Introduction
With the ongoing economic development, changes in
lifestyle and an aging population, diabetes mellitus is currently
among the most prevalent chronic diseases in the world. Apart from
micro- and macro-vascular diabetic complications, the
susceptibility of diabetics to infections, e.g., with bacteria or
fungi, has shown yearly increases (1). Patients with diabetes mellitus are
susceptible to certain pathogens, such as mucor. The present study
presented a case of a type 2 diabetes patient with
rhino-orbito-cerebral (ROC) mucormycosis.
Case report
The present case was approved by the Ethics
Committee of the Second Hospital of Hebei Medical University
(Shijiazhuang, China). Written informed consent was obtained from
the patient for the publication of this study.
A 27-year-old man was admitted to the Department of
Endocrinology of the Second Hospital of Hebei Medical University on
June 2, 2013, complaining of a painful swelling in the left
retro-orbital region and nose for five days. Since the first day of
presenting with these signs, he was unable to open the left eye and
his vision of the left eye and the left papillary light reflex were
lost. The patient had a history of type 2 diabetes mellitus with
uncontrolled blood glucose for two years as well as a family
history of diabetes mellitus.
On admission, the patient was conscious and had an
elevated body temperature of 38.4°C, a blood pressure of 116/78
mmHg and a pulse of 136/min. Apart from the abovementioned signs
and symptoms, the physical and neurological presentation was
normal. The patient's white blood cell count was 21,100 cells/µl
and differential count results were as follows: Neutrophils,
(80.5%; normal range, 40–75%); lymphocytes, (2.4%; normal range,
20–50%); monocytes, (17.1; normal range, 3–10%); eosinophils, (0%;
normal range, 0.4–8%); basophils, (05; normal range, 0–1%). His
hemoglobin was 10.8 g/dl. Other laboratory values, including liver
function, renal function and electrolytes were normal. His random
blood glucose level was 22.4 mmol/l and hemoglobin A1C was 15.7%.
On admission, the patient's urine specimen was positive for acetone
and blood gas analysis confirmed metabolic acidosis. A definite
diagnosis of diabetic ketoacidosis and cheek infection was made and
the patient was immediately administered an intravenous insulin
infusion, an intravenous fluid replacement was performed and an
insulin sliding scale therapy was commenced. The patient's blood
glucose levels were strictly controlled with insulin. After one
day, the patient's urine specimen was negative for acetone, but the
painful swelling on the left side of the face aggravated and burst
open. The vision of left eye and the left pupillary light reflex
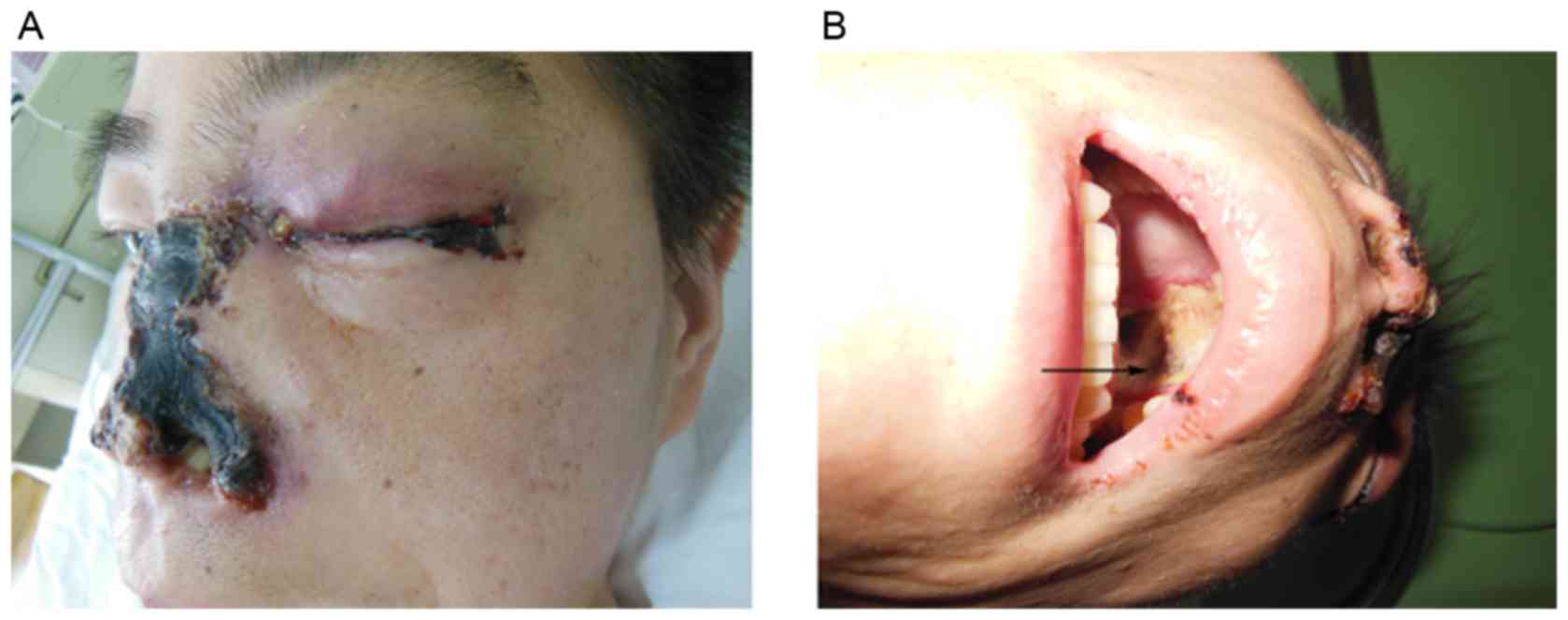
were completely lost (Fig. 1A). His
left pupil was mid-dilated and his left eyeball was fixed.
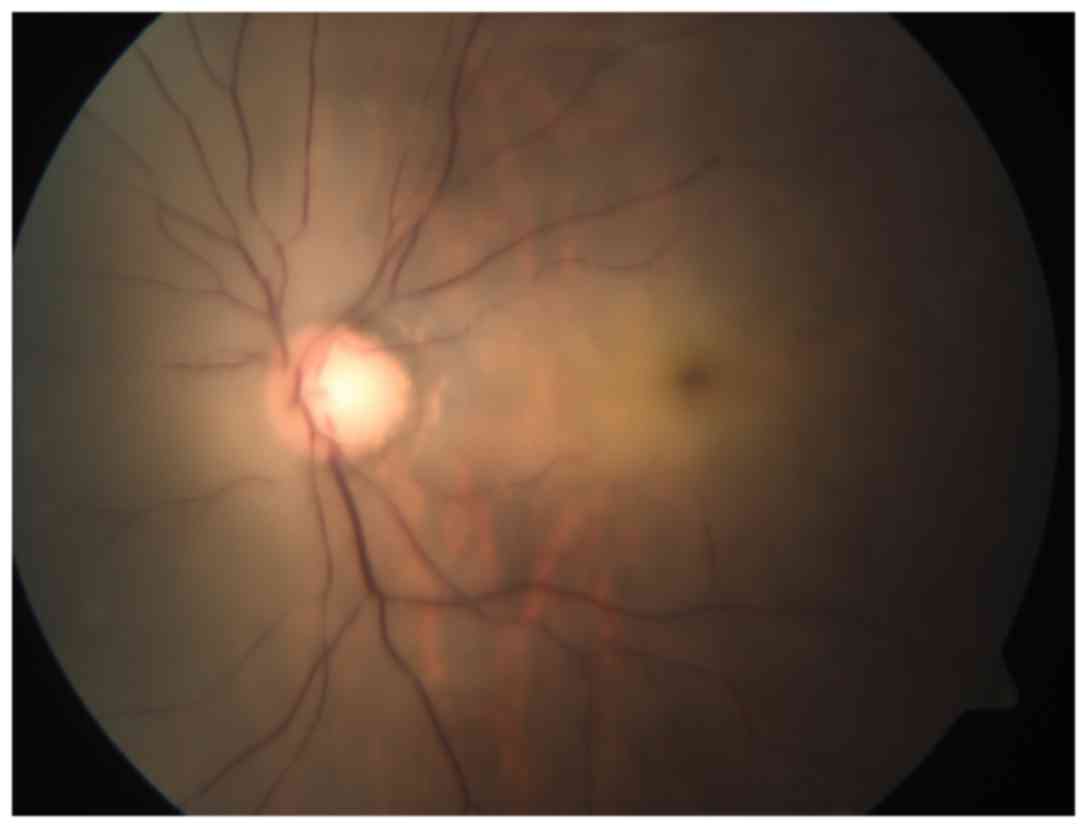
Fundoscopic examination of the left eye revealed that the optic
disc was pale and a cherry-red spot was present in the macula
(Fig. 2). The retinal arteries were
narrow. The patient was diagnosed with left central retinal artery
occlusion. A large amount of purulent secretion was noted in the
patient's left eye and nose. Extensive regions with black necrotic
lumps were present in the nasal cavity. The patient's nasal
structure was completely destroyed and the hard palate was
perforated (Fig. 1B). On admission,
the infectious etiology was repeatedly investigated. A nasal swab
and a large necrotic mass in the nasal cavity were
microbiologically assessed by fungal smears and cultures. The
fungal culture of the patient's purulent secretions was consistent
with mucormycosis. Based on the clinical findings and fungal
culture result, the definitive diagnosis of ROC mucormycosis was
made. Therefore, antifungal therapy using amphotericin B was
intravenously administered at 0.3 mg/kg/day at once and was
thereafter gradually increased to 1 mg/kg/day. Due to the side
effects of amphotericin B, the patient's serum electrolytes and
renal function was monitored. After two weeks, the patient
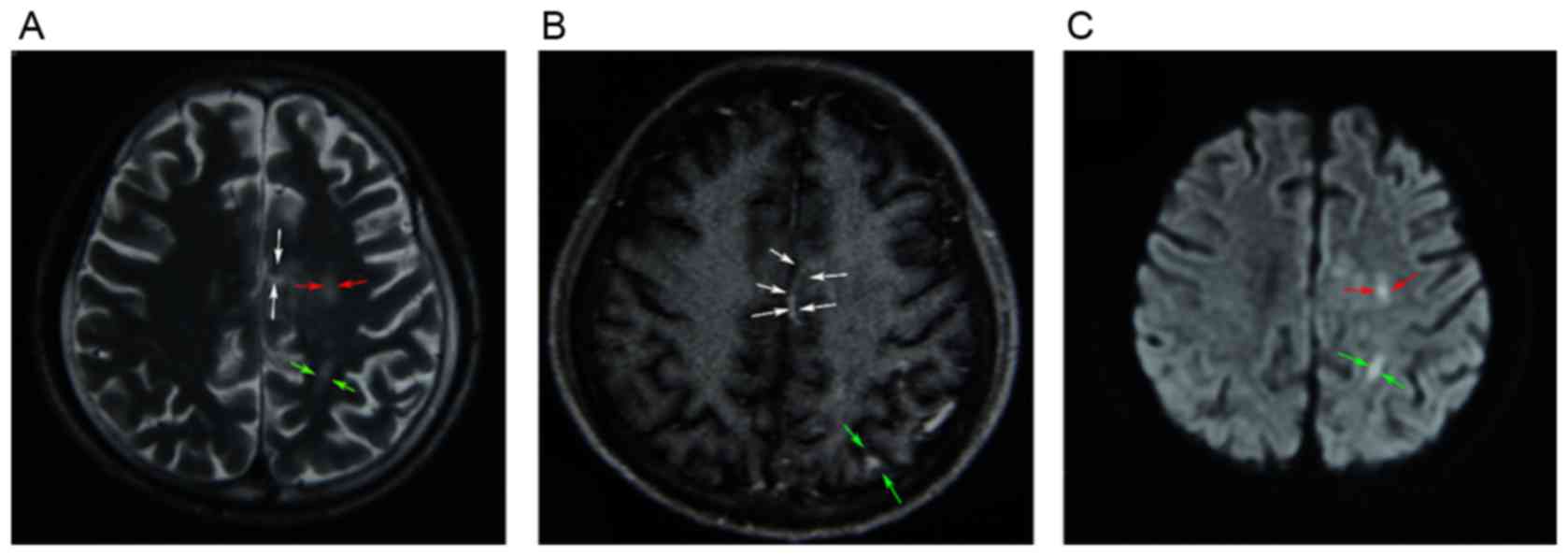
complained of a dull headache. On enhanced magnetic resonance
imaging, multiple infarcts in the cerebral cortex, particularly in
the parietal lobe, frontal lobe and the corpus callosum were
revealed (Fig. 3). Although
extensive local excision was required, the patient was not able to
endure the surgery due to the patient's overall condition being
poor. The necrotic tissue was too broad; therefore, surgery was not
feasible. Following antifungal therapy, the patient's temperature
did not obviously improve. The necrosis of local tissue was
developing, which may be life threatening. After the patient's self
discharge against medical advice, he was transferred to a superior
hospital.
Discussion
Mucormycosis is a rare, acute and opportunistic
infection caused by fungi of the order Mucorales that may be fatal
(2). The infection may manifest in
any part of the body and exclusively affects patients with
metabolic acidosis or immune deficiency, including diabetic
ketoacidosis, organ transplantation and hematological tumors. ROC
mucormycosis represents an acute life-threatening disease,
particularly in patients with diabetic ketoacidosis. The gold
standard for diagnosing ROC mucormycosis is the histopathological
examination of biopsy specimens and fungal culture. The typical
fungal hyphae are broad, nonseptate and had right-angular branches.
In the present case, the patient was a known diabetic and had
developed diabetic ketoacidosis on admission. He presented with a
painful swelling in the left retro-orbital region and nose. The
infection spread to the paranasal sinuses via vessels and to the
central nervous system via the eye orbit and cribriform plate
within the two subsequent weeks. At present, the patient had
progressed to ROC mucormycosis. In normal hosts, mucor is
eliminated by mononuclear and polymorphonuclear phagocytes.
Patients with diabetic ketoacidosis are known to have impaired
function of these phagocytes (3) and
are thus highly susceptible to mucormycosis. In addition, multiple
lines of evidence supported a link between iron availability and
the risk of mucormycosis (4). Due to
elevated available serum iron, patients with diabetic ketoacidosis
have a high risk of developing mucormycosis. The mucor invades the
human host through attachment to the endothelial cell lining of the
blood vessels. A hallmark of mucormycosis is the presence of
extensive angioinvasion. Therefore, the major clinical
manifestation of mucormycosis is vascular thrombosis and tissue
necrosis (2,5). In the present case, the patient's left
eye and nose had numerous black necrotic lumps, which was is in
line with the clinical manifestation of mucormycosis.
At present, antifungal therapy and aggressive
surgical intervention are used to treat mucormycosis. Based on
retrospective clinical studies, amphotericin B is currently used as
the first-line antifungal agent. Several case reports have
documented that patients with rhino-cerebral mucormycosis were
successfully treated by amphotericin B (6,7).
Unfortunately, despite antifungal therapy and disfiguring surgical
debridement, the overall mortality of mucormycosis patients remains
high and approaches 40% in diabetic patients with rhino-cerebral
mucormycosis (2). In this case, this
patient did not receive any surgical debridement previously or at
our department. Given the high mortality of mucormycosis patients,
alternative efficacious therapies are being explored. A large
amount of experimental evidence showed that posaconazole and
ravuconazole have activity against the mucor in vitro
(8,9). According to a case study, a patient
with ROC mucormycosis was successfully treated with posaconazole
and amphotericin (10). In addition
to posaconazole, isavuconazole was recently approved by the Food
and Drug Administration for the treatment of mucormycosis.
Isavuconazole, which has been approved for the treatment of
invasive mucormycosis, may have therapeutic advantages over its
predecessors (11). Due to the
central role of iron metabolism in the pathogenesis of
mucormycosis, it is possible that effective iron chelators serve as
adjunctive agents in combination with antifungal therapies
(2). The establishment of these
novel therapies for mucormycosis in the clinic depends on long-term
observations and research.
References
|
1
|
Peleg AY, Weerarathna T, McCarthy JS and
Davis TM: Common infections in diabetes: Pathogenesis, management
and relationship to glycaemic control. Diabetes Metab Res Rev.
23:3–13. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Spellberg B, Edwards J Jr and Ibrahim A:
Novel perspectives on mucormycosis: Pathophysiology, presentation,
and management. Clin Microbiol Rev. 18:556–569. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chinn RY and Diamond RD: Generation of
chemotactic factors by Rhizopus oryzae in the presence and absence
of serum: Relationship to hyphal damage mediated by human
neutrophils and effects of hyperglycemia and ketoacidosis. Infect
Immun. 38:1123–1129. 1982.PubMed/NCBI
|
|
4
|
Ibrahim AS, Gebermariam T, Fu Y, Lin L,
Husseiny MI, French SW, Schwartz J, Skory CD, Edwards JE Jr and
Spellberg BJ: The iron chelator deferasirox protects mice from
mucormycosis through iron starvation. J Clin Invest. 117:2649–2657.
2007. View
Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ibrahim AS: Host cell invasion in
mucormycosis: Role of iron. Curr Opin Microbiol. 14:406–411. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cagatay AA, Oncü SS, Calangu SS, Yildirmak
TT, Ozsüt HH and Eraksoy HH: Rhinocerebral mucormycosis treated
with 32 gram liposomal amphotericin B and incomplete surgery: A
case report. BMC Infect Dis. 1:222001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ericsson M, Anniko M, Gustafsson H, Hjalt
CA, Stenling R and Tärnvik A: A case of chronic progressive
rhinocerebral mucormycosis treated with liposomal amphotericin B
and surgery. Clin Infect Dis. 16:585–586. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pfaller MA, Messer SA, Hollis RJ and Jones
RN: SENTRY Participants Group: Antifungal activities of
posaconazole, ravuconazole, and voriconazole compared to those of
itraconazole and amphotericin B against 239 clinical isolates of
Aspergillus spp. and other filamentous fungi: Report from SENTRY
Antimicrobial Surveillance Program, 2000. Antimicrob Agents
Chemother. 46:1032–1037. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sun QN, Fothergill AW, McCarthy DI,
Rinaldi MG and Graybill JR: In vitro activities of posaconazole,
itraconazole, voriconazole, amphotericin B, and fluconazole against
37 clinical isolates of zygomycetes. Antimicrob Agents Chemother.
46:1581–1582. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yoon YK, Kim MJ, Chung YG and Shin IY:
Successful treatment of a case with rhino-orbital-cerebral
mucormycosis by the combination of neurosurgical intervention and
the sequential use of amphotericin B and posaconazole. J Korean
Neurosurq Soc. 47:74–77. 2010. View Article : Google Scholar
|
|
11
|
Rybak JM, Marx KR, Nishimoto AT and Rogers
PD: Isavuconazole: Pharmacology, pharmacodynamics, and current
clinical experience with a new triazole antifungal agent.
Pharmacotherapy. 35:1037–1051. 2015. View Article : Google Scholar : PubMed/NCBI
|