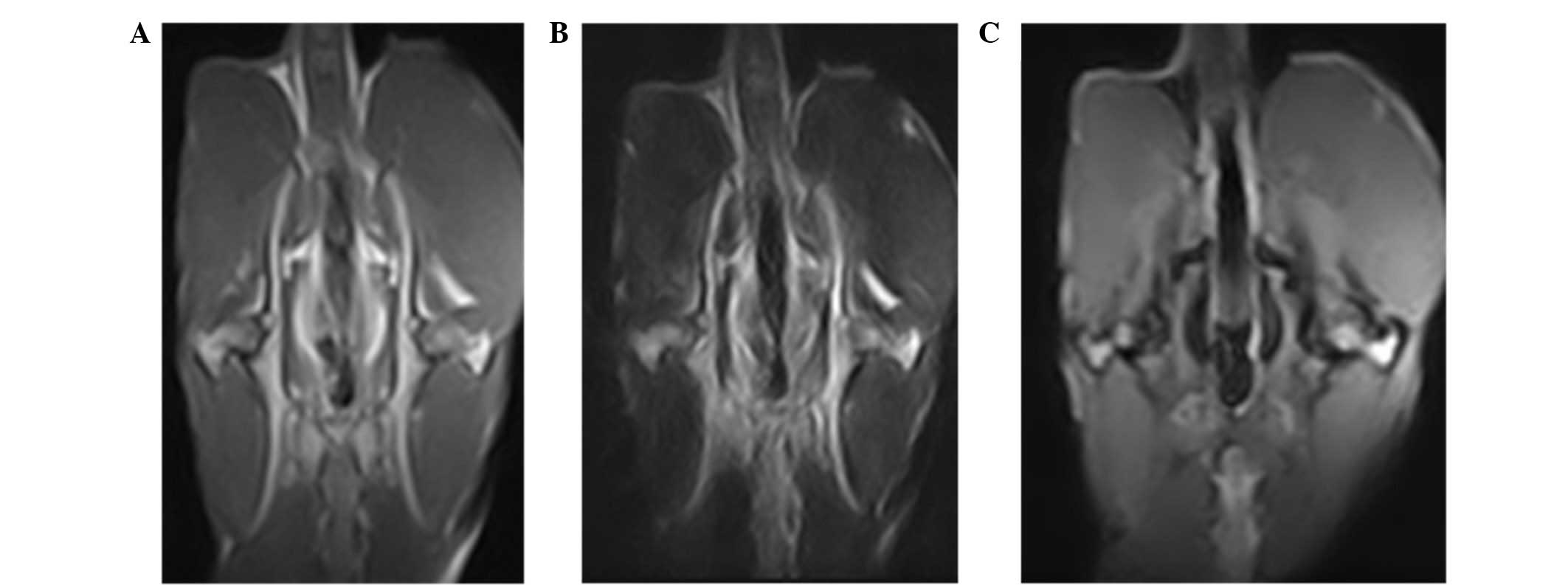
MRI examination
T1-weighted images of groups A (n=11) and B (n=7)
demonstrated that the femoral heads exhibited spotty, thin-thread,
patchy low signals, and the T2-weighted images were also spotty,
thin-thread, patchy high or low signals. Fat-suppression images
were spotty, thin-thread, patchy high signals (Fig. 2). Group C exhibited no abnormal MR
signals.
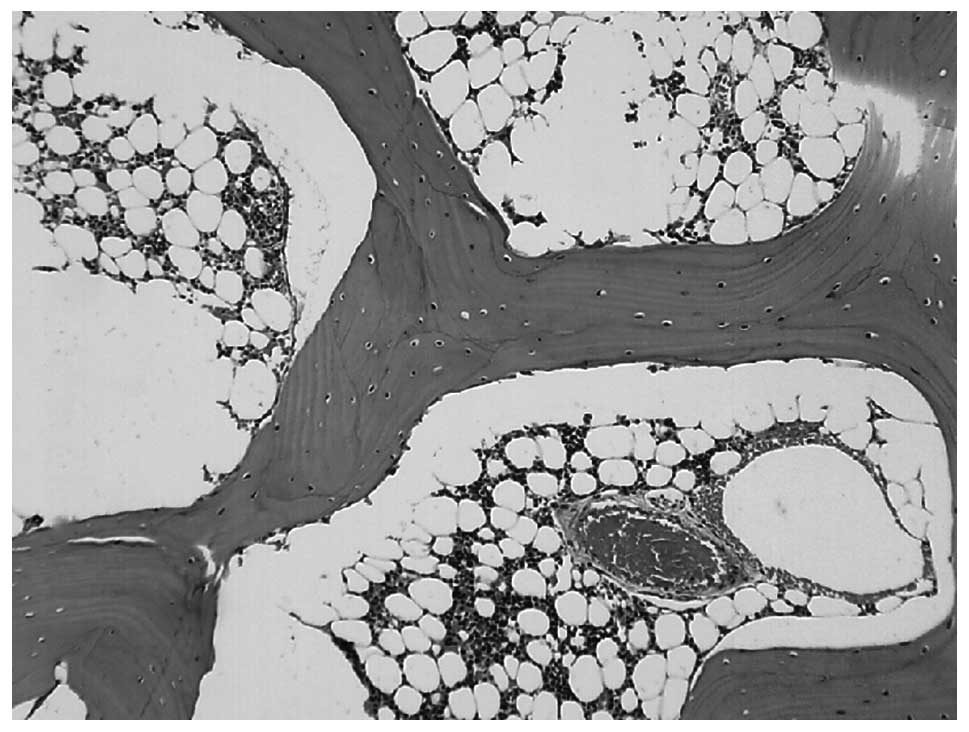
Histopathologic changes
In group A at the 6th week, the bone trabeculae
became thinner, sparser, the intramedullary hematopoietic cells
were decreased, the fat cells proliferated and exhibited
hypertrophy, and partial bone cellular nuclei were deeply stained.
At the 8th week, the subchondral bone plate of the femoral head and
the bone trabeculae became thinner, the continuity was interrupted,
more bone cellular nuclei exhibited karyopyknosis, and the nuclei
were deviated and deeply stained. The changes in the subchondral
bone marrow area included: Large bone marrow fat tissues exhibited
steatosis and dissolved; necrosis was aggravated; intramedullary
vessels were compressed; the lumina was narrowed with visible fat
emboli and thrombosis (Fig. 3);
partial bones exhibited degeneration and necrosis; the number of
normal cells in bone trabeculae were reduced; bone cells
disappeared in the partial bone lacuna; and the empty bone lacuna
were significantly increased (P<0.01), with aggravated vacuole
degrees in bone lacuna. The average rate of empty bone lacunae was
33.86±8.38%.
In group B at weeks 6–8, the bone trabecular
structures were intact and arranged regularly, without continuous
interruption; empty bone lacunae was partially visible, and the
average rate of empty bone lacunae was 25.97±6.29%, which was
higher than the group C control group 11.83±2.45% (P<0.01) and
lower than than group A (P<0.01). Intramedullary blood vessels
were normal, without significant formation of blood clots and fat
embolism, and steatosis of the intramedullary stromal cells was
decreased. In the necrotic areas, fiber tissues repair could be
seen, with increased osteoblasts and capillary proliferation, and
cartilages exhibited obvious bone formation.
Group C exhibited normal integral structures of the
femoral head. The empty bone lacuna rates of the femoral heads of
each group are shown in Table I.
 | Table I.Empty bone lacuna rate and AI of each
group (x±s; n=7). |
Table I.
Empty bone lacuna rate and AI of each
group (x±s; n=7).
|
| 6th week | 8th week |
|---|
|
|
|
|
|---|
| Group | Empty bone lacuna
rate (%) | AI (‰) | Empty bone lacuna
rate (%) | AI (‰) |
|---|
| A |
21.44±4.77a,b |
102.56±18.96a,b |
33.86±8.38a,b |
202.02±18.99a,b |
| B | 13.33±3.06 |
74.93±14.32a |
25.97±6.29a |
120.67±13.13a |
| C | 10.57±3.08 | 47.23±10.12 | 11.83±2.45 | 45.27±12.11 |
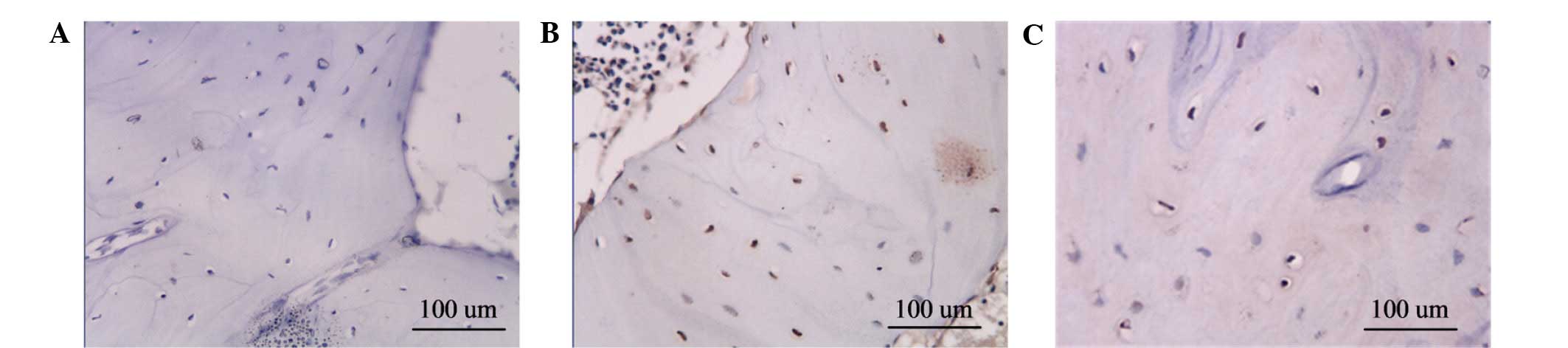
Apoptosis detection
Specimens in group A exhibited the highest rate of
apoptosis of the bone cells, with apoptosis-positive cells
containing brown particles visible in the bone lacuna. A large
number of apoptotic bone cells were observed inside the bone
trabeculae. Group B exhibited moderate apoptosis of the bone cells,
whereas group C exhibited minimal apoptotic bone cells (Fig. 4). The AI of each group is shown in
Table I.
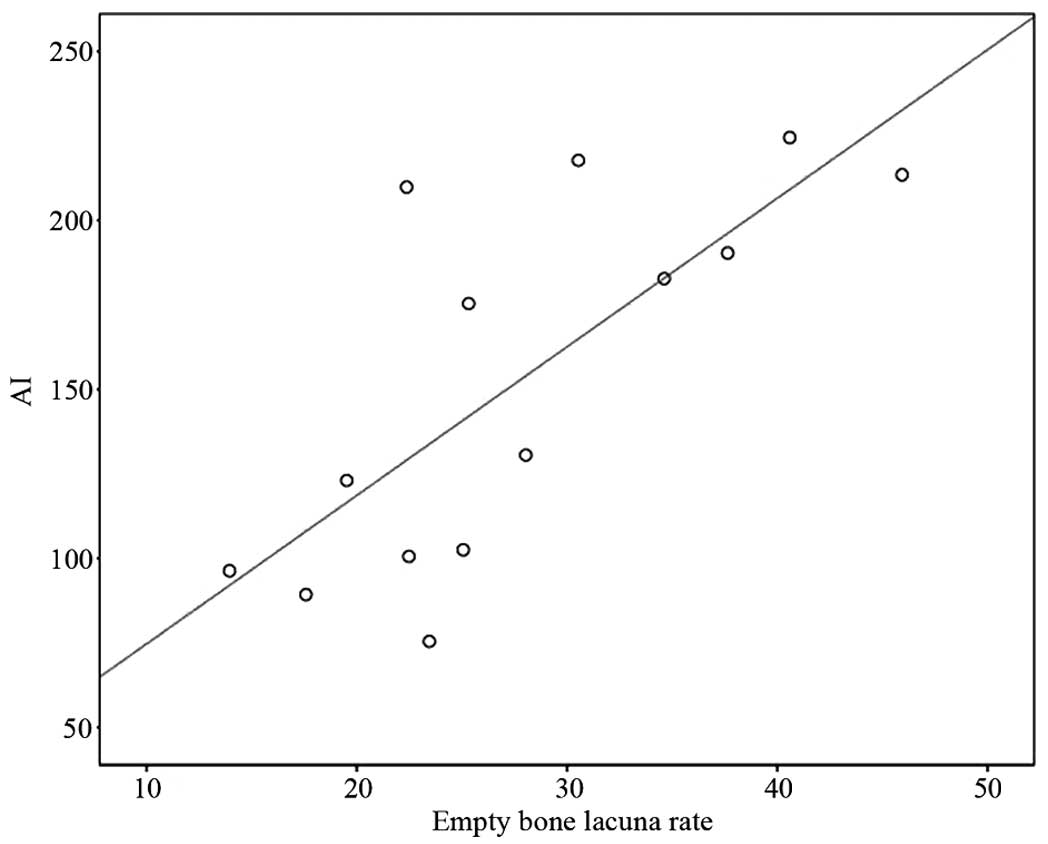
Empty bone lacunae rate and
TUNEL-positive bone cellular apoptosis
Group A exhibited a positive correlation between
TUNEL-positive AI and empty bone lacuna rate, with a coefficient
r=0.74 (P<0.01) and a regression equation of y=30.77+4.39x,
indicating that early SANFH was related with cellular apoptosis in
the present study (Fig. 5).
Serum IGF-1 levels
Serum IGF-1 levels in groups A, B and C were
10.12±2.49, 14.78±2.37 and 7.91±0.85 ng/ml, respectively.
Statistical analysis demonstrated that the differences were
statistically significant (F=20.5558; P<0.01). Comparison
between groups A and C exhibited no statistically significant
difference (P=0.058); whereas the serum IGF-1 content of group B
was significantly higher than that of groups A and C
(P<0.01).
Discussion
Cellular apoptosis was first proposed by Kerr in
1972 (12). Cellular apoptosis is an
active process which has been confirmed to be gene-regulated
programmed cell death, also known as programmed cell death. In a
previous study on this topic, Weinstein et al (13) performed surgical resection of the
femoral head in 14 patients with NFH caused by steroid induction
(n=5), alcoholism (n=3), trauma (n=1) and sickle cell disease
(n=5), and used TUNEL staining to detect the apoptotic cells. The
results revealed that SANFH induced the apoptosis of a large number
of bone cells, whereas patients with alcoholism-induced NFH
exhibited less apoptotic cells, and no apoptotic cells were
detected in the cases of NFH induced by the remaining causes.
Therefore, it was concluded that SANFH was induced by the apoptosis
of bone cells; however, this study was unable to prove the
existence of apoptosis inside the necrotic bone cells of femoral
head. Eberhardt et al (14)
discovered that large doses of hormones were able to cause changes
in cellular viabilities, with apoptosis demonstrated to be the
primary change of SANFH. When bone cellular apoptosis was
widespread, although blood vessels had no significant change, bone
necrosis had already occurred. Calder et al (15) performed an immunohistochemical study
of specimens from patients with non-traumatic osteonecrosis, and
found that the nitric oxide synthase content was increased, which
was considered to be due to the hormone's direct cytotoxic effects,
leading to increased nitric oxide and mediating the occurrence of
apoptosis. It was suggested that the apoptosis of bone cells has an
important role in the pathogenesis of femoral head necrosis. In
addition, it was shown that glucocorticoids are able to affect the
proliferation and differentiation of bone cells, thus affecting the
reconstruction and resorption of bones and decreasing the bone
conversion rate, which further leads to osteoporosis, and the
deposit of apoptotic bone cells (16). Glucocorticoids were recognized as one
of factors that may contribute cellular apoptosis (17), thus promoting the apoptosis of
osteoblasts and bone cells, leading to the reduction of bone cells.
Furthermore, glucocorticoids may also affect the functions of
osteoblasts, thus delaying bone formation and resulting in bone
loss.
The findings of the present study indicated that
apoptotic bone cells were detected in the three groups, and the
number of these apoptotic cells was significantly increased in
group A compared with groups B and C. TUNEL assay analysis
demonstrated that, 6 weeks after medication, the number of
apoptotic bone cells of group A was 102.56±18.96%, which was
significantly higher than group C 47.23±10.12%. As time increased
to 8 weeks after treatment, the number of apoptotic bone cells
increased further, was demonstrated to be positively correlated
with the increasing empty bone lacuna. This phenomenon was most
obvious in the subchondral area, which is consistent with the
changing sites of empty bone lacuna, indicating that bone cellular
apoptosis has an important role in early SANFH. These findings also
suggested that hormones may increase the apoptosis of bone cells,
thus affecting bone metabolism and bone mass changes.
The present study also investigated the
interventional effects of LEV on rabbit SANFH. In a previous study,
Pritchett (18) orally administered
LEV to treat delayed fracture healing, and 84% of patients achieved
fracture healing. Therefore, in the present study LEV was orally
administered to liquid nitrogen-induced experimental NFH animal
models, which indicated that the formation of new bones in the
necrotic areas was higher than in the control group. The present
study was designed to further investigate the mechanism of this
drug.
L-3-(3,4-dihydroxyphenyl) alanine (LEV), which is
the L-isomer of dopa, was absorbed inside the intestine after oral
administration to subsequently peak at a plasma concentration of
1–2 h. When LEV enters the central nervous system, it may increase
the concentration of dopamine at the median eminence, stimulating
dopamine receptors to increase the level of norepinephrine inside
the hypothalamus. The latter would then excite the α-receptor and
promote the release of growth hormone releasing factor, leading to
the increased secretion of growth hormone (GH). GH is able to
promote the synchronic proliferation of proosteoblasts and
osteoblasts in fractures and peri-periosteal cambium layer, thus
accelerating the repair process of NFH (19). In addition, GH promotes the secretion
of IGF-1 and other factors; IGF-1 is able to promote the synthesis
of DNA and RNA in cartilage cells and cell mitosis to accelerate
the speed of cartilaginous ossification. Previous in vitro
studies have shown that IGF-1 inhibits the apoptosis of bone cells
and osteoblasts, inducing the growth and maturation of bones and
cartilages, reducing subendosteal bone resorption, increasing the
net increase of bone mass, and thereby reducing the incidence of
NFH and accelerating the repair process (19).
Hill et al (20) considered that there were a variety of
extracellular signals that may affect the viability of osteoblasts.
For example, lacking GF, IGF and bone nutrients results in
osteoblasts prematurely entering apoptosis; whereas IGF-1, insulin
and basic fibroblast growth factor are able to prevent the
apoptosis of osteoblasts. Tumor necrosis factor-α may promote the
apoptosis of osteoblasts, among which IGF-1 has been demonstrated
to be one of the major growth factors that promotes bone formation.
Glucocorticoids are able to inhibit IGF-1 gene transcription inside
osteoblasts, thereby regulating the expression of IGF-1 in
osteoblasts.
IGF-1 is also a major regulator of anti-apoptotic
signals. Glucocorticoids have been demonstrated to inhibit the
autocrine and (or) paracrine signaling pathways of IGF-1; thus
promoting apoptosis (21,22) and suppressing the formation of
osteoblasts, resulting in reduced bone formation and the
accumulation of apoptotic cells, which subsequently leads to bone
necrosis (23).
The results of the present study demonstrated that
the animals in group B exhibited a more typically shaped femoral
head with no collapse on dual-hip X-ray at the 8th week, and the
bone density was uniformly increased, which was distinct from the
group A. Histopathological analysis showed that the bone trabecular
structures were substantially complete and arranged regularly with
no continuous interruption, although partial empty bone lacunae
were visible. The average rate of empty bone lacunae was
25.97±6.29% in group B, which was significantly lower than group A
(33.86±8.38%) and significantly higher than group C (11.83±2.45%).
The necrotic area exhibited the repair of fibrous tissues; the
osteoblasts were increased, the capillaries were proliferated, and
the osteoblasts were active. These findings showed that LEV was
able to reduce the incidence of NFH; furthermore, LEV accelerated
the repair of necrotic areas. TUNEL assay results demonstrated that
the treatment group exhibited scattered positive cells with brown
particles inside the partial bone nuclei, with AI as 120.67 ±
13.13%, which was significantly lower than that of group A
(202.02±18.99%). These findings suggest that LEV may reduce the
apoptosis of bone cells, thereby preventing NFH. The results showed
that the serum IGF-1 levels in group B were significantly
increased, compared with group A, indicating the biological pathway
of LEV may function through the promotion the synthesis and release
of IGF-1, thus reducing bone cellular apoptosis, reducing the
incidence of NFH, and accelerating the repair of necrotic
areas.
References
|
1
|
Heimann WG and Freiberger RH: Avascular
necrosis of the femoral and humeral heads after high-dosage
corticosteroid therapy. N Eng J Med. 263:672–675. 1960. View Article : Google Scholar
|
|
2
|
LaPorte DM, Mont MA, Mohan V, Jones LC and
Hungerford DS: Multifocal osteonecrosis. J Rheumatol. 25:1968–1974.
1998.PubMed/NCBI
|
|
3
|
Chernetsky SG, Mont MA, LaPorte DM, Jones
LC, Hungerford DS and McCarthy EF: Pathologic features in steroid
and nonsteroid associated osteonecrosis. Clin Orthop Relat Res.
368:149–161. 1999. View Article : Google Scholar
|
|
4
|
Arlet J: Nontraumatic avascular necrosis
of the femoral head. Past, present, and future. Clin Orthop Relat
Res. 277:12–21. 1992.
|
|
5
|
Mont MA and Hungerford DS: Nontraumatic
avascular necrosis of the femoral head. J Bone Joint Surg.
77:459–474. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ono K, Tohjima T and Komazawa T: Risk
factors of avascular necrosis of the femoral head in patients with
systemic lupus erythematosus under high-dose corticosteroid
therapy. Clin Orthop Relat Res. 277:89–97. 1992.
|
|
7
|
Mankin HJ: Nontraumatic necrosis of bone
(osteonecrosis). N Engl J Med. 326:1473–1479. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lavernia CJ, Sierra RJ and Grieco FR:
Osteonecrosis of the femoral head. J Am Acad Orthop Surg.
7:250–261. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cui Q, Wang GJ, Su CC and Balian G: The
Otto Aufranc Award. Lovastatin prevents steroid induced
adipogenesis and osteonecrosis. Clin Orthop Relat Res. 344:8–19.
1997. View Article : Google Scholar
|
|
10
|
Mutijima E, De Maertelaer V, Deprez M,
Malaise M and Hauzeur JP: The apoptosis of osteoblasts and
osteocytes in femoral head osteonecrosis: Its specificity and its
distribution. Clin Rheumatol. 33:1791–1795. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Weinstein RS: Glucocorticoid-induced
osteonecrosis. Endocrine. 41:183–190. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kerr JF, Wyllie AH and Currie AR:
Apoptosis: a basic biological phenomenon with wide ranging
implication in tissue kinetics. Br J Cancer. 26:239–257. 1972.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Weinstein RS, Nicholas RW and Manolagas
SC: Apoptosis of osteocytes in glucocorticoid-induced osteonecrosis
of the hip. J Clin Endecrinol Metab. 85:2907–2912. 2000. View Article : Google Scholar
|
|
14
|
Eberhardt AW, Yeaqer-Jones A and Blair HC:
Regional trabecular bone matrix degeneration and osteocyte death in
femoral of glucocorticoid-treated rabbits. Endocrinology.
142:1333–1340. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Calder JD, Buttery L, Revell PA, Pearse M
and Polak JM: Apoptosis - a significant cause of bone cell death in
osteonecrosis of the femoral head. J Bone Joint Surg Br.
86:1209–1213. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kalb RE, Grossman ME and Hutt C: Avascular
necrosis of bone in dyskeratosis congenita. Am J Med. 80:511–513.
1986. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li Z, Zhang N and Yue D: Experimental
steroid osteonecrosis in rabbits and pathologic findings. Zhonghua
Wai Ke Za Zhi. 33:485–487. 1995.(In Chinese). PubMed/NCBI
|
|
18
|
Pritchett JW: L-dopa in the treatment of
nonunited fractures. Clin Orthop Relat Res. 255:293–300. 1990.
|
|
19
|
DiGirolamo DJ, Mukherjee A, Fulzele K, Gan
Y, Cao X, Frank SJ and Clemens TL: Mode of growth hormone action in
osteoblasts. J Biol Chem. 282:31666–31674. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hill PA, Tumber A and Meikle MC: Multiple
extracellular signals promote osteoblast survival and apoptosis.
Endocrinology. 138:3849–3858. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Delany AM, Durant D and Canalis E:
Glucocorticoid suppression of IGF-I transcription in osteoblasts.
Mol Endocrinol. 15:1781–1789. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mushtaq T and Ahmed SF: The impact of
corticosteroids on growth and bone health. Arch Dis Child.
87:93–96. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Manolagas SC and Weinstein RS: New
developments in the pathogenesis and treatment of steroid-induced
osteoporosis. J Bone Mineral Res. 14:1061–1066. 1999. View Article : Google Scholar
|