Introduction
Patients with retinal detachment often require
vitrectomies, and silicone oil is a commonly used intraocular
filler (1). However, the long-term
retention of silicone oil may interfere with intraocular energy
metabolism and damage normal ocular tissues, leading to a variety
of complications, including secondary glaucoma, corneal
degeneration and silicone emulsion (2). Secondary glaucoma is a common disease
with an incidence rate as high as 10–40% (3), and its mechanism of incidence and
development are not yet fully understood. Currently, postoperative
inflammation, leakage of silicone oil into the anterior chamber,
silicone emulsion, and other factors are considered as primary
candidates to be involved in the process (4). IL-17 is an inflammation mediator. It
promotes the secretion of inflammatory cytokines, and IL-6 and
TNF-α are both effector molecules of IL-17 (5). The presernt study thus investigated the
roles of IL-17, IL-6 and TNF-α in secondary glaucoma after silicone
oil tamponade.
Patients and methods
Inclusion and exclusion criteria
Inclusion criteria were as follows: i) retinal
detachment patients who previously underwent vitrectomies combined
with silicone oil tamponade currently undergoing silicone oil
removal; ii) patients with unilateral eye lesions; iii) patients
provided informed written consent; and iv) complete medical records
for the patient were available. Exclusion criteria were as follows:
i) patients with primary glaucoma, uveitis, and other autoimmune
eye diseases prior to the silicone oil tamponade; ii) patients with
high blood pressure, diabetes, systemic inflammation, or other
systemic diseases; iii) patients with anterior chamber hyphema
after silicone oil tamponade; iv) patients who had continuously
used glucocorticoids for more than 2 weeks after the silicone oil
tamponade; and v) patients who had systemic trauma.
Diagnostic criteria for secondary
glaucoma
Secondary glaucoma was diagnosed in patients who had
post-tamponade intraocular pressures (IOP) ≥24 mmHg, which was also
≥10 mmHg than their preoperative IOP. In addition, this increase in
IOP had persisted >6 weeks.
General patient information
Fifty-eight patients treated between January 2015
and June 2016 who satisfied the inclusion and exclusion criteria
were included in this study. Patients were divided into observation
and control groups depending on the presence of secondary glaucoma.
The observation group consisted of 19 patients (11 males and 8
females) with postoperative secondary glaucoma aged between 41 to
69 years (mean age, 51.6±8.3 years). The time elapsed between
silicon oil tamponade and silicon oil removal was between 3 to 36
months (average time, 10.8±7.1 months). These patients had elevated
IOPs 2 days to 2.1 years after the surgery, with the maximal IOP
values ranging from 32.1 to 51.4 mmHg (average, 40.6±9.3 mmHg. The
control group consisted of 39 patients (24 males and 15 females)
without secondary glaucoma aged between 40 to 73 years (mean age,
51.1±8.1 years). The time between the silicon oil tamponade and the
removal of silicon oil was between 3 and 32 months (average,
11.5±7.1 months). Maximal IOP values in this group were between
10.7 and 20.2 mmHg (average, 15.3±.1 mmHg). Other than IOP, no
significant differences were observed in any of the general
information criteria between the two groups (P>0.05). This study
was approved by the Ethics Committee of the Fourth Affiliated
Hospital of Nanchang University.
Methods
Routine preoperative ultrasound biomicroscopy (UBM)
and slit lamp examinations, as well as IOP measurements, were
conducted prior to the removal of silicone oil. Before removal,
aqueous humor samples were collected, placed in vials and stored at
−80°C. Enzyme-linked immunosorbent assay (ELISA) was used to detect
IL-17, IL-6 and TNF-α expression levels in aqueous humor samples.
All ELISA kits were purchased from R&D Systems (Minneapolis,
MN, USA). All operations strictly followed the manufacturers
instructions. Optical density (OD) values at 450 nm were detected,
and sample protein concentrations were determined using previously
established protein concentration standard curves.
Statistical analysis
The SPSS 19.0 software (IBM Corp., Armonk, NY, USA)
was used for data processing. Measurement data were expressed as
mean ± standard deviation. Comparisons between the groups were
conducted using independent sample t-test. Correlation analysis was
performed using Pearson correlation analysis. Count data were
converted to proportions, and χ2 test or Fishers exact
probability test were used for comparisons. Receiver operating
characteristic (ROC) curves were used to determine the diagnostic
abilities of IL-17, IL-6 and TNF-α for secondary glaucoma, as well
as to calculate the sensitivity, specificity and other indicators.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Comparisons of the preoperative
examination results of the two groups
UBM examinations revealed that 27 of the 58 patients
(46.6%) had silicone particles in the anterior chamber, 9 (15.5%)
patients had peripheral anterior synechiae and 4 (6.9%) patients
had pupillary block. Slit lamp microscope examinations showed that
17 (29.3%) patients had silicone oil emulsion, 4 (6.9%) patients
had artificial intraocular lens and 7 (12.1%) patients had aphakia.
The incidence of these complications in the observation and control
groups were not significantly different (P>0.05; Table I).
 | Table I.Preoperative examination result
comparison [n (%)]. |
Table I.
Preoperative examination result
comparison [n (%)].
| Group (n) | Silicone particles in
the anterior chamber | Peripheral anterior
synechiae | Pupillary block | Silicone oil
emulsion | Artificial
intraocular lens | Aphakia |
|---|
| Observation (19) | 10 (52.6) | 4 (21.1) | 2 (10.5) | 6 (31.6) | 2 (10.5) | 3 (15.8) |
| Control (39) | 17 (43.6) | 5 (12.8) | 2 (5.1) | 11 (28.2) | 2 (5.1) | 4 (10.3) |
| χ2 | 0.135 | –a | –a | 0.002 | –a | –a |
| P-value | 0.713 | 0.456 | 0.591 | 0.966 | 0.591 | 0.673 |
Comparison of inflammatory mediator
levels in the aqueous humor
The observation group had higher levels of IL-17
(204.2±18.3), IL-6 (351.1±28.4), and TNF-α (850.0±51.7) than those
in the control group (152.3±22.2, 254.4±26.8 and 625.6±61.2)
respectively (P<0.001; Table
II).
 | Table II.Comparison of inflammatory mediator
levels in the aqueous humor (mean ± SD, pg/ml). |
Table II.
Comparison of inflammatory mediator
levels in the aqueous humor (mean ± SD, pg/ml).
| Group (n) | IL-17 | IL-6 | TNF-α |
|---|
| Observation (19) | 204.2±18.3 | 351.1±28.4 | 850.0±51.7 |
| Control (39) | 152.3±22.2 | 254.4±26.8 | 625.6±61.2 |
| t-value | 8.805 | 12.651 | 13.750 |
| P-value | <0.001 | <0.001 | <0.001 |
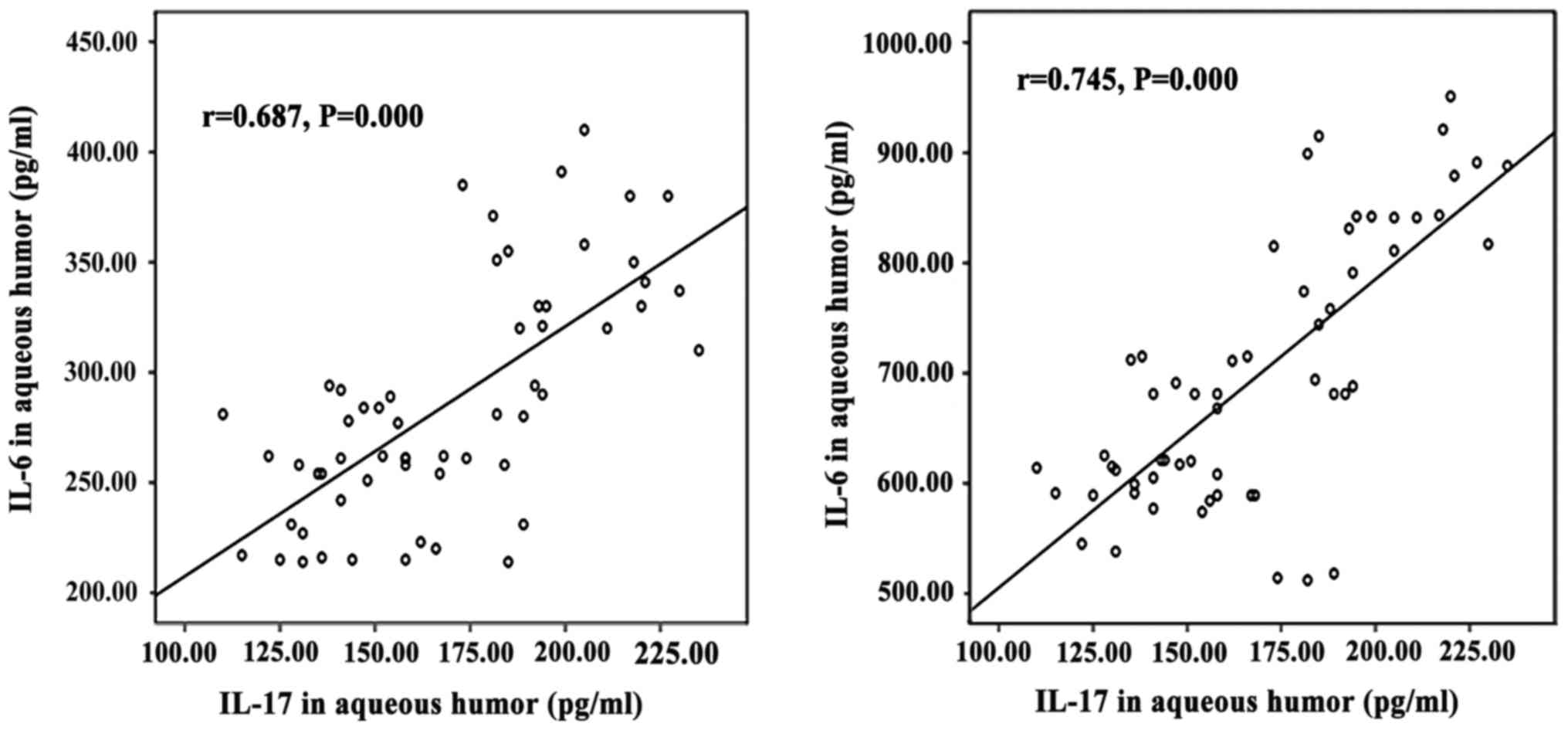
Correlation of IL-17 with IL-6 and
TNF-α
IL-17 levels showed positive correlations with IL-6
(r=0.697; P<0.001) and TNF-α (r=0.745, P<0.001) levels
(Fig. 1).
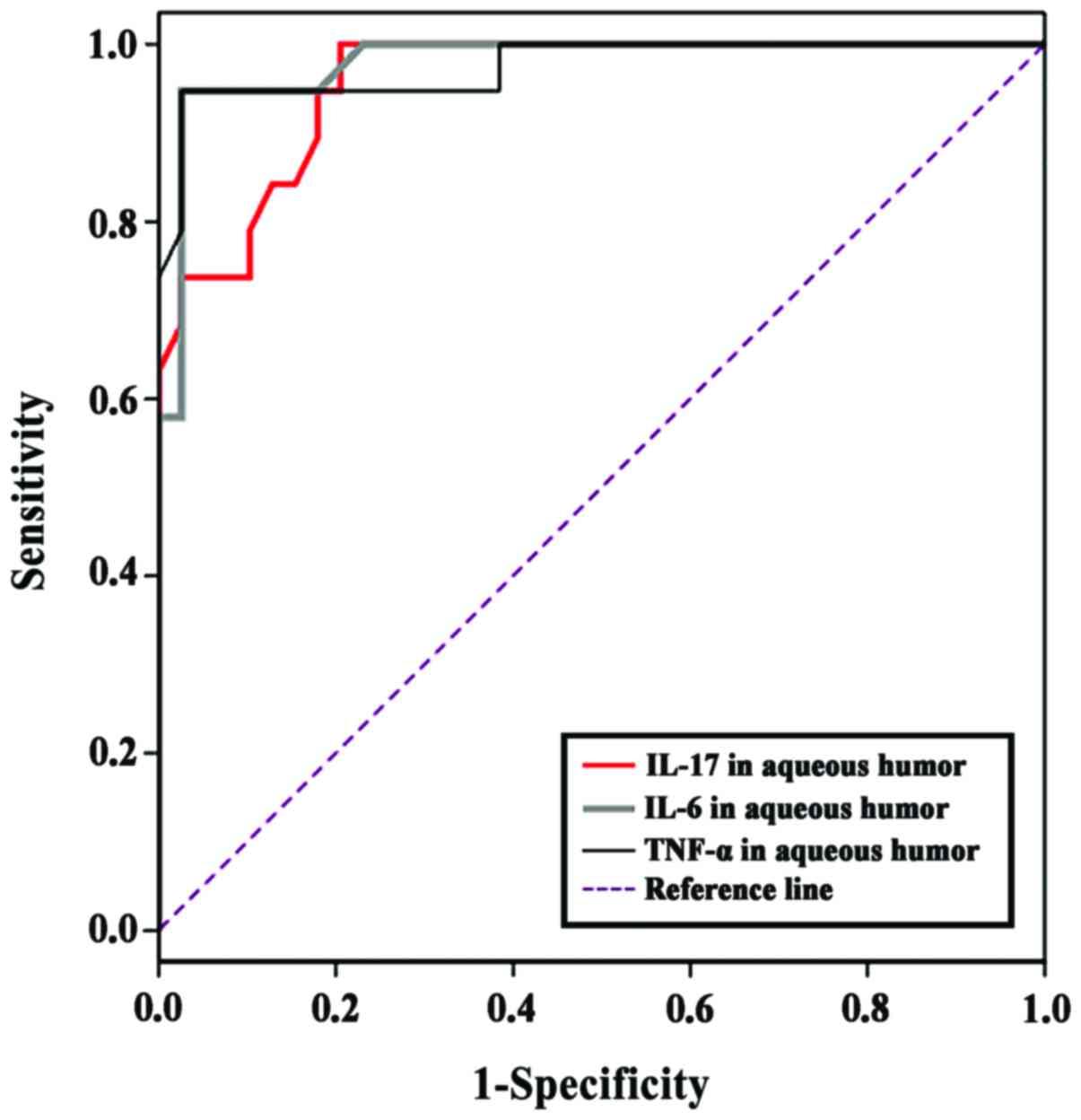
Diagnostic value of aqueous humoral
IL-17, IL-6 and TNF-α levels for secondary glaucoma
ROC curves indicating the diagnostic values of
aqueous humoral IL-17, IL-6 and TNF-α levels for secondary glaucoma
are shown in Fig. 2. The area under
the curve for IL-17 for the prediction of glaucoma was 0.957
(β=0.023, P<0.001, 95% CI, 0.913–1.000). The optimal cut-off
value for the diagnosis of secondary glaucoma was 177.5 pg/ml with
a sensitivity of 1.000 and a specificity of 0.881. The area under
the curve for IL-6 for the prediction of glaucoma was 0.980
(β=0.016, P<0.001, 95% CI, 0.949–1.000). The optimal cut-off
value for the diagnosis of secondary glaucoma was 302.0 pg/ml with
a sensitivity of 0.947 and a specificity of 0.974. The area under
the curve for TNF-α for the prediction of glaucoma was 0.975
(β=0.021, P<0.001, 95% CI, 0.933–1.000). The optimal cut-off
value for the diagnosis of secondary glaucoma was 751.0 pg/ml with
a sensitivity of 0.947 and a specificity of 0.974.
Discussion
Vitreoretinal surgery is an important treatment
method for retinal detachment, retinal vein occlusion and other
diseases (6,7). With the development of medical
technology, its safety has been significantly improved, but
incidences of injected silicone oil-related complications still
exist. Teke et al (8)
reported that 10–40% of patients suffered from secondary glaucoma
after surgery. This may be because the biological functions of
silicone oil could not completely replace those of the vitreous.
Silicone oil filling can potentially impede nutrition exchange
between inner vitreous cells and the vitreous. Also, it cuts off
effective molecular stimuli to the inner cells. Together with
feedback production of harmful substances, these adverse effects of
silicon oil can cause glaucoma, as well as serious and permanent
damage to the optic nerve cells (9–11).
Previous studies have shown that glaucoma-related injuries were
associated with ocular hypertension. However, recent studies have
shown that serious optic nerve damage can also occur in glaucoma
patients without ocular hypertension (12,13),
suggesting that it was difficult to predict secondary glaucoma by
monitoring IOP alone, and that there were other biological
mechanisms causing glaucomatous optic nerve damage. Secondary
glaucoma caused by silicone oil tamponade typically showed
inconsistences between clinical symptoms and IPO values. The
majority of these patients showed no obvious symptoms. Only a small
number of patients had mild swelling and blurred vision when the
IOP was over 40 mmHg. However, physical examination still did not
show conjunctival hyperemia and the pupils often lacked
characteristic signs, making it difficult to predict glaucoma. By
the time the patients first presented obvious symptoms,
irreversible damage had often already occurred (14–17).
This study showed that the observation group and the control group
did not have significant differences regarding incidence of
silicone particles in the anterior chamber, peripheral anterior
synechiae, pupillary block, silicone oil emulsification, artificial
intraocular lens, and aphakia, suggesting the development of other
complications did not increase the risk of secondary glaucoma. This
situation made the early identification and control of secondary
glaucoma more difficult.
Inflammation is one of the mechanisms by which
glaucoma causes damage to the optic nerve cells. Ohira et al
(18) observed that concentrations
of IL-6, IL-8 and TNF-α in the aqueous humor were 171.1, 214.5 and
3.5 pg/ml, respectively, in patients with uveitic glaucoma. These
numbers were significantly higher than those found in people
without glaucoma. Yi et al (19) found elevated levels of IL-6 and VEGF
in the serum and aqueous humor of patients with neovascular
glaucoma. In addition, they noted that ranibizumab could treat
neovascular glaucoma by inhibiting the expression of IL-6 and VEGF.
Based on these findings, we speculated that inflammation was also
involved in the pathogenesis of secondary glaucoma after silicone
oil tamponade. We examined the expression levels of IL-17 and its
effector molecules IL-6 and TNF-α in aqueous humor samples. The
results showed that patients with secondary glaucoma had IL-17
levels of 204.2±18.3 pg/ml, which was significantly higher than in
those without secondary glaucoma (152.3±22.2 pg/ml), suggesting
IL-17 might be involved in the development of secondary glaucoma
after silicone oil tamponade IL-17 is an important inflammatory
mediator involved in the pathogenesis of many diseases, and is the
initial element in inflammatory responses (20). The increased IL-17 in the aqueous
humor of patients with silicone oil tamponade could promote the
aggregation of neutrophils and macrophages, which would lead to
inflammation (21). Neutrophils and
macrophages could worsen inflammation primarily by secreting IL-6,
TNF-α and other factors (22). TNF-α
is directly involved in induction of apoptosis and could destroy
the function of the trabecular cells (23). IL-6 is a pleiotropic factor which can
induce the expression of a variety of inflammatory mediators and
the activation of lymphocytes and NK cells, thus, exacerbating
inflammation (24). This study
showed that the expression of IL-17 was positively correlated with
that of IL-6 and TNF-α, confirming that IL-17 could induce IL-6 and
TNF-α. Also, these results indicated that inflammation was involved
in the optic nerve damage. Understanding the upstream regulatory
mechanisms of glaucoma pathogenesis could aid the development of
targeted treatment plans.
The direct detection of IL-17, IL-6 and TNF-α levels
may also contribute to the ability to diagnose secondary glaucoma
with high sensitivity and specificity, suggesting effective control
of misdiagnosis and missed diagnosis. This finding was consistent
with the conclusion of Qin et al (25). However, it is difficult to prove that
abnormal increases in these indicators could help to predict early
phase secondary glaucoma and guide targeted interventions.
Follow-up studies are needed to answer these questions.
In conclusion, levels of the inflammatory mediators
IL-17, IL-6 and TNF-α were increased in the aqueous humor of
patients with silicone oil tamponade-induced secondary glaucoma,
suggesting the involvement of inflammation in the pathogenesis of
this type of glaucoma. Early monitoring of inflammatory reactions
in patients might help to improve the effective control of
secondary glaucoma.
References
|
1
|
Jančo L, Tkáčová Villemová K, Ondrejková
M, Vida R, Bartoš M and Mesárošová M: Retinal tamponade with
silicone oil - long term results. Cesk Slov Oftalmol. 70:178–182.
2014.(In Czech). PubMed/NCBI
|
|
2
|
Scheerlinck LM, Schellekens PA, Liem AT,
Steijns D and Leeuwen R: Incidence, risk factors, and clinical
characteristics of unexplained visual loss after intraocular
silicon oil for macula-on retinal detachment. Retina. 36:342–350.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Miller JB, Papakostas TD and Vavvas DG:
Complications of emulsified silicone oil after retinal detachment
repair. Semin Ophthalmol. 29:312–318. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zhang Z and Luan J: Clinical observations
of secondary glaucoma post silicone oil tamponade. Chin J Ocul
Fundus Dis. 27:363–365. 2011.
|
|
5
|
Wasilewska A, Winiarska M, Olszewska M and
Rudnicka L: Interleukin-17 inhibitors. A new era in treatment of
psoriasis and other skin diseases. Postepy Dermatol Alergol.
33:247–252. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wang F: Efficacy of selective laser
trabeculoplasty in the treatment of secondary glaucoma eye after
silicone oil tamponade. Chin J Prim Med Pharm. 21:2475–2477.
2014.
|
|
7
|
Dooley IJ, Duignan ES and Kilmartin DJ:
Long-term heavy silicone oil intraocular tamponade. Int Ophthalmol.
36:3–7. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Teke MY, Elgin U, Sen E, Ozdal P and
Ozturk F: Intravitreal silicone oil induced changes in corneal
biomechanics. Int Ophthalmol. 34:457–463. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kong YL, Hu XR, Gao JH and Zheng LD:
Clinical analysis of secondary glaucoma after silicone oil
tamponade. Shanxi Med J. 42:1280–1281. 2013.
|
|
10
|
Gao L and Liu S: Anterior chamber silicone
oil emulsion. Zhonghua Yan Ke Za Zhi. 50:379. 2014.(In
Chinese).
|
|
11
|
Rosca C, Munteanu M, Tamasoi I, Petrovic
Z, Balica N, Nicula C and Cretu O: Calcification of hydrophilic
acrylic intraocular lens in eyes with silicone oil tamponade - an
interventional case series report. Acta Ophthalmol. 94:625–627.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ichhpujani P, Jindal A and Jay Katz L:
Silicone oil induced glaucoma: A review. Graefes Arch Clin Exp
Ophthalmol. 247:1585–1593. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Farrahi F, Feghhi M, Ostadian F and
Alivand A: Pars plana vitrectomy and silicone oil injection in
phakic and pseudophakic eyes; corneal endothelial changes. J
Ophthalmic Vis Res. 9:310–313. 2014.PubMed/NCBI
|
|
14
|
Falavarjani KG, Modarres M and Nazari H:
Therapeutic effect of bevacizumab injected into the silicone oil in
eyes with neovascular glaucoma after vitrectomy for advanced
diabetic retinopathy. Eye (Lond). 24:717–719. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zoric Geber M, Bencic G, Vatavuk Z,
Ivekovic R and Friberg TR: Retinal nerve fibre layer thickness
measurements after successful retinal detachment repair with
silicone oil endotamponade. Br J Ophthalmol. 99:853–858. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Guo XQ, Tian B, Liu ZC, Wei WB, Tao Y, Sun
SJ and Zhang Y: A new rat model of glaucoma induced by intracameral
injection of silicone oil and electrocoagulation of limbal vessels.
Chin Med J (Engl). 124:309–314. 2011.PubMed/NCBI
|
|
17
|
Zhang M, Li B, Wang J, Liu W, Sun Y and Wu
X: Clinical results of selective laser trabeculoplasty in silicone
oil-induced secondary glaucoma. Graefes Arch Clin Exp Ophthalmol.
252:983–987. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ohira S, Inoue T, Iwao K, Takahashi E and
Tanihara H: Factors influencing aqueous proinflammatory cytokines
and growth factors in uveitic glaucoma. PLoS One. 11:e01470802016.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yi Z, Jiang S, Liu T and Du EG: Effects of
ranibizumab on the serum and aqueous humor IL-6 and VEGF in
patients with neovascular glaucoma. Chin J Biol Pharm. 36:151–153.
2016.
|
|
20
|
Guedes MC, Borrego LM and Proença RD:
Roles of interleukin-17 in uveitis. Indian J Ophthalmol.
64:628–634. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Speeckaert R, Lambert J, Grine L, Van Gele
M, De Schepper S and van Geel N: The many faces of interleukin-17
in inflammatory skin diseases. Br J Dermatol. 175:892–901. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Boshtam M, Asgary S, Kouhpayeh S, Shariati
L and Khanahmad H: Aptamers against pro- and anti-inflammatory
cytokines: A review. Inflammation. 40:340–349. 2016. View Article : Google Scholar
|
|
23
|
Bećarević M: TNF-alpha and annexin A2:
Inflammation in thrombotic primary antiphospholipid syndrome.
Rheumatol Int. 36:1649–1656. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kumari N, Dwarakanath BS, Das A and Bhatt
AN: Role of interleukin-6 in cancer progression and therapeutic
resistance. Tumour Biol. 37:11553–11572. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Qin Y, Chen X, Liu J and Dai SY: The
expression of aqueous humor IL-17 in patients with secondary
glaucoma caused by silicon oil tamponade and its relationship with
glaucoma. Chin J Ocul Trauma Occup Eye Dis. 38:365–368. 2016.
|