Introduction
The occurrence rate of female infertility is on the
increase, and 30–60% of female infertility results from oviduct
obstruction. Oviduct obstruction is mainly caused by congenital
dysplasia, salpingitis, paramorphia, tumor or cyst (1).
At present, X-ray hysterosalpingography (HSG) is
mainly applied in clinic, and the advantages include identification
of the impact of uterine oviduct (2). Previous findings showed that X-ray HSG
was more objective and accurate, and more safe and effective for
patients. As such patients are likely to suffer little pain and
accept the said treatment method more readily. Disadvantages of the
method include that contrast agent sensitivity is more common, and
lipiodol stimulation may result in chronic granuloma, exacerbating
distal tubal obstruction and even leading to pulmonary artery
embolism. Thus, the false-positive rate is higher and the radiation
quantity of inspection ray is larger and patients receiving X-ray
HSG should avoid getting pregnant within 3 months.
The laparoscopic (hysteroscopic) methylene blue
hydrotubation is considered the ‘golden standard’ for diagnosing
oviduct obstruction which can conduct examination and be used to
provide therapy at the same time. However, it usually cannot be
considered the conventional screening method because as a type of
invasive inspection, it has greater surgical risks (3). With the clinical application of
second-generation ultrasound contrast agent SonoVue,
three-dimensional hysterosalpingo-contrast sonography (3D-HyCoSy)
is widely applied for its non-invasion, repeatability, and high
accuracy rate (4). The majority of
previous studies have focused on the diagnostic accuracy of
3D-HyCoSy on oviduct obstruction (5,6).
However, to the best of our knowledge, previous studies have paid
less attention to the radiographic characteristics of 3D-HyCoSy,
especially to the nature of obstruction.
The aim of the present study was to analyze the
diagnostic value of 3D-HyCoSy in the identification of oviduct
obstruction, thus providing a new reference for clinical
diagnosis.
Patients and methods
Patients
In total, 52 patients were admitted to the Dongying
People's Hospital (Shandong, China) and diagnosed with infertility
and oviduct obstruction during the period January, 2015 to January,
2016. The patients had failed to become pregnant within 1 year
without taking any contraceptive measures, and excluded any
patients who were diagnosed with infertility and contrast medium
sensitivity resulting from intrauterine operation, trauma history,
being elderly, endocrine disease, male infertility, reproductive
system disease and diseases occurring in other organs of the body.
The age range of the patients was 22–35 years, with an average age
of 26.4±5.3 years. The infertility time of patients was 1–5 years,
and the average age was 2.7±1.3 years. Thirty patients were
diagnosed with primary infertility and 22 patients were diagnosed
with secondary infertility. The study was approved by the Ethics
Committee of the Dongying People's Hospital. Written informed
consent was obtained from patients and their family members. The
patients with primary infertility and secondary infertility were
treated with 3D-HyCoSy and CLP (CLP), respectively.
3D-HyCoSy method
The 3D-HyCoSy method was applied to patients within
3–5 days after menstruation, and the instruments used included
MyLab 90 color ultrasound meter (Esaote, Italy) which was equipped
with radiography function, contrast-tuned imaging (CnTI) technology
and transvaginal intracavitary probe with a frequency of 5–9 MHz.
The index of 2D and 3D ultrasound contrast instruments was 0.08.
SonoVue (Bracco, Milan, Italy) and was chosen as the contrast
agent, and the suspension used for the examination was prepared by
nurses during the inspection.
The physicians informed the patients of the
angiographic methods, process and objectives in detail prior to the
radiography to reduce the patients' anxiety. Subsequently, 0.25 mg
of intramuscular atropine was applied to the patients. Normal
saline (5 ml) was added to the contrast agent, agitated and
diluted, and the microbubble suspension containing 1 ml (5 mg/ml) +
20 ml of normal saline was extracted for standby application after
the contrast agent was well mixed. The physician first conducted 2D
transabdominal or transvaginal conventional ultrasound examination
to primarily screen the qualified patients. The patients were
allowed to urinate completely and lie in bed in lithotomy position,
and the physician made the intracavitary probe colored with
moderate amount of couplant and covered with condom, and hold the
transvaginal probe in right hand to place it into the vagina to
make it cling to the cervix. Subsequently, the examination was
conducted in an ordered, comprehensive and all-around manner to
observe the basic conditions of the patients' uterus and
surrounding positions, to identify the position of uterus and
bilateral ovary, to check whether there was hydrops in the pelvic
cavity or not and to primarily seek and determine the position of
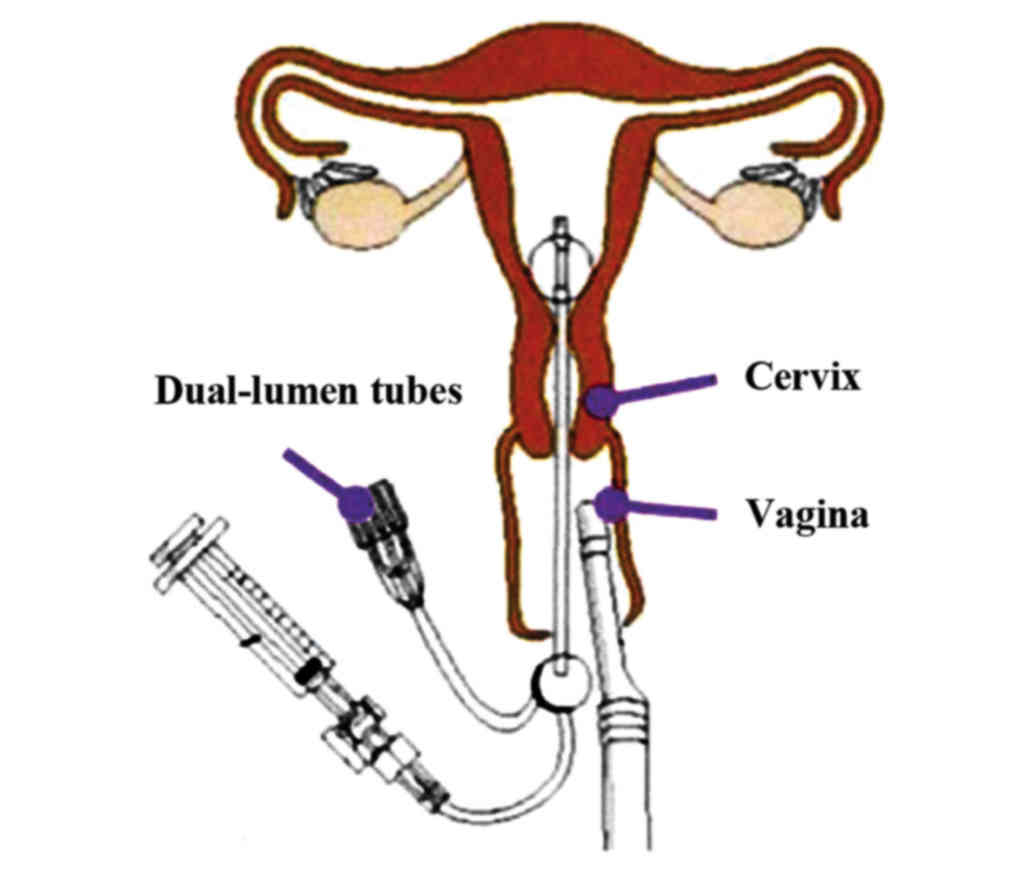
bilateral cornua uteri. The physician placed the dual-lumen
saccular duct into the uterine cavity after applying conventional
disinfection to the vulva and vagina of patients, and then the
physician injected 3–4 ml of normal saline into the sacculus to
take out of the duct and block the intracervical mouth to finally
drop the bivalve speculum out (Fig.
1). Following the beginning of radiography, the diluted
contrast medium of 10–20 ml was slowly injected through the duct at
a uniform speed to probe whether there was any adhesion or polyp
and other occupying lesions in the uterine cavity and to seek the
best section plane at the opening of oviducts of the cornua uteri.
The contrast and 3D model was initiated to determine the region of
interest, after which the volume sampling frame was placed and
adjusted to completely wrap the lesion, and the physician kept the
probe stable and asked the patient to lie on the examining couch.
The static 3D ultrasound radiography model with free arm was
chosen, and the probe was scanned from top to bottom after the
injection of contrast medium to complete the sampling once and the
sampling was conducted after every 10 sec. The sampling angle was
adjusted to be 85–90° after 90 sec to collect the angiography
images of bilateral oviducts, and the source materials were stored
in the hard disk of the instrument for image analysis. The
physician recorded and observed the distribution situation of the
microbubble around the bilateral ovary and in intestine and womb
rectum concave. Once the oviducts were found to be partially
obstructive, they were appropriately pressurized. The images of
radiography volume were captured after ending of the radiography to
analyze and reconstruct the volume and to track the filling of
contrast medium in proximal and umbrella end of uterine and
bilateral oviducts. The results can be divided as follows:
i) Unobstruction: The operator did not feel any
obvious resistance when injecting contrast medium, and the patients
suffered no abdominal pain. Upon the injection of contrast medium
into the uterine cavity, the physician observed that the strong
echo of contrast medium rapidly moves towards the oviducts from
bilateral cornua uteri and completely fills the oviducts. The
stronger echo of contrast medium rapidly overflowed from the
umbrella end and formed the shape of a ring or a half ring around
the ovary, and free fluid sonolucent region was distributed in the
uterus-rectum fossa or the scope of the original fluid sonolucent
area expanded, and the dense strong echo of contrast medium floated
in the free fluid sonolucent area. After 3D reconstruction, the
uterine cavity was completely filled and in the shape of an
inverted triangle, and the whole oviducts had the shape of a band
with its development in the bilateral uterine cavity, and the
terminal of oviducts had wrapped the ovary in the shape of a ring
or a half ring.
ii) Partial obstruction: The resistance is stronger
and a small amount of backflow appears when injecting contrast
medium, and the patients may feel mild and moderate pain in the
hypogastric region. The strong echo of contrast medium in the
patients' uterine cavity slowly moves towards the oviducts, and
physicians did not observe that the obvious jet-shaped strong echo
overflowing from the umbrella end of oviducts, and the circular
belt around the ovary and a small number of echo-free areas exist
in uterus-rectum fossa or the expanded scope of the original
echo-free area is not evident. After 3D reconstruction, the
development of oviducts in the affected side was tenuous, distorted
and reflexed, and the physicians identified interruption of partial
echoes.
iii) Obstruction: The injection resistance was high,
thus the injection was conducted by adding pressure, and the liquid
was not injected when the injection volume reached 5–6 ml. The
physicians observed that all or part of the contrast medium flowed
in a reverse manner when they stopped adding pressure and
injection. The contrast medium completely filled the uterine
cavity, and the whole oviducts were not developed or partially
developed, and the strong echo overflowed from the umbrella end of
oviducts, and no ring-like substance wraps the ovary. There was no
echo-free area in rectum fossa or the original echo-free area was
not altered following reconstruction. The physicians observed that
the stripped hyperecho appeared in the proximal end of the
obstructive region but not in the distal end thereof.
CLP method
By determining whether methylene blue overflowed
from the umbrella end, the results of the laparoscopic examination
were divided as follows: i) Oviduct patency: No resistance occurred
when methylene blue was injected into the patients' body, and the
methylene blue completely filled the oviduct and overflowed from
the umbrella end of the oviduct; ii) partial oviduct obstruction:
The injection pressure was higher, and methylene blue completely
filled the oviducts, and partial oviducts became swollen for >1
min or became adhesive to the umbrella end, and methylene blue
slowly overflowed from the umbrella end in the shape of small
beads; and iii) oviduct obstruction: The injection pressure of
methylene blue was large, and methylene blue failed to completely
fill the oviducts, or completely filled the swollen oviducts but
failed to overflow from the umbrella end, and the tension of uterus
was high.
The examination results were concluded and
interpreted by two experienced senior physicians.
Observation target
The accuracy of 3D-HyCoSy was evaluated based on the
diagnostic results of CLP. The physicians analyzed the features of
different images of oviduct obstruction as diagnosed by 3D-HyCoSy
as well as the pain degree, injection pressure of contrast medium
and quantity of backflow of the patients. According to the pain
standards suggested by the World Health Organization (WHO), pain
can be classified as: The pain-free and quietness can be classified
as grade 0, mild pain and tolerability were classified as grade I,
moderate pain, tolerability, moaning and uneasiness were classified
as grade II, and severe pain, intolerance, interruption of
examination were classified as grade III.
Statistical methods
SPSS 19.0 statistical software (Chicago, IL, USA)
was used to conduct data input and analysis. The quantitative data
were expressed as mean ± standard deviation, and the comparison
among groups was analyzed by ANOVA. Qualitative data were expressed
by the number of cases or as a percentage (%), the inter-group
comparison was tested by the χ2 test (correction).
Sensitivity was calculated as: true positive population/(true
positive population + false negative population) × 100%,
specificity as true negative population/(true negative population +
false positive population) × 100%, positive predictive value as
true positive population/(true positive population + false positive
population) × 100%, and negative predictive value as true negative
population/(true negative population + false negative population) ×
100%. P<0.05 indicated that the difference was statistically
significant.
Results
Comparison of diagnostic results of
3D-HyCoSy and CLP
According to CLP diagnosis, 40 oviducts were
obstructed, 30 were partially obstructed, 12 were tortuous and 22
were completely obstructed. The 40 oviducts were unilaterally
pathological, and 24 were bilaterally pathological. Among the 64
cases, 10 were diagnosed as congenital dysplasia, 35 as
inflammation and 19 as tumor and cyst. Based on the diagnostic
criteria of CLP, the diagnostic sensitivity, specificity, positive
and negative predictive values of 3D-HyCoSy were 82.4, 88.3, 77.9
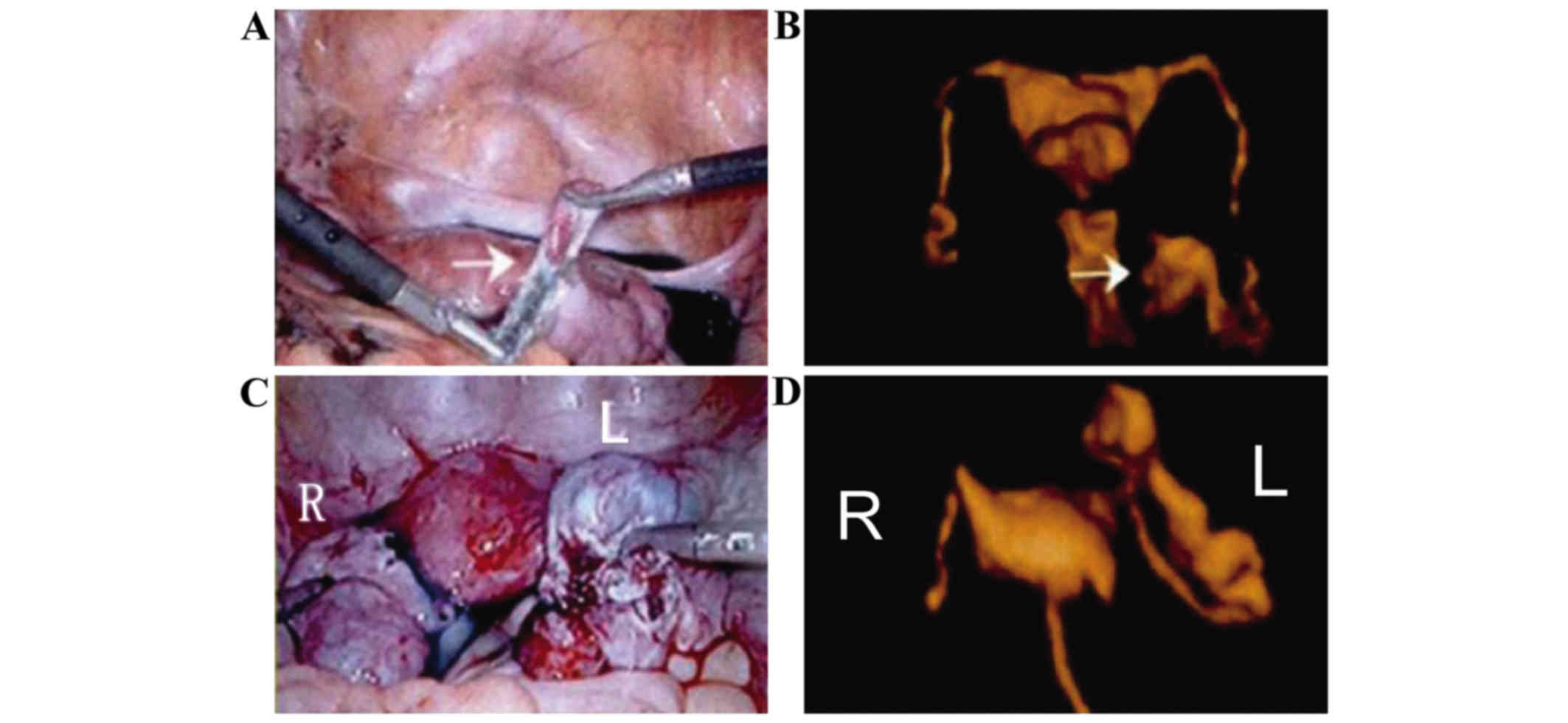
and 90.2%, respectively (Fig.
2).
Fig. 2 shows the
contrast between 3D-HyCoSy and CLP Fig.
2A and B shows partial obstruction of the left oviduct, and the
arrow shows the adhesive umbrella end. Fig. 2C and D shows the proximal obstruction
of the left oviduct, and that the proximal end of the oviduct was
obviously swollen.
Comparison of obstruction of different
nature as diagnosed by 3D-HyCoSy
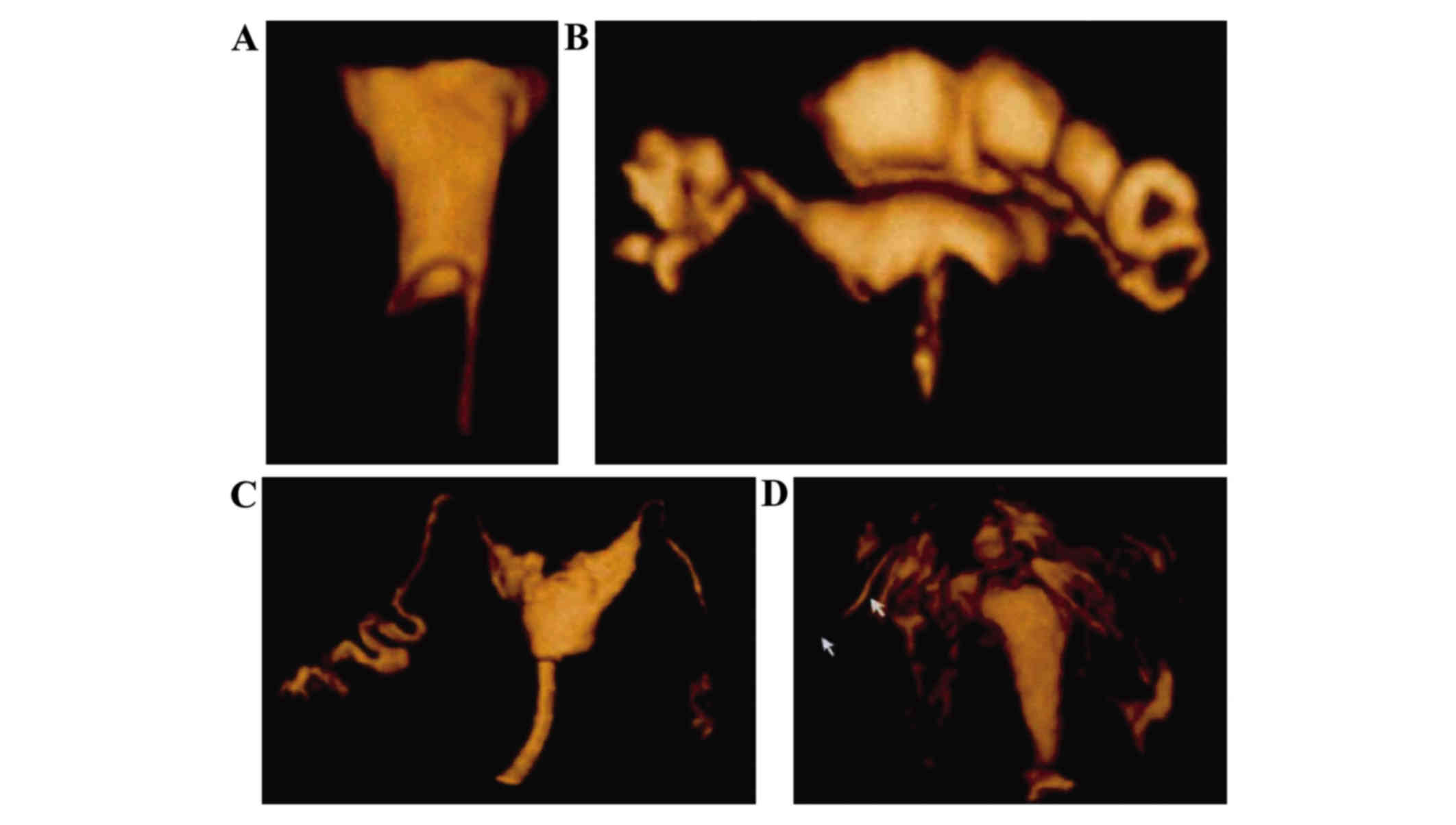
The contrast agent flow time of oviduct obstruction
(tortuosity and complete obstruction) as diagnosed by 3D-HyCoSy was
significantly prolonged when compared with that of partial oviduct
obstruction (ratio between 4.2±1.3, 5.8±1.4 and 2.9±1.1 sec;
F=5.624, P=0.015), and flow time of inflammation as diagnosed
subsequently was longer than that of congenital dysplasia, tumor
and cyst. Following the diagnosis of inflammation, the shape of the
contrast agent was tenuous, swollen, angled, rigid and distorted
and the occurrence rate of inflammation was higher, and the degree
of pain suffered by patients, injection pressure of contrast medium
and quantity of backflow was significantly increased following the
diagnosis of inflammation (P<0.05) (Table I and Fig.
3).
 | Table I.Comparison of obstruction of different
nature as diagnosed by 3D-HyCoSy. |
Table I.
Comparison of obstruction of different
nature as diagnosed by 3D-HyCoSy.
| Parameters | Flow time (sec) | Shape of contrast
medium, n (%) | Pain degree | Injection pressure
(kPa) | Quantity of backflow
(ml) |
|---|
| Inflammation
(n=35) | 4.7±1.3 | 28 (80.0) | 1.5±0.4 | 39.5±4.2 | 1.8±0.6 |
| Congenital dysplasia
(n=10) | 2.5±1.2 | 5 (50.0) | 0.7±0.2 | 34.2±4.3 | 0.5±0.2 |
| Tumor and cyst lesion
(n=19) | 3.2±1.3 | 9 (47.4) | 0.8±0.3 | 37.6±4.5 | 1.2±0.3 |
| F
(χ2) | 5.443 | 7.189 | 5.714 | 5.532 | 6.635 |
| P-value | 0.021 | 0.027 | 0.018 | 0.020 | 0.009 |
Discussion
It has been shown that the 3D-HyCoSy can acquire 3D
images of oviducts through the reconstruction of 3D surface modes,
and can display three mutually perpendicular section planes
(coronal plane, sagittal section and cross section) at the same
time, and can better acquire important information concerning the
shape, way, patency degree and obstruction sites to evaluate the
patency and oviducts as well as the spatial relationship between
oviducts and ovary in a more comprehensive and accurate manner
(7,8). Due to the application combining
hysterosalpingo contrast sonography and 3D ultrasound, the
diagnostic sensibility and specificity were obviously increased
(9,10). Based on the diagnostic criteria of
CLP, the diagnostic sensitivity, specificity, positive predictive
and negative predictive values of 3D-HyCoSy were 82.4, 88.3, 77.9
and 90.2%, respectively. 3D-HyCoSy was easily operated and
non-invasive and was important in diagnosing and identifying
uterine cavity lesion and oviducts obstruction. We found that the
contrast agent flow time of oviduct obstruction (tortuosity and
complete obstruction) as diagnosed by 3D-HyCoSy was significantly
prolonged when compared with that of partial oviduct obstruction,
and flow time of inflammation as diagnosed subsequently was longer
than that of congenital dysplasia, tumor and cyst. Following the
diagnosis of inflammation, the shape of contrast agent was tenuous,
swollen, angled, rigid and distorted and the occurrence rate of
inflammation was higher. Additionally, the degree of pain suffered
by patients, injection pressure of contrast medium and quantity of
backflow obviously increased following the diagnosis of
inflammation, and the difference was of statistical significance.
This is where the innovation of the study was and it had better
application value in judging the nature of oviducts obstruction in
clinic, especially the inflammation.
Of course, although the advantages of 3D-HyCoSy has
become more and more obvious in clinic, the observation range of 3D
transvaginal ultrasonography is narrow and is not applicable to the
patients with uterus augmentation and larger uterine fibroids, and
it may influence the reconstruction of oviducts when the adnexal
masses become larger or the structure becomes complicated (11,12). At
the same time, 3D-HyCoSy did not display the inside oviducts
clearly, especially the lesion occurring in the oviducts mucosa and
pelvic cavity adhesion (12,13). In addition, research studies should
continue to explore reduction in the pseudo obstruction resulting
from oviducts spasm in examination (14). Additionally, 3D-HyCoSy was completed
under the assistance of more advanced apparatus and instruments
(radiography function) and better contrast medium, therefore the
application of 3D-HyCoSy has a few limitations.
In conclusion, SonoVue 3D-HyCoSy has some
significant advantages in diagnosing the patency of oviduts, and
the application of SonoVue contrast medium combined with 3D volume
imaging technology and codes contrast imaging technology greatly
makes up the shortfall of 2D hysterosalpingo contrast sonography.
Since the physicians can acquire the coronal plane of uterine
cavity and the stereo images of the whole oviducts through 3D
imaging, they can acquire more comprehensive and accurate
information to conduct comprehensive analysis and evaluation
towards the oviducts. Thus, 3D imaging can replace X-ray iodized
oil imaging and even the laparoscopy to some extent, and can
provide a more convenient, non-invasive and radiation-free
examination method without any toxicity and side effects for the
majority of patients with infertility. It can also play a certain
role in treating infertility during the radiography, and has
therefore become a new method to treat oviduct diseases, which is
characteristic of high safety and high diagnostic accuracy.
Therefore, 3D-HyCoSy is expected to become the most valuable and
promising examination method in the field of gynecology.
References
|
1
|
Lovsin B and Tomazevic T:
Hysterosalpingo-contrast sonography for infertility investigation.
Int J Gynaecol Obstet. 108:70–71. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hamed HO, Shahin AY and Elsamman AM:
Hysterosalpingo-contrast sonography versus radiographic
hysterosalpingography in the evaluation of tubal patency. Int J
Gynaecol Obstet. 105:215–217. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Saunders RD, Shwayder JM and Nakajima ST:
Current methods of tubal patency assessment. Fertil Steril.
95:2171–2179. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
El-Sherbiny W and Nasr AS: Value of
3-dimensional sonohysterography in infertility work-up. J Minim
Invasive Gynecol. 18:54–58. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Exacoustos C, Zupi E, Szabolcs B, Amoroso
C, Di Giovanni A, Romanini ME and Arduini D: Contrast-tuned imaging
and second-generation contrast agent SonoVue: a new ultrasound
approach to evaluation of tubal patency. J Minim Invasive Gynecol.
16:437–444. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Savelli L, Pollastri P, Guerrini M, Villa
G, Manuzzi L, Mabrouk M, Rossi S and Seracchioli R: Tolerability,
side effects, and complications of hysterosalpingocontrast
sonography (HyCoSy). Fertil Steril. 92:1481–1486. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhou L, Zhang X, Chen X, Liao L, Pan R,
Zhou N and Di N: Value of three-dimensional
hysterosalpingo-contrast sonography with SonoVue in the assessment
of tubal patency. Ultrasound Obstet Gynecol. 40:93–98. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kupesic S and Plavsic BM: 2D and 3D
hysterosalpingo-contrast-sonography in the assessment of uterine
cavity and tubal patency. Eur J Obstet Gynecol Reprod Biol.
133:64–69. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Coyne L, Jayaprakasan K and Raine-Fenning
N: 3D ultrasound in gynecology and reproductive medicine. Womens
Health (Lond Engl). 4:501–516. 2008. View Article : Google Scholar
|
|
10
|
Fleischer AC, Lyshchik A, Jones HW Jr,
Crispens M, Loveless M, Andreotti RF, Williams PK and Fishman DA:
Contrast-enhanced transvaginal sonography of benign versus
malignant ovarian masses: preliminary findings. J Ultrasound Med.
27:1011–1018; quiz 1019–1021. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Alcázar JL, Martinez-Astorquiza Corral T,
Orozco R, Dominguez-Piriz J, Juez L and Errasti T:
Three-dimensional hysterosalpingo-contrast-sonography for the
assessment of tubal patency in women with infertility: a systematic
review with meta-analysis. Gynecol Obstet Invest. 30:2–4. 2016.
|
|
12
|
Cheng Q, Wang SS, Zhu XS and Li F:
Evaluation of tubal patency with transvaginal three-dimensional
hysterosalpingo-contrast sonography. Chin Med Sci J. 30:70–75.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chan CC, Ng EH, Tang OS, Chan KK and Ho
PC: Comparison of three-dimensional
hysterosalpingo-contrast-sonography and diagnostic laparoscopy with
chromopertubation in the assessment of tubal patency for the
investigation of subfertility. Acta Obstet Gynecol Scand.
84:909–913. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Watermann D, Denschlag D, Hanjalic-Beck A,
Keck C, Karck U and Prömpeler H:
Hystero-salpingo-contrast-sonography with 3-d-ultrasound - a pilot
study. Ultraschall Med. 25:367–372. 2004.(In German). View Article : Google Scholar : PubMed/NCBI
|