Introduction
Gliomas account for approximately 30% of all brain
and central nervous system tumors (1), and glioblastoma is the most common and
malignant glioma (2). Despite
advances in surgical resection, radiotherapy, chemotherapy and
other therapeutic approaches, including immune and gene therapy,
the prognosis for patients with glioblastoma remains poor (3–7). A
previous study demonstrated that the median survival time of
patients with glioblastoma was 4.9 months following diagnosis
(8). Resistance of glioblastoma
cells to irradiation therapy is a major obstacle in the treatment
of human glioblastoma (9).
Therefore, it is important to elucidate the mechanisms underlying
this resistance to irradiation therapy and identify efficient
radiosensitizers.
MicroRNAs (miRNAs or miRs) are a class of small,
functional and non-coding RNAs that regulate the expression of
target mRNAs at the post-transcriptional level (10,11). The
altered expression of specific miRNAs has been implicated to serve
important roles in the initiation and progression of tumors,
including tumor radiation resistance (12,13).
The human miR-590 family has two mature members,
miR-590-3p and miR-590-5p. It has been demonstrated that miR-590 is
associated with the development of various types of cancer,
including breast cancer (14),
cervical cancer (15), clear cell
renal carcinoma (16) and
hepatocellular carcinoma (17). To
the best of our knowledge, the present study is the first to
investigate the expression and function of miR-590 in human
gliomas.
Leucine-rich repeats and immunoglobulin-like domains
protein 1 (LRIG1) is considered to be a tumor suppressor in various
types of cancer and is frequently downregulated in gliomas
(18–21). Therefore, the present study
elucidated whether LRIG1 is a novel direct target by which
miR-590-3p exerts its effect on radiosensitivity, as LRIG1 is
predicted to be a target of miR-590-3p (http://www.microrna.org/microrna/home.do) and the
expression of LRIG1 is associated with radiosensitivity in human
glioblastoma (22). Furthermore, the
levels of miR-590-3p and miR-590-5p expression in human glioma
tissues and radioresistant human glioblastoma cells (U251R) were
evaluated and the effect of miR-590-3p on the radiosensitivity of
U251R cells in vitro was investigated.
Materials and methods
Tissue collection
The collection of tissue samples was approved by the
Ethics Committee of The First Affiliated Hospital of Soochow
University (Suzhou, China). All participants provided written
informed consent prior to enrollment. Glioma tissue and matched
adjacent normal tissue were collected from 35 patients with glioma
who underwent surgery at The First Affiliated Hospital of Soochow
University between May 2013 and March 2015, including 5 patients
with grade I, 12 patients with grade II, 6 patients with grade III
and 12 patients with grade IV. The grades of gliomas were
determined according to WHO criteria (23). None of these patients had received
radiotherapy or chemotherapy prior to surgery.
Cell culture and irradiation
treatment
U251 and HEK293 cells were purchased from the cell
bank of the Type Culture Collection of the Chinese Academy of
Sciences (Shanghai, China), and were cultured in Dulbecco's
modified Eagle's medium (DMEM) with 10% fetal bovine serum and 2 mM
L-glutamine (all Gibco; Thermo Fisher Scientific, Inc., Waltham,
MA, USA). Cells were maintained at 37°C in an atmosphere containing
5% CO2. The U251 cells were then exposed to a series of
increasing X-ray doses from 1–10 Gy at a dose rate of 1 Gy/min for
ten repeats, and the surviving cells were harvested, cultured in
DMEM supplemented with 10% fetal bovine serum and 2 mM L-glutamine
at 37°C and designated as the radioresistant subline (U251R). U251
and U251R cells were treated with 6 Gy X-ray radiation 24 h prior
to MTT assay and flow cytometry. For colony formation assay, the
U251 and the U251R cells were exposed to 0–8 Gy X-ray
radiation.
Cell transfection
Cells were seeded onto six-well plates at 5×104
cells/well at 37°C overnight until 50% confluence was reached. A
total of 5 µl Lipofectamine® 2000 (Invitrogen; Thermo Fisher
Scientific, Inc.), 10 nM miR-590-3p mimic, 10 nM miR-590-3p
inhibitor and 10 nM LRIG1 short interfering (si)RNA (forward,
5′-CCGGUUCUAUUUCAGCUAATT-3′ and reverse,
5′-UUAGCUGAAAUAGAACCGGTT-3′; all from Shanghai GenePharma Co.,
Ltd., Shanghai, China) were diluted in 250 µl Opti-MEM I
(Invitrogen; Thermo Fisher Scientific, Inc.) separately and
incubated at room temperature for 5 min. The mimic/inhibitor or
siRNA was subsequently mixed gently with Lipofectamine® 2000 and
incubated at room temperature for 20 min to form complexes. The
complexes were added to each well and plates were incubated at 37°C
for 6 h. The medium was subsequently replaced with fresh
medium.
Luciferase assay
The wild type or mutant LRIG1 3′ untranslated region
(UTR; Shenzhen Lvshiyuan Biotechnology Co., Ltd., Shenzhen, China)
was cloned into the pmirGLO luciferase reporter vector (Promega
Corporation, Madison, WI, USA), and co-transfected with the
miR-590-3p mimic or the miR-negative control (NC) (Shanghai
GenePharma Co., Ltd., Shanghai, China) into the HEK293 cells using
Lipofectamine® 2000 (Invitrogen; Thermo Fisher Scientific, Inc.).
The pRL-TK Renilla luciferase reporter vector (Promega Corporation)
was transfected into cells as an internal control. At 24 h
following transfection, luciferase activity was measured using a
Dual-Luciferase Reporter Assay System (Promega Corporation)
following cells lysis with Passive Lysis Buffer included in the
Reporter Assay System. Relative luciferase activity was calculated
as the ratio of firefly luciferase activity to Renilla luciferase
activity.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
miRNAs were isolated from the harvested tissues and
cultured cells using the miRNeasy Mini kit (Qiagen GmbH, Hilden,
Germany) according to the manufacturer's protocols. A total of 1 µg
RNA was reverse transcribed to cDNA using the First Strand cDNA
Synthesis kit (Fermentas, Vilnius, Lithuania). Specific primers for
miR-590-3p (forward, 5′-TAATTTTATGTATAAGCTAGT-3′ and reverse,
5′-TGGTGTCGTGGAGTCG-3′) and miR-590-5p (forward,
5′-TAATTTTATGTATAAGCTAGT-3′ and reverse, 5′-TGGTGTCGTGGAGTCG-3′)
were obtained from Sangon Biotech Co., Ltd. (Shanghai, China). qPCR
was performed using the SYBR-Green PCR kit (Applied Biosystems;
Thermo Fisher Scientific, Inc.) in an ABI Prism 7900HT Sequence
Detection System (Applied Biosystems; Thermo Fisher Scientific,
Inc.). The PCR reaction conditions were as follows: 40 cycles at
95°C for 30 sec, 1 cycle at 59°C for 30 sec and 1 cycle at 72°C for
30 sec. All reactions were repeated three times. The U6 gene was
used for the internal control. miR-590-3p and miR-590-5p levels
were quantified using the 2−ΔΔCq method (24).
Western blot analysis
Total protein was extracted from the cultured cells
using a Total Protein Extraction kit (Nanjing KeyGen Biotech Co.,
Ltd., Nanjing, China) and centrifuged at 1,000 × g at room
temperature for 10 min. A 10% SDS-PAGE gel was used to separate
total proteins (20 µg/lane), which was subsequently transferred
onto nitrocellulose membranes (EMD Millipore, Billerica, MA, USA)
via electroblotting. Following blocking with non-fat milk at 4°C
overnight, membranes were incubated with the primary rabbit
polyclonal LRIG1 antibody (1:400; cat. no. ab36707) and rabbit
polyclonal GAPDH antibody (1:1,000; cat. no. ab37168; Abcam,
Cambridge, MA, USA) at 37°C for 1 h, respectively, followed by
incubation with the mouse monoclonal anti-rabbit immunoglobulin
horseradish peroxidase-conjugated secondary antibody (1:2,000; cat.
no. ab99702; Abcam) at 37°C for 1 h. GAPDH antibody was used as a
loading control. The signals were detected using a Pierce™ Fast
Western Blot kit with ECL Substrate (Pierce; Thermo Fisher
Scientific, Inc.). Band density was quantified using ImageJ 1.48
software (National Institutes of Health, Bethesda, MD, USA).
Experiments were repeated three times.
MTT assay
Cells were incubated in 96-well plates at a density
of 5×104 cells/ml and allowed to grow at 37°C for 24, 48, 72 and 96
h. A total of 10 µl MTT (0.5 mg/ml; Sigma-Aldrich; Merck KGaA,
Darmstadt, Germany) was added to each well and cells were incubated
at 37°C for another 4 h. Culture medium was subsequently discarded,
and 150 µl dimethylsulfoxide (Sigma-Aldrich; Merck KGaA) was added
to each well to dissolve the formazan crystals. Absorbance was
measured at 570 nm using a microplate reader.
Flow cytometry
Cell apoptosis rate was determined using the Annexin
V-fluorescein isothiocyanate and propidium iodide (PI) Apoptosis
assay kit (Nianjin KeyGen Biotech Co., Ltd.) and flow cytometry. A
total of 5×105 cells/well were seeded into six-well plates and were
cultured in DMEM supplemented with 10% fetal bovine serum and 2 mM
L-glutamine. Cells were treated with 6 Gy radiation. Following 24
h, cells were subsequently harvested, washed 3 times with
phosphate-buffered saline, and dual-stained with PI and Alexa Fluor
488-Annexin V. The stained cells were analyzed via flow cytometry
on a BD Accuri C6 flow cytometer and CFlow Plus software,
v1.0.172.9 (BD Biosciences, Franklin Lakes, NJ, USA).
Colony formation assay
Cells were plated in six-well plates at densities of
100, 400, 600, 800 and 1,000 cells/well and were exposed to 0, 2,
4, 6 and 8 Gy radiation, respectively. Following incubation at 37°C
for 14 days, the cells were fixed with 4% paraformaldehyde at room
temperature for 15 min and then stained with 0.5% crystal violet.
Colonies with >50 cells were counted under a light
microscope.
Statistical analysis
Data are expressed as the mean + standard deviation.
SPSS 19.0 software (IBM SPSS, Armonk, NY, USA) was used for
statistical analysis. Comparison of data between two groups was
performed using the Student's t-test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Expression of miR-590 in human glioma
tissues
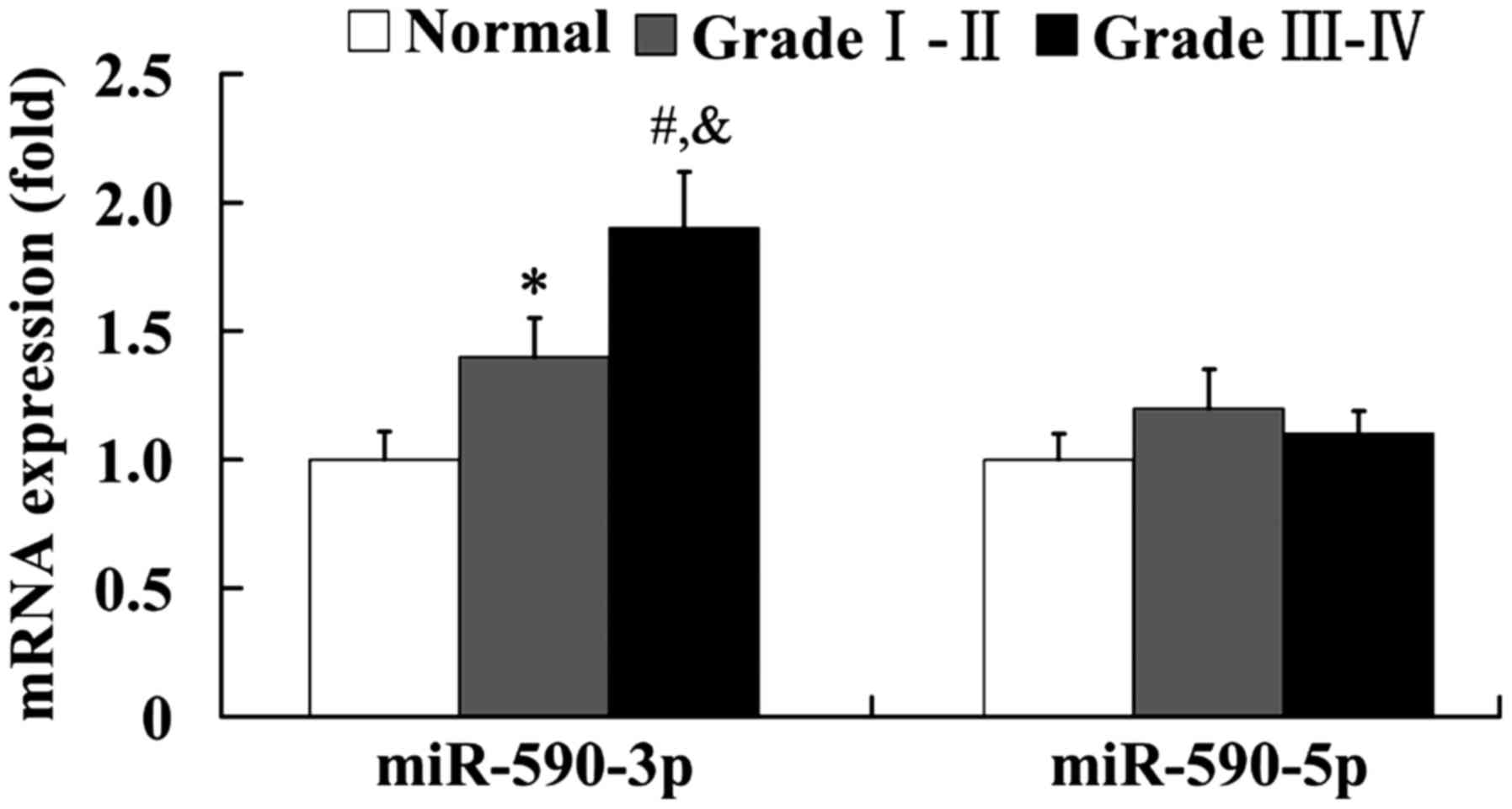
The expression of miR-590-3p and miR-590-5p in human
glioma tissues was examined using RT-qPCR. As shown in Fig. 1, the mRNA level of miR-590-3p was
significantly upregulated in the grades I–II and III–IV glioma
tissues compared with the normal brain tissues (P<0.05 and
P<0.01, respectively). Furthermore, it was found that miR-590-3p
expression levels were significantly higher in the high grade
gliomas (grades III and IV) than in the low grade gliomas (grades I
and II; P<0.05). However, the mRNA level of miR-590-5p did not
show any significant difference between the normal and glioma
tissues (Fig. 1).
Establishment of U251R glioblastoma
cell
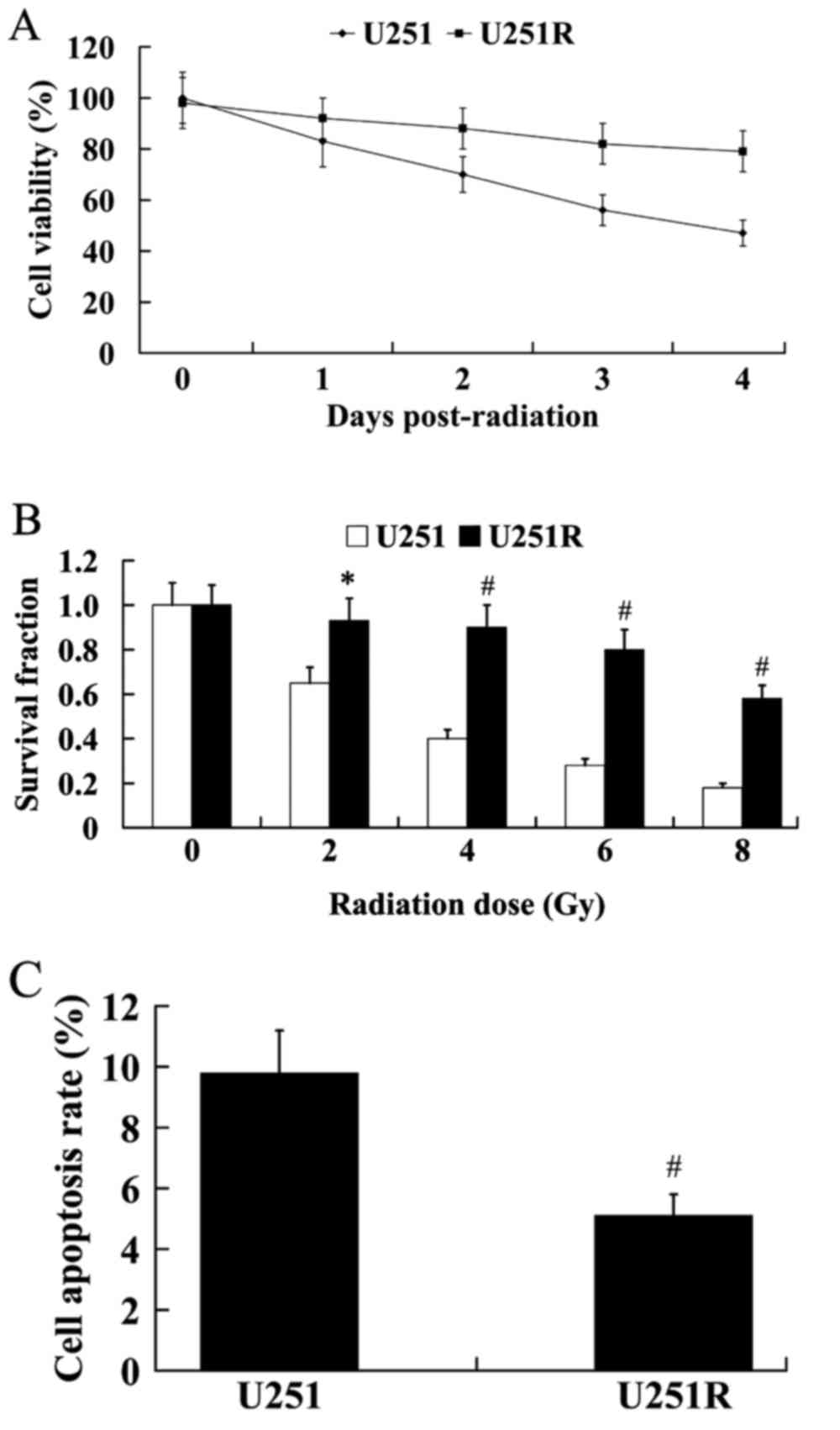
As shown in Fig. 2A,
the U251R cells exhibited higher cell viability compared with the
U251 cells. The results from colony formation assay demonstrated
that U251R cells exhibited significantly higher colony formation
capacity following irradiation than U251 cells (Fig. 2B; P<0.05 at 2 Gy; P<0.01 at 4,
6 and 8 Gy). In addition, U251R cells had a significantly lower
cell apoptosis rate than U251 cells following irradiation (Fig. 2C; P<0.01).
Expression of miR-590 and LRIG1 in
U251R cells
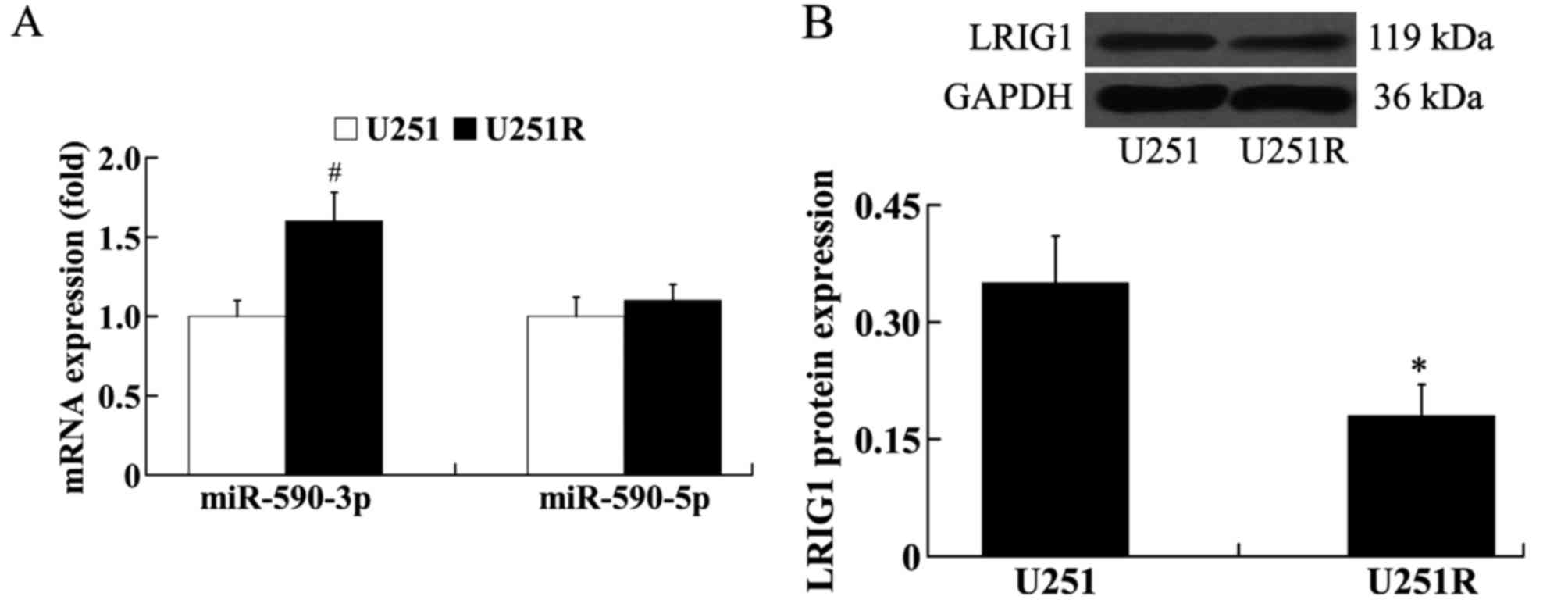
The expression of miR-590-3p, miR-590-5p and LRIG1
in the radioresistant cells U251R was evaluated using RT-qPCR and
western blot analysis. The results from RT-qPCR analysis showed
that, compared with U251 cells, the expression level of miR-590-3p
was significantly increased in the U251R cells (P<0.01);
however, the expression level of miR-590-5p was not significantly
different between U251 and U251R cells (Fig. 3A). The results from western blot
analysis demonstrated that the expression of LRIG1 protein was
significantly downregulated in U251R cells compared with U251 cells
(Fig. 3B; P<0.05).
Effect of miR-590-3p on the
radiosensitivity of U251R cells
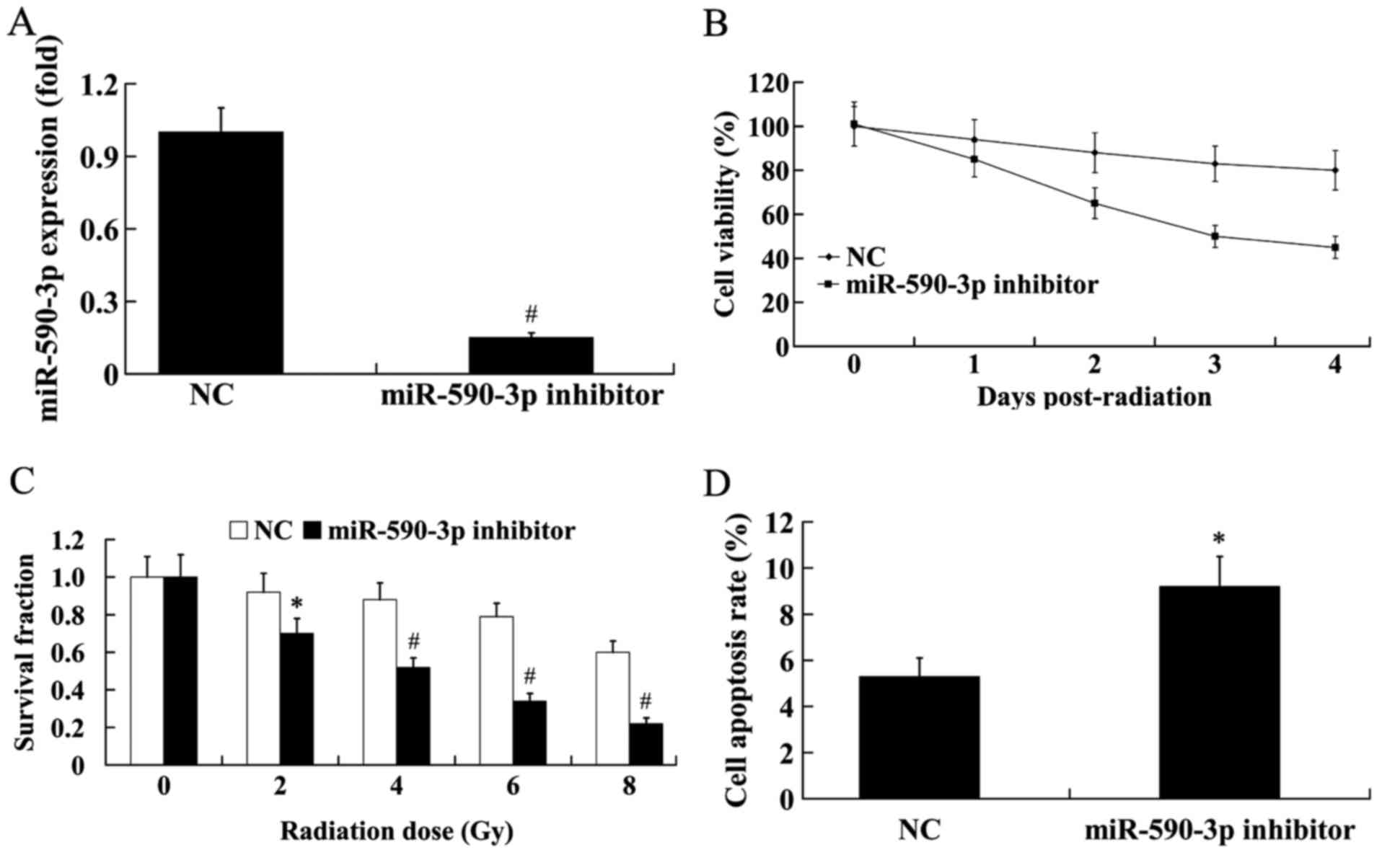
To investigate the effect of miR-590-3p on the
radiosensitivity of U251R cells, the miR-590-3p inhibitor was
transfected into the U251R cells, and the cells were exposed to 6
Gy radiation for 24 h. As shown in Fig.
4A, the mRNA level of miR-590-3p in cells transfected with the
miR-590-3p inhibitor significantly decreased to 15% of the control
(P<0.01). The results from MTT assay revealed that the cells
transfected with the miR-590-3p inhibitor exhibited markedly
decreased cell viability compared with the control (Fig. 4B). Colony formation capacity was also
significantly decreased in the cells transfected with the
miR-590-3p inhibitor following irradiation, compared with controls
(Fig. 4C; P<0.05 at 2 Gy;
P<0.01 at 4, 6 and 8 Gy). Furthermore, flow cytometry
demonstrated that transfection with the miR-590-3p inhibitor
significantly increased the cell apoptosis rate (Fig. 4D; P<0.05).
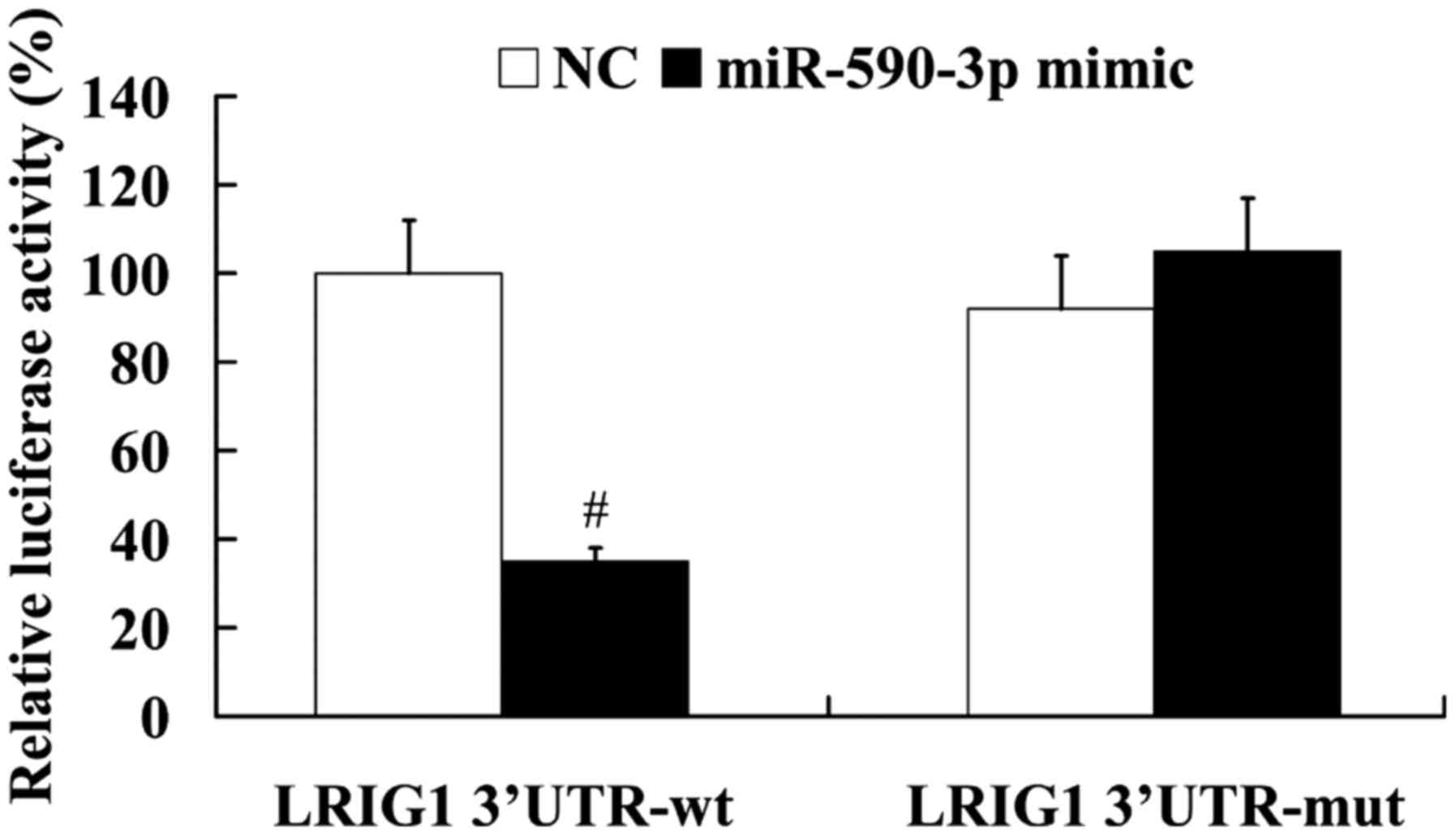
LRIG1 is a direct target of
miR-590-3p
To elucidate the association between miR-590-3p and
LRIG1, the LRIG1 3′UTR containing the wild type or mutant potential
target site of miR-590-3p was constructed, and co-transfected with
the miR-590-3p mimic into HEK293 cells. The results from the
luciferase reporter assay demonstrated that the miR-590-3p mimic
significantly decreased the luciferase activity of wild type LRIG1
3′UTR (P<0.01), whereas the luciferase activity of mutant LRIG1
3′UTR was not significantly affected by the miR-590-3p mimic
(Fig. 5).
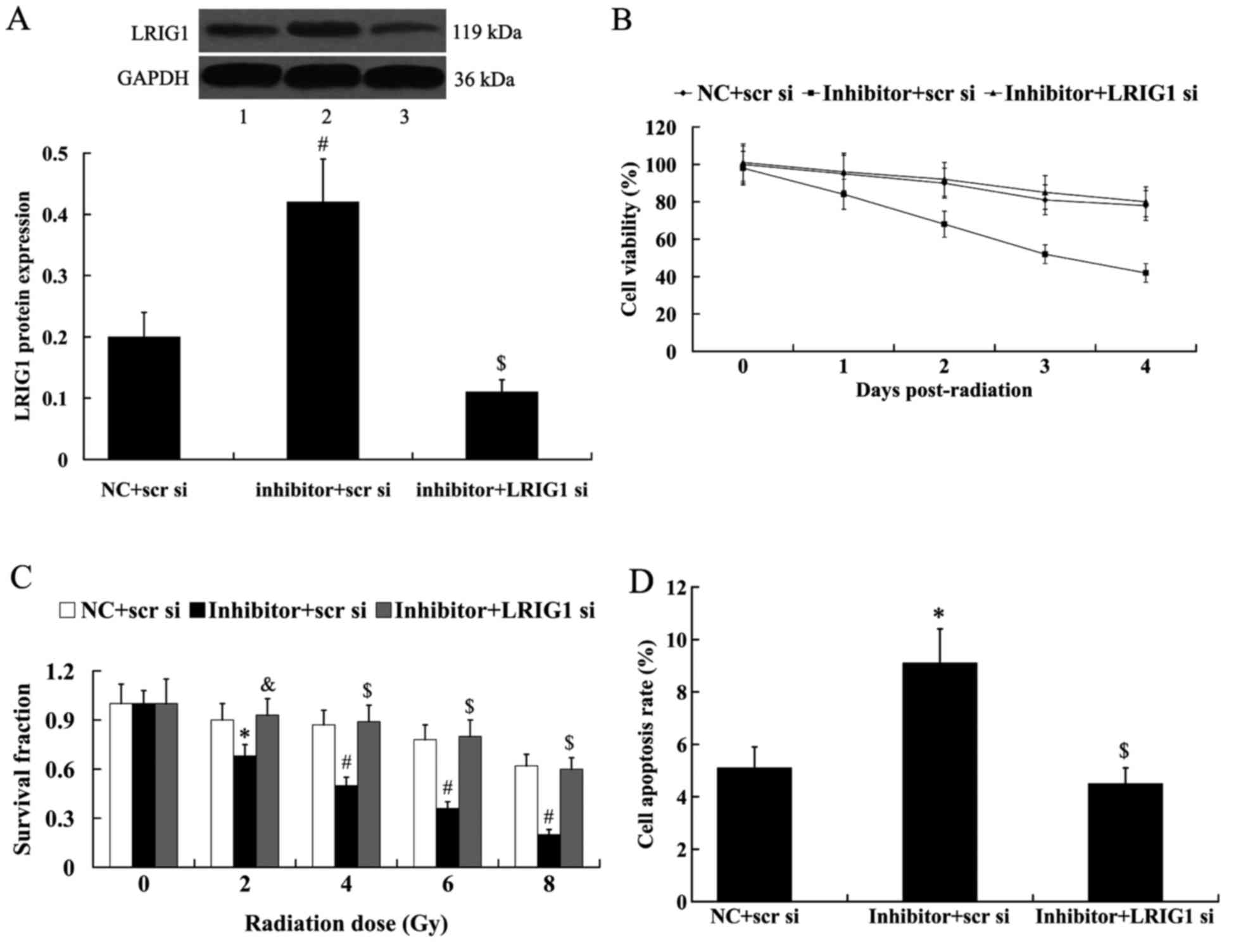
LRIG1 mediates the effect of
miR-590-3p on the radiosensitivity of U251R cells
To identify whether LRIG1 mediates the effect of
miR-590-3p on the radiosensitivity of U251R cells, LRIG1 siRNA was
transfected into U251R cells to knockdown LRIG1, and the cells were
exposed to 6 Gy radiation for 24 h. As shown in Fig. 6A, miR-590-3p inhibitor significantly
increased the expression of LRIG1 protein in U251R cells compared
with controls (P<0.01); however, this increased LRIG1 expression
was abolished by the transfection of LRIG1 siRNA. The effect of
miR-590-3p on the radiosensitivity of U251R cells was significantly
attenuated by LRIG1 (P<0.01). As demonstrated in Fig. 6B, suppression of miR-590-3p by
treatment with miR-590-3p inhibitor resulted in markedly decreased
cell viability; however, these effects were reversed by the
transfection of LRIG1 siRNA. Colony formation capacity was also
significantly decreased in the cells transfected with the
miR-590-3p inhibitor + scramble siRNA following irradiation,
compared with controls (Fig. 6C;
P<0.05 at 2 Gy; P<0.01 at 4, 6 and 8 Gy). These effects were
significantly reversed in the miR-590-3p inhibitor + LRIG1 siRNA
group (Fig. 6C; P<0.05 at 2 Gy;
P<0.01 at 4, 6 and 8 Gy). The cell apoptosis rate were
significantly different between the miR-590-3p inhibitor + scramble
siRNA group and the miR-590-3p inhibitor + LRIG1 siRNA group
(Fig. 6D; P<0.01).
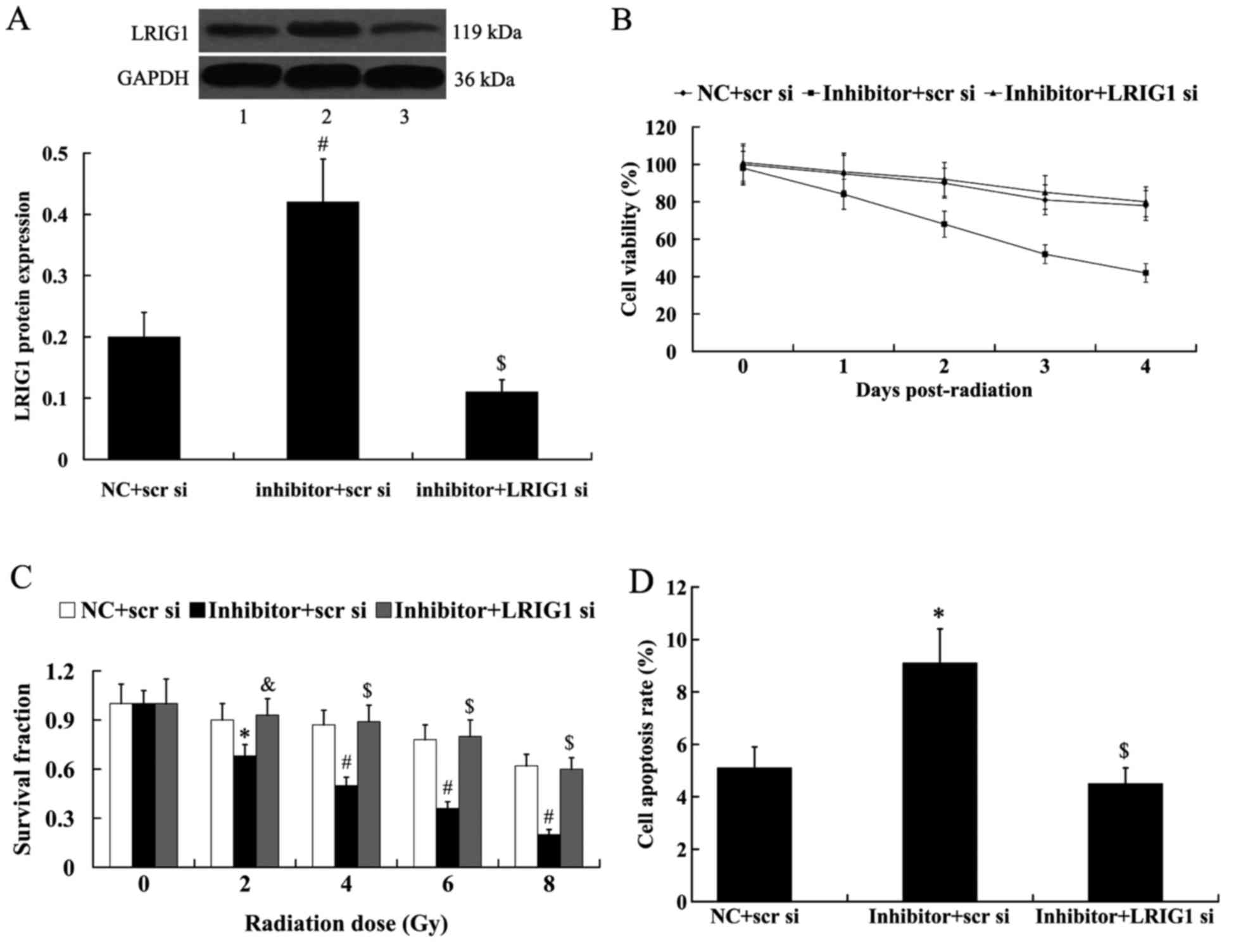 | Figure 6.LRIG1 reversed the effect of
miR-590-3p on the radiosensitivity of U251R cells. U251R cells were
exposed to radiation following transfection. (A) Relative protein
level of LRIG1 in U251R cells following transfection with the
miR-590-3p inhibitor and LRIG1 siRNA. Lane 1, NC + scr si; lane 2,
inhibitor + scr si; lane 3, inhibitor + LRIG1 si. (B) Cell
viability of U251R cells following transfection with the miR-590-3p
inhibitor and LRIG1 siRNA. (C) Survival fraction of U251R cells
following transfection with the miR-590-3p inhibitor and LRIG1
siRNA. (D) Cell apoptosis rate of U251R cells following
transfection with the miR-590-3p inhibitor and LRIG1 siRNA.
*P<0.05, #P<0.01 vs. NC + scr si; &P<0.05, $P<0.01
vs. inhibitor + scr si. LRIG1, leucine-rich repeats and
immunoglobulin-like domains protein 1; miR, microRNA; U251R,
radioresistant U251; si, short interfering; NC, negative control;
scr, scramble. |
Discussion
In the present study, it was initially demonstrated
that miR-590-3p was upregulated in the human glioma tissues, and
its expression level was higher in high grade than in low grade
gliomas. These data suggested that miR-590-3p may contribute to the
initiation and development of human gliomas.
Radiotherapy is essential for the treatment of
>30% of newly diagnosed cancer patients (25). Various miRNAs have been demonstrated
to be associated with the radiosensitivity of human glioma cells,
such as miR-181a, miR-124 and miR-26a (26–30). The
present results indicate that the expression level of miR-590-3p
was higher in the radioresistant human glioblastoma cells than that
in the parental glioblastoma cells. In vitro experiments
were subsequently performed to elucidate the role of miR-590-3p in
the radiosensitivity of glioblastoma cells. It was demonstrated
that downregulation of miR-590-3p enhanced the radiosensitivity of
the radioresistant human glioblastoma cells U251R, as demonstrated
by suppressed cell viability, decreased colony formation capacity,
and increased cell apoptosis rate. These results indicated that
miR-590-3p decreases radiation sensitivity of glioblastoma
cells.
LRIG1 is a transmembrane protein that functions as a
tumor suppressor in various human cancer cell types (18–20).
LRIG1 downregulation has been implicated to be associated with a
poor prognosis of patients with renal cell carcinoma or ocular
surface squamous neoplasia (31,32).
Previous studies have indicated that LRIG1 was frequently decreased
in gliomas (21), and the expression
level of LRIG1 is significantly correlated with the malignancy of
glioma (21,33). It has also been reported that
upregulation of LRIG1 expression suppresses malignant glioma cell
growth and induces cell apoptosis (21,34–36),
whereas downregulation of LRIG1 expression promotes the
proliferation and aggressive properties of glioma cells (37,38).
Furthermore, previous studies have suggested that LRIG1 is
associated with the regulation of chemosensitivity of human cancer
cells (39,40). It has been elucidated that LRIG1
sensitizes glioma cells to cisplatin and temozolomide (22,41–43).
Recently, Yang et al (22)
reported that LRIG1 expression was associated with the
radiosensitivity of human glioblastoma cells, and LRIG1
overexpression enhances the radiosensitivity of radioresistant
human glioblastoma U251 cells. Consistent with these findings, the
present study demonstrated that LRIG1 was downregulated in
radioresistant human glioblastoma cells. Furthermore, the
luciferase reporter assay demonstrated that LRIG1 was a direct
target of miR-590-3p. The effect of miR-590-3p suppression on cell
viability, colony formation capacity and cell apoptosis rate was
attenuated by the knockdown of LRIG1 in U251R cells. These results
suggested that LRIG1 is able to mediate the effect of miR-590-3p on
the radiosensitivity of human glioblastoma cells.
In conclusion, the present study identified
miR-590-3p as a potential target of radioresistance in human
gliomas, and demonstrated that LRIG1 was associated with mediating
the effect of miR-590-3p on the radiosensitivity of human
glioblastoma cells. These findings may improve the understanding of
the association between miRNAs and radiosensitivity in gliomas, and
may provide potential therapeutic strategies to prevent
radioresistance.
References
|
1
|
Dolecek TA, Propp JM, Stroup NE and
Kruchko C: CBTRUS statistical report: Primary brain and central
nervous system tumors diagnosed in the United States in 2005–2009.
Neuro Oncol. 14 Suppl 5:v1–v49. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mihailović G, Marković M, Zivković N,
Mihailović G, Marković M, Berisavac I and Spaić M: Epidemiological
features of brain tumors. Srp Arh Celok Lek. 141:823–829. 2013.(In
Serbian). View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Stupp R, Mason WP, Van den Bent MJ, Weller
M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn
U, et al: Radiotherapy plus concomitant and adjuvant temozolomide
for glioblastoma. New Engl J Med. 352:987–996. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wang Y and Jiang T: Understanding high
grade glioma: Molecular mechanism, therapy and comprehensive
management. Cancer Lett. 331:139–146. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Carlsson SK, Brothers SP and Wahlestedt C:
Emerging treatment strategies for glioblastoma multiforme. EMBO Mol
Med. 6:1359–1370. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Omuro A and DeAngelis LM: Glioblastoma and
other malignant gliomasa: Clinical review. JAMA. 310:1842–1850.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Van Meir EG, Hadjipanayis CG, Norden AD,
Shu HK, Wen PY and Olson JJ: Exciting new advances in
neuro-oncology: The avenue to a cure for malignant glioma. CA
Cancer J Clin. 60:166–193. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ohgaki H, Dessen P, Jourde B, Horstmann S,
Nishikawa T, Di Patre PL, Burkhard C, Schüler D, Probst-Hensch NM,
Maiorka PC, et al: Genetic pathways to glioblastoma: A
population-based study. Cancer Res. 64:6892–6899. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Atkins RJ, Ng W, Stylli SS, Hovens CM and
Kaye AH: Repair mechanisms help glioblastoma resist treatment. J
Clin Neurosci. 22:14–20. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ambros V: The functions of animal
microRNAs. Nature. 431:350–355. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bartel DP: MicroRNAs: Genomics,
biogenesis, mechanism and function. Cell. 116:281–297. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Calin GA, Sevignani C, Dumitru CD, Hyslop
T, Noch E, Yendamuri S, Shimizu M, Rattan S, Bullrich F, Negrini M
and Croce CM: Human microRNA genes are frequently located at
fragile sites and genomic regions involved in cancers. Proc Natl
Acad Sci USA. 101:pp. 2999–3004. 2004; View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sevignani C, Calin GA, Nnadi SC, Shimizu
M, Davuluri RV, Hyslop T, Demant P, Croce CM and Siracusa LD:
MicroRNA genes are frequently located near mouse cancer
susceptibility loci. Proc Natl Acad Sci USA. 104:pp. 8017–8022.
2007; View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Miranda PJ, Vimalraj S and Selvamurugan N:
A feedback expression of microRNA-590 and activating transcription
factor-3 in human breastcancer cells. Int J Biol Macromol.
72:145–150. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chu Y, Ouyang Y, Wang F, Zheng A, Bai L,
Han L, Chen Y and Wang H: MicroRNA-590 promotes cervical cancer
cell growth and invasion by targeting CHL1. J Cell Biochem.
115:847–853. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Xiao X, Tang C, Xiao S, Fu C and Yu P:
Enhancement of proliferation and invasion by MicroRNA-590-5p via
targeting PBRM1 in clear cell renal carcinoma cells. Oncol Res.
20:537–544. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yang H, Zheng W, Zhao W, Guan C and An J:
Roles of miR-590-5p and miR-590-3p in the development of
hepatocellular carcinoma. Nan Fang Yi Ke Da Xue Xue Bao.
33:804–811. 2013.(In Chinese). PubMed/NCBI
|
|
18
|
Yokdang N, Hatakeyama J, Wald JH, Simion
C, Tellez JD, Chang DZ, Swamynathan MM, Chen M, Murphy WJ, Iii KL
Carraway and Sweeney C: LRIG1 opposes epithelial-to- mesenchymal
transition and inhibits invasion of basal-like breast cancer cells.
Oncogene. 35:2932–2947. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kou C, Zhou T, Han X, Zhuang H and Qian H:
LRIG1, a 3p tumor suppressor, represses EGFR signaling and is a
novel epigenetic silenced gene in colorectal cancer. Biochem
Biophys Res Commun. 464:519–525. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sheu JJ, Lee CC, Hua CH, Li CI, Lai MT,
Lee SC, Cheng J, Chen CM, Chan C, Chao SC, et al: LRIG1 modulates
aggressiveness of head and neck cancers by regulating
EGFR-MAPK-SPHK1 signaling and extracellular matrix remodeling.
Oncogene. 33:1375–1384. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ye F, Gao Q, Xu T, Zeng L, Ou Y, Mao F,
Wang H, He Y, Wang B, Yang Z, et al: Upregulation of LRIG1
suppresses malignant glioma cell growth by attenuating EGFR
activity. J Neurooncol. 94:183–194. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yang JA, Liu BH, Shao LM, Guo ZT, Yang Q,
Wu LQ, Ji BW, Zhu XN, Zhang SQ, Li CJ and Chen QX: LRIG1 enhances
the radiosensitivity of radioresistant human glioblastoma U251
cells via attenuation of the EGFR/Akt signaling pathway. Int J Clin
Exp Pathol. 8:3580–3590. 2015.PubMed/NCBI
|
|
23
|
Louis DN, Ohgaki H, Wiestler OD, Cavenee
WK, Burger PC, Jouvet A, Scheithauer BW and Kleihues P: The 2007
WHO classification of tumours of the central nervous system. Acta
Neuropathol. 114:97–109. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-tie quantitative PCR and
the 2(−Delta Delta C(T)) Method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
One in three newly diagnosed cancer
patients now receives radiation therapy. Oncology (Williston Park).
10:17761996.PubMed/NCBI
|
|
26
|
Chen G, Zhu W, Shi D, Lv L, Zhang C, Liu P
and Hu W: MicroRNA-181a sensitizes human malignant glioma U87MG
cells to radiation by targeting Bcl-2. Oncol Rep. 23:997–1003.
2010.PubMed/NCBI
|
|
27
|
Deng X, Ma L, Wu M, Zhang G, Jin C, Guo Y
and Liu R: miR-124 radiosensitizes human glioma cells by targeting
CDK4. J Neurooncol. 114:263–274. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Guo P, Lan J, Ge J, Nie Q, Guo L, Qiu Y
and Mao Q: MiR-26a enhances the radiosensitivity of glioblastoma
multiforme cells through targeting of ataxia-telangiectasia
mutated. Exp Cell Res. 320:200–208. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Li W, Guo F, Wang P, Hong S and Zhang C:
miR-221/222 confers radioresistance in glioblastoma cells through
activating Akt independent of PTEN status. Curr Mol Med.
14:185–195. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Upraity S, Kazi S, Padul V and Shirsat NV:
MiR-224 expression increases radiation sensitivity of glioblastoma
cells. Biochem Biophys Res Commun. 448:225–230. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Thomasson M, Hedman H, Guo D, Ljungberg B
and Henriksson R: LRIG1 and epidermal growth factor receptor in
renal cell carcinoma: A quantitative RT-PCR and immunohistochemical
analysis. Brit J Cancer. 89:1285–1289. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Nagata M, Nakamura T, Sotozono C, Inatomi
T, Yokoi N and Kinoshita S: LRIG1 as a potential novel marker for
neoplastic transformation in ocular surface squamous neoplasia.
PLoS One. 9:e931642014. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Guo D, Nilsson J, Haapasalo H, Raheem O,
Bergenheim T, Hedman H and Henriksson R: Perinuclear leucine-rich
repeats and immunoglobulin-like domain proteins (LRIG1-3) as
prognostic indicators in astrocytic tumors. Acta Neuropathol.
111:238–246. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Johansson M, Oudin A, Tiemann K, Bernard
A, Golebiewska A, Keunen O, Fack F, Stieber D, Wang B, Hedman H and
Niclou SP: The soluble form of the tumor suppressor Lrig1 potently
inhibits in vivo glioma growth irrespective of EGF receptor status.
Neuro Oncol. 15:1200–1211. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Mao F, Wang B, Xiao Q, Xi G, Sun W, Zhang
H, Ye F, Wan F, Guo D, Lei T and Chen X: A role for LRIG1 in the
regulation of malignant glioma aggressiveness. Int J Oncol.
42:1081–1087. 2013.PubMed/NCBI
|
|
36
|
Ye F, Guo DS, Niu HQ, Tao SZ, Ou YB, Lu YP
and Lei T: Molecular mechanism of LRIG1 cDNA-induced apoptosis in
human glioma cell line H4. Ai Zheng. 23:1149–1154. 2004.(In
Chinese). PubMed/NCBI
|
|
37
|
Xie R, Yang H, Xiao Q, Mao F, Zhang S, Ye
F, Wan F, Wang B, Lei T and Guo D: Downregulation of LRIG1
expression by RNA interference promotes the aggressive properties
ofglioma cells via EGFR/Akt/c-Myc activation. Oncol Rep.
29:177–184. 2013.PubMed/NCBI
|
|
38
|
Mao F, Wang B, Xi G, Sun W, Zhang H, Ye F,
Guo D and Lei T: Effects of RNAi-mediated gene silencing of LRIG1
on proliferation and invasion of glioma cells. J Huazhong Univ Sci
Technolog Med Sci. 32:227–232. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wu X, Hedman H, Bergqvist M, Bergström S,
Henriksson R, Gullbo J, Lennartsson J, Hesselius P and Ekman S:
Expression of EGFR and LRIG proteins in oesophageal carcinoma with
emphasis on patient survival and cellular chemosensitivity. Acta
Oncol. 51:69–76. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Sheu JJ, Lee CC, Hua CH, Li CI, Lai MT,
Lee SC, Cheng J, Chen CM, Chan C, Chao SC, et al: LRIG1 modulates
aggressiveness of head and neck cancers by regulating
EGFR-MAPK-SPHK1 signaling and extracellular matrix remodeling.
Oncogene. 33:1375–1384. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Guo Z, Chen Q, Liu B, Tian D, Zhang S and
Li M: LRIG1 enhances chemosensitivity by modulating BCL-2
expression and receptor tyrosine kinase signaling in glioma cells.
Yonsei Med J. 55:1196–1205. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Qi XC, Xie DJ, Yan QF, Wang YR, Zhu YX,
Qian C and Yang SX: LRIG1 dictates the chemo-sensitivity of
temozolomide (TMZ) in U251 glioblastoma cells via down-regulation
of EGFR/topoisomerase-2/Bcl-2. Biochem Biophys Res Commun.
437:565–572. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Wang X, Xiao Q, Xing X, Tian C, Zhang H,
Ye F, Wan F, Wang B, Guo D and Lei T: LRIG1 enhances cisplatin
sensitivity of glioma cell lines. Oncol Res. 20:205–211. 2012.
View Article : Google Scholar : PubMed/NCBI
|