Introduction
Bronchogenic cysts are congenital lesions resulting
from aberrant budding of the embryonic foregut (1). They may occur at any point along the
tracheobronchial tree and are commonly localized in the mediastinum
and lung parenchyma (2). It has
previously been reported that bronchogenic cysts account for 10% of
all mediastinal masses and are more common in males (3). However, bronchogenic cysts rarely occur
in the larynx (4). To the best of
our knowledge, only two cases of bronchogenic cysts arising from
the larynx have been reported in China (4,5). The
symptoms vary depending on the location and size of the cyst,
typically including chronic cough, dyspnea, dysphagia, chest pain,
hoarseness and increased stridor during sleeping (6). In the present study, a bronchogenic
cyst that developed in the supraglottic area of a 12-year-old
female with consequent hoarseness and increased stidor is
reported.
A 12-year-old female presented with a 2-month
history of dyspnea and a progressively worsening hoarseness lasting
>10 years. No other part of the patient's medical history was
contributory. The patient was admitted to the Emergency Department
of the West China Hospital, Sichuan University (Chengdu, China)
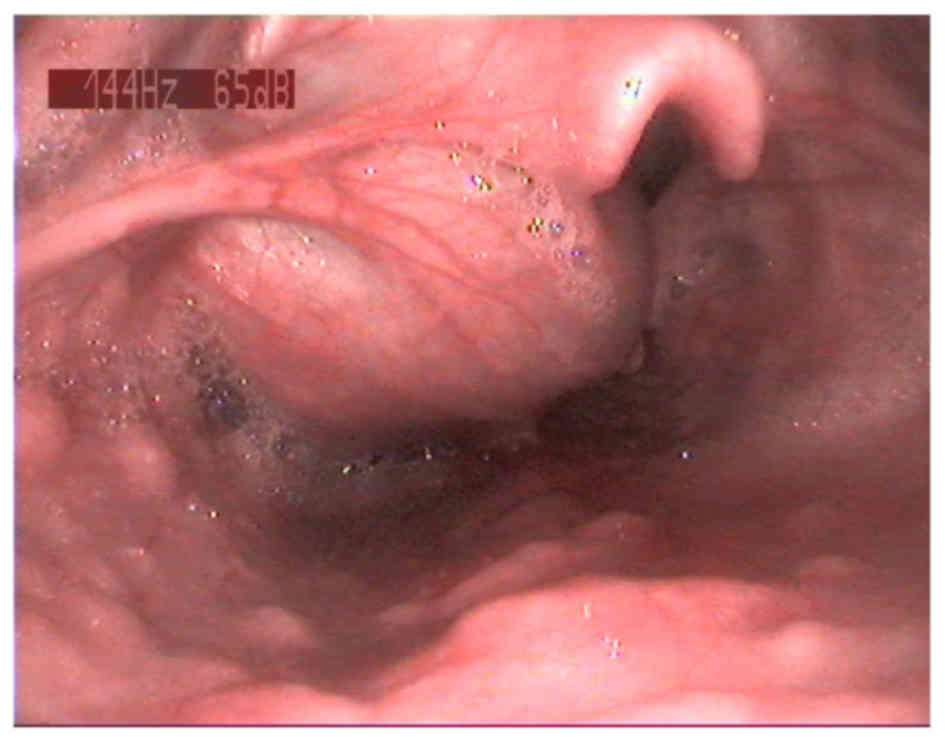
with a grade 2 laryngeal obstruction (7) in May 2015. A flexible laryngoscopy
revealed a large globular mass lesion with a smooth mucosal surface
in the patient's supraglottic area, which obstructed around
two-thirds of the patient's laryngeal cavity (Fig. 1). Physical examinations of the
patient's neck and other otorhinolaryngological areas, analysis of
the patient's blood biochemistry and radiographic analysis of the
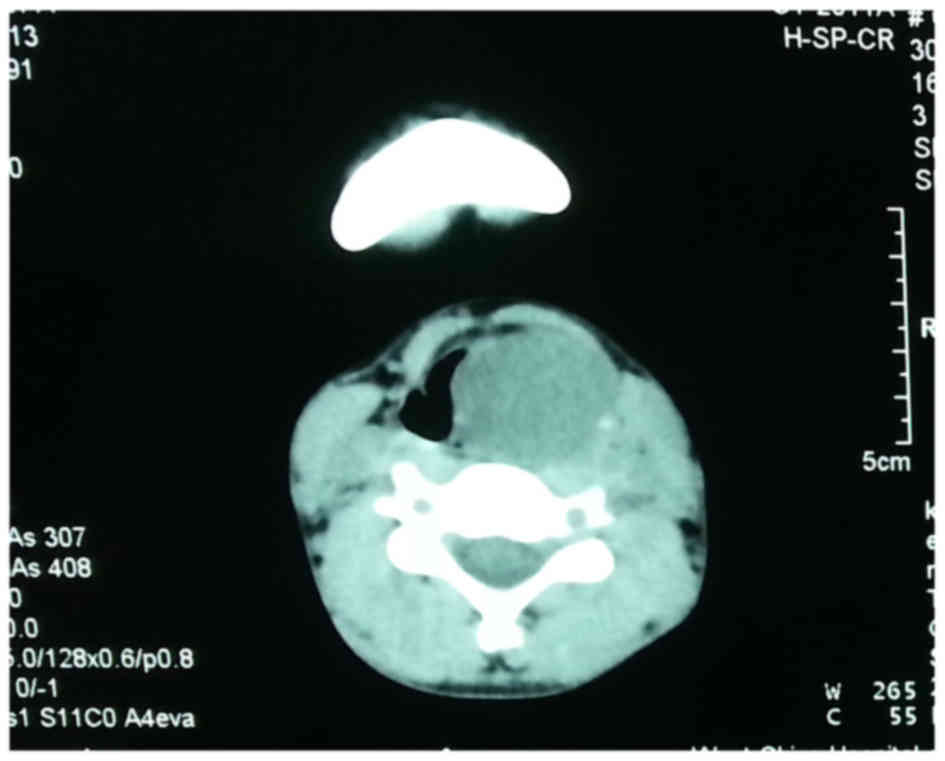
patient's chest were normal and unremarkable. A computed tomography
(CT) scan of the patient's larynx revealed a large, well-defined
cystic mass lesion measuring 3×2×1 cm; as the lesion was located in
the paralaryngeal space, between the patient's hyoid bone and
thyroid gland, narrowing of the patient's glottic area was observed
(Fig. 2). Since the large laryngeal
lesion prevented intubation, a preventive tracheotomy was performed
to secure an unobstructed airway, and then the lesion was excised
using a laser and suspension laryngoscope (Fig. 3).
The vocal folds of the patient were protected by
covering with wet saline gauze during the surgery and the cyst was
determined to arise from the left ventricle of the larynx. The
lesion was excised and identified to contain a clear yellow viscous
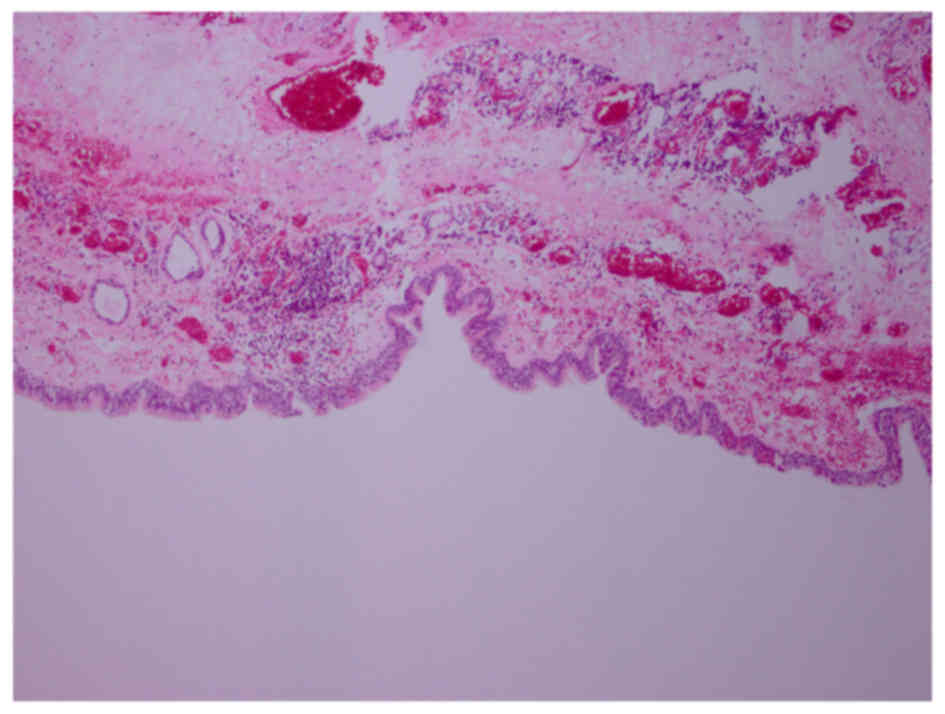
liquid. Postsurgical histopathology revealed that the lesion was
lined by a pseudostratified columnar epithelium and contained a
section of the cyst wall, thus it was diagnosed as a bronchogenic
cyst (Fig. 4). The staining
procedure was performed as previously described. (8,9). Tissue
samples were fixed in 10% formalin for 10 h at room temperature and
embedded in paraffin. Paraffin-embedded tissue specimens were cut
to 3 µm sections and stained with hematoxylin-eosin-saffron as
previously described (9) and
observed under a light microscope (magnification, ×100). There were
no complications during or following the surgery, and the patient
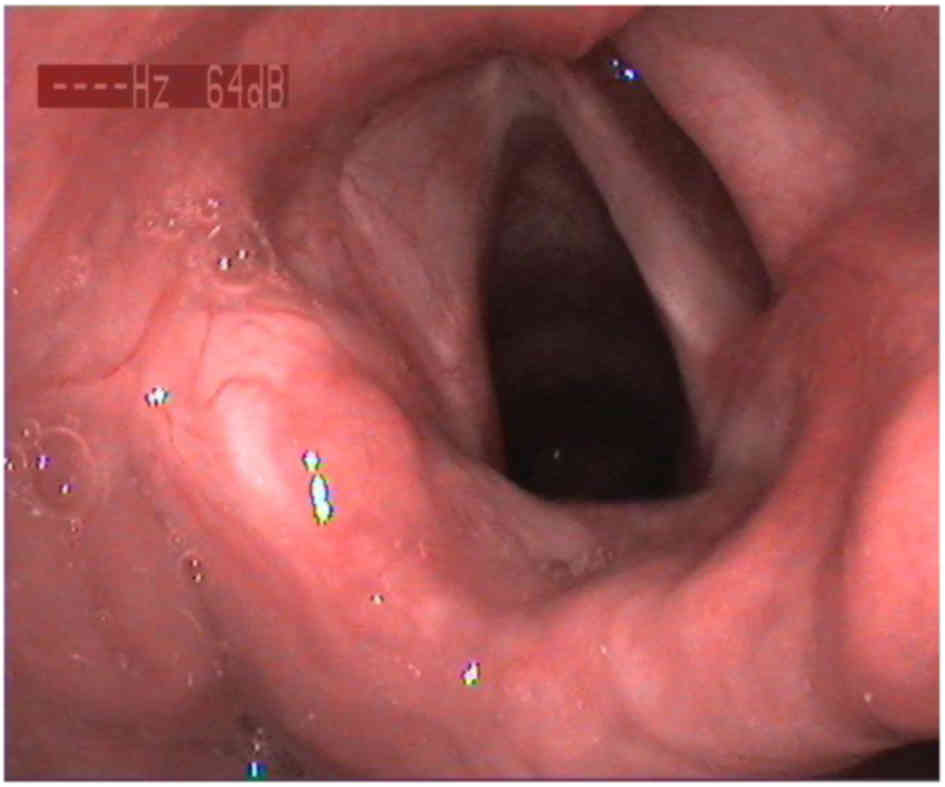
was discharged from hospital 5 days after surgery. During the first
follow-up 2 months after surgery, the patient's supraglottic and
glottic structures were normal, and symmetrical movement of the
vocal folds was observed. The patient's laryngeal cavity was
demonstrated to be sufficiently large, thus the tracheal cannula
was removed and the patient was able to breathe and speak normally
(Fig. 5). The 2-year follow-up
demonstrated that there was no recurrence of the bronchogenic cyst
and that the patient exhibited normal vocal fold mobility. The
patient provided written informed consent for their inclusion in
the present study.
Discussion
Bronchogenic cysts are usually benign congenital
lesions arising from abnormal budding of the ventral foregut, which
forms between the third and sixth weeks of gestation. Although
bronchogenic cysts are primarily located in the trachea and bronchi
(10), they may also occur in other
parts of the body, including the lungs, retroperitoneum,
intrapericardial, anterior cranial fossa and neck (2,11–13). The
first description of a laryngeal cyst was reported by Verneuil in
1852, and Abercrombie reported the next description in 1881
(14). Congenital laryngeal cysts
are rare, occurring in 1.87/100,000 live births (15). Laryngeal cysts are the most common
cysts located on the lingual surface of the epiglottis, followed by
vallecular, ventricular and subglottic cysts (16). Bronchogenic cysts are congenital
lesions that are rarely found in the larynx. Since patients with
bronchogenic cysts do not typically present until the cyst is big
enough to compress surrounding structures and thus cause symptoms,
the true incidence of this type of disease is unknown. The clinical
presentations of bronchogenic cysts vary depending on the location
and size of the mass, and the age of the patient. In the present
study, the patient had progressively worsening hoarseness and
dyspnea because the increasing size of the cyst had caused
compression of the vocal folds and glottis.
The accurate presurgical diagnosis of cysts can be
difficult, and cysts may initially be misdiagnosed by radiologists
and surgeons. The differential diagnosis for bronchogenic cysts
includes congenital laryngeal cartilage dysplasia and pneumonia in
infants, and sebaceous cysts, hemangiomas and solid tumors in
adults. Ribet et al (17)
reviewed the cases of 14 adults with bronchogenic cysts and
identified that the presurgical misdiagnosis rate was 50%. A
combination of flexible laryngoscopy, CT, magnetic resonance
imaging (MRI) and 2-(18F)-fluoro-2-deoxy-D-glucose positron
emission tomography/CT can provide an assessment of the properties
and location of the lesion, the degree of laryngeal constriction
and the association of the lesion with surrounding vital structures
(18). In CT images, bronchogenic
cysts typically manifest as masses of soft tissue or water
attenuation with distinct margins; MRI images can be useful in
revealing the cystic nature of the mass. The majority of
bronchogenic cysts have intermediate to higher signal intensity on
T1-weighted images and characteristically exhibit high signal
intensities on T2-weighted images (19). In the present study, CT images
demonstrated a well-defined cystic lesion and as the cystic lesion
was considered benign an MRI was not performed.
Histopathology is a technique used to aid in the
diagnosis of bronchogenic cysts, which are typically cystic lesions
lined by pseudostratified columnar epithelium, and often contain
cartilage and bronchial mucus glands (20). The cysts are typically filled with
clear fluid, hemorrhagic secretions or air, and occasionally
calcium oxalate crystals are detected in the fluid (21). In the present study, the cyst
contained a clear viscous liquid.
The treatment provided to patients with bronchogenic
cysts is dependent on the location and size of the cyst, and the
degree of respiratory comprise. In the past, a conservative
‘watch-and-wait’ treatment strategy was advocated for asymptomatic
adults or high-risk patients (22);
however, modern studies recommend surgical excision of the cyst to
alleviate airway obstruction, and prevent possible infection
(23), hemorrhage (24) and malignant degeneration (12). Therefore, once a bronchogenic cyst is
suspected, surgical excision should be undertaken, even in an
asymptomatic child (25). However,
it is worth noting that sufficient preparation prior to surgery is
very important for patients. If standard endotracheal intubation
cannot be performed prior to surgery, a tracheotomy is required to
alleviate airway obstruction. During surgery, the blood vessels,
nerves and integrity of the laryngeal mucosa should be protected as
far as possible, to ensure the quality of the patient's voice.
Large obstructing cysts may be removed by the transoral route, but
may require a lateral pharyngotomy or laryngofissure for
excision.
Rather than transoral surgery, a minimally invasive
surgery using a laser and suspension laryngoscope was performed in
the present case to excise the lesion; this was performed for
cosmetic reasons and to protect the vocal function of the patient.
Following complete resection, the prognosis for bronchogenic cysts
is good. However, long-term follow-up remains necessary for such
patients because there are several reports in the literature
indicating the malignant potential of bronchogenic cysts, including
conversion into large cell carcinomas, bronchoalveolar carcinomas,
adenocarcinomas, squamous cell carcinomas and metastasis to the
lymph nodes (12). In the present
case, the lesion was excised and the patient experienced no
complications or recurrence of the bronchogenic cyst 2 year after
surgery.
Acknowledgements
The present study was supported by the Sichuan
Province Science and Technology Development Plan Item (grant nos.
2016FZ0106 and 2012FZ0014).
References
|
1
|
Borges AC, Knebel F, Lembcke A, Panda A,
Komoda T, Hiemann NE, Meyer R, Baumann G and Hetzer R: Bronchogenic
cyst of the interatrial septum presenting as atrioventricular
block. Ann Thorac Surg. 87:1920–1923. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Castro R, Oliveira MI, Fernandes T and
Madureira AJ: Retroperitoneal bronchogenic cyst: MRI findings. Case
Rep Radiol. 2013:8537952013.PubMed/NCBI
|
|
3
|
Goswamy J, de Kruijf S, Humphrey G,
Rothera MP and Bruce IA: Brochogenic cysts as a cause of infantile
stridor: Case report and literature review. J Laryngol Otol.
125:1094–1097. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen YW, Gu DS and Wang TS: One case of
bronchogenic cyst in larynx. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke
Za Zhi. 46:1045–1046. 2011.(In Chinese). PubMed/NCBI
|
|
5
|
Zhou LJ, Zhang TS and Lin JY: A
bronchogenic cyst in larynx: A case report. Chin Arch Otolaryngol
Head Neck Surg. 5:3072003.
|
|
6
|
Williams HJ and Johnson KJ: Imaging of
congenital cystic lung lesions. Paediatr Respir Rev. 3:120–127.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wang LP, Zhang M, Li W, Tian Y, Xue XD and
Wang SX: Etiologic analysis of severe neonatal upper respiratory
tract obstruction. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi.
42:753–756. 2007.(In Chinese). PubMed/NCBI
|
|
8
|
Lepidi H, Casalta JP, Fournier PE, Habib
G, Collard F and Raoult D: Quantitative histologic examination of
mechanical heart valves. Clin Infect Dis. 40:655–661. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lepidi H, Casalta JP, Fournier PE, Habib
G, Collard F and Raoult D: Quantitative histologic examination of
bioprosthetic heart valves. Clin Infect Dis. 42:590–596. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shanmugam G, MacArthur K and Pollock JC:
Congenital lung malformations-antenatal and postnatal evaluation
and management. Eur J Cardiothorac Surg. 27:45–52. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Xu Q, Feng Y, Ye K, Zhou Y and Zhan R:
Bronchogenic cyst in left anterior cranial fossa. Neurology.
84:1181–1182. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jun HH, Kim SM, Lee YS, Hong SW, Chang HS
and Park CS: Cervical bronchogenic cysts mimic metastatic lymph
nodes during thyroid cancer surgery. Ann Surg Treat Res.
86:227–231. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li Z, Wang X, Yang E, Gao K and Huang L:
Gigantic intrapericardial bronchogenic cyst. Heart J.
19:5322011.
|
|
14
|
Lee WS, Tsai CS, Lin CH, Lee CC and Hsu
HT: Airway obstruction caused by a congenital epiglottic cyst. Int
J Pediatr Otorhinolaryngol. 53:229–233. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Pak MW, Woo JK and van Hasselt CA:
Congenital laryngeal cysts: Current approacg to management. J
Laryngol Otol. 110:854–856. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Saha D, Sinha R, Pai RR, Kumar A and
Chakraborti S: Laryngeal cysts in infants and children - a
pathologist's perspective (with review of literature). Int J
Pediatr Otorhinolaryngol. 77:1112–1117. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ribet ME, Copin MC and Gosselin B:
Bronchogenic cysts of the mediastinum. J Thorac Cardiovasc Surg.
109:1003–1110. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yoon YR, Choi J, Lee SM, Kim YJ, Cho HD,
Lee JW and Jeon YS: Retroperitoneal bronchogenic Cyst presenting
paraadrenal tumor incidentally detected by (18)F-FDG PET/CT. Nucl
Med Mol Imagi. 49:69–72. 2015. View Article : Google Scholar
|
|
19
|
Govaerts K, van Eyken P, Verswijvel G and
Van der Speeten K: A bronchogenic cyst, presenting as a
retroperitoneal cystic mass. Rare Tumors. 4:e132012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Liang MK and Marks JL: Congenital
bronchogenic cyst in the gastric mucosa. J Clin Pathol.
58:13442005.PubMed/NCBI
|
|
21
|
McAdams HP, Kirejczyk WM,
Rosado-de-Christenson ML and Matsumoto S: Bronchogenic cyst:
Imaging features with clinical and histopathologic correlation.
Radiology. 217:441–446. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tiwari MK, Yadav R, Mathur RM and
Shrivastava CP: Mediastinal bronchogenic cyst presenting with
dysphagia and back pain. Lung India. 27:86–88. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Hernández-Solís A, Cruz-Ortiz H,
Gutiérrez-Díaz Ceballos ME and Cicero-Sabido R: Bronchogenic cysts.
Importance of the infection in adults. Study of 12 cases. Cir Cir.
83:112–116. 2015.(In Spanis). View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kluger MD, Tayar C, Belli A, Salceda JA,
van Nhieu JT, Luciani A and Cherqui D: A foregut cystic neoplasm
with diagnostic and therapeutic similarities to mucinous cystic
neoplasms of the pancreas. JOP. 14:446–449. 2013.PubMed/NCBI
|
|
25
|
Stewart B, Cochran A, Iglesia K, Speights
VO and Ruff T: Unusual case of stridor and wheeze in an infant:
Tracheal bronchogenic cyst. Pediatr Pulmonol. 34:320–323. 2002.
View Article : Google Scholar : PubMed/NCBI
|