Introduction
As a common disease in orthopedics, lumbar disc
herniation is a common cause of low back pain (1). Incidence of lumbar disc herniation is
gradually increasing, seriously affecting people's physical and
mental health. Traditional open discectomy is an effective method
for the treatment of lumbar disc herniation. However, this
treatment usually brings relatively large trauma to patients and
may also damage the patient's spinal stability and induce
complications. Thus, the application of this treatment is limited
(2,3). How to reduce surgical trauma, maintain
the integrity and stability of spine and reduce the incidence of
postoperative complications is a difficult point for the treatment
of lumbar disc herniation. With the rapid development of modern
spine surgery technology, percutaneous endoscopic lumbar discectomy
was introduced and has attracted attention (4,5). This
technology has the advantages of small trauma, less blood loss, low
incidence of complications and rapid recovery (6). However, percutaneous endoscopic lumbar
discectomy is still a relatively new technique, and the short-term
and long-term clinical efficacy still need to be further
investigated. Our study aimed to investigate the therapeutic effect
of percutaneous endoscopic lumbar discectomy on lumbar disc
herniation, and to explore its effect on oxidative stress in
patients with lumbar disc herniation, so as to provide valuable
references for the clinical treatment of lumbar disc
herniation.
Patients and methods
General information
A total of 110 patients with lumbar disc herniation
who were treated in the Affiliated People's Hospital of Shanxi
Medical University from May 2015 to May 2016 were selected as
subjects. Inclusion criteria: 1) patients met the diagnostic
criteria of lumbar disc herniation (7); 2) with single segmental lumbar disc
herniation determined by imaging examination, which is consistent
with clinical symptoms; 3) no improvement in symptoms after
conservative treatment for 3 months; 4) without surgery
contraindications. Exclusion criteria: 1) with intervertebral disc
inflammation changes; 2) with recurrent lumbar disc herniation; 3)
with instable lumbar; 4) patients combined with heart, lung, liver
and kidney and other vital organs disease. According to different
surgery strategies, patients were divided into control group (n=50)
and observation group (n=60). In control group, there were 30 males
and 20 females, and the ages ranged from 20 to 65 years with an
average age of 3.67±4.28 years, and the course of disease ranged
from 1 to 9 years with an average course of 5.24±1.74 years. In
observation group, there were 40 males and 20 females, and the ages
ranged from 19 to 64 years with an average age of 52.54±4.12 years,
and the course of disease ranged from 2 to 8 years with an average
course of 5.01±2.32 years. There was no significant difference in
sex, age and course of disease between the two groups (P>0.05).
This study was approved by the Ethics Committee of The Affiliated
People's Hospital of Shanxi Medical University, and all patients
signed written informed consent.
Traditional open discectomy was performed for
patients in control group. An incision was made on the
intervertebral space of the lesion center (6 cm). Supraspinous
ligament and erector spinae muscle were cut in turn to expose
lumbar spine. A window was made by bone rongeur, and fiavum
ligamentum flavum was removed to expose dural sac. Dural sac was
separated to expose prominent discs. Nucleus pulposus of
intervertebral disc was then removed and drainage tube was placed
after surgery.
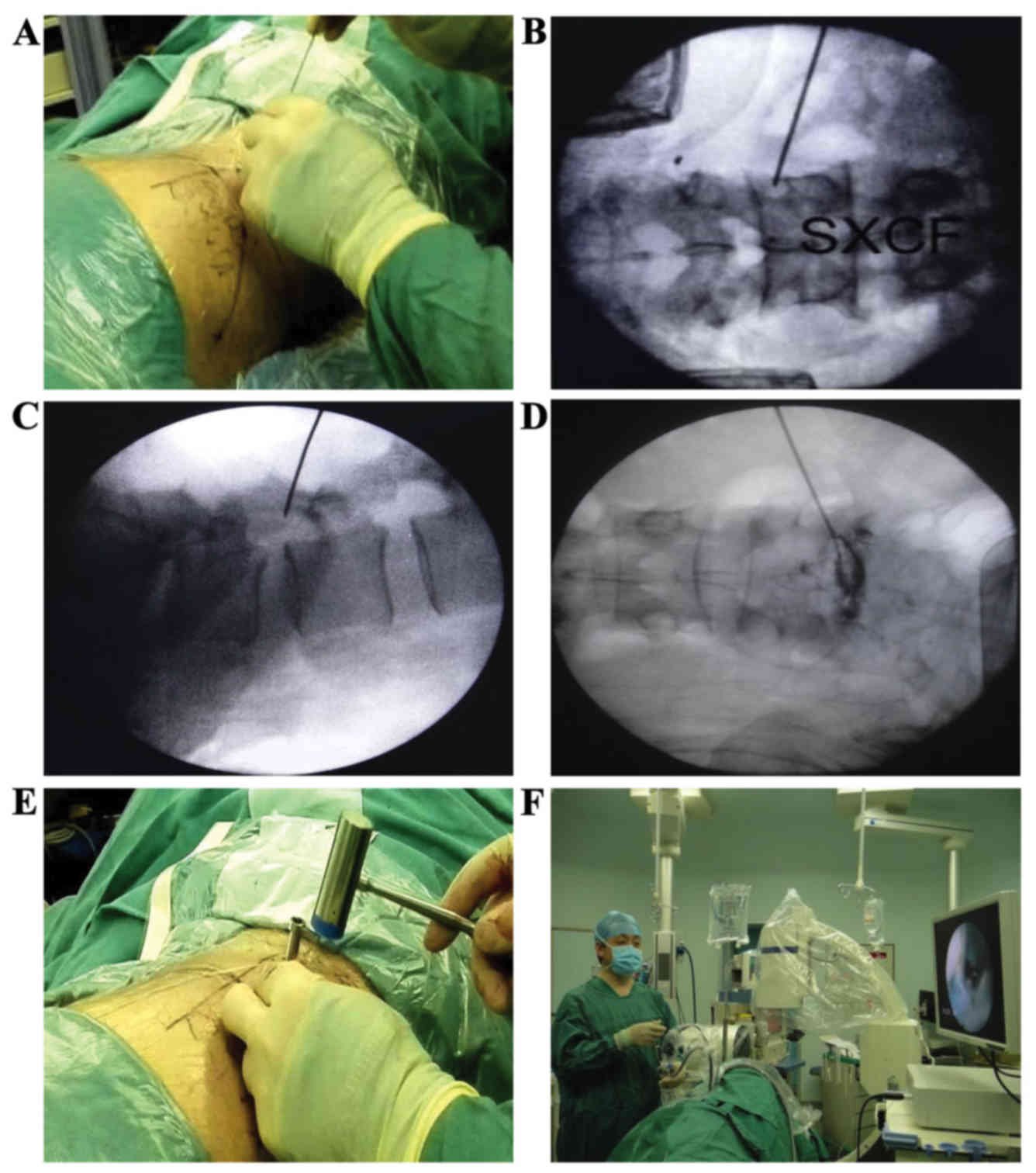
Percutaneous endoscopic lumbar discectomy was
performed for patients in observation group. Lateral position was
taken. After local anesthesia, percutaneous puncture was performed
under the guidance of c-arm, and a guide needle was placed. The
ideal needle point is to locate the lower tip of the needle to the
line connected to the center pedicle of vertebra under positive
perspective and to the line connected to the edge of adjacent
lumbar spines under lateral perspective (Fig. 1A-C). Deformed nucleus pulposus was
subjected to methylene blue staining, and lumbar diskography was
also performed (Fig. 1D). Bone
reamer was used to grind prominent facet joint and to expand
intervertebral foramen (Fig. 1E).
Saline (3,000 ml) was used in full endoscopic discectomy to remove
the nucleus pulposus in spinal canal, outside fibrous ring, the
stained nucleus pulposus was also removed (Fig. 1F). Conditions of fibrosus ring, dural
sac and nerve root were checked. Hemostasis was performed after
cleaning tissue debris, and the incision was sutured.
Observation indicators and evaluation
criteria
i) Surgery related indicators including
intraoperative blood loss, operation time, incision size and
postoperative time of bed rest were recorded. ii) According to
Oswestry disability index (ODI), the disability before and 3 months
after surgery was scored (8) from
the following aspects: social life, standing, walking, degree of
pain and self-dependent ability. Score = actual score/50 (highest
score) ×100%. Lower score indicated better function. iii) According
to the visual analogue scale (VAS), pain of the two groups of
patients was evaluated (9):
painless, 0 points, mild pain, 1–3 points, moderate pain, 4–6
points, severe pain, 7–10 points. iv) Levels of serum tumor
necrosis factor-α (TNF-α) and CRP (C-reactive protein) were
measured before and 3 months after operation. TNF-α level was
determined by double antibody sandwich ELISA method, and CRP level
was determined by latex-enhanced immunoassay. All operations were
performed in strict accordance with the instructions of the kits.
v) Levels of serum malondialdehyde (MDA), myeloperoxidase (MPO),
superoxide dismutase (SOD) and total antioxidant capacity (TAC)
before and 3 months after surgery were compared between groups.
Levels of MDA, MPO, SOD and TAC were measured by double antibody
sandwich ELISA, and all operations were performed in strict
accordance with the instructions of kits.
Statistical analysis
Statistical analysis was performed using SPSS 20.0
(IBM, Armonk, NY, USA). Measurement data were expressed as mean ±
SD, and processed using t-test. Comparisons with groups were
performed by t-test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Comparison of surgery related
indicators between two groups
There was no significant difference in operation
time between the groups. Blood loss, incision size and time of bed
rest in observation group were better than those in control group
(P<0.05) (Table I).
 | Table I.Comparison of surgery related
indicators between two groups (mean ± SD). |
Table I.
Comparison of surgery related
indicators between two groups (mean ± SD).
| Groups | Blood loss (ml) | Operation time
(min) | Incision size
(cm) | Bed rest time
(days) |
|---|
| Observation group
(n=60) | 25.21±9.35 | 75.03±20.21 | 2.10±0.08 | 2.61±1.07 |
| Control group
(n=50) | 52.42±12.74 | 77.95±18.56 | 5.15±0.31 | 6.20±2.44 |
| t-value | 7.451 | 0.126 | 8.735 | 9.307 |
| P-value | <0.05 | >0.05 | <0.05 | <0.05 |
Comparison of ODI scores between two
groups
Compared with preoperative levels, ODI scores of the
groups were significantly decreased, but the decrease in
observation group was higher than that in control group (P<0.05)
(Table II).
 | Table II.Comparison of ODI scores between two
groups (mean ± SD, points). |
Table II.
Comparison of ODI scores between two
groups (mean ± SD, points).
| Groups | n | Preoperative | Postoperative | t-valuea | P-valuea |
|---|
| Observation
group | 60 | 52.16±17.07 | 18.33±9.72 | 12.623 | <0.05 |
| Control group | 50 | 53.28±18.45 | 29.14±11.31 |
9.421 | <0.05 |
| t-valueb |
| 0.007 | 7.523 |
|
|
| P-valueb |
| >0.05 | <0.05 |
|
|
Comparison of VAS scores between two
groups
VAS scores of the groups were significantly
decreased after operation, but the decrease in observation group
was higher than that in control group (P<0.05) (Table III).
 | Table III.Comparison of VAS scores between two
groups (mean ± SD, points). |
Table III.
Comparison of VAS scores between two
groups (mean ± SD, points).
| Groups | n | Preoperative | Postoperative | t-valuea | P-valuea |
|---|
| Observation
group | 60 | 7.96±2.44 | 2.21±1.57 | 8.254 | <0.05 |
| Control group | 50 | 7.99±2.57 | 4.82±2.31 | 4.017 | <0.05 |
| t-valueb |
| 0.115 | 8.925 |
|
|
| P-valueb |
| >0.05 | <0.05 |
|
|
Comparison of changes in serum
inflammatory factors between two groups
There was no significant difference in serum TNF-α
and CRP between the groups before surgery (P>0.05). Levels of
serum TNF-α and CRP in observation group were significantly lower
than those in control group (P<0.05) (Table IV).
 | Table IV.Comparison of serum TNF-α and CRP
levels between groups (mean ± SD). |
Table IV.
Comparison of serum TNF-α and CRP
levels between groups (mean ± SD).
|
|
| TNF-α (µg/l) | CRP (mg/l) |
|---|
|
|
|
|
|
|---|
| Groups | n | Preoperative | Postoperative | Preoperative | Postoperative |
|---|
| Observation
group | 60 | 27.11±3.26 | 3.21±0.45 | 28.34±4.18 | 3.54±0.32 |
| Control group | 50 | 27.26±3.15 | 5.78±0.67 | 28.45±4.35 | 6.68±0.58 |
| t-value |
| 0.258 | 8.021 | 0.306 | 8.935 |
| P-value |
| >0.05 | <0.05 | >0.05 | <0.05 |
Comparison of changes in serum
oxidative stress indicator between two groups
There were no significant differences in serum MDA,
MPO, SOD and TAC levels between the groups preoperatively
(P>0.05). Postoperative levels of serum MDA and MPO were
significantly lower and levels of SOD and TAC were significantly
higher in observation group than in control group (P<0.05)
(Table V).
 | Table V.Comparison of changes in serum
oxidative stress indicator between two groups (mean ± SD). |
Table V.
Comparison of changes in serum
oxidative stress indicator between two groups (mean ± SD).
|
|
| MDA (nmol/l) | MPO (mg/l) | SOD (nU/ml) | TAC (kU/l) |
|---|
|
|
|
|
|
|
|
|---|
| Groups | n | Preoperative | Postoperative | Preoperative | Postoperative | Preoperative | Postoperative | Preoperative | Postoperative |
|---|
| Observation
group | 60 | 4.65±0.27 | 1.34±0.32 | 2.83±0.34 | 0.82±0.14 | 54.78±3.42 | 76.15±4.77 | 6.03±1.26 | 9.81±1.75 |
| Control group | 50 | 4.73±0.29 | 2.56±0.45 | 2.91±0.37 | 1.35±0.22 | 54.83±3.65 | 63.86±5.74 | 6.12±1.33 | 8.43±1.61 |
| t-value |
| 0.108 | 6.735 | 0.275 | 6.072 | 0.204 | 7.155 | 0.014 | 8.826 |
| P-value |
| >0.05 | <0.05 | >0.05 | <0.05 | >0.05 | <0.05 | >0.05 | <0.05 |
Discussion
Lumbar disc herniation is a common orthopedic
disease. Open discectomy is used as the main treatment of lumbar
disc herniation, but the application of open discectomy is limited
by the big surgical trauma and the incidence of postoperative
complications including adhesions of nerve roots and lumbar
instability (10). In order to
reduce the damage of normal tissue caused by surgical operations
and the incidence of postoperative complications, percutaneous
endoscopic lumbar discectomy has been widely applied and is
attracting increased attention. In this study, 110 cases of lumbar
disc herniation were selected for different surgical treatment to
further evaluate the effectiveness and reliability of percutaneous
endoscopic lumbar discectomy.
Results of this study showed that blood loss,
incision size and time of bed rest were better in observation group
than in the control group. Compared with preoperative levels, ODI
and VAS scores of the two groups were significantly decreased, but
the decreases in observation group was lower than those in control
group. This finding is consistent with the results of Mroz et
al (11), indicating that
treatment of lumbar disc herniation with percutaneous endoscopic
lumbar discectomy can avoid large surgical trauma, reduce blood
loss, promote postoperative recovery, shorten hospitalization and
reduce economic burden of patients' families. The possible
explanations may be that the working channel in percutaneous
endoscopic lumbar discectomy can be used to directly access the
prominent disc to remove the nucleus pulposus, so as to directly
cut the prominent part. Moreover, the targeting is more accurate,
so nerve root will be decompressed directly (12–14).
Local anesthesia was used in percutaneous endoscopic lumbar
discectomy, which avoided the risk of general anesthesia and reduce
the probability of nerve root damage. At the same time, lumbar
facet joints and neural scute were not cut, which in turn avoided
the damage of adjacent paravertebral ligament and muscle. The
effect on spinal canal and nerve structure was not strong, and scar
tissue would not form in spinal canal (8,15,16). The
surgical incision was small, which brought less pain to patients.
Washing with saline performed during surgery could remove
inflammatory mediators and prevent the accumulation of by-products.
Thus, postoperative pain and the incidence of postoperative
infection were reduced (1,17,18).
TNF-α and CRP are common serum inflammatory factors,
and serum contents of TNF-α and CRP can reflect patient's recovery
condition (19). Results of this
study showed that there was no significant difference in serum
levels of TNF-α and CRP between the groups before surgery
(P>0.05), while serum levels of TNF-α and CRP were significantly
lower in observation group than in control group postoperatively
(P<0.05). The data suggest that the application of percutaneous
endoscopic lumbar discectomy can effectively reduce the serum
contents of TNF-α and CRP, which maybe the pathophysiological basis
of the advantages of this technique in the treatment of lumbar disc
herniation.
Studies have shown that oxidative stress indicators
would change after damage (20).
Thus, the recovery can be evaluated by the changes in oxidative
stress indicators. Results of this study showed that there was no
significant difference in serum MDA, MPO, SOD and TAC between two
groups before surgery (P>0.05), while serum levels of MDA and
MPO were significantly lower and serum levels of SOD and TAC were
significantly higher in observation group than in control group
postoperatively (P<0.05). Those data suggest that the
application of percutaneous endoscopic lumbar discectomy can
effectively improve oxidative stress. This study is still limited
by the environment, small sample size and time of clinical
observation. Further studies are still needed to investigate the
long-term effects of this method.
In summary, treatment of lumbar disc herniation by
percutaneous endoscopic lumbar discectomy has the advantages of
small trauma, less blood loss and rapid postoperative recovery.
This method can effectively improve dysfunction, reduce pain and
serum levels of inflammatory factors, and improve oxidative stress,
thereby improving the surgical results. Thus, this technique should
be popularized in clinical practice.
References
|
1
|
Zheng C, Wu F and Cai L: Transforaminal
percutaneous endoscopic discectomy in the treatment of far-lateral
lumbar disc herniations in children. Int Orthop. 40:1099–1102.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Karamouzian S, Ebrahimi-Nejad A,
Shahsavarani S, Keikhosravi E, Shahba M and Ebrahimi F: Comparison
of two methods of epidural steroid injection in the treatment of
recurrent lumbar disc herniation. Asian Spine J. 8:646–652. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cong L, Zhu Y and Tu G: A meta-analysis of
endoscopic discectomy versus open discectomy for symptomatic lumbar
disk herniation. Eur Spine J. 25:134–143. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jha SC, Tonogai I, Takata Y, Sakai T,
Higashino K, Matsuura T, Suzue N, Hamada D, Goto T, Nishisho T, et
al: Percutaneous endoscopic lumbar discectomy for a huge herniated
disc causing acute cauda equina syndrome: A case report. J Med
Invest. 62:100–102. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wang SJ, Chen BH, Wang P, Liu CS, Yu JM
and Ma XX: The effect of percutaneous endoscopic lumbar discectomy
under different anesthesia on pain and immunity of patients with
prolapse of lumbar intervertebral disc. Eur Rev Med Pharmacol Sci.
21:2793–2799. 2017.PubMed/NCBI
|
|
6
|
Löhr M, Lebenheim L, Berg F, Stenzel W,
Hescheler J, Molcanyi M, Ernestus RI and Bosche B: Gadolinium
enhancement in newly diagnosed patients with lumbar disc
herniations are associated with inflammatory peridiscal tissue
reactions – evidence of fragment degradation? Clin Neurol
Neurosurg. 119:28–34. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dalbayrak S, Yaman O, Yilmaz M and Özer
AF: Transforaminal approach in lumbar disc herniations:
Transforaminal microdiscectomy (TFMD) technique. Turk Neurosurg.
25:29–35. 2015.PubMed/NCBI
|
|
8
|
Li X, Dou Q, Hu S, Liu J, Kong Q, Zeng J
and Song Y: Treatment of cauda equina syndrome caused by lumbar
disc herniation with percutaneous endoscopic lumbar discectomy.
Acta Neurol Belg. 116:185–190. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kogias E, Franco Jimenez P, Klingler JH
and Hubbe U: Minimally invasive redo discectomy for recurrent
lumbar disc herniations. J Clin Neurosci. 22:1382–1386. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gotecha S, Ranade D, Patil SV, Chugh A,
Kotecha M, Sharma S and Punia P: The role of transforaminal
percutaneous endoscopic discectomy in lumbar disc herniations. J
Craniovertebr Junction Spine. 7:217–223. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mroz TE, Lubelski D, Williams SK, O'Rourke
C, Obuchowski NA, Wang JC, Steinmetz MP, Melillo AJ, Benzel EC,
Modic MT, et al: Differences in the surgical treatment of recurrent
lumbar disc herniation among spine surgeons in the United States.
Spine J. 14:2334–2343. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jang JS, An SH and Lee SH: Transforaminal
percutaneous endoscopic discectomy in the treatment of foraminal
and extraforaminal lumbar disc herniations. J Spinal Disord Tech.
19:338–343. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kamper SJ, Ostelo RW, Rubinstein SM,
Nellensteijn JM, Peul WC, Arts MP and van Tulder MW: Minimally
invasive surgery for lumbar disc herniation: A systematic review
and meta-analysis. Eur Spine J. 23:1021–1043. 2014.PubMed/NCBI
|
|
14
|
Kerr D, Zhao W and Lurie JD: What are
long-term predictors of outcomes for lumbar disc herniation? A
randomized and observational study. Clin Orthop Relat Res.
473:1920–1930. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Golinvaux NS, Bohl DD, Basques BA, Yacob A
and Grauer JN: Comparison of the lumbar disc herniation patients
randomized in SPORT to 6,846 discectomy patients from NSQIP:
Demographics, perioperative variables, and complications correlate
well. Spine J. 15:685–691. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yoshimoto M, Iwase T, Takebayashi T, Ida K
and Yamashita T: Microendoscopic discectomy for far lateral lumbar
disk herniation: Less surgical invasiveness and minimum 2-year
follow-up results. J Spinal Disord Tech. 27:E1–E7. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Yamashita K, Higashino K, Sakai T, Takata
Y, Abe M, Morimoto M, Nagamachi A and Sairyo K: Revision
percutaneous endoscopic lumbar discectomy under the local
anesthesia for the recurrent lumbar herniated nucleus pulposus in a
high class athlete: A Case Report. J Med Invest. 63:135–139. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kapetanakis S, Giovannopoulou E,
Charitoudis G and Kazakos K: Transforaminal percutaneous endoscopic
discectomy for lumbar disc herniation in Parkinson's disease: A
Case-Control Study. Asian Spine J. 10:671–677. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Strömqvist F, Strömqvist B, Jönsson B and
Karlsson MK: Gender differences in patients scheduled for lumbar
disc herniation surgery: A National Register Study including 15,631
operations. Eur Spine J. 25:162–167. 2016. View Article : Google Scholar
|
|
20
|
Motor S, Ozturk S, Ozcan O, Gurpinar AB,
Can Y, Yuksel R, Yenin JZ, Seraslan G and Ozturk OH: Evaluation of
total antioxidant status, total oxidant status and oxidative stress
index in patients with alopecia areata. Int J Clin Exp Med.
7:1089–1093. 2014.PubMed/NCBI
|