Introduction
With the development of science and technology,
people's living standards are improving. Considerable progress has
also been made in transportation, causing an increase in the number
of traffic accidents. Most of the traffic injuries are caused by
open injury and usually accompanied by contamination (1). Due to these contaminations, one-time
operation usually can lead to postoperative infection, which may
affect wound-healing, limb function, and even cause bloodstream
infection induced shock (2–5). Therefore, the second-stage surgery has
become increasingly widely used, thus, infection should be
controlled first and then the fixation would be performed with the
secondary surgery (6–9). However, there are some discussions
regarding the timing of the secondary surgery. If the secondary
surgery is performed at an early stage after the first surgery, the
surgical outcomes may be affected by the infection which is not
fully controlled (10–12). However, if the secondary surgery is
performed at a late stage after the first surgery, the financial
burden can increase significantly. Also, the healing time can be
extended, and the psychological burden on patients and their
families can also increase. This may negatively impact the recovery
process (13–16). Therefore, it is significantly useful
if we can find a way to accurately predict the timing of the
secondary surgery. However, due to the application of antibiotics
after the first surgery, the differences in clinical indicators
such as erythrocyte sedimentation rate (ESR), white blood cell and
neutrophil count and other indexes between infected and
non-infected patients are not noticeable. Prior studies have shown
that the C-reactive protein levels are significantly different
between these two groups of patients (17). So, this study aimed to find a
surgical index that can accurately determine the timing of
secondary surgery in order to promote early rehabilitation.
Materials and methods
Clinical data and general
information
A total of 100 patients with open fractures of the
tibia and fibula diagnosed in Zhengzhou No. 7 People's Hospital
from 2007 to 2016 were enrolled in this study. They were all
subjected to staging surgery treatment. Patients were divided into
the infection group (n=52) and the non-infection group (n=48)
according to whether or not infection occurred after operation.
There was no significant difference between those two groups except
a significant difference in surgical timing (Table I). This study was approved by the
Ethics Committee of Zhengzhou Orthopaedics Hospital. Signed written
informed consents were obtained from all participants before the
study.
 | Table I.Comparison of general information
between the infection and non-infection groups. |
Table I.
Comparison of general information
between the infection and non-infection groups.
| Items | Non-infection
group | Infection group | t-value | P-value |
|---|
| Surgical timing
(days) | 9.23±5.74 | 4.30±1.03 | 6.091 | <0.001 |
| C- reactive protein
level before surgery (mg/l) | 20.53±17.60 | 21.64±15.37 | 0.337 | 0.737 |
| White cell count
(*109/l) | 8.73±2.56 | 9.24±1.95 | 1.126 | 0.263 |
| Neutrophil count
(*109/l) | 5.43±1.98 | 6.02±1.87 | 1.532 | 0.129 |
| Proportion of
neutrophil (%) | 67.01±11.76 | 66.22±1.93 | 0.478 | 0.634 |
| Body temperature
(°C) | 36.38±0.33 | 36.40±0.28 | 0.328 | 0.743 |
| ESR (mm/l) | 50.63±25.68 | 54.57±33.79 | 0.652 | 0.516 |
| Age (years) | 45.66±14.32 | 43.54±13.96 | 0.749 | 0.455 |
Methods
Clinical indexes of the patents before and after
surgery, including Gustilo-Anderson classification, white cell and
neutrophil counts, ESR, body temperature, and timing of surgery
were evaluated and recorded. Patients pathological data were also
collected.
Information on Gustilo-Anderson, timing of surgery,
C-reactive protein, white cell and neutrophil counts, proportion of
neutrophil, body temperature, ESR, sex and age were all subjected
to univariate analysis. C-reactive protein levels and surgical
timings were selected from univariate logistic correlation analysis
for multivariate logistic regression analysis.
Observation indexes
Fasting venous blood (3–5 ml) was collected from the
patients (fasting for >8 h) in both groups after 7:00 in the
morning before and after surgery. Serum was separated and
C-reactive protein levels were measured using enzyme-linked
immunosorbent assay (ELISA). ELISA kits were provided by Beckman
Coulter, Inc. (Brea, CA, USA). White cell and neutrophil counts
were also conducted. ESR and body temperature were determined and
the timing of the surgery was recorded.
Statistical analysis
SPSS 19.0 software (SPSS Inc., Chicago, IL, USA) was
used for statistical analysis. The data are expressed as mean ±
standard deviation and tested by t-test. The categorical variables
were assigned with numbers to facilitate logistic analysis.
Univariate logistic regression analysis with odds ratio (OR) and
95% confidence interval was used to select correlated variables for
multivariate correlation analysis. The correlation was analyzed by
Pearson correlation analysis. The effects of C-reactive protein
levels on postoperative infection were analyzed by ROC curve.
P<0.05 was considered to be statistically significant.
Results
Value assignment for the related
categorical variables
Value was assigned to non-numerical variables for
logistic regression analysis (Table
II).
 | Table II.Value assignment for the related
categorical variables. |
Table II.
Value assignment for the related
categorical variables.
| Items | Categories | Assigned value |
|---|
| Sex | Male | 1 |
|
| Female | 0 |
| Infection | Yes | 1 |
|
| No | 0 |
| Gustilo-Anderson | I | 1 |
| classification | II | 2 |
|
| IIIA | 3 |
|
| IIIB | 4 |
|
| IIIC | 5 |
Univariate logistic regression
analysis on indexes before surgery
The relevant factors were first subjected to
univariate analysis, if P-value was <0.05, then the relevant
factor was related to postoperative infection. Univariate analysis
showed that timing of surgery and C-reactive protein were
correlated with postoperative infection (P<0.05). There was a
negative correlation between timing of surgery and postoperative
infection. A positive correlation was established between
C-reactive protein and postoperative infection (Table III).
 | Table III.Univariate logistic regression
analysis on indexes before surgery. |
Table III.
Univariate logistic regression
analysis on indexes before surgery.
| Items | P-value | OR-value | OR and 95% confidence
interval |
|---|
| Gustilo-Anderson
classification (X1) | 0.076 | 1.97 | 0.084–4.125 |
| Surgical timing
(X2) | 0.025 | 0.196 | 0.034–0.067 |
| C-reactive protein
(X3) | 0.019 | 1.055 | 1.002–1.072 |
| White cell count
(X4) | 0.215 | 1.584 | 0.851–1.863 |
| Neutrophil count
(X5) | 0.291 | 1.197 | 0.734–1.652 |
| Proportion of
neutrophil (X6) | 0.521 | 0.857 | 0.749–1.023 |
| Body temperature
(X7) | 0.452 | 0.371 | 0.014–5.774 |
| ESR (X8L) | 0.521 | 1.052 | 0.845–1.013 |
| Sex (X9) | 0.256 | 0.351 | 0.027–2.954 |
| Age (X10) | 0.295 | 1.026 | 0.857–1.032 |
Multivariate logistic regression
analysis on C-reactive protein and timing of surgery
Timing of surgery and C-reactive protein levels were
subjected to multivariate logistic regression analysis. Results
showed that OR of timing of surgery was 0.648. There was a negative
correlation between postoperative infection and timing of surgery.
The OR-value of C-reactive protein was 1.052. We detected a
positive correlation between postoperative infection and C-reactive
protein (Table IV).
 | Table IV.Multivariate logistic regression
analysis on C-reactive protein and timing of surgery. |
Table IV.
Multivariate logistic regression
analysis on C-reactive protein and timing of surgery.
| Items | P-value | OR-value | OR and 95% confidence
interval |
|---|
| Items | P-value | OR-value | confidence
interval |
| Timing of surgery
(X2) | 0.023 | 0.684 | 0.575–0.958 |
| C-reactive protein
(X3) | 0.016 | 1.052 | 1.003–1.065 |
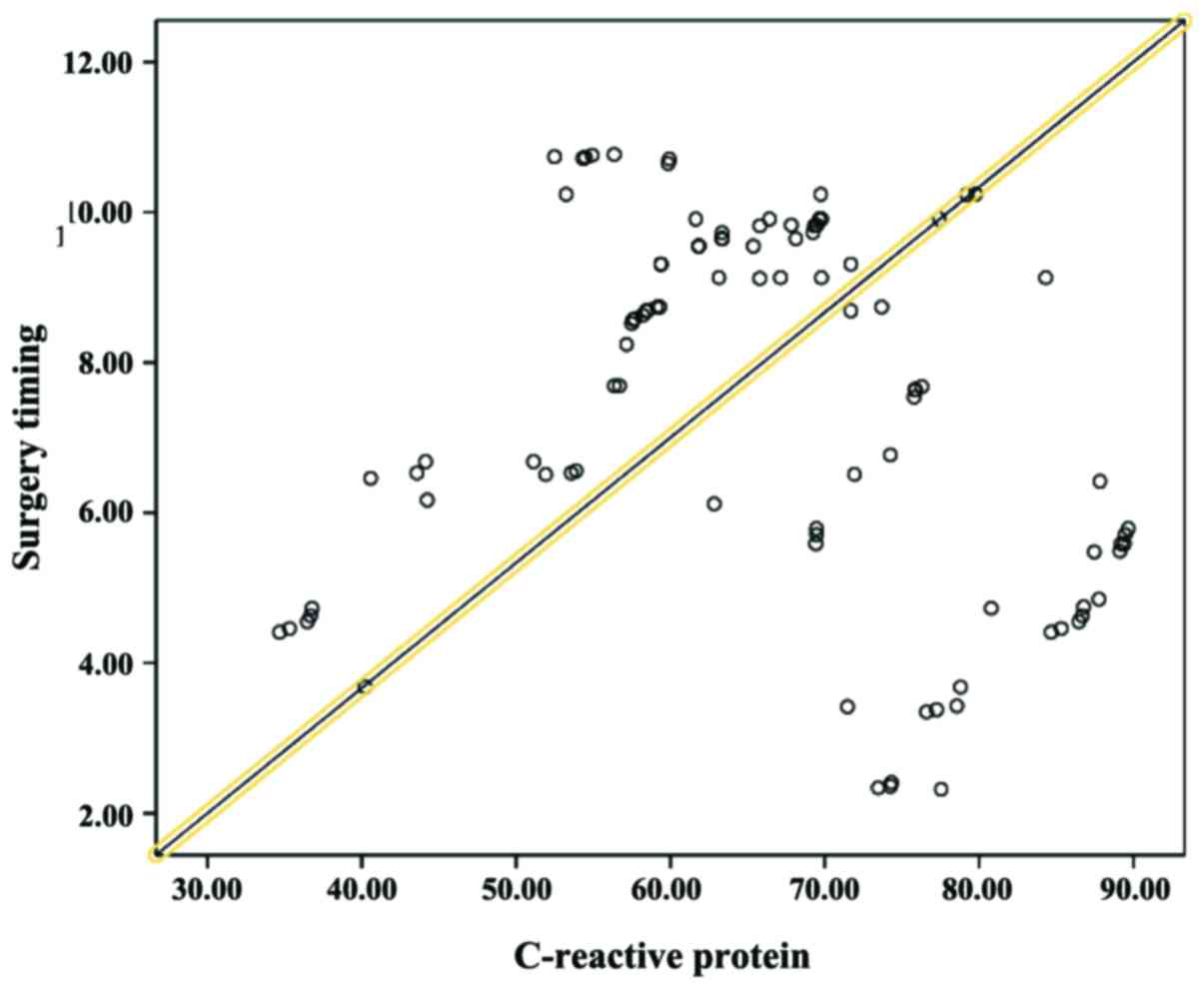
Pearson correlation analysis of
C-reactive protein and timing of surgery
In order to determine the possible correlation
between C-reactive protein and timing of surgery, Pearson
correlation analysis was applied. The P-value was >0.05 and
Pearson correlation coefficient value was 0.039, therefore no
correlation between the two factors was established (Table V, Fig.
1).
 | Table V.Pearson correlation analysis of
C-reactive protein and timing of surgery. |
Table V.
Pearson correlation analysis of
C-reactive protein and timing of surgery.
| Item | Pearson correlation
value | P-value |
|---|
| C-reactive protein
and timing of surgery | 0.039 | 0.841 |
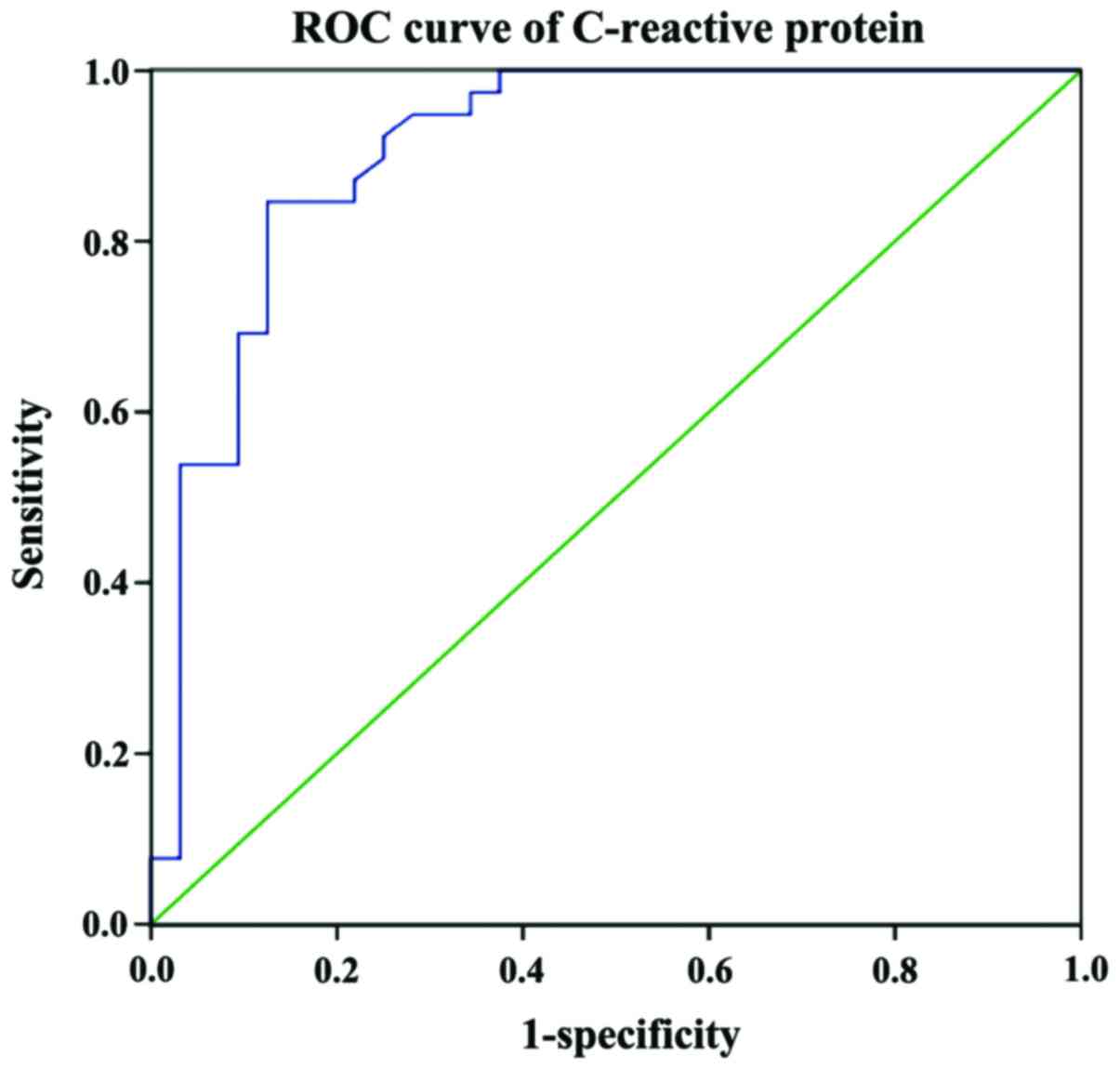
Analysis of cut-off point of surgical
timing and postoperative infection
Using 7 days as the cut-off point of surgical
timing, the ROC curve analysis showed that the sensitivity and
specificity were 100 and 72.3%, respectively. The false negative
and false positive rates were 0 and 27.7%, respectively. The Youden
index value was 72.3%. The positive and negative predictive values
were 42.5 and 100%, respectively (Table
VI, Fig. 2).
 | Table VI.Analysis of cut-off point of surgical
timing and postoperative infection. |
Table VI.
Analysis of cut-off point of surgical
timing and postoperative infection.
|
| Infection |
|
|---|
|
|
|
|
|---|
| Timing of
surgery | Positive (cases) | Negative (cases) | Total |
|---|
| Positive (<7
days) | 17 | 23 | 40 |
| Negative (>7
days) | 0 | 60 | 60 |
| Total | 17 | 83 | 100 |
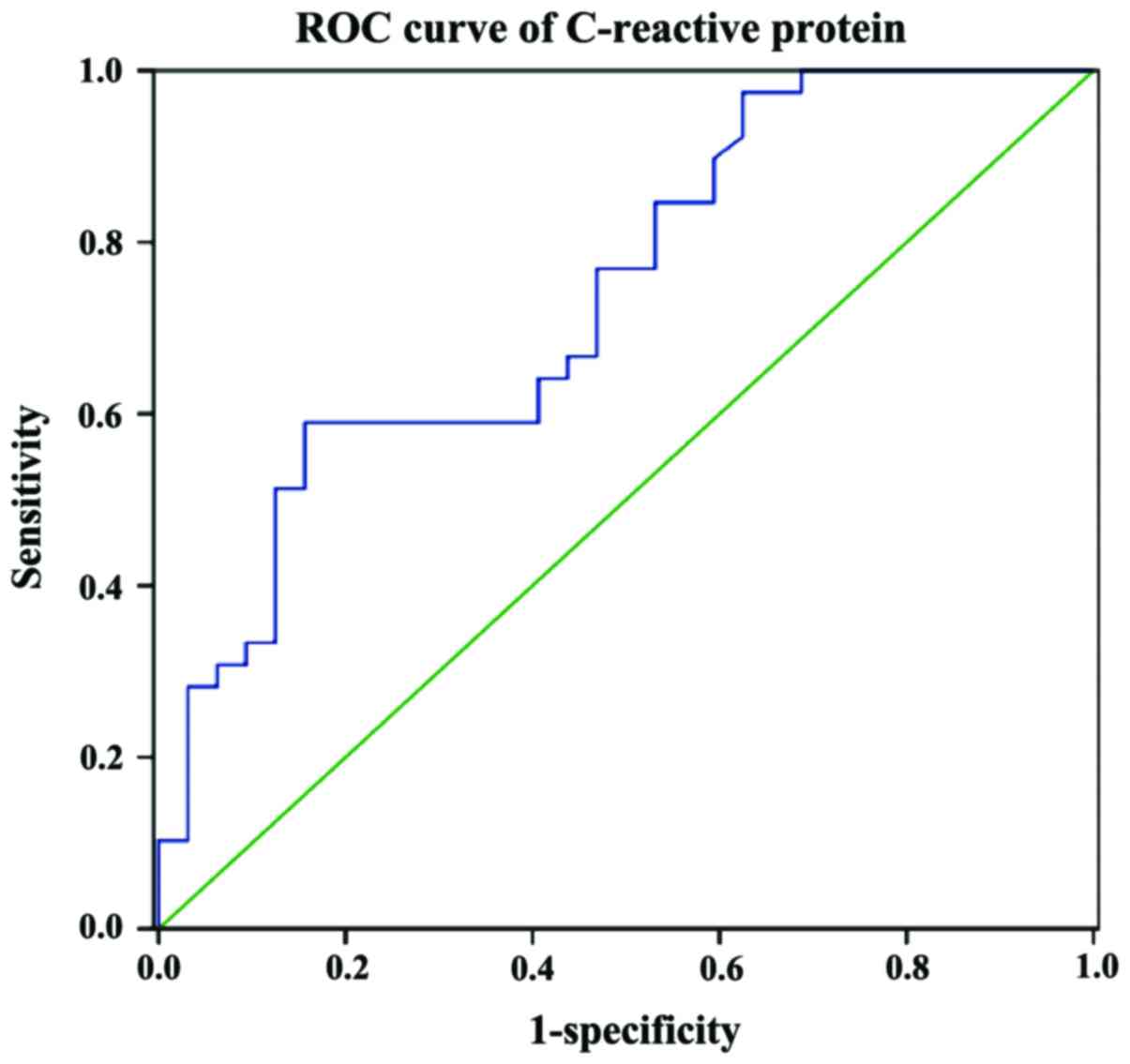
Analysis on cut-off point of
C-reactive protein and postoperative infection
ROC curve analysis was applied. With 54.55 mg/l as
the cut-off point of C-reactive protein, the sensitivity and
specificity of prediction were 88.2 and 94.1%, respectively. The
false negative and false positive rates were 11.8 and 5.9%,
respectively. The Youden index was 82.3%. The positive predictive
and negative predictive values were 75 and 96.7%, respectively
(Table VII, Fig. 3).
 | Table VII.Analysis on cut-off point of
C-reactive protein and postoperative infection. |
Table VII.
Analysis on cut-off point of
C-reactive protein and postoperative infection.
|
| Infection |
|
|---|
|
|
|
|
|---|
| C-reactive
protein | Positive (cases) | Negative (cases) | Total |
|---|
| Positive (>54.55
mg/l) | 15 | 5 | 20 |
| Negative (<54.55
mg/l) | 2 | 78 | 80 |
| Total | 17 | 83 | 100 |
Accuracy analysis of C-reactive
protein and the timing of surgery joint prediction on postoperative
infection
ROC curve analysis was used. For the surgery time of
7 days and C-reactive protein level of 54.55 mg/l, the predictive
sensitivity and specificity were 88.2 and 97.6%, respectively. The
false negative and false positive rates were 11.8 and 2.4%,
respectively. The Youden index value was 85.8%; positive predictive
value and negative predictive values were 88.2 and 97.6%,
respectively (Table VIII).
 | Table VIII.Accuracy analysis C-reactive protein
and the timing of surgery joint prediction on postoperative
infection. |
Table VIII.
Accuracy analysis C-reactive protein
and the timing of surgery joint prediction on postoperative
infection.
|
| Infection |
|
|---|
|
|
|
|
|---|
| C-reactive protein
and the timing of surgery | Positive
(cases) | Negative
(cases) | Total |
|---|
| Positive | 15 | 2 | 17 |
| Negative | 2 | 81 | 83 |
| Total | 17 | 83 | 100 |
Discussion
With the improvement of living standards, we have
witnessed an increase in the number of multi-level construction and
a significant improvement in the modes of transportation.
Correspondingly, the high-altitude falling injuries and injuries
caused by car accidents are on the rise. Most of those injuries are
open injuries and are usually accompanied by infection. In these
cases, a two-stage surgery is considered to be beneficial for the
victims of these types of accidents. There is no controversy over
the first surgery, which contains debridement and external fixation
and the surgical approach is fairly matured. However, controversy
still exists over the timing of secondary surgery. Ruedi et
al recommended that the secondary surgery be performed 3 weeks
after the first surgery (18).
However, Nanchahal et al considered that the secondary
surgery should be carried out 10 days after the first surgery
(19). The reason for this ambiguity
in the timing of the secondary surgery is largely due to the
inability of determination of the risk of infection. Currently, the
indicators used to determine infection mainly include body
temperature, white cell and neutrophil counts and ESR. However, due
to the use of antibiotics, most studies have shown no significant
difference among these clinical indicators in infected and
non-infected patients. Nevertheless, some studies have shown a
significant difference in C-reactive protein level between infected
patients and non-infected patients (17,20).
Therefore, in this study, we investigated the relationship between
C-reactive protein and postoperative infection to predict the
timing of secondary surgery for open fractures.
We discovered that the timing of surgery and
C-reactive protein were correlated with postoperative infection
(P<0.05). A negative correlation between the timing of surgery
and postoperative infection as well as a positive correlation
between C-reactive protein and postoperative infection were
established. With 7 days as the cut-off point of surgical timing,
the sensitivity and specificity of prediction were 100 and 72.3%,
respectively. False positive and false negative rates were 0 and
27.7%, respectively. The Youden index was 72.3% and the positive
predictive and negative predictive values were 42.5 and 100%,
respectively. The sensitivity and specificity were 88.2 and 94.1%,
respectively. With 54.55 mg/l as the cut-off point of C-reactive
protein, the sensitivity and specificity of prediction were 88.2
and 94.1%, respectively. The false negative and false positive
rates were 11.8 and 5.9%, respectively. The Youden index value was
82.3% and the positive predictive and negative predictive values
were 75 and 96.7%, respectively. With 7 days as the cut-off point
of surgical timing and 54.55 mg/l as the cut-off point of
C-reactive protein at the same time, the positive predictive and
negative predictive values were 88.2 and 97.6%, respectively. The
false negative and false positive rates were 11.8 and 2.4%,
respectively. The Youden index was 85.8%. The positive predictive
and negative predictive values were 88.2 and 97.6%,
respectively.
We showed that surgical timing and C-reactive
protein were strongly correlated with postoperative infection and
this correlation was not affected by age, sex and other
inflammatory indexes. We concluded that the incidence of
postoperative infection can be reduced if both factors were applied
for the determination of surgery. In addition, incidence of
complications could be reduced and the cure rate improved.
References
|
1
|
Morris BJ, Unger RZ, Archer KR, Mathis SL,
Perdue AM and Obremskey WT: Risk factors of infection after ORIF of
bicondylar tibial plateau fractures. J Orthop Trauma. 27:e196–e200.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yu X, Pang QJ, Chen L, Yang CC and Chen
XJ: Postoperative complications after closed calcaneus fracture
treated by open reduction and internal fixation: A review. J Int
Med Res. 42:17–25. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Korim MT, Payne R and Bhatia M: A
case-control study of surgical site infection following operative
fixation of fractures of the ankle in a large U.K. trauma unit.
Bone Joint J. 96-B:1–640. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hur JW, Park YK, Kim BJ, Moon HJ and Kim
JH: Risk factors for delayed hinge fracture after plate-augmented
cervical open-door laminoplasty. J Korean Neurosurg Soc.
59:368–373. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hull PD, Johnson SC, Stephen DJ, Kreder HJ
and Jenkinson RJ: Delayed debridement of severe open fractures is
associated with a higher rate of deep infection. Bone Joint J.
96-B:1–384. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wei SJ, Cai XH, Wang HS, Qi BW and Yu AX:
A comparison of primary and delayed wound closure in severe open
tibial fractures initially treated with internal fixation and
vacuum-assisted wound coverage: A case-controlled study. Int J
Surg. 12:688–694. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kurylo JC, Axelrad TW, Tornetta P III and
Jawa A: Open fractures of the distal radius: The effects of delayed
debridement and immediate internal fixation on infection rates and
the need for secondary procedures. J Hand Surg Am. 36:1131–1134.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Watanabe K, Kino Y and Yajima H: Factors
affecting the functional results of open reduction and internal
fixation for fracture-dislocations of the proximal interphalangeal
joint. Hand surg. 20:107–114. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wongwai T, Wajanavisit W and Woratanarat
P: Non-union and avascular necrosis of delayed reduction and screw
fixation in displaced femoral neck fracture in young adults. J Med
Assoc Thai Suppl. 10:S120–S127. 2012.
|
|
10
|
Asif N, Ahmad S, Qureshi OA, Jilani LZ,
Hamesh T and Jameel T: Unstable intertrochanteric fracture fixation
- is proximal femoral locked compression plate better than dynamic
hip screw. J Clin Diagn Res. 10:RC09–RC13. 2016.PubMed/NCBI
|
|
11
|
Wetzel RJ, Minhas SV, Patrick BC and
Janicki JA: Current practice in the management of type I open
fractures in children: A survey of POSNA membership. J Pediatr
Orthop. 35:762–768. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhang L, Liu Y, Chen S and Wang Y:
Clinical observation of the vitreous surgery for open-globe
injuries in different timing after the trauma. Zhonghua Yan Ke Za
Zhi. 50:121–125. 2014.(In Chinese). PubMed/NCBI
|
|
13
|
Ovaska MT, Mäkinen TJ, Madanat R, Vahlberg
T, Hirvensalo E and Lindahl J: Predictors of poor outcomes
following deep infection after internal fixation of ankle
fractures. Injury. 44:1002–1006. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lin S, Mauffrey C, Hammerberg EM, Stahel
PF and Hak DJ: Surgical site infection after open reduction and
internal fixation of tibial plateau fractures. Eur J Orthop Surg
Traumatol. 24:797–803. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gross CE, P N Chalmers, Ellman M,
Fernandez JJ and Verma NN: Acute brachial plexopathy after
clavicular open reduction and internal fixation. J Shoulder Elbow
Surgery. 22:e6–e9. 2013. View Article : Google Scholar
|
|
16
|
Chapman TWL, Harris NM, Rogers M, Wilson P
and McDiarmid J: Delayed brachial plexopathy in clavicular fracture
with tri-cord neurapraxia and complete recovery. Eur J Plast Surg.
29:295–297. 2007. View Article : Google Scholar
|
|
17
|
Zhang B, Yang M, Zhou Q and Liu Q: Open
reduction and internal fixation of delayed intracapsular comminuted
condylar fracture of mandible with preoperative computer-aided
design. Int J Oral Maxillofac Surg. 44:e313–e314. 2015. View Article : Google Scholar
|
|
18
|
Ruedi TP, Buckley RE and Moran CG: AO
Principles of Fracture Management. 2nd. Thieme; Sttutgart, New
York: pp. 3222007
|
|
19
|
Nanchahal J, Nayagam S, Khan U, Moran C,
Barrett S, Sanderson F and Pallister I: Standards for the
Management of Open Fractures of the Lower Limb. Royal Society of
Medicine Press; London: pp. 8–10. 2009
|
|
20
|
Eriksson AL, Moverare-Skrtic S, Ljunggren
Ö, Karlsson M, Mellstrom D and Ohlsson C: High-sensitivity CRP is
an independent risk factor for all fractures and vertebral
fractures in elderly men: The MrOS Sweden study. J Bone Miner Res.
29:418–423. 2014. View Article : Google Scholar : PubMed/NCBI
|