Introduction
Acidosis is the most common acid-base disturbance,
with metabolic acidosis potentially indicating a more severe course
and worse outcome. The actual incidence and prevalence of metabolic
acidosis have not been established in critically ill and general
patients. Often this disorder is a marker for underlying pathology,
and the most commonly encountered causes of metabolic acidosis are
renal insufficiency, sepsis, and diabetic ketoacidosis. Although
recent studies showed that metabolic acidosis is associated with
high mortality and increased the length of stay in the hospital and
ICU (1,2), it remains uncertain whether or not
there is a true cause relationship between metabolic acidosis and
adverse clinical outcomes.
The kidney is a principally responsible organ for
retention and excretion of electrolytes and maintaining acid-base
homeostasis in healthy individuals (3). Both acute kidney injury (AKI) and
chronic kidney disease (CKD) can cause metabolic acidosis. But on
the other hand, accumulating evidence identifies metabolic acidosis
not only as a consequence of but as a contributor to, the
progression of kidney dysfunction in patients with CKD (4). The mechanisms may be that metabolic
acidosis can reduce renal blood flow in healthy human volunteers
(5) and increase inflammatory
mediator release (6). A recent
experimental study proved that metabolic acidosis exacerbates
ischemia/reperfusion-induced AKI (7). However, Limited data exist about the
harmful effect of metabolic acidosis on the development of AKI.
In general, a diagnosis of metabolic acidosis is
based on arterial blood gas (ABG) analysis after an arterial
puncture which may lead to local hematoma and other complications.
Carbon dioxide combining power (CO2CP) in the venous
blood which is a measure of the alkali reserve, can help in the
diagnosis of the metabolic types of acidosis and alkalosis. Even
though CO2CP does not give any idea of the ratio between
carbonic acid and bicarbonate, it enables timely diagnosis and
proper corrective therapy in metabolic acidosis if respiratory
types of acid-base disturbances do not exist.
In this study, we hypothesized that metabolic
acidosis might be associated with the development of AKI and
hospital mortality, and decreased CO2CP can be used to
an indicator of metabolic acidosis in non-respiratory patients. The
study was aimed at identifying the variables in acid-base status at
admission which were associated with the occurrence of renal
dysfunction and hospital mortality. The secondary aims were to
determine the relationship between CO2CP and other
variables in the electrolyte and acid-base status and to screen
high-risk patients of AKI and hospital mortality when decreased
CO2CP occurs.
Materials and methods
Study population and data
collection
This retrospective study included all adult patients
admitted consecutively to Zhongshan Hospital, Fudan University in
Shanghai, China, between October 01, 2014 and September 30, 2015.
This study was approved by the institutional review board of the
ethics committee, Zhongshan Hospital, Fudan University, Shanghai
China. The requirement for informed consent was waived for this
observational survey. The patient records and information were
anonymized and de-identified before analysis.
Exclusion criteria were the following: Age of fewer
than 18 years, serum creatinine (SCr) at admission >115 µmol/l,
CO2CP at admission >29 mmol/l, history of CKD and
respiratory diseases, hospital admissions for respiratory diseases.
The respiratory diseases included inflammatory lung diseases,
restrictive lung diseases, respiratory tract infections, lung
tumors, pleural cavity diseases and pulmonary vascular
diseases.
All the data were collected from an electronic
medical record database. The data included demographics, categories
of underlying diseases, mean blood pressure (MBP) and laboratory
values at admission. However, we focused on the data of electrolyte
and acid-base status in all included patients. The incidence of
AKI, hospital mortality, hospital stay, and costs was also
recorded.
Definitions and calculation
AKI was defined using Kidney Disease: Improving
Global Outcomes criteria (8) as an
increase in serum creatinine (SCr) ≥0.3 mg/dl (≥26.5 µmol/l) within
48 h, or an increase in SCr to ≥1.5 times baseline known or
presumed to have occurred within the prior seven days. The patients
who developed AKI during the following hospitalization were divided
into AKI group, while those who did not be split into the non-AKI
group.
All samples were analyzed in the central laboratory
of the Institution. Anion gap (AG) was calculated by the standard
formula (9):
AG=[Na+]−[Cl−]−[HCO3−],
with an elevated AG defined as greater than or equal to 16 mmol/l.
Strong ion difference (SID) is the sum of strong cations minus the
sum of strong anions. Strong ion gap (SIG) is the difference
between the apparent SID (SIDa) and the effective SID (SIDe). SIG
represents the sum of any unmeasured strong positive and negative
ions with an elevated SIG defined as greater than 2 mmol/l.
SIDa=[Na+]+[K+]+[Ca2+]+[Mg2+]-[Cl−].
SIDe=[HCO3−]+(0.123xpH-0.631)x[Alb]+(pH-0.469)x[Pi].
SIG=SIDa-SIDe (10). Calculated
osmolality=2x[Na+] +[glucose]+[urea], with the normal
range from 280 to 310 mOsm/l. Hypernatremia, hyponatremia,
hyperkalemia, hypokalemia, hyperchloremia, hypochloremia,
hypercalcemia, hypocalcemia, hyperphosphatemia, hypophosphatemia,
hypermagnesemia, hypomagnesemia, hyperuricemia and hypouricemia
were defined according to the reference ranges provided by the
central laboratory. Metabolic acidosis includes simple and complex
metabolic acidosis, and the latter may exist in dual or triple
acid-base disturbances. Simple, dual and triple acid-base
disturbances were diagnosed according to the flow diagrams
described by Milford Fulop (11).
Decreased CO2CP was defined when it was lower than 23
mmol/l (normal range: 23–29 mmol/l).
Statistical methods
The data were analyzed using SPSS version 24.0
software (SPSS, Chicago, IL, USA). Continuous variables are
presented as mean ± SD if they were statically normally distributed
and categorical variables as numbers and percentages. Moreover,
they were compared using the Student t-test for continuous
variables and the χ2 test for categorical variables.
Medians and interquartile ranges are presented when variables are
not normally distributed, and they were compared using Mann-Whitney
U test. Multiple regression binary logistic regression with the
Wald forward stepwise method was performed to evaluate the
independent risk factors for the occurrence of AKI and hospital
mortality, and the results are presented as odds ratios (ORs) and
95% confidence intervals (CIs). We also used Cox proportional
hazard model with the Wald forward stepwise method to analyze the
independent predictors of AKI and hospital mortality after
propensity scores matching, and the results are presented as hazard
ratios (HRs) and 95% CIs. The significant acceptance and removal
levels for a covariate were set at 0.05 and 0.1, respectively.
Multiple linear regression analysis with the stepwise method was
used to determine the relationship of CO2CP and other
variables. The ability of CO2CP to predict AKI and
hospital mortality, and to diagnose acid-base disturbances was
assessed by plotting the receiver operating characteristic (ROC)
curves and further reported as areas under the curve (AUC) with 95%
CIs. An AUC-ROC value of >0.7 was taken to indicate reasonable
biomarker performance (12). ROC
curve optimal cut-off values were defined as the point that
maximized the Youden index, defined as (sensitivity +
specificity)-1 (13). A P-value
<0.05 was considered to indicate statistical significance.
Propensity score matching
To reduce the impact of potential confounding
factors in an observational study, we also performed propensity
score matching for each AKI using a multivariable logistic
regression analysis model based on the following covariates: Age,
sex, SCr and BUN at admission. Propensity scores were then employed
using the nearest neighbor matching algorithm. Matching was
performed with a computer application implemented in SPSS 24.0 and
R software version 3.2.2 to select for the most similar propensity
scores and to create 1:2 matched pairs (matching the non-AKI to
AKI). To identify independent risk factors of AKI and hospital
mortality in patients with ABG, we conducted three Cox proportional
hazard models. We included all potential factors associated with
AKI and hospital mortality in model 1, the level of
HCO3− was not included in model 2, and
PaCO2 was not considered in model 3.
Results
Patient characteristics
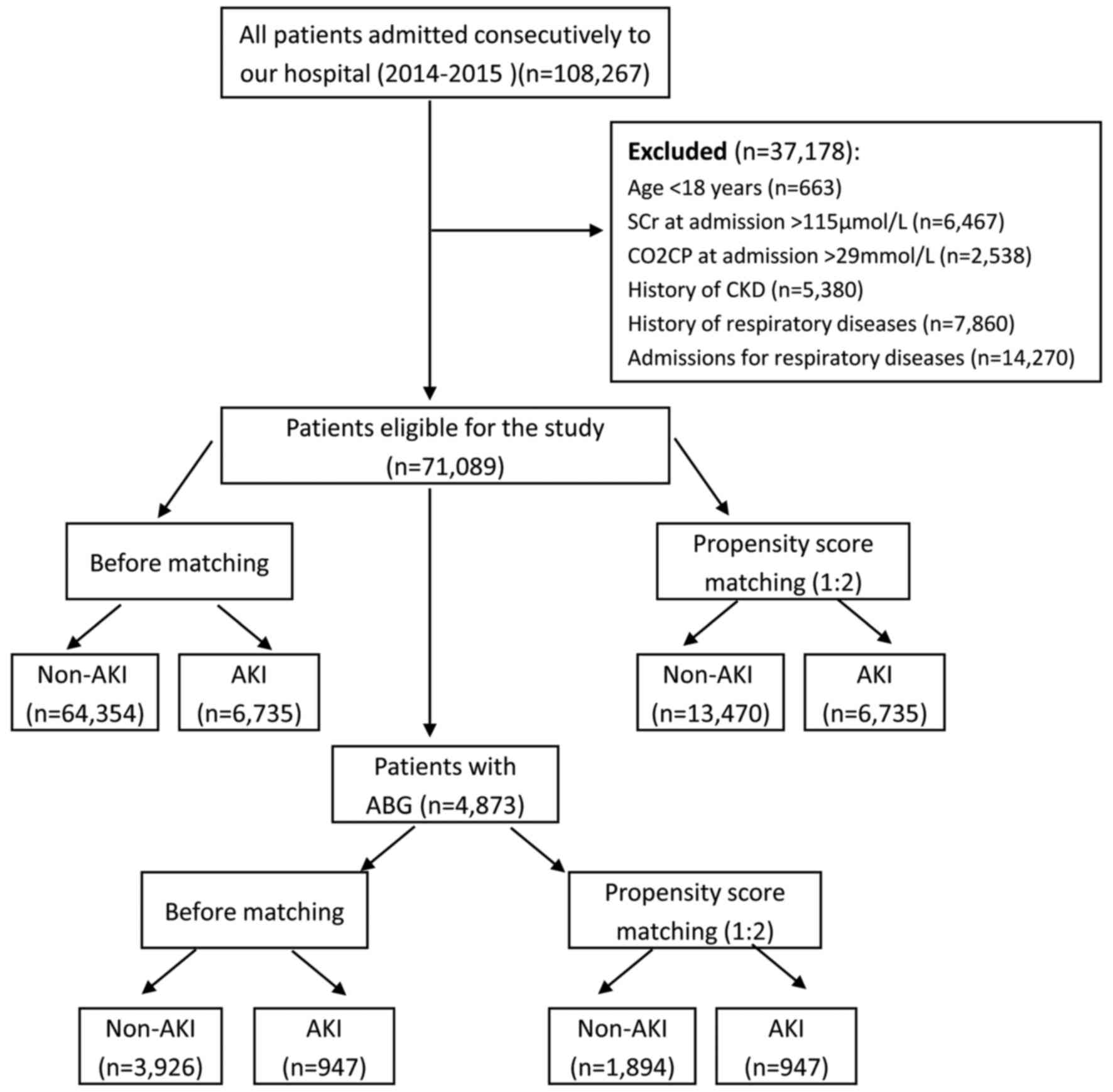
After screening, a total of 71,089 patients met the
inclusion criteria, and there were 4,873 patients with ABG
analysis. The flow-chart of this study was showed in Fig. 1. In all included patients, the
incidence of AKI was 9.5%, and the hospital mortality was 0.7%,
while the rates in patients with ABG were 19.4 and 1.6%,
respectively. The top four underlying diseases with a high
incidence of AKI were cardiothoracic surgery (40.7%), cancer
(15.8%), general surgery (10.3%) and neurological diseases (10.1%),
while the incidence of AKI in cardiovascular patients was 4.3%.
Characteristics of all subjects before and after propensity score
matching were listed in Table I,
while the details of patients with ABG were showed in Table II. By the propensity score, patients
in AKI group were successfully matched to patients in the non-AKI
group with the ratio of 1:2 in all patients and patients with ABG.
After propensity score matching, no statistically significant
baseline characteristics in age, sex, SCr and BUN at admission
between AKI and non-AKI groups were found. After propensity
matching of all patients, the hospital mortality in AKI group was
eight times higher than that in the non-AKI group (4.0 vs. 0.5%,
respectively, P<0.001). The hospital stay was longer
(P<0.001), and the cost was higher (P<0.001) in AKI group
than these in the non-AKI group.
 | Table I.Baseline characteristics of all
included patients before and after propensity score matching. |
Table I.
Baseline characteristics of all
included patients before and after propensity score matching.
|
| Before matching | Propensity score
matching (1:2) |
|---|
|
|
|
|
|---|
| Variable | Non-AKI
(n=64,354) | AKI (n=6,735) | P-value | Non-AKI
(n=13,470) | AKI (n=6,735) | P-value |
|---|
| Age, yr | 57.0±14.3 | 59.3±14.6 |
<0.001a | 59.1±14.5 | 59.3±14.6 | 0.275a |
| Male sex, n (%) | 38,131(59.3) | 4,274 (63.5) | <0.001 | 8467
(62.9) | 4274
(63.5) | 0.404 |
| Renal function at
admission |
|
|
|
|
|
|
| SCr,
µmol/l | 70.0
(59.0–82.0) | 76.0
(63.0–91.0) | <0.001 | 76.0
(63.0–89.0) | 76.0
(63.0–91.0) | 0.086 |
| BUN,
mmol/l | 4.8 (3.9–5.9) | 5.2 (4.1–6.1) | <0.001 | 5.3 (4.2–6.2) | 5.2 (4.1–6.1) | 0.096 |
| Underlying
diseases, n (%) |
|
|
|
|
|
|
|
Cardiovascular | 16,543 (25.7) | 741
(11.0) | <0.001 | 3,886 (28.8) | 741
(11.0) | <0.001 |
| General
surgery | 9,323
(14.5) | 1,073 (15.9) | 0.001 | 1,771 (13.1) | 1,073 (15.9) | <0.001 |
|
Digestive | 7,895
(12.3) | 326
(4.8) | <0.001 | 1,565 (11.6) | 326
(4.8) | <0.001 |
|
Cancer | 7,297
(11.3) | 1,371 (20.4) | <0.001 | 1,410 (10.5) | 1,371 (20.4) | <0.001 |
|
Orthopedic surgery | 3,533 (5.5) | 147
(2.2) | <0.001 | 700
(5.2) | 147
(2.2) | <0.001 |
|
Cardiothoracic surgery | 2,549 (4.0) | 1,752 (26.0) | <0.001 | 589
(4.4) | 1,752 (26.0) | <0.001 |
|
Endocrine | 2,297 (3.6) | 58
(0.9) | <0.001 | 457
(3.4) | 58
(0.9) | <0.001 |
|
Hematological | 2,199 (3.4) | 352
(5.2) | <0.001 | 407
(3.0) | 352
(5.2) | <0.001 |
|
Renal | 1,941 (3.0) | 114
(1.7) | <0.001 | 476
(3.5) | 114
(1.7) | <0.001 |
|
Neurological | 1,835 (2.9) | 207
(3.1) | 0.299 | 382
(2.8) | 207
(3.1) | 0.344 |
|
Gynecological | 1,779 (2.8) | 104
(1.5) | <0.001 | 312
(2.3) | 104
(1.5) | <0.001 |
|
Others | 7,163
(11.1) | 490
(7.3) | <0.001 | 1,515 (11.2) | 490
(7.3) | <0.001 |
| Clinical data at
admission |
|
|
|
|
|
|
|
CO2CP, mmol/l | 24.0
(23.0–26.0) | 24.0
(22.0–26.0) | <0.001 | 24.0
(23.0–26.0) | 24.0
(22.0–26.0) | <0.001 |
| MBP,
mmHg | 93.3
(86.7–98.7) | 92.7
(83.3–97.3) | <0.001 | 93.3
(86.7–98.7) | 92.7
(83.3–97.3) | <0.001 |
| WBC,
109/l | 5.9 (4.7–7.7) | 6.1 (4.8–7.8) | <0.001 | 5.9 (4.8–7.8) | 6.1 (4.8–7.8) | <0.001 |
|
Hemoglobin, g/l | 131.0
(119.0–143.0) | 126.0
(111.0–139.0) | <0.001 | 131.0
(118.0–143.0) | 126.0
(111.0–139.0) | <0.001 |
| AST,
U/l | 20.0
(16.0–28.0) | 23.0
(17.0–36.0) | <0.001 | 20.0
(16.0–28.0) | 23.0
(17.0–36.0) | <0.001 |
| ALT,
U/l | 19.0
(13.0–30.0) | 20.0
(13.0–36.0) | <0.001 | 19.0
(13.0–30.0) | 20.0
(13.0–36.0) | <0.001 |
| TBIL,
µmol/l | 9.5 (7.0–13.0) | 10.5
(7.4–15.4) | <0.001 | 9.5 (7.0–13.0) | 10.5
(7.4–15.4) | <0.001 |
|
Albumin, g/l | 40.0
(37.0–43.0) | 38.0
(35.0–41.0) | <0.001 | 40.0
(37.0–43.0) | 38.0
(35.0–41.0) | <0.001 |
| SUA,
mmol/l | 297.0
(240.0–357.0) | 305.0
(239.0–377.0) | <0.001 | 311.0
(251.0–376.0) | 305.0
(239.0–377.0) | <0.001 |
|
Glucose, mmol/l | 5.2 (4.7–6.7) | 5.3 (4.7–6.7) | 0.126 | 5.3 (4.8–6.8) | 5.3 (4.7–6.7) | 0.315 |
| Na,
mmol/l | 141.0
(139.0–143.0) | 141.0
(138.0–143.0) | <0.001 | 141.0
(139.0–143.0) | 141.0
(138.0–143.0) | <0.001 |
| K,
mmol/l | 4.0 (3.8–4.8) | 4.0 (3.8–4.8) | 0.780 | 4.0 (3.9–4.9) | 4.0 (3.8–4.8) | 0.001 |
| Cl,
mmol/l | 103.0
(101.0–105.0) | 103.0
(100.0–105.0) | <0.001 | 103.0
(101.0–105.0) | 103.0
(100.0–105.0) | <0.001 |
| Mg,
mmol/l | 0.91
(0.86–0.86) | 0.90
(0.84–0.84) | <0.001 | 0.91
(0.86–0.86) | 0.90
(0.84–0.84) | <0.001 |
| Ca,
mmol/l | 2.31
(2.23–2.23) | 2.28
(2.16–2.16) | <0.001 | 2.31
(2.23–2.23) | 2.28
(2.16–2.16) | <0.001 |
| P,
mmol/l | 1.12
(0.99–1.99) | 1.12
(0.95–1.95) | <0.001 | 1.11
(0.98–1.98) | 1.12
(0.95–1.95) | 0.255 |
|
Osmolality, mOsm/l | 293.3
(289.6–296.6) | 292.9
(288.5–297.5) | <0.001 | 293.9
(290.1–297.1) | 292.9
(288.5–297.5) | <0.001 |
| Death, n (%) | 256 (0.4) | 268 (4.0) | <0.001 | 68 (0.5) | 268 (4.0) | <0.001 |
| Hospital stay,
days | 5.0 (2.5–8.5) | 12.5
(8.0–19.0) | <0.001 | 5.0 (3.0–8.0) | 12.5
(8.0–19.0) | <0.001 |
| Hospital cost,
RMB | 14,803.5 | 52,479.7 | <0.001 | 14,961.9 | 52,479.7 | <0.001 |
|
|
(8,020.7-35,359.8) |
(22,202.9-108,512.1) |
|
(7,993.8-37,631.1) |
(22,202.9-108,512.1) |
 | Table II.Baseline characteristics of included
patients with arterial blood gas analysis before and after
propensity score matching. |
Table II.
Baseline characteristics of included
patients with arterial blood gas analysis before and after
propensity score matching.
|
| Before
matching | Propensity score
matching (1:2) |
|---|
|
|
|
|
|---|
| Variable | Non-AKI
(n=3,926) | AKI (n=947) | P-value | Non-AKI
(n=1,894) | AKI (n=947) | P-value |
|---|
| Age, yr | 58.9±12.6 | 59.3±13.3 | 0.461a | 59.5±12.7 | 59.3±13.3 | 0.583a |
| Male sex, n
(%) | 2,366 (60.3) | 637 (67.3) | <0.001 | 1242 (65.6) | 637 (67.3) | 0.370 |
| Renal function at
admission |
|
|
|
|
|
| SCr,
µmol/l | 62.0
(55.0–72.0) | 64.0
(56.0–74.0) | 0.060 | 63.0
(56.0–72.0) | 64.0
(56.0–74.0) | 0.162 |
| BUN,
mmol/l | 4.6 (3.8–5.8) | 4.8 (3.8–5.8) | 0.001 | 4.9 (3.9–5.9) | 4.8 (3.8–5.8) | 0.501 |
| Clinical data at
admission |
|
|
|
|
|
|
CO2CP, mmol/l | 24.1±2.5 | 23.9±2.6 | 0.002a | 24.1±2.5 | 23.9±2.6 | 0.028a |
| MBP,
mmHg | 93.3
(86.0–96.0) | 93.0
(84.3–96.3) | 0.457 | 92.7
(85.3–96.3) | 93.0
(84.3–96.3) | 0.795 |
| WBC,
109/l | 5.9 (4.7–7.7) | 6.0 (4.8–7.8) | 0.093 | 5.9 (4.7–7.7) | 6.0 (4.8–7.8) | 0.128 |
|
Hemoglobin, g/l | 130.0
(118.0–141.0) | 129.0
(115.0–141.0) | 0.071 | 130.0
(118.0–142.0) | 129.0
(115.0–141.0) | 0.045 |
| AST,
U/l | 19.0
(15.0–27.0) | 21.0
(16.0–33.0) | <0.001 | 19.0
(15.0–27.0) | 21.0
(16.0–33.0) | <0.001 |
| ALT,
U/l | 18.0
(12.0–29.0) | 20.0
(13.0–34.0) | <0.001 | 18.0
(12.0–29.0) | 20.0
(13.0–34.0) | <0.001 |
| TBIL,
µmol/l | 9.5 (7.1–13.1) | 10.7
(7.6–15.6) | <0.001 | 9.5 (7.1–13.1) | 10.7
(7.6–15.6) | <0.001 |
|
Albumin, g/l | 39.0
(37.0–42.0) | 39.0
(35.0–41.0) | <0.001 | 39.0
(36.0–42.0) | 39.0
(35.0–41.0) | <0.001 |
| SUA,
mmol/l | 278.0
(226.8–332.8) | 276.0
(212.0–341.0) | 0.398 | 280.0
(229.0–334.0) | 276.0
(212.0–341.0) | 0.188 |
|
Glucose, mmol/l | 5.8±2.1 | 5.9±2.2 | 0.422a | 5.9±2.3 | 5.9±2.2 | 0.970a |
| Na,
mmol/l | 141.0
(140.0–143.0) | 141.0
(139.0–143.0) | 0.003 | 141.0
(140.0–143.0) | 141.0
(139.0–143.0) | 0.029 |
| K,
mmol/l | 4.0 (3.8–4.8) | 4.0 (3.7–4.7) | 0.255 | 4.0 (3.8–4.8) | 4.0 (3.7–4.7) | 0.126 |
| Cl,
mmol/l | 103.0
(101.0–105.0) | 103.0
(100.0–105.0) | 0.002 | 103.0
(101.0–105.0) | 103.0
(100.0–105.0) | 0.008 |
| Mg,
mmol/l | 0.92
(0.86–0.86) | 0.90
(0.84–0.84) | <0.001 | 0.92
(0.86–0.86) | 0.90
(0.84–0.84) | <0.001 |
| Ca,
mmol/l | 2.29
(2.20–2.20) | 2.27
(2.15–2.15) | <0.001 | 2.28
(2.19–2.19) | 2.27
(2.15–2.15) | 0.003 |
| P,
mmol/l | 1.12
(0.99–1.99) | 1.10
(0.94–1.94) | 0.003 | 1.11
(0.99–1.99) | 1.10
(0.94–1.94) | 0.128 |
|
Osmolality, mOsm/l | 293.3
(289.6–296.6) | 292.9
(288.5–296.5) | 0.026 | 293.3
(289.0–296.0) | 292.9
(288.5–296.5) | 0.008 |
| PH | 7.42
(7.40–7.40) | 7.42
(7.39–7.39) | 0.870 | 7.42
(7.40–7.40) | 7.42
(7.39–7.39) | 0.783 |
|
PaCO2, mmHg | 40.0
(36.0–43.0) | 39.0
(35.4–42.4) | <0.001 | 40.0
(26.0–43.0) | 39.0
(35.4–42.4) | 0.001 |
|
HCO3-, mmol/l | 25.4
(23.4–27.4) | 24.4
(21.7–26.7) | <0.001 | 23.3
(25.4–27.4) | 24.4
(21.7–26.7) | <0.001 |
| BE,
mmol/l | 1.2 (−0.7–2.7) | 0.6 (−1.9–2.9) | <0.001 | 1.2 (−0.8–2.8) | 0.6 (−1.9–2.9) | <0.001 |
| AG,
mmol/l | 14.0
(13.0–16.0) | 14.0
(13.0–16.0) | 0.172 | 14.2±2.6 | 14.4±2.9 | 0.091a |
| SIDa,
mmol/l | 48.4
(46.7–50.7) | 48.2
(46.3–50.3) | 0.046 | 48.4
(46.6–49.6) | 48.2
(46.3–50.3) | 0.222 |
| SIDe,
mmol/l | 44.2
(41.5–46.5) | 42.8
(39.0–45.0) | <0.001 | 44.0
(41.4–46.4) | 42.8
(39.0–45.0) | <0.001 |
| SIG,
mmol/l | 4.3 (2.1–6.1) | 5.6 (3.0–8.0) | <0.001 | 4.4 (2.2–6.2) | 5.6 (3.0–8.0) | <0.001 |
| Death, n (%) | 28 (0.7) | 48 (5.1) | <0.001 | 17 (0.9) | 48 (5.1) | <0.001 |
| Hospital stay,
days | 10.0
(7.0–13.0) | 15.5
(11.5–23.5) | <0.001 | 10.0
(7.0–23.0) | 15.5
(11.5–23.5) | <0.001 |
| Hospital cost,
RMB | 39,559.3
(19,529.7-58,308.5) | 73,051.7
(45,782.8-121,322.4) | <0.001 | 39,481.1
(19,587.8-58,471.2) | 73,051.7
(45,782.8-121,322.4) | <0.001 |
Clinical data at admission after
propensity matching
In all included patients, the patients in AKI group
had lower mean blood pressure, hemoglobin, albumin and a higher
number of white blood cell and indexes of liver function
(P<0.001). There was significant differences in the levels of Na
(P<0.001), K (P=0.001), Cl (P<0.001), Mg (P<0.001), Ca
(P<0.001), osmolality (P<0.001) and serum uric acid
(P<0.001) between AKI and non-AKI group. Although the median of
CO2CP in these two groups was same, the lower
interquartile was lower in AKI group than that in the non-AKI
group, and there was a significant difference (P<0.001)
(Table I).
In 4,873 patients with ABG, those in AKI group had
still lower hemoglobin and albumin, higher indexes of liver
function than these in the non-AKI group. There were significant
differences in the levels of electrolytes, including Na (P=0.029),
Cl (P=0.008), Mg (P<0.001), and Ca (P=0.003). The osmolality in
AKI group was lower than that in the non-AKI group (P=0.0008). Even
though there was no significant difference in pH and AG between
these two groups, the levels of PaCO2 (P=0.001),
HCO3− (P<0.001), BE (P<0.001), SIDe
(P<0.001) and SIG (P<0.001) were significantly different. The
CO2CP in AKI group was lower than that in the non-AKI
group (P=0.028).
Independent risk factors for incidence
of AKI
For patients with ABG, multivariate logistic
regression analysis, and three Cox proportional hazards models were
used to determine the independent risk factors of incidence of AKI.
For the final multiple logistic analysis, 13 variables were kept in
the model for AKI, including male sex, hyponatremia, pH>7.45,
HCO3−<22 mmol/l,
HCO3−>27 mmol/l, BE<-3 mmol/l, BE>3
mmol/l and so on. To cut off the interaction of acid-base indexes,
we conducted three Cox proportional hazards models. In model 1, all
potential variables were included for final analysis, and ten
variables were identified including pH<7.35 (HR 1.810, 95% CI:
1.298–2.524, P<0.001), HCO3−<22 mmol/l
(HR 2.051, 95% CI: 1.498–2.809, P<0.001), hypomagnesemia,
hypermagnesemia and so forth. In model 2, the variable of
HCO3− was not included. Further, two
variables were kept: metabolic acidosis (HR 1.160, 95% CI:
1.001–1.344, P=0.049) and PaCO2<35 mmHg (HR 1.253,
95% CI: 1.053–1.492, P=0.011). In model 3, the variable of
PaCO2 was not included; the final analysis was similar
to model 1. The detailed results were listed in Table III.
 | Table III.Independent risk factors for acute
kidney injury including patients with arterial blood gas
analysis. |
Table III.
Independent risk factors for acute
kidney injury including patients with arterial blood gas
analysis.
|
| Multiple logistic
analysis | Cox proportional
hazards model 1 | Cox proportional
hazards model 2 | Cox proportional
hazards model 3 |
|---|
|
|
|
|
|
|
|---|
| Variable | OR (95%CI) | P-value | HR (95%CI) | P-value | HR (95%CI) | P-value | HR (95%CI) | P-value |
|---|
| Male sex | 1.427
(1.214–1.214) | <0.001 |
|
|
|
|
|
|
| Hyponatremia | 0.510
(0.271–0.271) | 0.037 |
|
|
|
|
|
|
| Hypernatremia | 0.653
(0.332–1.332) | 0.215 |
|
|
|
|
|
|
| Hypomagnesemia | 0.601
(0.467–0.467) | <0.001 | 3.399
(1.578–7.578) | 0.002 | 2.191
(1.299–3.299) | 0.003 | 2.123
(1.257–3.257) | 0.005 |
|
Hypermagnesemia | 2.040
(1.065–3.065) | 0.032 | 1.965
(1.509–2.509) | <0.001 | 1.631
(1.303–2.303) | <0.001 | 1.593
(1.272–1.272) | <0.001 |
|
Hypophosphatemia | 0.728
(0.576–0.576) | 0.008 |
|
|
|
|
|
|
|
Hyperphosphatemia | 0.911
(0.679–1.679) | 0.532 |
|
|
|
|
|
|
| Hypouricemia | 0.596
(0.445–0.445) | 0.001 | 1.270
(1.023–1.023) | 0.031 | 1.165
(0.986–1.986) | 0.073 | 1.150
(0.973–1.973) | 0.101 |
| Hyperuricemia | 0.730
(0.521–1.521) | 0.068 | 1.768
(1.272–2.272) | 0.001 | 1.397
(1.098–1.098) | 0.006 | 1.399
(1.101–1.101) | 0.006 |
| Metabolic
acidosis |
|
|
|
| 1.160
(1.001–1.001) | 0.049 |
|
|
| pH<7.35 | 1.022
(0.816–1.816) | 0.849 | 1.810
(1.298–2.298) | <0.001 | 1.386
(1.107–1.107) | 0.004 | 1.357
(1.072–1.072) | 0.011 |
| pH>7.45 | 1.853
(1.306–2.306) | 0.001 | 1.029
(0.805–1.805) | 0.820 | 1.010
(0.832–1.832) | 0.922 | 1.034
(0.856–1.856) | 0.727 |
| HCO3-
<22 mmol/l | 1.553
(1.179–2.179) | 0.002 | 2.051
(1.498–2.498) | <0.001 |
|
| 1.497
(1.194–1.194) | <0.001 |
| HCO3-
>27 mmol/l | 3.072
(2.142–4.142) | <0.001 | 0.640
(0.476–0.476) | 0.003 |
|
| 0.745
(0.587–0.587) | 0.015 |
| PaCO2
<35 mmHg |
|
|
|
| 1.253
(1.053–1.053) | 0.011 |
|
|
|
PaCO2> 45 mmHg |
|
|
|
| 1.097
(0.884–1.884) | 0.399 |
|
|
| BE <-3
mmol/l | 0.631
(0.478–0.478) | 0.001 | 0.754
(0.518–1.518) | 0.141 |
|
| 0.866
(0.661–1.661) | 0.296 |
| BE >3
mmol/l | 0.513
(0.339–0.339) | 0.002 | 1.639
(1.213–2.213) | 0.001 |
|
| 1.369
(1.084–1.084) | 0.008 |
| AST, per 40 U/l
increase | 1.140
(1.075–1.075) | <0.001 | 1.148
(1.073–1.073) | <0.001 | 1.060
(1.018–1.018) | 0.005 | 1.068
(1.026–1.026) | 0.001 |
| Albumin, per 5 g/l
decrease | 1.211
(1.110–1.110) | <0.001 | 1.184
(1.077–1.077) | 0.001 | 1.106
(1.029–1.029) | 0.006 | 1.103
(1.028–1.028) | 0.006 |
In all included patients, multivariate logistic
regression analysis and Cox proportional hazards model were used to
determine the independent risk factors of incidence of AKI during
the following hospitalization. For the final multiple logistic
analysis, 22 variables were kept in the model for AKI, including
age, male sex, CO2CP <23 mmol/l (OR 1.220, 95% CI:
1.150–1.295, P<0.001), mean blood pressure <70 mmHg,
hyponatremia, hypernatremia, and so on. After propensity matching,
14 variables were selected in Cox proportional hazards model for
the development of AKI, including CO2CP <23 mmol/l
(HR 1.099, 95% CI: 1.041–1.161, P=0.001), mean blood pressure
<70 mmHg, hypernatremia, and so on. The detailed results were
listed in Table IV.
 | Table IV.Independent risk factors for acute
kidney injury including all patients. |
Table IV.
Independent risk factors for acute
kidney injury including all patients.
|
| Multiple logistic
analysis | Cox proportional
hazards model |
|---|
|
|
|
|
|---|
| Variable | OR (95%CI) | P-value | HR (95%CI) | P-value |
|---|
| Age, per 10-year
increase | 1.077
(1.057–1.057) | <0.001 |
|
|
| Male sex | 1.141
(1.079–1.079) | <0.001 |
|
|
|
CO2CP<23 mmol/l | 1.220
(1.150–1.150) | <0.001 | 1.099
(1.041–1.041) | 0.001 |
| MBP<70 mmHg | 2.232
(1.771–2.771) | <0.001 | 1.360
(1.130–1.130) | 0.001 |
| Hyponatremia | 1.159
(1.052–1.052) | 0.003 | 1.085
(0.999–1.999) | 0.054 |
| Hypernatremia | 1.590
(1.224–2.224) | 0.001 | 1.522
(1.244–1.244) | <0.001 |
| Hypokalemia | 1.109
(1.006–1.006) | 0.037 |
|
|
| Hyperkalemia | 1.843
(1.197–2.197) | 0.006 |
|
|
| Hypochloremia | 1.375
(1.241–1.241) | <0.001 | 1.197
(1.096–1.096) | <0.001 |
| Hyperchloremia | 0.905
(0.689–1.689) | 0.473 | 0.862
(0.692–1.692) | 0.185 |
| Hypocalcemia | 1.658
(1.523–1.523) | <0.001 | 1.319
(1.224–1.224) | <0.001 |
| Hypercalcemia | 1.007
(0.803–1.803) | 0.949 | 0.992
(0.803–1.803) | 0.944 |
| Hypomagnesemia | 2.373
(1.862–3.862) | <0.001 | 1.319
(1.090–1.090) | 0.005 |
|
Hypermagnesemia | 1.340
(1.193–1.193) | <0.001 | 1.085
(0.977–1.977) | 0.126 |
|
Hypophosphatemia | 1.181
(1.085–1.085) | <0.001 | 1.113
(1.032–1.032) | 0.005 |
|
Hyperphosphatemia | 1.604
(1.472–1.472) | <0.001 | 1.347
(1.246–1.246) | <0.001 |
| Hypouricemia | 0.863
(0.797–0.797) | <0.001 | 1.021
(0.952–1.952) | 0.568 |
| Hyperuricemia | 1.765
(1.632–1.632) | <0.001 | 1.160
(1.081–1.081) | <0.001 |
| Hypoosmolality | 0.935
(0.807–1.807) | 0.368 |
|
|
|
Hyperosmolality | 3.255
(2.334–4.334) | <0.001 |
|
|
| Hemoglobin, per 10
g/l decrease | 1.073
(1.052–1.052) | <0.001 | 1.021
(1.004–1.004) | 0.018 |
|
WBC<4×109/l | 0.996
(0.922–1.922) | 0.924 | 1.094
(1.019–1.019) | 0.014 |
|
WBC>12×109/l | 1.727
(1.546–1.546) | <0.001 | 1.242
(1.130–1.130) | <0.001 |
| AST, per 40 U/l
increase | 1.088
(1.071–1.071) | <0.001 | 1.033
(1.022–1.022) | <0.001 |
| TBIL, per 20 µmol/l
increase | 1.023
(1.006–1.006) | 0.007 |
|
|
| Albumin, per 5 g/l
decrease | 1.220
(1.179–1.179) | <0.001 | 1.120
(1.087–1.087) | <0.001 |
Independent risk factors for hospital
mortality
For patients with ABG, multivariate logistic
regression analysis, and three Cox proportional hazards models were
used to determine the independent risk factors for hospital
mortality. For the final multiple logistic analysis, four variables
were kept in the model for hospital mortality, including age,
pH>7.45, AST, and albumin. Three Cox proportional hazards models
were also conducted as above; six variables were kept in more than
one model, including age, pH<7.35, PaCO2 <35 mmHg,
hypo-osmolality, AST, and decreased albumin. The detailed results
were listed in Table V.
 | Table V.Independent risk factors for hospital
mortality including patients with arterial blood gas analysis. |
Table V.
Independent risk factors for hospital
mortality including patients with arterial blood gas analysis.
|
| Multiple logistic
analysis | Cox proportional
hazards model 1 | Cox proportional
hazards model 2 | Cox proportional
hazards model 3 |
|---|
|
|
|
|
|
|
|---|
| Variable | OR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value |
|---|
| Age, per 10-year
increase | 1.500
(1.233–1.233) | <0.001 | 1.360
(1.103–1.103) | 0.004 | 1.333
(1.092–1.092) | 0.005 | 1.346
(1.103–1.103) | 0.003 |
| pH<7.35 | 0.674
(0.370–1.370) | 0.198 | 5.064
(2.438–10.438) | <0.001 | 3.915
(1.966–7.966) | <0.001 | 4.533
(2.328–8.328) | <0.001 |
| pH>7.45 | 2.827
(1.316–6.316) | 0.008 | 1.793
(0.928–3.928) | 0.082 | 1.879
(1.005–3.005) | 0.048 | 2.295
(1.258–4.258) | 0.007 |
|
PaCO2<35 mmHg | 0.551
(0.246–1.246) | 0.148 | 2.636
(1.406–4.406) | 0.003 | 2.491
(1.360–4.360) | 0.003 |
|
|
|
PaCO2>45 mmHg | 1.307
(0.556–3.556) | 0.539 | 2.103
(0.892–4.892) | 0.089 | 1.951
(0.866–4.866) | 0.107 |
|
|
| Hypoosmolality | 1.192
(1.032–1.032) | 0.072 | 2.233
(1.109–4.109) | 0.024 | 1.870
(0.988–3.988) | 0.054 | 2.052
(1.091–3.091) | 0.026 |
|
Hyperosmolality | 0.480
(0.075–3.075) | 0.438 | 4.032
(0.669–24.669) | 0.128 | 3.610
(0.818–15.818) | 0.090 | 3.921
(0.876–17.876) | 0.074 |
| AST, per 40 U/l
increase | 1.462
(1.245–1.245) | <0.001 | 1.220
(1.095–1.095) | <0.001 | 1.173
(1.065–1.065) | 0.001 | 1.217
(1.106–1.106) | <0.001 |
| Albumin, per 5 g/l
decrease | 1.688
(1.348–2.348) | <0.001 | 1.647
(1.296–2.296) | <0.001 | 1.507
(1.217–1.217) | <0.001 | 1.425
(1.120–1.120) | 0.004 |
In all included patients, multivariate logistic
regression analysis and Cox proportional hazards model were used to
identify the independent risk factors for hospital mortality. For
the final multiple logistic analysis, 14 variables were kept in the
model for hospital mortality, including age, male sex,
CO2CP <23 mmol/l (OR 1.344, 95% CI: 1.107–1.632,
P=0.003), hyponatremia, hypochloremia, and so on. After propensity
matching, 11 variables were selected in Cox proportional hazards
model for hospital mortality. CO2CP<23 mmol/l was
also an independent risk factor for hospital mortality (HR 1.294,
95% CI: 1.026–1.632, P=0.030). The detailed results were listed in
Table VI.
 | Table VI.Independent risk factors for hospital
mortality including all patients. |
Table VI.
Independent risk factors for hospital
mortality including all patients.
|
| Multiple logistic
analysis | Cox proportional
hazards model |
|---|
|
|
|
|
|---|
| Variable | OR (95% CI) | P-value | HR (95% CI) | P-value |
|---|
| Age, per 10-year
increase | 1.611
(1.504–1.504) | <0.001 |
|
|
| Male sex | 1.364
(1.124–1.124) | 0.002 |
|
|
|
CO2CP<23 mmol/l | 1.344
(1.107–1.107) | 0.003 | 1.294
(1.026–1.026) | 0.030 |
| Hyponatremia | 1.563
(1.190–2.190) | 0.001 | 1.592
(1.147–2.147) | 0.005 |
| Hypernatremia | 1.916
(0.935–3.935) | 0.076 | 1.647
(0.749–3.749) | 0.214 |
| Hypokalemia |
|
| 1.453
(1.081–1.081) | 0.013 |
| Hyperkalemia |
|
| 1.487
(0.685–3.685) | 0.315 |
| Hypochloremia | 1.968
(1.484–2.484) | <0.001 | 1.877
(1.349–2.349) | <0.001 |
| Hyperchloremia | 0.728
(0.378–1.378) | 0.342 | 0.676
(0.323–1.323) | 0.299 |
| Hypomagnesemia | 0.295
(0.090–0.090) | 0.044 | 0.350
(0.111–1.111) | 0.072 |
|
Hypermagnesemia | 1.565
(1.104–2.104) | 0.012 | 1.594
(1.112–2.112) | 0.011 |
| Hypouricemia | 1.283
(1.025–1.025) | 0.030 | 1.278
(0.980–1.980) | 0.070 |
| Hyperuricemia | 1.742
(1.324–2.324) | <0.001 | 1.520
(1.127–2.127) | 0.006 |
| Hypoosmolality | 0.936
(0.684–1.684) | 0.679 | 1.086
(0.761–1.761) | 0.650 |
|
Hyperosmolality | 5.029
(2.549–9.549) | <0.001 | 3.588
(1.767–7.767) | <0.001 |
| Hemoglobin, per 10
g/l decrease | 1.204
(1.145–1.145) | <0.001 | 1.128
(1.067–1.067) | <0.001 |
|
WBC<4×109/l | 1.064
(0.817–1.817) | 0.645 | 0.889
(0.635–1.635) | 0.546 |
|
WBC>12×109/l | 2.917
(2.274–3.274) | <0.001 | 2.096
(1.580–2.580) | <0.001 |
| AST, per 40 U/l
increase | 1.126
(1.094–1.094) | <0.001 | 1.068
(1.039–1.039) | <0.001 |
| TBIL, per 20 µmol/l
increase | 1.032
(1.001–1.001) | 0.043 |
|
|
| Albumin, per 5 g/l
decrease | 1.492
(1.355–1.355) | <0.001 | 1.294
(1.026–1.026) | <0.001 |
ROC curves of CO2CP
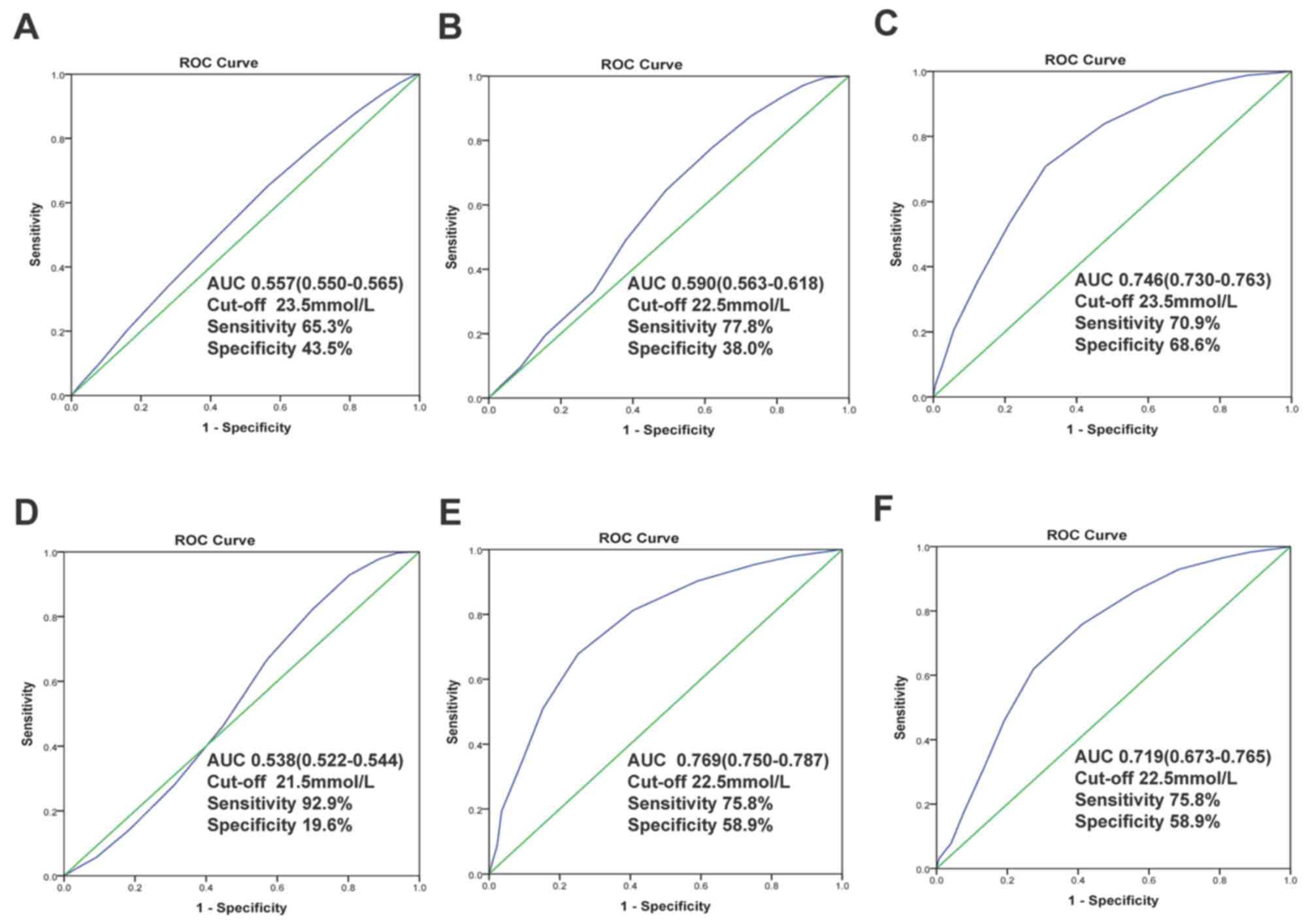
In all included patients, the area under the ROC of
CO2CP was 0.557 (95% CI: 0.550–0.565, P<0.001) for
predicting of not developing AKI and 0.590 (95% CI: 0.563–0.618,
P<0.001) for predicting of no hospital death. And the optimal
cut-off values of CO2CP were 23.5 (sensitivity 65.3%,
specificity 43.5%) and 22.5 mmol/l (sensitivity 77.8%, specificity
38.0%), respectively (Fig. 2A and
B). In patients with ABG, the area under the ROC of
CO2CP was 0.746 (95% CI: 0.730–0.763, P<0.001) for
diagnosis of no metabolic acidosis and the optimal cut-off values
of CO2CP were 23.5 (sensitivity 70.9%, specificity
68.6%), indicating reasonable biomarker performance (Fig. 2C). We also conduct ROC curves of
CO2CP for excluding the diagnosis of any acid-base
disturbances (Fig. 2D), simple, dual
and triple acid-base disturbances. There were reasonable biomarker
performances to exclude diagnosis of dual (AUC 0.769, 95%: CI
0.750–0.787, P<0.001, Fig. 2E)
and triple (AUC 0.719, 95%: CI 0.673–0.765, P<0.001, Fig. 2F) acid-base disturbances with 22.5
mmol/l as the optimal cut-off value.
Subgroup analysis of CO2CP
as a contributor of AKI and hospital mortality
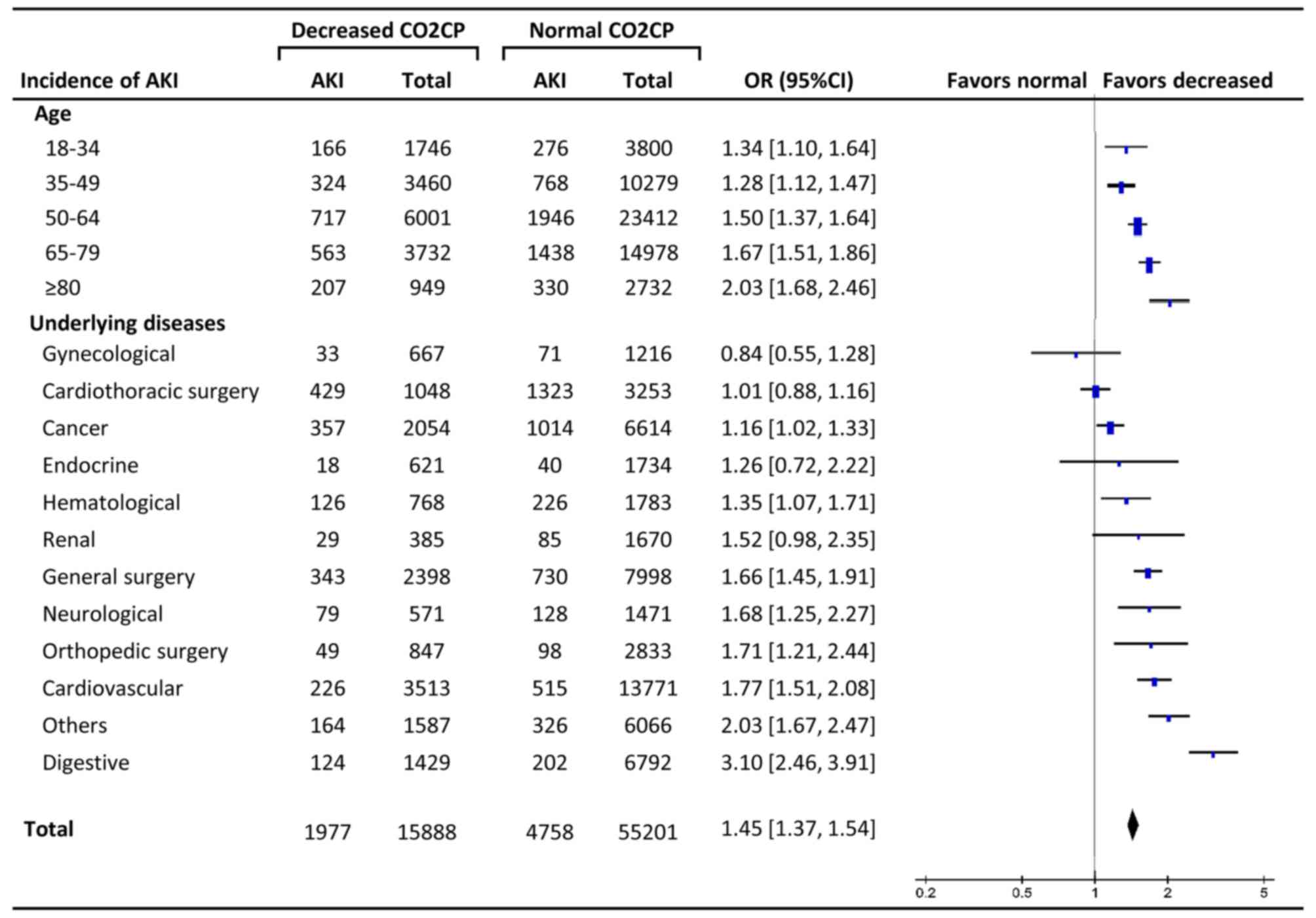
The total incidence of AKI in decreased
CO2CP group was significantly higher than normal
CO2CP group (12.4% and 8.6, respectively, OR 1.45, 95%
CI: 1.37–1.54, P<0.001). Subgroup analysis showed that the ORs
increased along with older age with significant differences at
every age stage (18–34 years, P=0.004; other stages, P<0.001).
The effect sizes of decreased CO2CP on AKI varied
according to different diseases, and there were significant
differences in digestive (OR 3.10, P<0.001), cardiovascular
diseases (OR 1.77, P<0.001), orthopedic surgery (OR 1.71,
P=0.002), neurological diseases (OR 1.68, P=0.001), general surgery
(OR 1.66, P<0.001), hematological diseases (OR 1.35, P=0.012),
cancer (OR 1.16, P=0.026) and others (OR 2.03, P<0.001)
(Fig. 3).
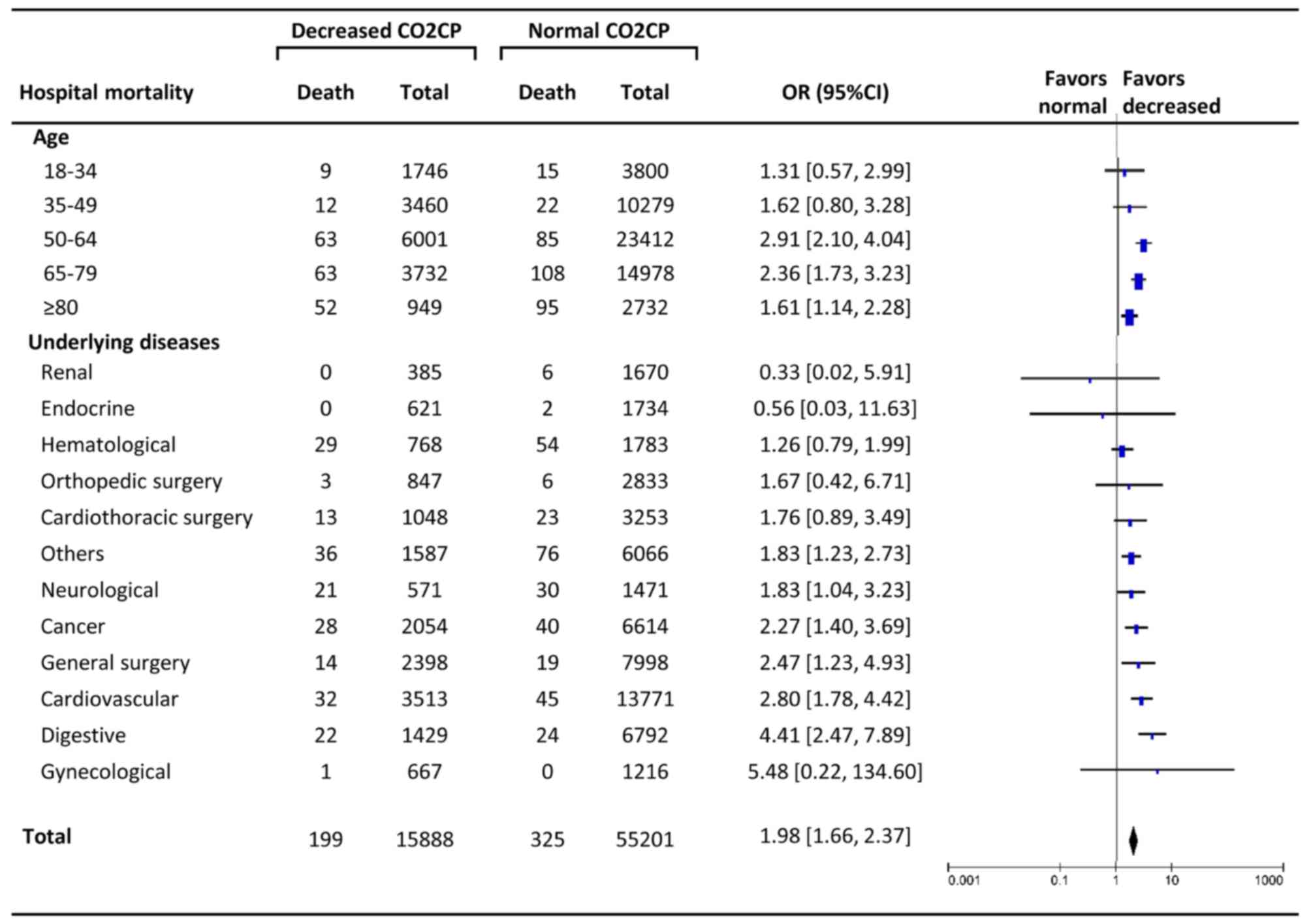
The total hospital mortality in decreased
CO2CP group was 1.3%, significantly higher than normal
CO2CP group (0.6%) (OR 1.98, 95% CI: 1.66–2.37,
P<0.001). The increasing trend of ORs along with older age was
not present, and there were significant differences only at the age
stages of 50–64 years (OR 2.91, P<0.001), 65–79 years (OR 2.36,
P<0.001), and >80 years (OR 1.61, P=0.007). The effect sizes
of decreased CO2CP on hospital mortality were
significantly different in digestive (OR 4.41, P<0.001),
cardiovascular diseases (OR 2.80, P<0.001), general surgery (OR
2.47, P=0.008), cancer (2.27 1.61, P=0.001), neurological diseases
(OR 1.83, P=0.033), and others (OR 1.83, P=0.003) (Fig. 4).
Discussion
The present study focuses on the variables in the
electrolyte and acid-base balance among non-respiratory patients
associated with the occurrence of AKI and hospital mortality using
a propensity score matching method. Primary analysis in patients
with ABG demonstrated that several variables which could result in
decreased CO2CP, such as acidosis (pH<7.35),
metabolic acidosis, decreased HCO3− and
hypocapnia were associated with the development of AKI, while
acidosis and hypocapnia were independent predictors of hospital
mortality. Further analysis found decreased CO2CP was an
independent risk factor for AKI and hospital mortality. AUC-ROC
indicated that CO2CP was a reasonable biomarker to
exclude metabolic acidosis, dual and triple acid-base disturbances
with 22.5 or 23.5 mmol/l as optimal cut-off values. Furthermore,
the effect sizes of decreased CO2CP on AKI and hospital
mortality varied according to age and different underlying
diseases.
Whether acid-base disturbances are contributors to
acute kidney injury or rather are simple epiphenomena has rarely
been discussed in previous studies. The role of serum bicarbonate
level as a risk factor for renal outcomes (end-stage renal disease
or 50% reduction in evaluated glomerular filtration rate) has been
evaluated in patients with CKD. Aſter adjustment for covariates,
the risk of developing a renal endpoint is 3% lower per 1 mM
increase in serum bicarbonate level (HR 0.97, 95% CI: 0.94–0.99)
(14). However, it is not known
whether metabolic acidosis affects the development of AKI in a
clinical setting. Our research found that acidosis, especially
metabolic acidosis, hypocapnia, and decreased CO2CP were
contributors to the incidence of AKI. Besides, the previous study
(1) showed that patients with
acidosis are 4 to 5 times as likely to die as patients who do not,
and the mortality among patients with metabolic acidosis is highest
for patients with lactic acidosis (high AG) and SIG acidosis. We
found that acidosis, hypocapnia, and decreased CO2CP
were predictors of hospital mortality, and significantly higher SIG
was observed in AKI group than the non-AKI group, indicating that
SIG should also be carefully monitored, especially in critically
ill patients. Although the roles of metabolic acidosis in the
development of AKI and death were confirmed, the benefits and
administration timing of sodium bicarbonate for prevention and
treatment of AKI are still not clear now (15).
In this study, we restricted our analysis to
patients without respiratory diseases and patients with increased
CO2CP at admission were also excluded, for several
reasons. As discussed above, CO2CP does not reflect the
actual state of the acid-base balance when respiratory acid-base
balances exist. Two major acid-base disturbances, respiratory
acidosis, and metabolic alkalosis, both of which can result in
increased CO2CP, are not uncommon in respiratory
patients. If respiratory diseases, such as chronic obstructive
pulmonary diseases, are excluded, the impact of respiratory
acid-base balances to CO2CP can be minimized. On the
other hand, reduced CO2CP suggests metabolic acidosis
(1) or respiratory alkalosis
(16), both of which are indicators
of poor outcomes. Although ABG analysis has become an essential
test to diagnose acid-base disturbances, only a small percentage of
patients received this test for its invasive procedure and
complications. In this respect, CO2CP is easier for
patients to obtain from venous blood than ABG analysis from
arterial blood. Furthermore, if integrated with clinical and
electrolytes for full consideration, more exact information about
acid-base disturbances can be obtained from CO2CP.
Most often, decreased CO2CP signifies the
presence of metabolic acidosis, but it also could reflect a decline
in the bicarbonate concentration as compensation for respiratory
alkalosis. Respiratory alkalosis is a disturbance in acid and base
balance due to alveolar hyperventilation. Respiratory alkalosis is
the most common acid-base disturbance observed in patients who are
critically ill. When respiratory alkalosis is present, the cause
may be a minor non-life-threatening disorder. However, more serious
disease processes may exist, especially in critically ill patients.
In our study, hypocapnia at admission in non-respiratory patients
was associated with poor outcomes, including the development of AKI
and hospital mortality. Furthermore, in non-respiratory patients,
AUC-ROC stated that CO2CP was a reasonable biomarker to
exclude metabolic acidosis, dual and triple acid-base disturbances
with 22.5 or 23.5 mmol/l as optimal cut-off values.
The relationship of electrolyte disturbances and
poor outcomes is complex. They may often be a para-phenomenon, as
an indicator of the severity of the underlying diseases. However,
according to our multiple logistic regression and
propensity-matched analysis, some disorders were independent
contributors to hospital mortality, such as hyponatremia,
hypochloremia, hyperkalemia, hypermagnesemia, and hyperosmolality.
We also found that several types of electrolyte disturbances were
associated with AKI (hyponatremia, hypernatremia, hypochloremia,
hypocalcemia, hypomagnesemia, hypophosphatemia and
hyperphosphatemia).
However, some limitations must be considered.
Firstly, although we attempted to control for confounders by using
multiple logistic regression analysis and Cox proportional hazards
model after propensity score matching, this retrospective
observational design does not establish causal relationships of
acid-base disturbances with the development of AKI and hospital
mortality. Secondly, only non-respiratory patients were considered
in this study, which may lead to potential bias and we could not
give a reasonable explanation for different effect sizes of
decreased CO2CP on various underlying diseases in our
study. Thirdly, although we tried to collect the data about the
intervention of acid-base disturbances, for example, the
administration of sodium bicarbonate and fluid management, it was
too hard to obtain these data for a retrospective study. Further
well-designed and prospective research is needed.
Metabolic acidosis is an independent risk factor for
the development of AKI and hospital mortality. In non-respiratory
patients without ABG, decreased CO2CP is also an
independent contributor to AKI and mortality, and can be used as an
indicator of metabolic acidosis. Further ABG test is needed, and
close attention should be paid to high-risk patients with decreased
CO2CP.
Acknowledgements
This study was supported by the Shanghai Key
Discipline Construction Project on the Fourth Round of Three-year
Action Plan for Public Health Systems: Subject of Dialysis and Body
Fluids (15GWZK0502), Grant of Chinese Ministry of Health 2013 and
14DZ2260200 from Shanghai Science and Technology Committee
Foundation (Shanghai Key Laboratory of Kidney Diseases and Blood
Purification).
References
|
1
|
Gunnerson KJ, Saul M, He S and Kellum JA:
Lactate versus non-lactate metabolic acidosis: A retrospective
outcome evaluation of critically ill patients. Crit Care.
10:R222006. View
Article : Google Scholar : PubMed/NCBI
|
|
2
|
Silva J, únior GB, Edf F Daher, Mota RM
and Menezes FA: Risk factors for death among critically ill
patients with acute renal failure. Sao Paulo Med J. 124:257–263.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bockenkamp B and Vyas H: Understanding and
managing acute fluid and electrolyte disturbances. Current
Paediatrics. 13:520–528. 2003. View Article : Google Scholar
|
|
4
|
Chen W and Abramowitz MK: Metabolic
acidosis and the progression of chronic kidney disease. BMC
Nephrol. 15:552014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chowdhury AH, Cox EF, Francis ST and Lobo
DN: A randomized, controlled, double-blind crossover study on the
effects of 2-L infusions of 0.9% saline and plasma-lyte®
148 on renal blood flow velocity and renal cortical tissue
perfusion in healthy volunteers. Ann Surg. 256:18–24. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Peppicelli S, Bianchini F, Contena C,
Tombaccini D and Calorini L: Acidic pH via NF-κB favours VEGF-C
expression in human melanoma cells. Clin Exp Metastasis.
30:957–967. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Magalhães PA, de Brito TS, Freire RS, da
Silva MT, dos Santos AA, Vale ML, de Menezes DB, Martins AM and
Libório AB: Metabolic acidosis aggravates experimental acute kidney
injury. Life Sci. 146:58–65. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Khwaja A: KDIGO clinical practice
guidelines for acute kidney injury. Nephron Clin Pract.
120:c179–c184. 2012.PubMed/NCBI
|
|
9
|
Engle JE: Clinical physiology of acid-base
and electrolyte disorders. JAMA. 263:2375–2376. 1990. View Article : Google Scholar
|
|
10
|
Fencl V, Jabor A, Kazda A and Figge J:
Diagnosis of metabolic acid-base disturbances in critically ill
patients. Am J Respir Crit Care Med. 162:2246–2251. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Fulop M: Flow diagrams for the diagnosis
of acid-base disorders. J Emerg Med. 16:97–109. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Swets JA: Measuring the accuracy of
diagnostic systems. Science. 240:1285–1293. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Youden WJ: Index for rating diagnostic
tests. Cancer. 3:32–35. 1950. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dobre M, Yang W, Chen J, Drawz P, Hamm LL,
Horwitz E, Hostetter T, Jaar B, Lora CM, Nessel L, et al:
Association of serum bicarbonate with risk of renal and
cardiovascular outcomes in CKD: A report from the chronic renal
insufficiency cohort (CRIC) study. Am J Kidney Dis. 62:670–678.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hewitt J, Uniacke M, Hansi NK,
Venkat-Raman G and McCarthy K: Sodium bicarbonate supplements for
treating acute kidney injury. Cochrane Database Syst Rev. CD009204.
2012. View Article : Google Scholar
|
|
16
|
Shirakabe A, Hata N, Kobayashi N, Shinada
T, Tomita K, Tsurumi M, Matsushita M, Okazaki H, Yamamoto Y,
Yokoyama S, et al: Clinical significance of acid-base balance in an
emergency setting in patients with acute heart failure. J Cardiol.
60:288–294. 2012. View Article : Google Scholar : PubMed/NCBI
|