Introduction
Tibial fractures account for 3–4% of all fractures,
and are one of the most common types of fractures in older people
(1). With the extension of human
longevity and bone loss, the incidence rate of osteoporosis and
tibial fractures has increased, especially in the aging population,
and has become a serious social problem (2). Open reduction and internal fixation are
usually used for the treatment of tibial fractures. However, a
clinical study found that using tourniquets for long periods of
time caused compression hemostasis, and after the surgery was
completed and the tourniquet was dismantled, patients were often
accompanied by varying degrees of ischemia-reperfusion injury of
the lower extremities (3). The
specific postoperative manifestations included lower limb swelling,
pain, numbness, minor lower limb necrosis, and soft tissue injury,
which severely influenced postoperative recovery and quality of
life of patients (4).
Studies found that when tourniquets were dismantled
and blood supply was restored postoperatively, excessive free
radicals in blood attack cells within the tissues that regained
blood supply, and caused tissue damage (5). This process is known as
ischemia-reperfusion injury. The ability to synthesize
antioxidative enzymes in ischemic tissue that could scavenge free
radicals was impaired, which aggravated tissue injury caused by
free radicals after ischemia and reperfusion. Superoxide dismutase
(SOD) can clear free radicals and has a protective effect against
ischemia-reperfusion injury.
Ischemia-reperfusion injury of the lower extremities
is often accompanied by different levels of release of inflammatory
cytokines from neutrophils (6) such
as interleukin (IL)-6 and TGF-α. In addition, it can decrease SOD
activity in vivo. Therefore, during anesthesia, maintaining
the highest possible levels of SOD activity can help to reduce the
release of inflammatory cytokines and inflammatory cell
infiltration, and therefore represents an important method of
improving the prognosis of patients (7).
Based on previous research, etomidate and propofol
were applied respectively for anesthesia maintenance during surgery
in the two groups of patients with tibial fracture, and the effects
of the two anesthetics on inflammatory factors and SOD activity
were analyzed (8).
Patients and methods
From December 2013 to June 2015, 60 patients with
tibial fractures that conformed with the surgical indications of
open reduction and internal fixation were selected. Patients were
randomly divided into two groups, the observation group and the
control group. There were no significant differences in age, body
mass index (BMI), and gender ratio between the two groups
(P>0.05) (Table I).
 | Table I.Baseline parameters of patients. |
Table I.
Baseline parameters of patients.
| Groups | Cases | Age (years) | BMI
(kg/m2) | Gender ratio
(male/female) |
|---|
| Observation | 30 | 52.4±4.3 | 22.3±2.2 | 24/25 |
| Control | 30 | 49.8±11.2 | 23.2±1.5 | 28/21 |
| T-value | – | 0.87 | 0.44 | 0.41 |
| P-value | – | 0.15 | 0.65 | 0.57 |
Inclusion criteria
The inclusion criteria were as follows: i) Patients
were diagnosed with tibial fractures though clinical and imaging
examinations; ii) age of patients was 18–60 years; and iii) manual
reduction was invalid, or patients were accompanied by tibial
structural damage and manual reduction could not be carried
out.
Exclusion criteria
The exclusion criteria were as follows: i) Patients
taking immunosuppressants; ii) patients with severe and/or chronic
bacterial and/or viral infections; iii) patients with autoimmune
diseases; iv) patients with connective tissue diseases; v) patients
with malignant tumors; vi) patients with liver and kidney
dysfunction; vii) patients with chronic muscle disease; viii)
patients with peripheral vascular disease, chronic heart failure,
thyroid disease, severe trauma that occurred half a year before the
study, and a history of surgery; ix) patients with diabetes; x)
patients with grade III and IV New York Heart Association
classification; xi) hormone replacement therapy or other immune
modulators were given to patients within the past 6 months; xii)
patients and their families could not cooperate; and xiii) patients
with a history of mental illness (2).
Specimen collection
Fasting venous blood (3 ml) was collected in the
early morning and placed in ordinary plastic tubes. Next, 1.8 ml
venous blood was transferred to anticoagulant tubes containing 0.2
ml 3.8% sodium citrate. Specimens were centrifuged (1,200 × g)
within 1 h for 10 min. Serum or plasma were separately extracted
and stored in 0.5 ml Eppendorf tubes at −30°C, and used within 1
month.
Measurement of serum TNF-α, IL-1, and
IL-6 by ELISA
Before surgery (T0), before surgery was completed
and anesthesia was stopped (T1), 24 h after surgery (T3), 48 h
after surgery (T4), and 1 week after surgery (T5), the levels of
tumor necrosis factor (TNF)-α, IL-1, and IL-6 was measured by
enzyme-linked immunosorbent assay (ELISA). All reagents in this
study were from Wuhan Boster Biological Engineering Co. (Wuhan,
China) and used according to the manufacturer's instructions.
Measurement of SOD activity
Before surgery (T0), before surgery was completed
and anesthesia was stopped (T1), 24 h after surgery (T3), 48 h
after surgery (T4), and 1 week after surgery (T5), the measurement
of serum SOD activity was performed strictly in accordance with the
instructions of the SOD kit (Nanjing Institute of Biological
Engineering, Nanjing, China).
Anesthesia
i) For anesthesia induction, the two groups of
patients were treated with remifentanil injection (0.2–0.3 µg/kg),
cisatracurium besilate (500 µg/kg, H20060927; Jiangsu Hengrui
Medicine Co., Ltd., Lianyungang, China), and midazolam injection
(0.5–0.1 mg/kg, H19990027; Jiangsu Enhua Pharmaceutical, Xuzhou,
China). Etomidate (3 mg/kg) was used in the observation group, and
propofol (1 mg/kg) was used in the control group for anesthesia
induction; and ii) for intraoperative maintenance, continuous micro
syringe pump infusion of propofol [3–6 mg/(kg·h)] and remifentanil
(0.1–0.25 µg/kg/min, remifentanil hydrochloride injection, batch
no. of product, 6130314; Humanwell Pharmaceutical Co., Ltd.,
Yichang, China) were applied for intravenous anesthesia in the
control group. Continuous micro syringe pump infusion of etomidate
[3–6 mg/(kg·h); Jiangsu Enhua Pharmaceutical] and remifentanil
(0.1–0.25 µg/kg/min) were applied for intravenous anesthesia in the
observation group.
Statistical analysis
SPSS 20.0 software was used for data analysis. Data
are presented as mean ± standard deviation (SD), independent sample
t-test was used for comparisons between groups, and a paired t-test
was used among groups. P<0.05 was considered statistically
significant.
Results
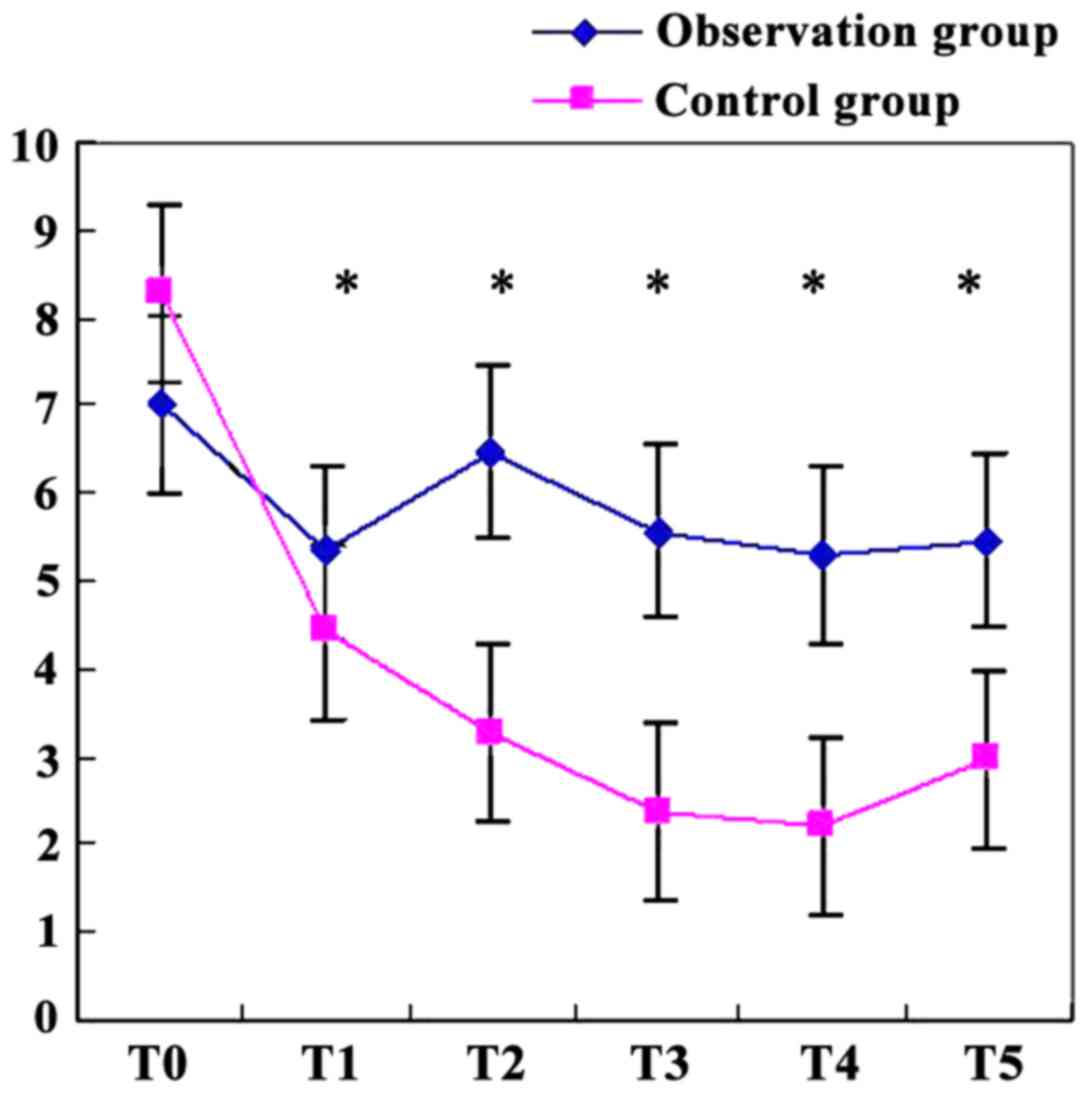
The comparison of serum SOD activity
between the two groups at six time points (mean ± SD)
The serum SOD activity between the two groups at the
six time points were recorded and compared. Beginning at T3, SOD
levels in the control group decreased significantly compared with
the observation group (P<0.05) (Table II and Fig. 1).
 | Table II.The comparison of serum SOD activity
between the two groups at the six time points (mean ± SD). |
Table II.
The comparison of serum SOD activity
between the two groups at the six time points (mean ± SD).
| Groups | Cases | T0 | T1 | T2 | T3 | T4 | T5 |
|---|
| Observation | 30 | 7.02±0.75 | 5.33±2.2 | 6.48±1.38 | 5.58±3.28 | 5.29±0.48 | 5.47±0.82 |
| Control | 30 | 8.27±0.48 | 4.42±1.5 | 3.27±0.58 | 2.37±0.48 | 2.21±0.42 | 2.60±0.47 |
| T-value | – | 0.87 | 0.44 | 19.42 | 10.78 | 12.84 | 11.38 |
| P-value | – | 0.15 | 0.65 | 0.004 | 0.005 | 0.006 | 0.007 |
The comparison of serum levels of
TNF-α, IL-1, and IL-6 between the two groups at six time points
(mean ± SD)
The comparison of the levels of TNF-α, IL-1, and
IL-6 in serum at the six time-points indicated that, beginning from
T2, the serum levels of TNF-α, IL-1, and IL-6 in the observation
group decreased significantly compared with the control group
(P<0.05) (Table III).
 | Table III.The comparison of serum levels of
TNF-α, IL-1, and IL-6 between the two groups at the six time points
(mean ± SD). |
Table III.
The comparison of serum levels of
TNF-α, IL-1, and IL-6 between the two groups at the six time points
(mean ± SD).
| Title | Groups | Cases | T0 | T1 | T2 | T3 | T4 | T5 |
|---|
| TNF-α (ng/ml) | Observation | 30 | 12.02±0.75 | 25.33±2.2 | 16.48±3.8 | 15.58±3.28 | 15.29±4.8 | 10.47±8.2 |
|
| Control | 30 | 13.12±0.48 | 34.42±1.5 | 33.27±5.8 | 22.37±0.48 | 22.21±4.2 | 20.60±4.7 |
|
| T-value | – | 0.87 | 0.24 | 18.42 | 12.78 | 16.84 | 17.38 |
|
| P-value | – | 0.17 | 0.62 | 0.003 | 0.004 | 0.005 | 0.006 |
| IL-1 (ng/ml) | Observation | 30 | 16.13±5.23 | 37.4±1.26 | 20.33±1.33 | 10.68±2.31 | 11.03±0.48 | 9.81±0.38 |
|
| Control | 30 | 15.21±3.28 | 31.5±0.47 | 19.42±1.28 | 15.47±3.28 | 16.32±2.31 | 18.82±2.43 |
|
| T-value | – | 0.34 | 0.67 | 12.47 | 13.23 | 14.37 | 20.38 |
|
| P-value | – | 0.78 | 0.38 | 0.024 | 0.021 | 0.031 | 0.002 |
| IL-6 (ng/ml) | Observation | 30 | 4.33±1.23 | 7.48±3.28 | 4.33±2.14 | 3.24±1.24 | 2.14±2.76 | 3.28±1.29 |
|
| Control | 30 | 4.18±1.33 | 8.48±1.24 | 8.60±1.29 | 9.03±0.48 | 8.74±1.27 | 7.38±2.13 |
|
| T-value | – | 0.61 | 0.52 | 19.32 | 21.25 | 13.24 | 9.84 |
|
| P-value | – | 0.39 | 0.44 | 0.002 | 0.001 | 0.016 | 0.023 |
Comparison of postoperative
complications between the two groups of patients
The postoperative complications of the two groups of
patients were compared, demonstrating that the symptoms, including
lower limb pain, numbness, and coldness, were significantly less in
the observation compared with the control group
(χ2=43.78, P<0.05) (Table
IV).
 | Table IV.The comparison of postoperative
complications between the two groups of patients. |
Table IV.
The comparison of postoperative
complications between the two groups of patients.
| Groups | Cases | Lower limb
pain | Numbness of the
lower limbs | Coldness of the
lower limbs | Normal |
|---|
| Observation | 30 | 2 | 5 | 3 | 39 |
| Control | 30 | 12 | 8 | 3 | 26 |
| χ2
value | – |
| 43.78 |
|
| P-value | – |
| 0.032 |
|
Discussion
Etomidate belongs to the class of nonbarbiturate
intravenous sedatives, and is a form of imidazole derivative used
in general anesthesia (9,10). It is believed that etomidate has a
better protective effect when patients with cardiovascular disease
are under anesthesia for surgery. When using routine clinical
doses, heart rate, mean arterial pressure, mean pulmonary arterial
pressure, pulmonary capillary wedge pressure, central venous
pressure, cardiac stroke volume, cardiac index, pulmonary vascular
resistance, and peripheral vascular resistance between cardiac
patients and normal patients had almost no differences. Etomidate
exerts its pharmacological function through the GABAA
receptors. The hypnotic effects of etomidate are mediated through
the β2 and β3 subunits of GABAA receptors rather than
the α1 subunit, and GABAA receptor antagonists can
antagonize the effects (11,12). In our study, serum SOD activity and
the levels of inflammatory factors of the two groups at six time
points were compared. Compared with the control group, the levels
of serum SOD and TNF-α, IL-1, and IL-6 released by neutrophils
after ischemia-reperfusion injury in the observation group (treated
with etomidate) were significantly decreased (P<0.05). These
results were similar to a previous study, which showed that in
ischemia-reperfusion injury, because of ischemia, the levels of
IL-10 and TNF-α increased, which can increase T lymphocyte
infiltration (13). SOD activity was
also an important factor. SOD is an active substance derived from
cells, that can eliminate harmful substances produced during
metabolic processes, and has an anti-aging effect. After tibial
fracture, because of ischemia and hypoxia, a large amount of
oxygen-free radical are generated in local tissue and in
circulation. SOD is a primary substance that scavenges reactive
oxygen species (ROS) (14). We found
that ROS levels increased significantly in patients with tibial
fracture, which may be related to ischemia-reperfusion injury after
using tourniquets for a long period of time.
Yu et al found that etomidate had a
protective effect on ischemia-reperfusion injury of the spinal cord
induced by interruption of the rabbit aorta (15). Ergün et al found that
anesthetic doses of propofol, ketamine, and etomidate had
protective effects on ischemia-reperfusion injury of skeletal
muscle, and there were no obvious differences between them
(16). However, Harman et al
employed an intrauterine model of hypoxia of fetal rats, simulated
by clamping the ovarian uterine artery of pregnant rats, and
etomidate, midazolam, propofol and other commonly used anesthetic
drugs were used during the intervention. The results indicated that
only propofol and midazolam had neuroprotective effects, and
significant neuroprotective roles of other narcotic drugs were not
observed (17). Yuzer et al
showed that propofol and thiopental can significantly reduce
ischemia-reperfusion injury of the kidney. The protective effects
of these drugs may be attributed to the antioxidant functions of
narcotic drugs. Their results showed that anesthesia with propofol
and thiopental had good effects on improving renal function
(18). We believe the controversy
surrounding these findings may be attributed to surgical
approaches, injury of organs, and ischemia-reperfusion injury,
although further animal studies are required for validation.
We observed that the postoperative length of stay in
hospital of patients in the observation group was significantly
shorter than that of the control group, and the occurrence rate of
anesthesia complications was significantly decreased (P<0.05).
We hypothesized that inflammatory cytokines are released from
ischemia-reperfusion injury of the lower limbs and that the levels
of ROS in the body affect the functions of the lower extremities.
While etomidate had a good effect on reducing the levels of ROS and
the release of inflammatory factors (16–23), the
specific mechanisms still need to be explored by in vivo and
in vitro experiments.
In conclusion, tourniquets are routinely applied for
hemostasis during surgery for open tibial fractures. The
intraoperative use of etomidate for maintaining sedation can
effectively decrease serum SOD levels and the release of
inflammatory factors after ischemia-reperfusion injury. In
addition, it can effectively decrease the occurrence rate of
complications from anesthesia after surgery.
References
|
1
|
Court-Brown CM and McBirnie J: The
epidemiology of tibial fractures. J Bone Joint Surg Br. 77:417–421.
1995.PubMed/NCBI
|
|
2
|
Ludwig M, Hymes RA, Schulman J, Pitta M
and Ramsey L: intramedullary nailing of open tibial fractures:
provisional plate fixation. Orthopedics. 30:1–6. 2016.
|
|
3
|
Brink O: Suprapatellar nailing of tibial
fractures: surgical hints. Curr Orthop Pract. 27:107–112. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fu B: Locked META intramedullary nailing
fixation for tibial fractures via a suprapatellar approach. Indian
J Orthop. 50:283–289. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chopineau J, Sommier MF and Sautou V:
Evaluation of free radical production in an ischaemia-reperfusion
model in the rabbit using a tourniquet. J Pharm Pharmacol.
46:519–520. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dai Y, Jia P, Fang Y, Liu H, Jiao X, He JC
and Ding X: miR-146a is essential for lipopolysaccharide
(LPS)-induced cross-tolerance against kidney ischemia/reperfusion
injury in mice. Sci Rep. 6:270912016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Han JQ, Liu CL, Wang ZY, Liu L, Cheng L
and Fan YD: Anti-inflammatory properties of lipoxin A4 protect
against diabetes mellitus complicated by focal cerebral
ischemia/reperfusion injury. Neural Regen Res. 11:636–640. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhou X: Effects of etomidate or propofol
on inflammation mediators in rabbit with spinal injury. Chin J
Pract Nervous Dis. 13:2010.
|
|
9
|
Sedighinejad A, Nabi B Naderi, Haghighi M,
Biazar G, Imantalab V, Rimaz S and Zaridoost Z: Comparison of the
effects of low-dose midazolam, magnesium sulfate, remifentanil and
low-dose etomidate on prevention of etomidate-induced myoclonus in
orthopedic surgeries. Anesth Pain Med. 6:e353332016.PubMed/NCBI
|
|
10
|
Wang L, Li W, Xu R and Long L: Meta
analysis for the anesthesia effect and adverse reactions of
etomidate and propofol on the painless abortion surgery. Zhong Nan
Da Xue Xue Bao Yi Xue Ban. 41:427–433. 2016.(In Chinese).
PubMed/NCBI
|
|
11
|
Allen C and Washington S: The role of
etomidate as an anaesthetic induction agent for critically ill
patients. Br J Hosp Med (Lond). 77:282–286. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yılmaz Çakirgöz M, Demirel İ, Duran E,
Özer AB, Hancı V, Türkmen ÜA, Aydın A, Ersoy A and Büyükyıldırım A:
Effect of gabapentin pretreatment on myoclonus after etomidate: a
randomized, double-blind, placebo-controlled study. Rev Bras
Anestesiol. 66:356–362. 2016.PubMed/NCBI
|
|
13
|
Patil CN, Wallace K, LaMarca BD, Moulana
M, Lopez-Ruiz A, Soljancic A, Juncos LA, Grande JP and Reckelhoff
JF: Low-dose testosterone protects against renal
ischemia-reperfusion injury by increasing renal IL-10-to-TNF-α
ratio and attenuating T-cell infiltration. Am J Physiol Renal
Physiol. 311:F395–F403. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jiang W, Bian Y, Wang Z and Chang TM:
Hepatoprotective effects of Poly-[hemoglobin-superoxide
dismutase-catalase-carbonic anhydrase] on alcohol-damaged primary
rat hepatocyte culture in vitro. Artif Cells Nanomed Biotechnol.
5:1–5. 2016.
|
|
15
|
Yu Q, Zhou Q, Huang H, Wang Y, Tian S and
Duan D: Protective effect of etomidate on spinal cord
ischemia-reperfusion injury induced by aortic occlusion in rabbits.
Ann Vasc Surg. 24:225–232. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ergün Y, Darendeli S, Imrek S, Kilinç M
and Oksüz H: The comparison of the effects of anesthetic doses of
ketamine, propofol, and etomidate on ischemia-reperfusion injury in
skeletal muscle. Fundam Clin Pharmacol. 24:215–222. 2010.PubMed/NCBI
|
|
17
|
Harman F, Hasturk AE, Yaman M, Arca T,
Kilinc K, Sargon MF and Kaptanoglu E: Neuroprotective effects of
propofol, thiopental, etomidate, and midazolam in fetal rat brain
in ischemia-reperfusion model. Childs Nerv Syst. 28:1055–1062.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yuzer H, Yuzbasioglu MF, Ciralik H,
Kurutas EB, Ozkan OV, Bulbuloglu E, Atli Y, Erdogan O and Kale IT:
Effects of intravenous anesthetics on renal ischemia/reperfusion
injury. Ren Fail. 31:290–296. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tvrdá E, Tušimová E, Kováčik A, Paál D,
Libová Ľ and Lukáč N: Protective effects of quercetin on selected
oxidative biomarkers in bovine spermatozoa subjected to ferrous
ascorbate. Reprod Domest Anim. 51:524–537. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhou X, Xu Y, Xie Z, Xu S and Bi J:
Association of extracellular superoxide dismutase gene methylation
with cerebral infarction. Zhonghua Yi Xue Yi Chuan Xue Za Zhi.
33:378–382. 2016.(In Chinese). PubMed/NCBI
|
|
21
|
Álvarez-Zaldiernas C, Lu J, Zheng Y, Yang
H, Blasi J, Solsona C and Holmgren A: Cellular redox systems impact
the aggregation of Cu, Zn Superoxide dismutase linked to familial
amyotrophic lateral sclerosis. J Biol Chem. 291:17197–17208. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bhasker TV, Gowda NK, Mondal S,
Krishnamoorthy P, Pal DT, Mor A, Bhat SK and Pattanaik AK: Boron
influences immune and antioxidant responses by modulating hepatic
superoxide dismutase activity under calcium deficit abiotic stress
in Wistar rats. J Trace Elem Med Biol. 36:73–79. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhao Y, Zhao E, Zhang C and Zhang H: Study
of the changes of acrosomal enzyme, nitric oxide synthase, and
superoxide dismutase of infertile patients with positive antisperm
antibody in seminal plasma. Cell Biochem Biophys. 73:639–642. 2015.
View Article : Google Scholar : PubMed/NCBI
|