Introduction
Orbital foreign body mainly enters the orbit between
the eye and orbital wall, but may occasionally enter the orbit
through the eye or by the paranasal sinus into the orbit. According
to the foreign species, they can be divided into metallic bodies
and non-metallic ones, and the latter can be further divided into
irritant and non-irritant foreign body. Stimulation of a foreign
body is an unstable substance of physicochemical properties, such
as plant bodies, gunpowder, grease and wax, which can cause severe
tissue reaction or infection and inflammation. Non-irritating
common foreign body such as glass, stones, gravel, and plastic do
not cause severe complications afterwards except mechanical injury
(1,2).
In this study, a retrospective analysis of 15
patients with an orbital foreign body was performed at the Research
Institute of Eye Diseases from May 2007 to November 2011. Among
these, there were 4 cases of plant bodies, 3 cases of metallic
foreign body, 2 cases of glass foreign body, 2 cases of osseous
foreign body and 4 others. Twelve cases had debridement and suture
before removing the foreign bodies. In 1 case, plant bodies were
taken out in two separate operations. The shortest miss diagnosis
time was 3 days, and the longest was 15 months. According to the
clinical imaging data and each operation case, the reasons for the
easily missed diagnosis of orbital foreign body were analyzed. This
study was approved by the Ethics Committee of Research Institute of
Eye Diseases. Signed written informed consents were obtained from
all participants before the study.
Case report
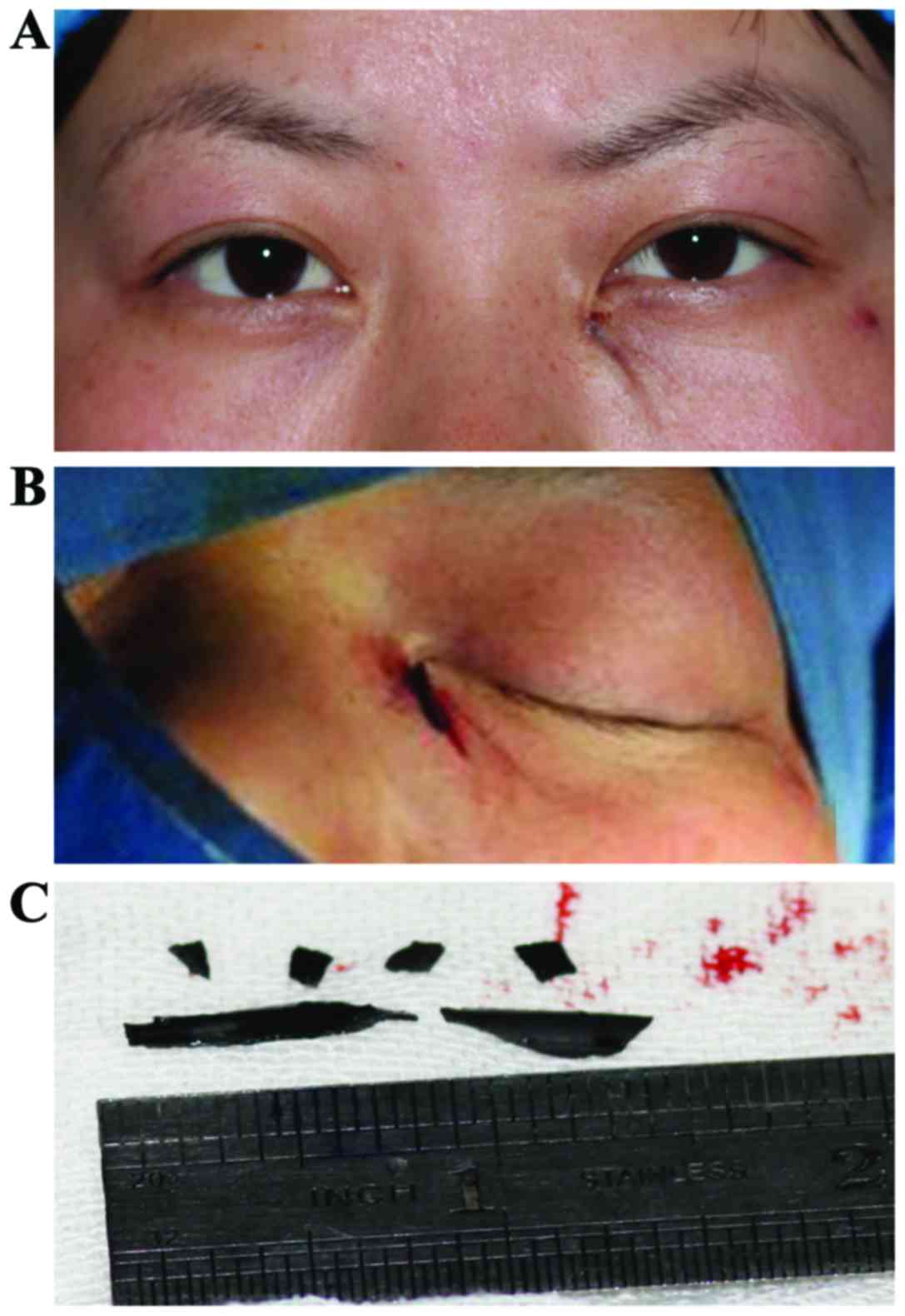
Case 1, subcutaneous eyewinker
A 25-year-old female patient had an unknown object
stab wound, and a suture skin wound by local debridement suture,
asked for treatment because of subcutaneous eyewinker feeling. The
patient was examined for left lacrimal sac area accessible cords,
hard nodules, wound healing, and flushing lacrimal passage.
Ophthalmology examination had no positive signs. CT examination was
conducted to examine the lacrimal sac area with a bar-shaped
high-density shadow, and suspected subcutaneous eyewinker. Under
local anesthesia, the area along the original wound was expanded
and several pieces of tin aluminum soft foreign body were removed
(Fig. 1).
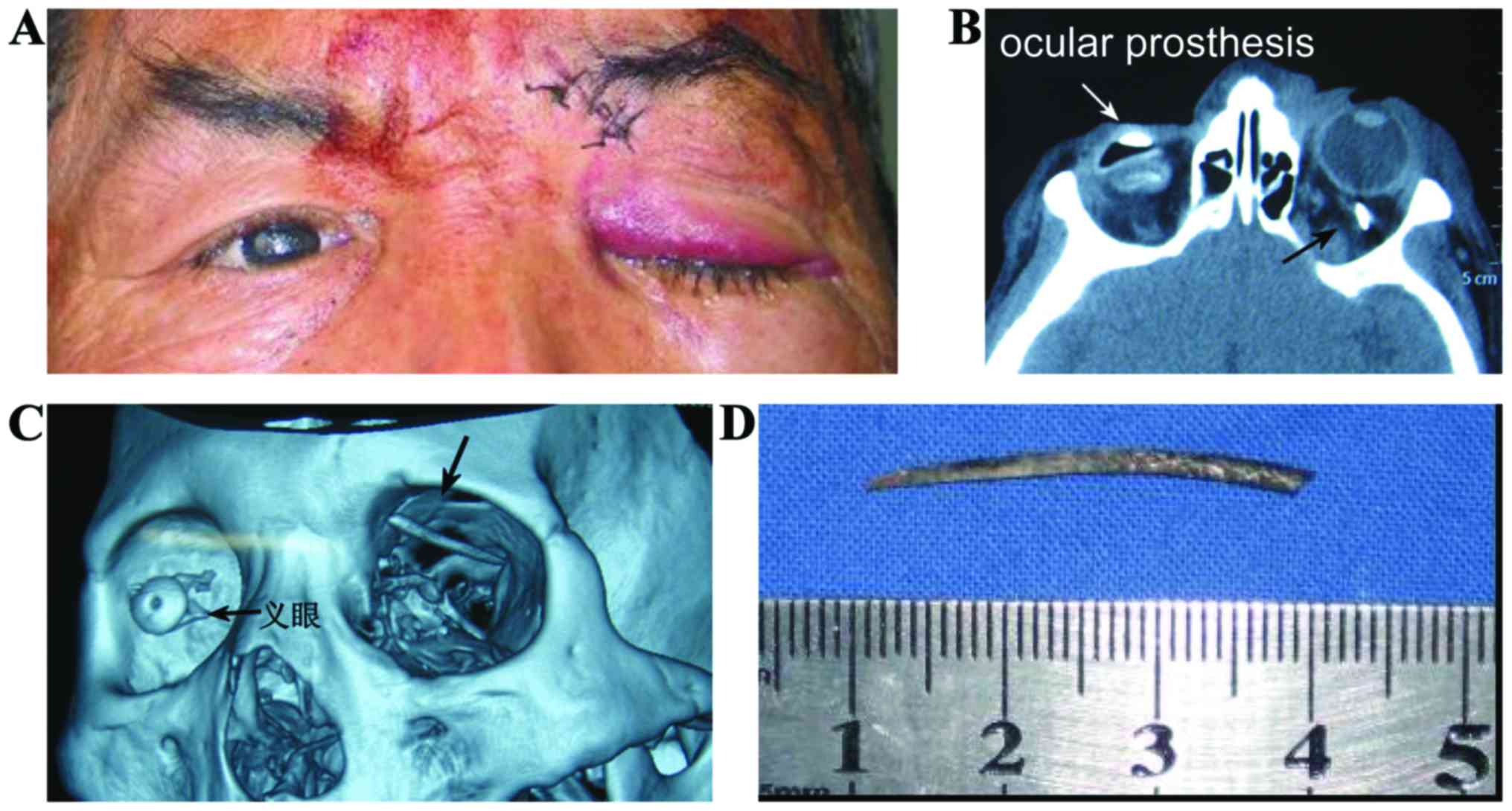
Case 2, metal foreign body
A male patient, aged 52 years, had reinforced stab
wound with the local skin suture, and had postoperative ptosis and
eye movement disorder. CT examination showed that the metallic
foreign body was present in orbit above. Under general anesthesia,
along the original road, a metal foreign body, approximately 3 cm
in length was removed (Fig. 2).
Case 3, wooden foreign body
A male patient aged 32 years had no special
treatment after a drunken motorcycle accident. A week later, an
upper eyelid mass was found at the admitting hospital where the
patient was given antibiotic treatment and the mass was considered
a ‘sty’ with poor efficacy. In December 2010 the patient presented
at the Research Institute of Eye Diseases, where a CT scan showed
that there were 2 pieces of low-density shadows above orbital with
suspected foreign body. Under local anesthesia, the region was
explored, and 2 blocks of wooden foreign body were removed.
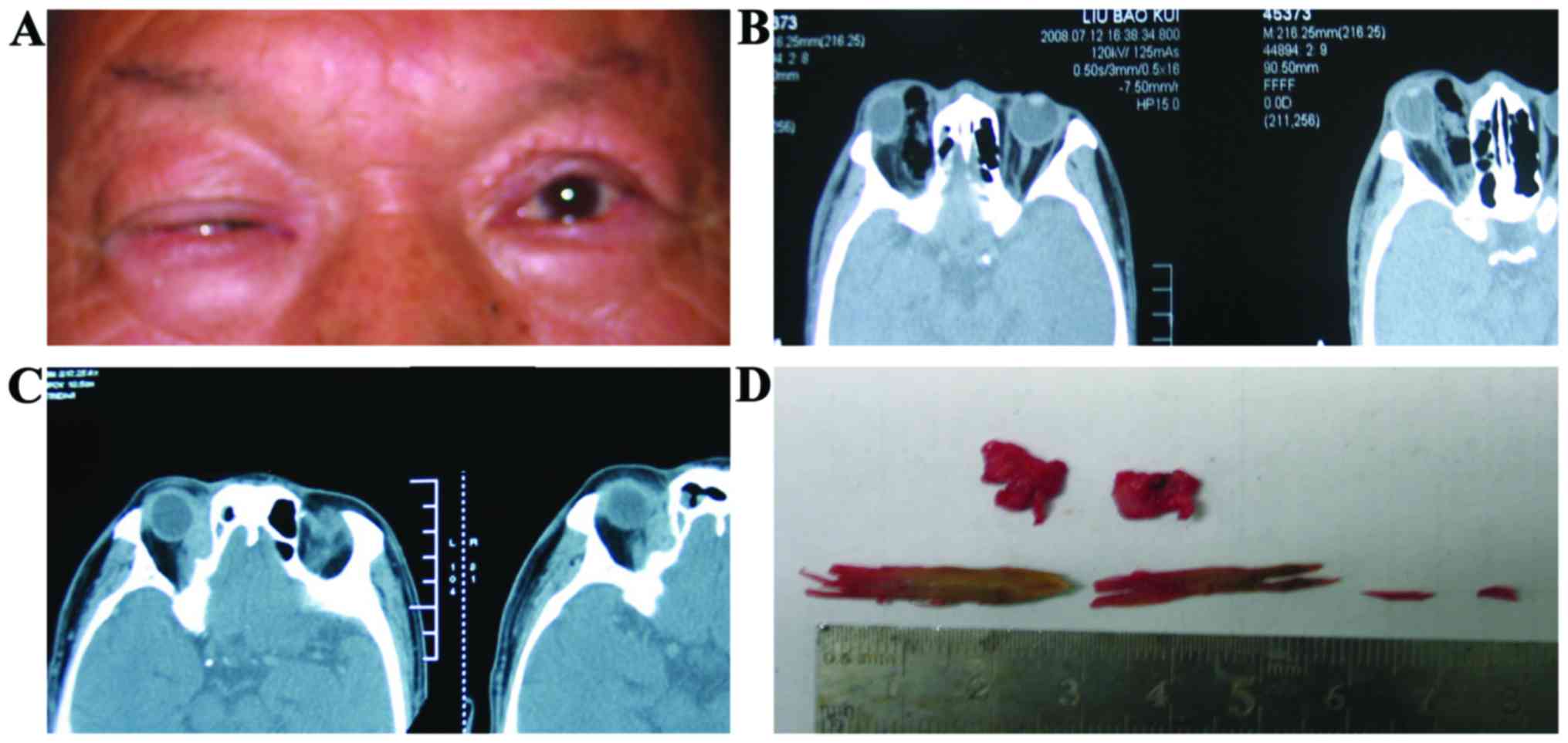
Case 4, wooden foreign body
A male patient, aged 56 years, had a branch stab
wound. Three months after debridement and suturing, postoperative
wound repeated inflammation with secreta outflow and eyeball
movement disorder to the internal oblique fixed, with declining
eyesight. In the local hospitals no foreign body was identified by
CT check. In our hospital, the CT was rechecked and an irregular
high-density shadow was identified in the medial orbital with a
low-density intermediate shadow, and intraorbital foreign body was
suspected. Under general anesthesia exploratory operation was
carried out and several short wooden foreign bodies were removed
(Fig. 3).
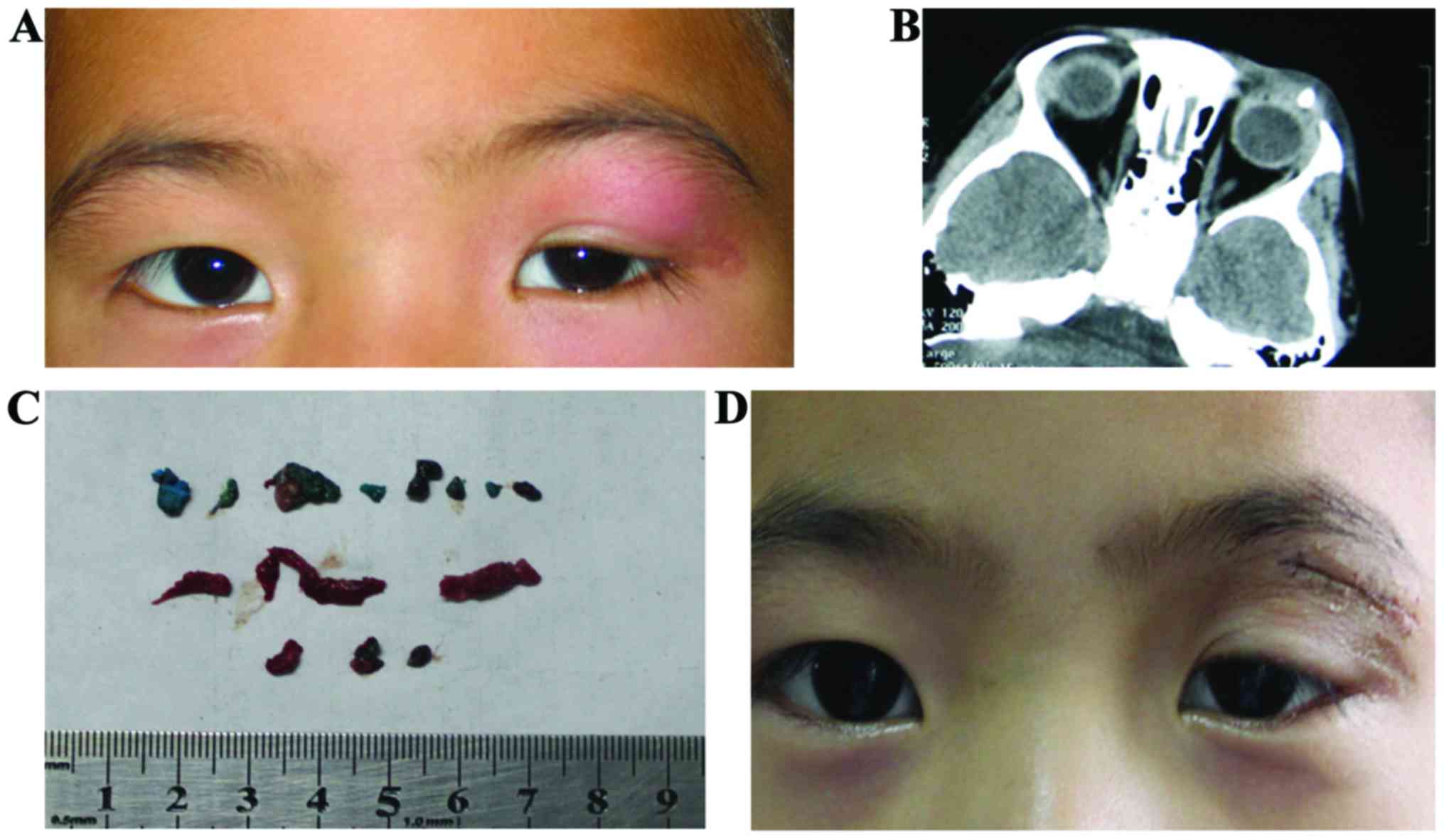
Case 5, chemical foreign bodies
Left upper eyelid of a 5-year-old boy was injured by
a door. A week with repeated redness and free remission after
antibiotic treatment. In our hospital, CT scan analysis identified
irregular high-density shadow above the orbital, a shadow similar
to a vein stone in the middle. His examination history was checked,
3 months earlier, debridement and suturing was performed following
a crayon stab wound. Under general anesthesia, local proliferation
of granulation tissue wrapped with green wax foreign body was
identified (Fig. 4).
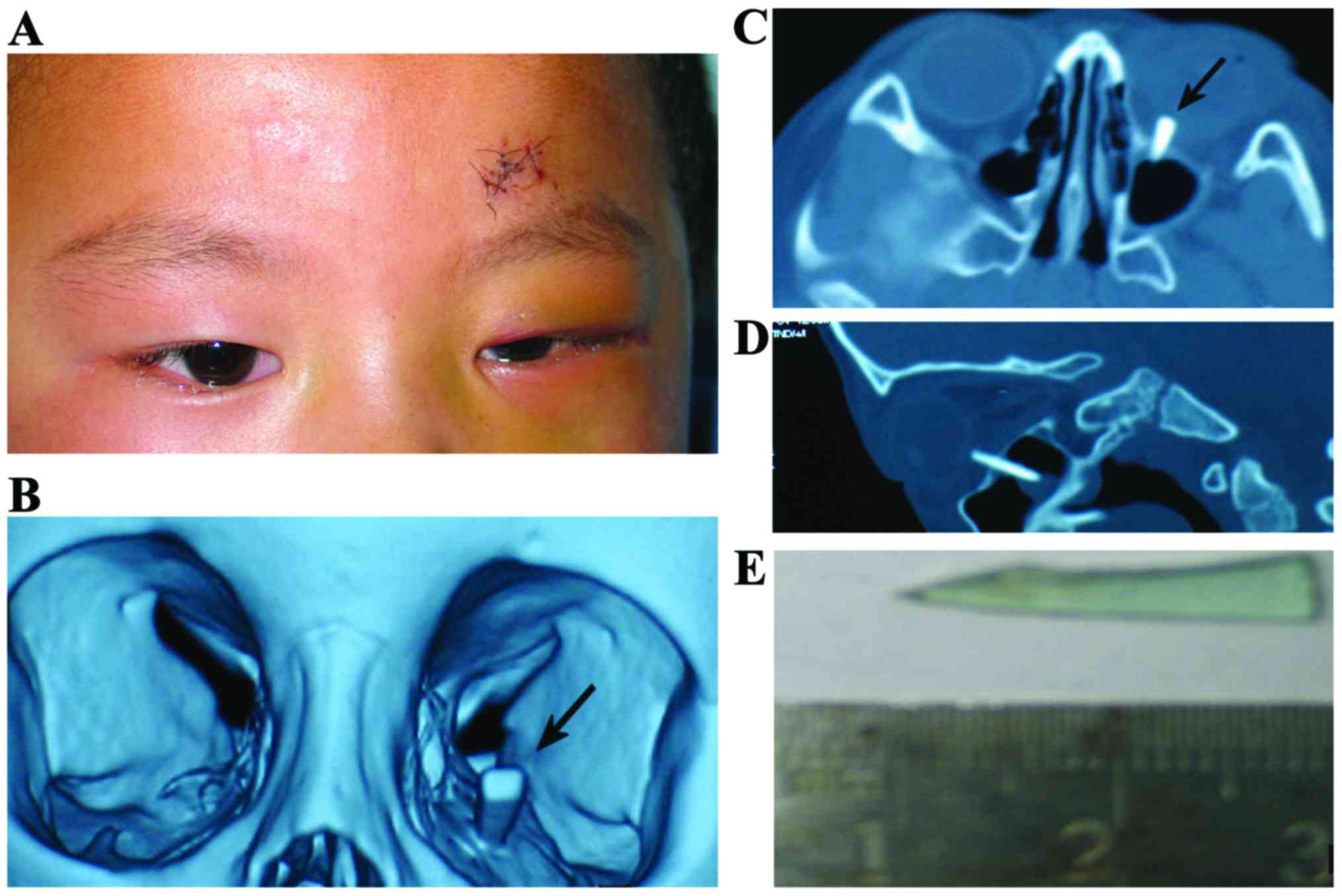
Case 6, glass foreign body
A male patient, aged 3 years, touched the door after
being hurt by glass. The local hospital took skin wound debridement
and sutured the superciliary arch. Due to eyeball movement disorder
and poor eyelid closure, treatment was requested. In our hospital,
the CT scan revealed a high-density foreign body shadow bar under
orbital. The glass foreign body was removed under general
anesthesia (Fig. 5).
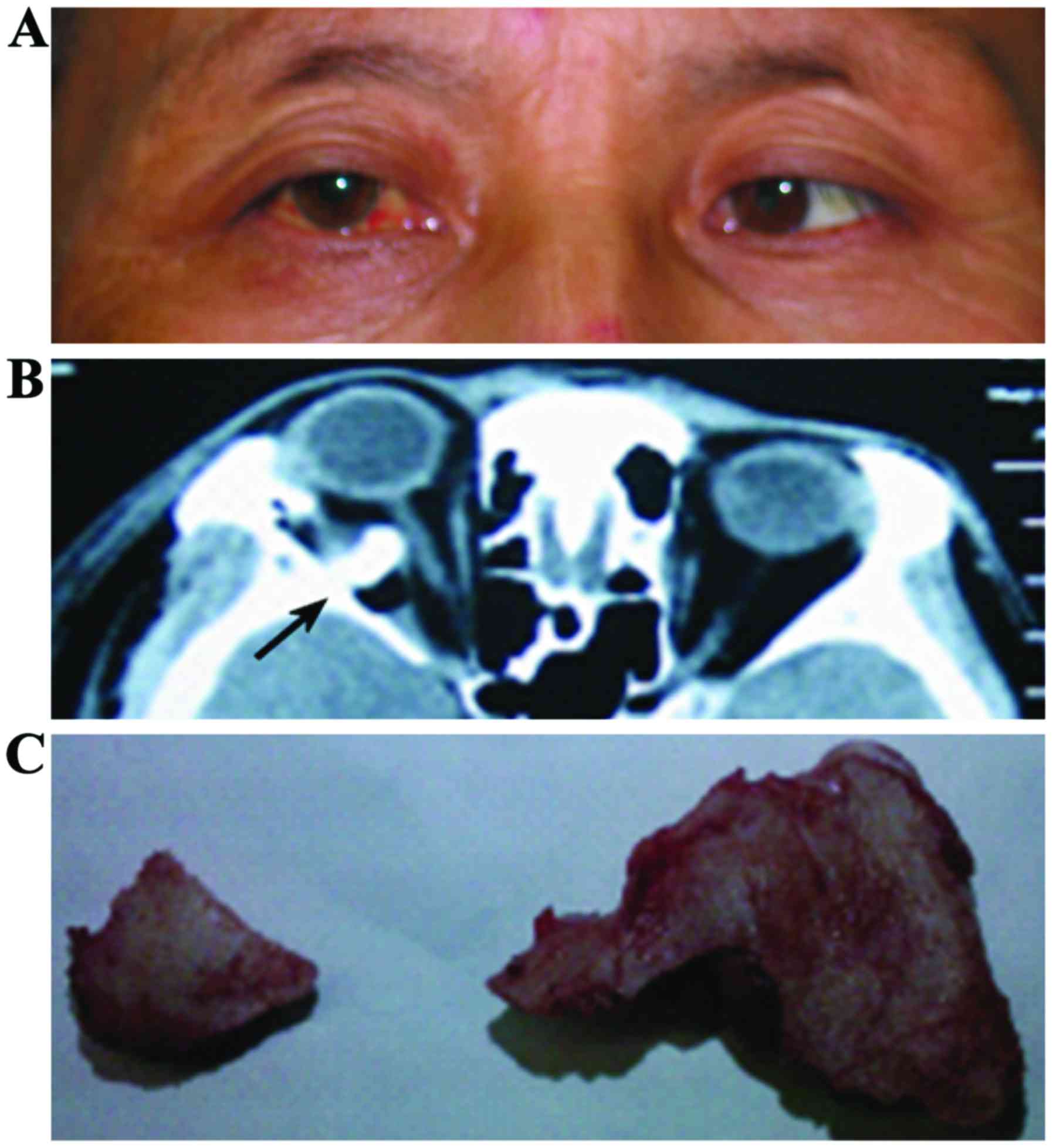
Case 7, bone foreign body
A male patient aged 56 years, after falling, had
diplopia with right-eye proptosis. The CT scan showed a fracture of
right lateral orbital zygomatic arch with intraorbital foreign body
and lateral rectus muscle transposition. Bone foreign body was
removed under general anesthesia (Fig.
6).
Discussion
The diagnosis of orbital foreign body has the
following limitations: i) The complexity of trauma among children,
and intoxicated patients who cannot describe detailed trauma after
a car accident, explosion, or the moment of injury and also cannot
determine the injury objects. ii) The imaging findings of
diversification, especially some non-metal foreign body lack
typical imaging findings. iii) During the clinical diagnosis and
treatment process, doctors often only pay attention to the wound
treatment, but fail to make an early diagnosis of orbital foreign
body resulting in missed diagnosis. Ophthalmology doctors should
master data, detailed history of skilled imaging data, be familiar
with orbital operation approach and have operation skills, in order
to reduce the rate of missed diagnosis of orbital foreign body, and
to improve the success rate of removal of foreign bodies (1,2).
Therefore, we summarize the experience of diagnosis and treatment
of orbital foreign bodies as follows:
i) Eyes perforating injury needs to pay attention to
the possibility of intraorbital foreign body retention: All orbital
penetrating injury patients should be asked in detail about the
environment where injury or wound occurred and possible vulnerant.
For local repeated inflammation, unknown cause should be traced
back to the history. The results of debridement and suturing should
be examined properly and attention should be paid for the possible
presence of residual foreign body. Once there are visible symptoms,
such as pain, swelling, heat, eyeball movement disorder, proptosis,
eyelid closure, and eyesight decline, further consideration should
be given to the possibility of orbital cellulitis and orbital apex
syndrome, orbital fracture, nerve injury, optic nerve injury,
carotid cavernous fistula, and combined with the history, signs,
imaging effects, an assessment of injury should be made to further
eliminate the intraorbital foreign body.
ii) Improved imaging examination: CT examination is
a reliable basis for diagnosis of orbital foreign body.
Ophthalmologists should be familiar with the CT imaging of the
intraorbital foreign body with different nature. CT check generally
chooses axial and coronal to fully understand the nature and the
position of the foreign body, and avoid some small foreign bodies
on the orbital roof and orbital floor resulting in misdiagnosis
caused by the volume effect. Tissue window can display the fracture
and rectus damage situation of orbital. Metal foreign body is easy
to be found in the CT examination. When it is a metallic foreign
body, the artifacts can be eliminated by using bone window. Glass
foreign body performance is that the density value is between
+300--+600 Hu and the boundary is clear. Plant or wooden foreign
bodies in the early period in general are negative on CT, but could
be identified with hemorrhage and air. Long-term retention of plant
foreign bodies due to absorption of tissue fluid or chronic
inflammation and other factors can be manifested as irregular
high-density shadow (3). Bone
foreign body in general is the same as defect orbital bone with the
same density.
iii) Indications and principle of orbital foreign
body removal: a) All stimulation of foreign body such as plants,
non-metal foreign body should be completely removed by operation as
soon as possible, in order to avoid the pyogenic infection and
fistula formation. b) A foreign body of eye movement disorder,
compression symptoms and visual dysfunction should be treated. c)
Orbital small metallic foreign body, glass and sand foreign bodies
that have not caused any eye symptoms can be observed without
removal. (d) For greater operation difficulty and vulnerable injury
of the more important normal tissue, blood vessels, nerves and
other factors, foreign body near the orbital apex, follow-up
observation is preferred, as long as it does not cause significant
visual impairment (3–6).
iv) Operation method to take out orbital foreign
body: a) A general anesthesia is usually a good idea to eliminate
the stress of the patient that will be good to cooperate, so
surgeons can fully expose the operation field and have full
debridement. If the object is clear with the superficial location,
local anesthesia can also be used. b) Generally, operation incision
along the original wound or foreign body can be near the skin
incision, when necessary, it is appropriate to expand the incision
for correct use of instruments. c) Along the original road into
looking for foreign body, Meilan mark can be injected through road
before entering. d) During separation, it was found that the pus
cavity had reached the peripheral location of foreign body. e)
Foreign body should be removed and area around the abscess cavity
should be cleaned up, because plant bodies could contaminate during
the process of removal and break foreign body into several segments
or debris which should be cleaned as far as possible. Foreign body
that has caused chemical reaction and contamination or inflammatory
reactions leading to decaying of tissue, should be appropriately
removed and rinsed thoroughly (7,8).
With the development of transportation and city
construction, orbital trauma incidences are increasing every year.
In addition, since the reforms and opening up, great changes have
taken place in China's occupational structure, but grassroots
employees such as the production workers and agricultural laborers
still account for a large proportion. But the basic labor people
especially manual workers are at a high risk of ocular trauma and
multiple injuries, and soon after injuries, majority of them have
treatment in primary hospitals because of distance and time. So
ophthalmologists particularly primary ophthalmologists should be
fully aware of more complexities of diagnosis and treatment of
orbital foreign body in order to avoid misdiagnosis, missed
diagnosis and delay in treatment. In the process of diagnosis and
treatment, attention should be paid to the following problems: i)
Inquire the details of injuries, and be alert to the possibility of
intraorbital foreign bodies. ii) During the emergency treatment of
the wound, necessary cleaning and exploration should be performed.
iii) After the injury or wound suture, CT check is necessary. iv)
Ability to correctly read scans and proper clinical training. v)
For patients with ocular symptoms or visual dysfunction, the
diagnosis should be further clarified, examined and explored. vi)
Patients who fail to be clearly diagnosed, should be transferred to
the orbital disease specialists or higher level hospitals for
further treatment as soon as possible.
References
|
1
|
Elsner H, Hoerauf H and Laqua H: Glass
orbital foreign body 15 years after windshield injury.
Ophthalmologe. 99:488–489. 2002.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nielsen R Tyranski, Christensen S, Rosbach
S Buur and Bjerre PK: Orbital injury following accidental fall.
Intra-orbital wooden foreign body. Radiologe. 38:545–547. 1998.(In
German). PubMed/NCBI
|
|
3
|
Zhu Y, Li ZG and Zhang XF: Problems in
diagnosis and treatment of orbital foreign body - an analysis of 24
cases. Zhonghua Yan Ke Za Zhi. 44:676–680. 2008.(In Chinese).
PubMed/NCBI
|
|
4
|
Chung IY, Seo SW, Han YS, Kim E and Jung
JM: Penetrating retrobulbar orbital foreign body: A transcranial
approach. Yonsei Med J. 48:328–330. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Naik MN, Das S, Oluyemi F and Honavar SG:
An extraordinary orbital foreign body. Ophthal Plast Reconstr Surg.
27:e149–e152. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zinreich SJ, Miller NR, Aguayo JB, Quinn
C, Hadfield R and Rosenbaum AE: Computed tomographic
three-dimensional localization and compositional evaluation of
intraocular and orbital foreign bodies. Arch Ophthalmol.
104:1477–1482. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Neumann K, Ehrich D and Bloching M:
Orbital foreign bodies - diagnostics, therapy and management.
Laryngorhinootologie. 84:187–192. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
van Putten SM, Wübben M, Plantinga JA,
Hennink WE, van Luyn MJ and Harmsen MC: Endotoxin contamination
delays the foreign body reaction. J Biomed Mater Res A. 98:527–534.
2011. View Article : Google Scholar : PubMed/NCBI
|