Introduction
Macula flava is the most sensitive spot on the
retina. The macular edema is an inflammatory reaction of the macula
falva, which is caused by fluid infiltration and can lead to a
severe reduction in the visual acuity (1). The macular edema is the ocular
manifestation of conditions such as central retinal vein occlusion,
diabetic retinopathy and uveitis (2). Currently, the treatment of the macular
edema is focused on pathogeny correction and symptomatic treatment.
IgG1 antibody can attach to vascular endothelial growth factor
(VEGF) and block its biological activity. This way it can inhibit
blood vessel growth, which has a prominent effect on treating
macula edema caused by diabetes (3).
Bevacizumab (Avastin®) is a recombinant humanized
monoclonal antibody that plays a significant role in the targeted
therapy in rectal cancer (4).
With the development of the fundus laser
photocoagulation treatment, more and more fundus diseases are being
cured fundamentally. Among these therapies, argon green laser can
make accretion of the retina scar through sealing the leaky
microvascular artery, thus promotes the regeneration of the retina
pigment epithelium and rebuilds the blood-retina barrier, which
accelerates the absorption of the edema (5). We employed Avastin® combined
with argon green laser in treating macular edema and achieved
satisfactory results.
Materials and methods
Group criteria
Inclusion criteria: Patients diagnosed with fundus
macular edema by slit lamp, 90D preset lens, three-mirror contact
lens, indirect ophthalmoscope, intraocular tension, and OCT
examination.
Exclusion criteria: i) Patients without macular
edema; ii) patients with cataract; iii) patients allergic to
Avastin®; iv) patients who refused to sign informed
consent papers; v) patients who were treated with surgery or
medicine; and vi) patients with mental or nervous system
diseases.
Clinical information
From May 2009 to April 2013, 78 patients seeking
treatment for macular edema in the First Affiliated Hospital of
Nanchang University were enrolled in this study. There were 28
males and 50 females with average age of 46.6±7.5 years. The
courses of the disease ranged from 6 months to 3.8 years (average,
1.52±0.73 years), and the medium course was 1.3 years. Patients
were divided into two groups on random control principle (Table I). Information such as age, disease
course, visual acuity in two groups had no statistical differences
(P>0.05). This study was approved by the Ethics Committee in the
First Affiliated Hospital of Nanchang University, and the patients
or their families signed the written informed consent papers.
 | Table I.Comparisons on basic information of
patients with macula rhegmatogenous retinal detachment. |
Table I.
Comparisons on basic information of
patients with macula rhegmatogenous retinal detachment.
| Groups | Case | Age (years) | Course of disease
(years) | logMAR-BCVA | Visual acuity
(°) |
|---|
| Experimental | 39 | 48.8±2.3 | 1.6±0.75 | 1.42±0.67 | 0.01±0.011 |
| Control | 39 | 43.6±1.1 | 1.8±0.83 | 1.51±0.87 | 0.01±0.012 |
| F-value | – | 0.37 | 0.78 | 0.28 | 0.07 |
| P-value | – | >0.05 | >0.05 | >0.05 | >0.05 |
Examination methods
Intracavitary injection of Avastin®
into vitreous chamber (
6)
Before surgery, we applied tropicamide (Yangze
Pharma, Taizhou, China) to dilate the pupil. Patients were draped
and sterilized, conjunctival sac was flushed, and surface
anesthesia with Alcaine (Yangze Pharma) was conducted. The anterior
chamber was punctured under the conducted. The anterior chamber was
punctured under the slit lamp microscope (Mule Co., Hangzhou,
China), and 0.1 ml of anterior aqueous fluid was collected. We
vertically punctured the bulbar conjunctiva and sclera from the
spot 3.5 mm behind the corneal limbus under the temple. We reached
the posterior segment of the vitreous chamber and slowly injected
the Avastin® solution into the chamber at the rate of
0.1 ml/min (total volume, 0.05 ml). Needle hole was gently pressed
the with wet cotton bud after injection for 1 to 2 min, and
intraocular tension was then examined. If the intraocular tension
was not high, we applied tobramycin eye ointment.
Argon green laser therapy (
7)
Tropicamide was applied to dilate the pupil and
local leaky spot was sealed using photocoagulation (distance from
the central fovea was 500 µm-1 mm, diameter of the light spot was
50–100 µm, exposure time was set at 0.1 sec, the energy was 75–100
mW, and reaction was class I of spot size effect classification).
Visual acuity was re-examined at 1, 3, 6 and 12 months after
surgery and the fundus fluorescein angiography examined 3 months
after surgery.
90D preset lens examination (
8)
During the examination, patients kept the same
position and posture with the slit lamp. Tropicamide was applied
and the preset lens was placed, while the light angle and the
microscope was adjusted. The focus point was regulated until the
vitreous body and the position of fundus lesion could be seen
clearly.
Intraocular tension examination (
9)
Intraocular examination with non-contact
ophthalmotonometer (NT-2000; Siou Co., Shanghai, China) was
conducted. Patient's posture was adjusted before the examination,
and submaxilla was placed on the bracket of the examination machine
properly. Both eyes look forward at the same time. Eyes were opened
to a certain degree and were made to stare at the indication point
of the machine. The non-contact ophthalmotonometer was used for
examination with airflow. Eyes were enjoined to avoid blinking
while the examiner regulated the controlling lever to focus. When
regulation was completed, intraocular tension was examined, and the
average value was recorded after 3 successive examinations.
Statistical analysis
All quantitative data were expressed as mean ±
standard deviation. Comparison between groups was done using
Student's t-test. Percentage (%) was used to express the
enumeration data and Chi-square test was used for data analysis. A
P-value of <0.05 was considered to indicate a statistically
significant difference.
Results
Central foveal thickness of the
macular lutea before and after treatment
We compared the central foveal thickness of the
macular lutea in both groups before and after treatment. Results
indicated that the macular central foveal thickness in both groups
reduced significantly after treatment, while the therapeutic effect
of the group with combined treatment was more prominent.
Differences were statistically significant (P<0.05) (Table II).
 | Table II.Central foveal thickness of the
macular lutea before and after treatment. |
Table II.
Central foveal thickness of the
macular lutea before and after treatment.
| Groups | Case | Before surgery
(µm) | 1 day after
surgery | 1 month after
surgery | 3 months after
surgery | 6 months after
surgery |
|---|
| Experimental | 39 | 387.3±12.2 | 382.3±9.7 |
335.4±28.7a |
267.8±18.4b | 234.4±9.8 |
| Control | 39 | 389.2±10.7 | 386.5±7.2 |
354.8±12.5a |
292.4±13.6b | 278.5±10.4 |
| T-value | – | 0.43 | 0.46 | 12.7 | 28.6 | 31.4 |
| P-value | – | 0.17 | 0.57 | 0.011 | 0.014 | 0.015 |
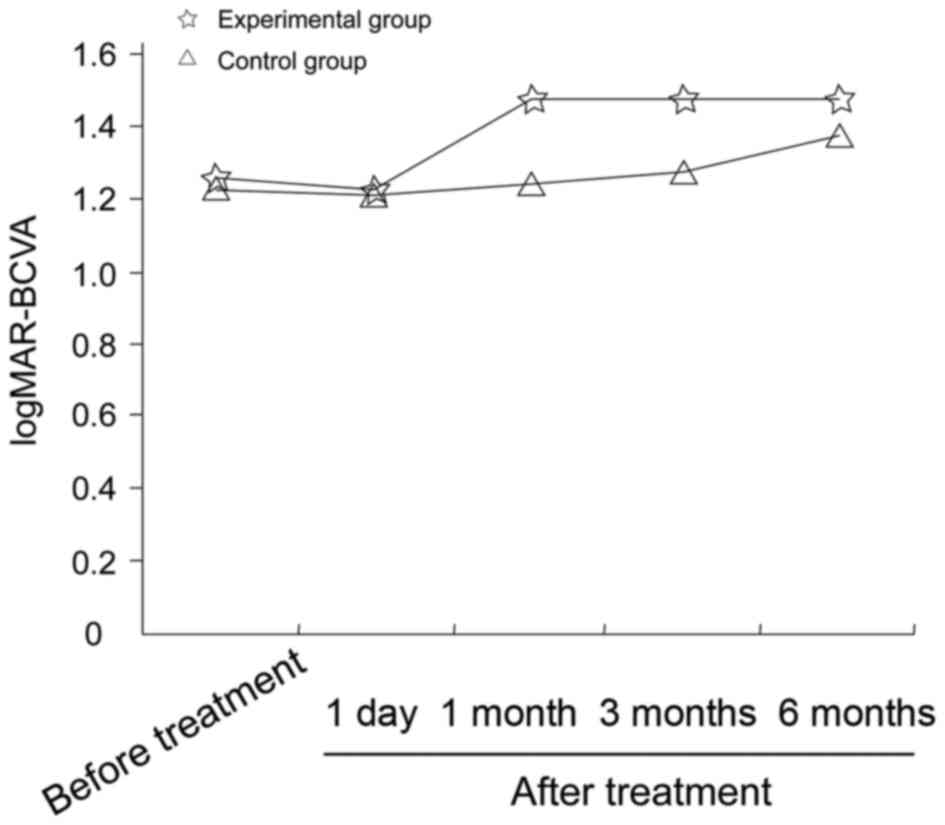
Best-corrected visual acuity
Patients in the combined treatment group achieved
the best-corrected visual acuity one month after treatment, while
patients in the green laser group achieved the best-corrected
visual acuity three months after treatment. Differences were
statistically significant (P<0.05). However, after 6 months, the
differences in visual acuity in both groups were not statistically
significant (P>0.05) (Table III
and Fig. 1).
 | Table III.Comparison of the logMAR-BCVA in both
groups. |
Table III.
Comparison of the logMAR-BCVA in both
groups.
| Groups | Case | Before surgery | 1 day after
surgery | 1 month after
surgery | 3 months after
surgery | 6 months after
surgery |
|---|
| Experimental | 39 | 1.25±0.67 | 1.23±0.71 |
1.48±0.82a | 1.49±0.95 | 1.49±0.72 |
| Control | 39 | 1.22±0.87 | 1.22±0.69 | 1.29±0.55 | 1.22±0.28 |
1.31±0.21b |
| T-value | – | 0.68 | 0.38 | 12.64 | 18.23 | 0.37 |
| P-value | – | >0.05 | 0.77 | 0.018 | 0.021 | 0.26 |
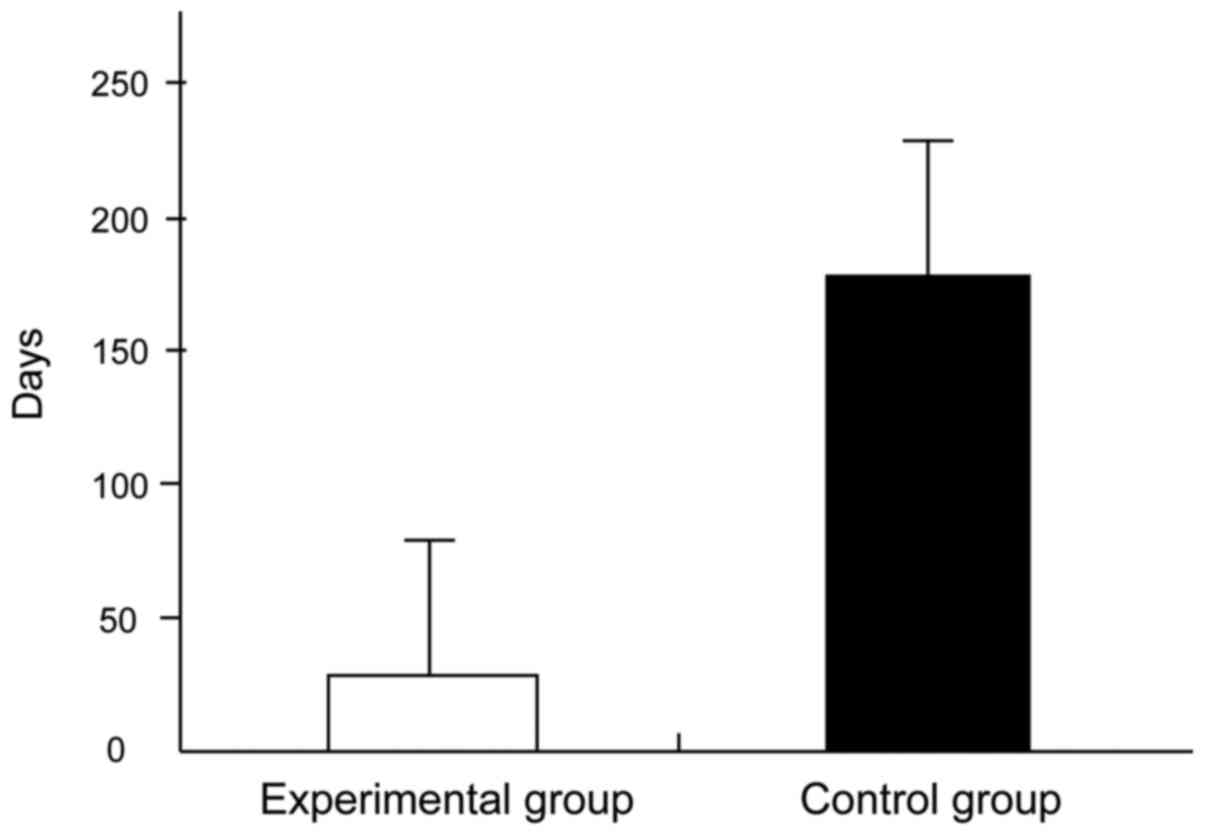
The average time to reach the best-corrected visual
acuity in the experimental group was 29.7±7.8 days while this time
in the control group was 172.6±12.4 days. Differences were
statistically significant (P<0.05) (Table IV and Fig. 2).
 | Table IV.Time before reaching the
best-corrected visual acuity (day). |
Table IV.
Time before reaching the
best-corrected visual acuity (day).
| Groups | Case | Time taken to reach
the best-corrected visual acuity |
|---|
| Experimental | 39 | 29.7±7.8 |
| Control | 39 | 172.6±12.4 |
| T-value | – | 49.3 |
| P-value | – | <0.001 |
Therapeutic effect
Therapeutic effects of two methods were compared one
year after treatment, and no statistically significant difference
was detected (P>0.05) (Table
V).
 | Table V.Comparison of the therapeutic
effects. |
Table V.
Comparison of the therapeutic
effects.
| Groups | Case | Effective | Ineffective | Rate of
effectiveness |
|---|
| Experimental | 39 | 37 | 2 | 0.95 |
| Control | 39 | 32 | 7 | 0.82 |
| P-value | – | 0.48 |
| 0.27 |
Complications after treatment
In the experimental group, we had no patient
suffering from increased intraocular tension and no macular edema
recurrence. We only observed 2 cases of visual acuity reduction in
the experimental group. In the control group, we observed 2 cases
of recurrence, 3 cases of increased intraocular tension and 2 cases
of visual acuity reduction. The incidence of postoperative
complications in the two groups were compared, and the differences
were not statistically significant (P>0.05) (Table VI).
 | Table VI.Comparison of after treatment
complications. |
Table VI.
Comparison of after treatment
complications.
| Groups | Case | Recurrence of macular
edema | Increase of
intraocular tension | Deceases of visual
acuity | Incidence of
complications |
|---|
| Experimental | 39 | 0 | 0 | 2 | 0.05 |
| Control | 39 | 2 | 3 | 2 | 0.18 |
| P-value | – | 0.27 | 0.33 |
|
|
Discussion
Fundus macular edema is a condition that usually
occur in medium stage of diabetes (1). Fundus macular edema has a complicated
pathogeny and can be the ocular manifestation of multiple ocular
diseases, including central retinal vein occlusion, diabetic
retinopathy and uveitis. It is usually caused by diseases such as
diabetes, retinal vein occlusion and uveitis. Fundus macular edema
is considered an important cause of visual acuity reduction in
elderly patients (2).
We know that an increase in VEGF level can promote
the vitreous cell proliferation, optic nerve swelling and mottling
bleeding, which finally lead to reduction of visual acuity
(10). Therefore, if we find a way
to decrease VEGF level in the vitreous chamber we can reduce the
risk of fundus macular edema (11).
In this study the recombinant humanized monoclonal
antibody-Avastin® (Bevacizumab) was used to attach to
VEGF in the vitreous chamber and block its biological activity.
This method can be considered a targeted therapy (2,9). In the
past, Avastin® was also used in the targeted therapy and
produced satisfactory results in treating mammary cancer, rectal
cancer and liver cancer (12).
To treat fundus macular edema, we injected
Avastin® into the vitreous chamber under local
anesthesia, and demonstrated that Avastin® had an
excellent effect in improving angiogenesis. However, its effect on
the oxygen supplement on proliferated vessel and the choroid blood
circulation was not ideal, and the visual acuity recovered slowly
after treatment with Avastin®.
Patients in our experimental group received
Avastin® to stop neovascularization, and were treated
with argon green laser to seal off the leaky microvascular artery.
Thus we promoted the regeneration of the retina pigment epithelium
and the rebuilding of the blood-retina barrier, and also
accelerated the absorption of the edema. We treated the macular
edema using two approaches and established good therapeutic effect.
We achieved excellent results in improving patients' visual acuity.
Results indicated that the macular foveal thickness in patients in
the experimental group was obviously decreased after this
treatment, and the decrease was more significant compared with that
in the control group. Patients in the experimental group achieved
the best-corrected visual acuity after one-month, while the
patients in the control group achieve that after three months. When
the postoperative adverse reactions (in the ocular region and whole
body) were compared, no statistically significant differences were
observed between the two groups.
Romero-Aroca et al treated macular edema
caused by diabetes using laser and reported good outcome (1). However, the argon green laser cannot
effectively reduce angiogenesis, therefore the probability of
recurrences is fairly high.
Nevertheless, Avastin® therapy priority
still needs further exploration with clinical and animal
experiments. Also, financial aspect of these two methods for
patients with limited financial resources should be studied in
future. We concluded that treatment of fundus macular edema with
Avastin® combined with argon green laser is safe and
effective. This method obviously improved the visual acuity with
relatively low adverse reactions.
Acknowledgements
The present study was supported by the National
Natural Science Foundation of China (nos. 81160118, 81400372,
81300729 and 81470601), the Clinical Medicine Research
Special-Purpose Foundation of China (no. L2012052), the ShanHai
Foundation of China (no. 2013SH008), the Jiangxi Province Voyage
Project (no. 2014022), the Science and Technology Platform
Construction Project of Jiangxi Province (no. 2013116), the Natural
Science Foundation of Fujian Province (no. 2015J05170), the Youth
Science Foundation of Jiangxi (no. 20151BAB215016), the Technology
and Science Foundation of Jiangxi Province (no. 20151BBG70223), the
Education Department Scientific Research Foundation (no. GJJ14170)
and the Health Development Planning Commission Science Foundation
of Jiangxi Province (no. 20155154).
References
|
1
|
Romero-Aroca P, Reyes-Torres J,
Baget-Bernaldiz M and Blasco-Suñe C: Laser treatment for diabetic
macular edema in the 21st century. Curr Diabetes Rev. 10:100–112.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Shamsi HN, Masaud JS and Ghazi NG:
Diabetic macular edema: new promising therapies. World J Diabetes.
4:324–338. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chan CK, Jain A, Sadda S and Varshney N:
Optical coherence tomographic and visual results at six months
after transitioning to aflibercept for patients on prior
ranibizumab or bevacizumab treatment for exudative age-related
macular degeneration (an American Ophthalmological Society thesis).
Trans Am Ophthalmol Soc. 112:160–198. 2014.PubMed/NCBI
|
|
4
|
Luttrull JK and Dorin G: Subthreshold
diode micropulse laser photocoagulation (SDM) as invisible retinal
phototherapy for diabetic macular edema: a review. Curr Diabetes
Rev. 8:274–284. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sarraf D, Joseph A and Rahimy E: Retinal
pigment epithelial tears in the era of intravitreal
pharmacotherapy: risk factors, pathogenesis, prognosis and
treatment (an American Ophthalmological Society thesis). Trans Am
Ophthalmol Soc. 112:142–159. 2014.PubMed/NCBI
|
|
6
|
Bressler SB, Almukhtar T, Aiello LP,
Bressler NM, Ferris FL 3rd, Glassman AR and Greven CM: Diabetic
Retinopathy Clinical Research Network: Green or yellow laser
treatment for diabetic macular edema: exploratory assessment within
the Diabetic Retinopathy Clinical Research Network. Retina.
33:2080–2088. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lee SJ, Kim ET and Moon YS: Intravitreal
bevacizumab alone versus combined with macular photocoagulation in
diabetic macular edema. Korean J Ophthalmol. 25:299–304. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Karim R, Sykakis E, Lightman S and
Fraser-Bell S: Interventions for the treatment of uveitic macular
edema: a systematic review and meta-analysis. Clin Ophthalmol.
7:1109–1144. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Stefanini FR, Badaró E, Falabella P, Koss
M, Farah ME and Maia M: Anti-VEGF for the management of diabetic
macular edema. J Immunol Res. 2014:6323072014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhang Z, Wei Y, Jiang X, Qiu S and Zhang
S: A machine-independent method to have active removal of 5,000
centistokes silicone oil using plastic infusion tube and 23-gauge
microcannulas. BMC Ophthalmol. 15:1142015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Oster SF, Mojana F, Bartsch DUG, Goldbaum
M and Freeman WR: Dynamics of the macular hole-silicone oil
tamponade interface with patient positioning as imaged by spectral
domain-optical coherence tomography. Retina. 30:924–929. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lordan JT, Wilkins M and Karanjia ND:
Delayed bile leakwith avastin after liver resection for metastatic
colorectalcancer. Hepatogastroenterology. 58:1769–1770.
2011.PubMed/NCBI
|