Introduction
Osteoarthritis is a degenerative disease affecting
the joints caused by multiple factors. Osteoarthritis is mainly
featured by progressive articular cartilage injury, subchondral
bone sclerosis, and formation of osteophyte around the joints;
arthralgia (pain in the joint) is the most typical clinical
manifestation (1–3). In clinical practice, osteoarthritis is
treated mainly by relieving the symptoms and improving joint
function with the main objective of improving quality of life. In
most cases, patients with end-stage knee osteoarthritis can only
get effective treatment through joint replacement surgery, but the
surgery has important risks, including large trauma, high costs and
high failure rates. Therefore, it is crucial to find effective
methods for early diagnosis of osteoarthritis that can prevent
further degeneration that lead to surgery (4–6). Knee
osteoarthritis (KOA) is a common form of osteoarthritis that is the
most extensively studied at present. Much attention has been paid
to the role of tissue inhibitor of metalloproteinases (TIMP) in KOA
in recent years. TIMP-1 is a new member of the TIMP family widely
distributed that inhibits specific matrix metalloproteases (MMPs)
wiht a crucial role in the occurrence and development of KOA
(7). B-cell lymphoma/leukemia-2
(Bcl-2) is an anti-apoptotic protein that promotes cell survival by
inhibiting apoptosis. Studies report that the expression level of
Bcl-2 may influence the occurrence and development of arthritis
(8).
Here, we explored the relationship between the
expression levels of TIMP-1 and Bcl-2 in synovial tissues and the
clinicopathologic characteristics of KOA, hoping to provide new
insights for the early diagnosis of KOA.
Subjects and methods
Research subjects
We enrolled 70 patients who came for medical
consultation, received treatment, and were diagnosed with KOA by
experts in Renji Hospital from August, 2014 to August, 2015.
Patients were aged 45–87 years, including 32 men and 30 women.
Patients were not affected by other degenerative conditions. We
completed clinical and pathological data for all patients as well
as treatment protocols. The control group consisted of 30 healthy
people who received physical examination, in which arthritis and
other degenerative diseases were excluded. The diagnosis of KOA was
done according to the KOA diagnostic criteria recommended by the
American College of Rheumatology in 2000 (9). Severity classification of KOA was
performed according to Lawrence radiographic grading criteria
(10): mild (joint space ≥7 mm, with
formation of osteophyte in the joint space), moderate (joint space
at 4–7 mm, with obvious osteophyte formed), and severe (joint space
disappeared, with massive osteophyte). All patients signed informed
consent before enrolling in the study. The study was approved by
the Ethics Committee of Ren Ji Hospital, School of Medicine,
Shanghai Jiao Tong University.
Collection and preservation of
synovial fluid
For collection of synovial fluid in knee joint, the
patient was placed in the supine position with the knee extended.
The puncture point was located at the junction of the lateral edge
of the quadriceps femoris muscle and the line joining the superior
edge of the patella. Synovial fluid (0.5–2 ml) was withdrawn from
the knee joint and collected in a tube with heparin. The synovial
fluid was snap-frozen after it was centrifuged within 2 h and then
it was placed at −80°C for long-term storage.
Semi-quantitative reverse
transcriptase PCR (RT-PCR)
Total RNA in the synovial fluids was extracted
according to the instructions of the TRIzol kit (Invitrogen,
Carlsbad, CA, USA). Agarose gel electrophoresis was used to confirm
RNA integrity. The 28S, 18S and 5S bands were clear and the 28S
band was twice as bright as the 18S band, indicating that the RNA
could be used in subsequent experiments. The RNA was reversely
transcribed into cDNA with the reverse transcription kit
(Invitrogen). The expression levels of TIMP-1 and
Bcl-2 mRNA were detected by semi-quantitative PCR (Thermo
Fisher Scientific GmbH, Dreieich, Germany) from synovial fluids of
KOA patients and controls, using glyceraldehyde 3-phosphate
dehydrogenase (GAPDH) as internal control. Reaction
conditions: 35 cycles of 30 sec at 95°C, 25 sec at 64°C and 30 sec
at 72°C. Primers were synthesized by Tiangen Biotech (Beijing,
China) (Table I). When the reaction
was completed, they were observed under the ultraviolet imaging
system (Biometra GmbH, Göttingen, Germany) after agarose gel
electrophoresis, and the relative expression of TIMP-1 and
Bcl-2 were presented normalized to GAPDH.
 | Table I.Sequence of PCR primers. |
Table I.
Sequence of PCR primers.
| Gene | Primer sequences |
|---|
| TIMP-1 | F:
5′-ATCCACCTTGACGATGCTTTAC-3′ |
|
| R:
5′-TTCAGATGTTCTAAGCCTACGG-3′ |
| Bcl-2 | F:
5′-TGGCCCTCGTAGCCTTGAGGAC-3′ |
|
| R:
5′-CCAGTGCTGCAGGGTCCGAGGT-3′ |
| GAPDH | F:
5′-GATGATTGGCATGGCTTT-3′ |
|
| R:
5′-CACCTTCCGTTCCAGTTT-3′ |
Enzyme-linked immunosorbent assay
(ELISA)
Hydrochloric acid (HCL) (0.1 mmol) was added to
synovial fluids at 1:5 (w:v). The synovial fluids were sonicated
with ultrasonic waves and then centrifuged at 1,000 × g for 15 min
at 4°C (ABI, Carlsbad, CA, USA). The precipitate was discarded and
the supernatant was collected. The pH of the fluid was adjusted to
7.0 using 1 mmol sodium hydroxide. The expression levels of TIMP-1
and Bcl-2 proteins were measured according to the instructions of
ELISA kit (R&D Systems, Minneapolis, MN, USA), the absorbance
of the samples was measured with a microplate reader (Thermo Fisher
Scientific GmbH), and the contents of TIMP-1 and Bcl-2 in each
group of samples were calculated.
Statistical analysis
Data were presented as mean ± standard deviation.
SPSS 19.0 software was used for data processing and analysis (SPSS,
Chicago, IL, USA). t-test was used for measurement data and
χ2 test was used to analyze enumeration data groups.
Homogeneity of variance test was performed; if there was
homogeneity of variance, the Bonferroni method was used for
pairwise comparison. If there was heterogeneity of variance, the
Welch method was be used for analysis. Dunnetts T3 method was used
for multiple comparisons and Pearsons correlation analysis was used
for correlation analysis. P<0.05 suggested that the difference
was statistically significant.
Results
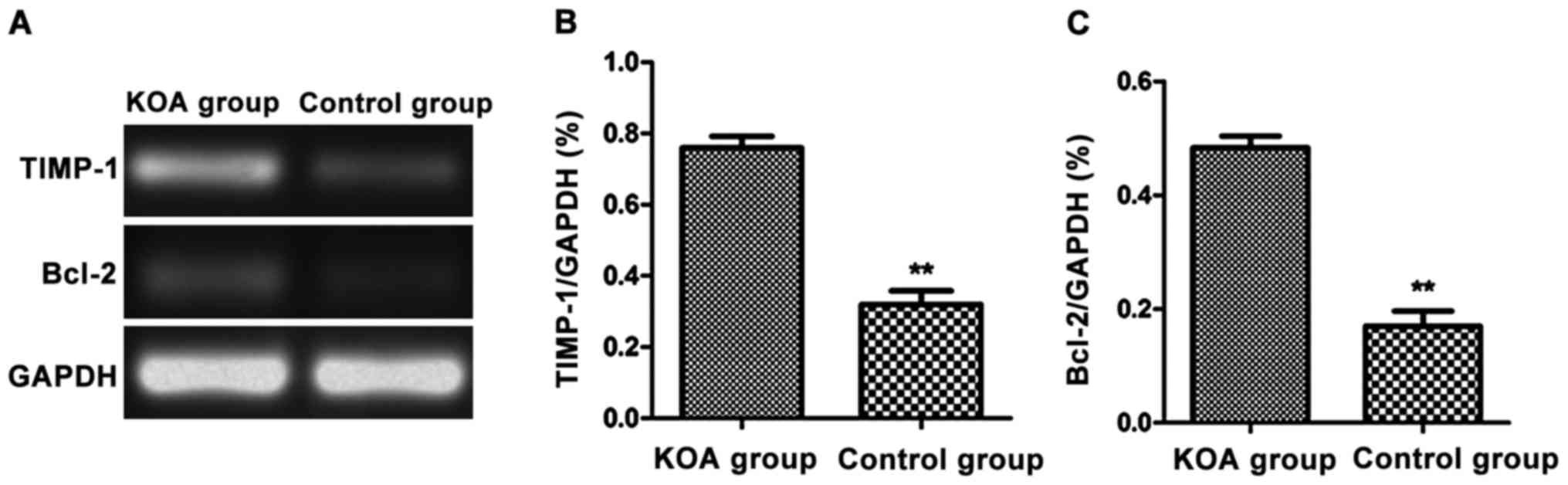
Expression of TIMP-1 and Bcl-2 mRNA in
synovial membranes in KOA
We used the synovial fluids from KOA patients and
normal controls to analyze the expression level of TIMP-1
and Bcl-2 mRNA via semi-quantitative RT-PCR. The relative
expression of TIMP-1 and Bcl-2 were significantly
increased in the synovial fluids of KOA patients compared with
those in the control group (P<0.01) (Fig. 1).
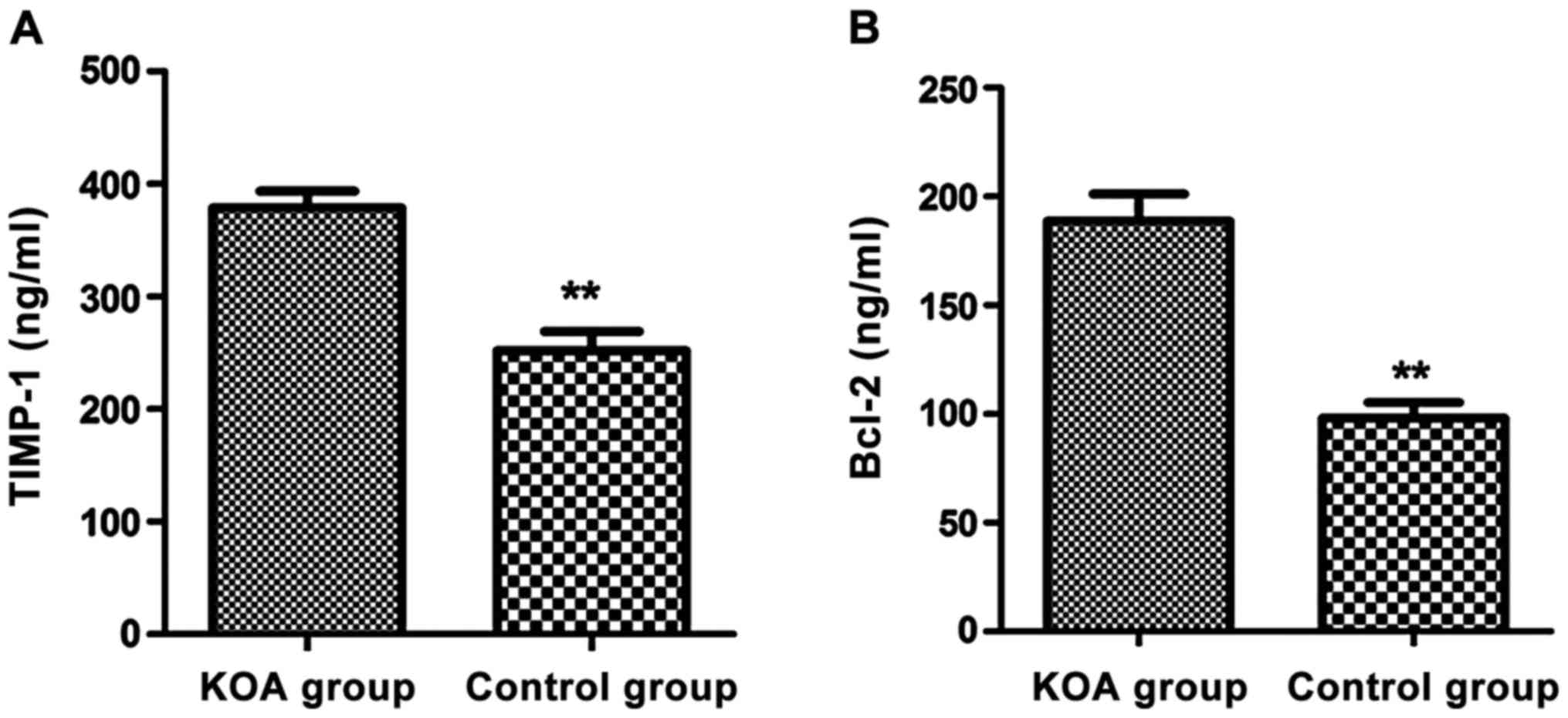
Expression of TIMP-1 and Bcl-2 protein
in synovial membranes in KOA
We next used the synovial fluids from KOA patients
and normal controls to analyze the expression level of TIMP-1 and
Bcl-2 proteins by ELISA. The relative expression of TIMP-1 and
Bcl-2 were significantly increased in the synovial fluids of KOA
patients compared with those in the control group (P<0.01)
(Fig. 2).
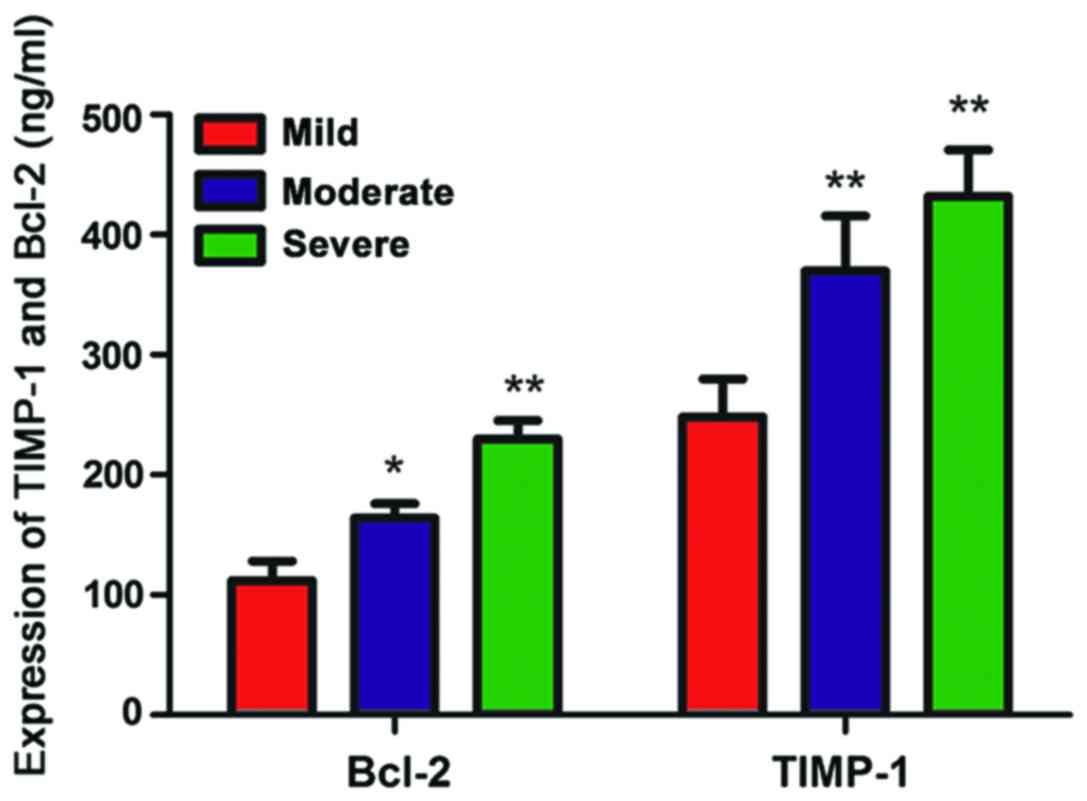
Expressions of TIMP-1 and Bcl-2 and
clinico-pathology
Next, we analyzed the expression of TIMP-1 and Bcl-2
in the synovial tissues of KOA patients in combination with age,
sex, and the severity and relapse of KOA. The relative expression
of TIMP-1 and Bcl-2 were not correlated with the age and sex of
patients (Table II). However, they
were closely related to the severity and relapse of KOA (Table II). The relationship between the
severity of KOA and the expression levels of TIMP-1 and Bcl-2 is
shown in Fig. 3.
 | Table II.Relationship between relative
expression of MMP-2 and TIMP-3 and clinical characteristics. |
Table II.
Relationship between relative
expression of MMP-2 and TIMP-3 and clinical characteristics.
| Category | n | Expression of TIMP-1
(ng/ml) | P-value | Expression of Bcl-2
(ng/ml) | P-value |
|---|
| Age (years) |
| ≤60 | 34 |
373.58±56.33 | 0.0692 |
185.53±21.08 | 0.0782 |
|
>60 | 36 |
364.16±49.28 |
|
176.85±19.12 |
|
| Sex |
| Male | 32 |
367.52±53.08 | 0.0719 |
164.63±33.62 | 0.0873 |
|
Female | 38 |
353.96±61.22 |
|
172.57±25.29 |
|
| Severity of KOA |
| Mild | 13 |
248.26±31.39 | 0.012 |
112.08±16.19 | 0.021 |
|
Moderate | 32 |
369.89±45.87 |
|
163.95±12.01 |
|
|
Severe | 35 |
431.86±38.65 |
|
229.72±15.32 |
|
| Relapse |
| Yes | 28 |
375.68±29.86 | 0.026 |
201.87±11.37 | 0.0085 |
| No | 42 |
304.52±25.36 |
|
115.96±16.69 |
|
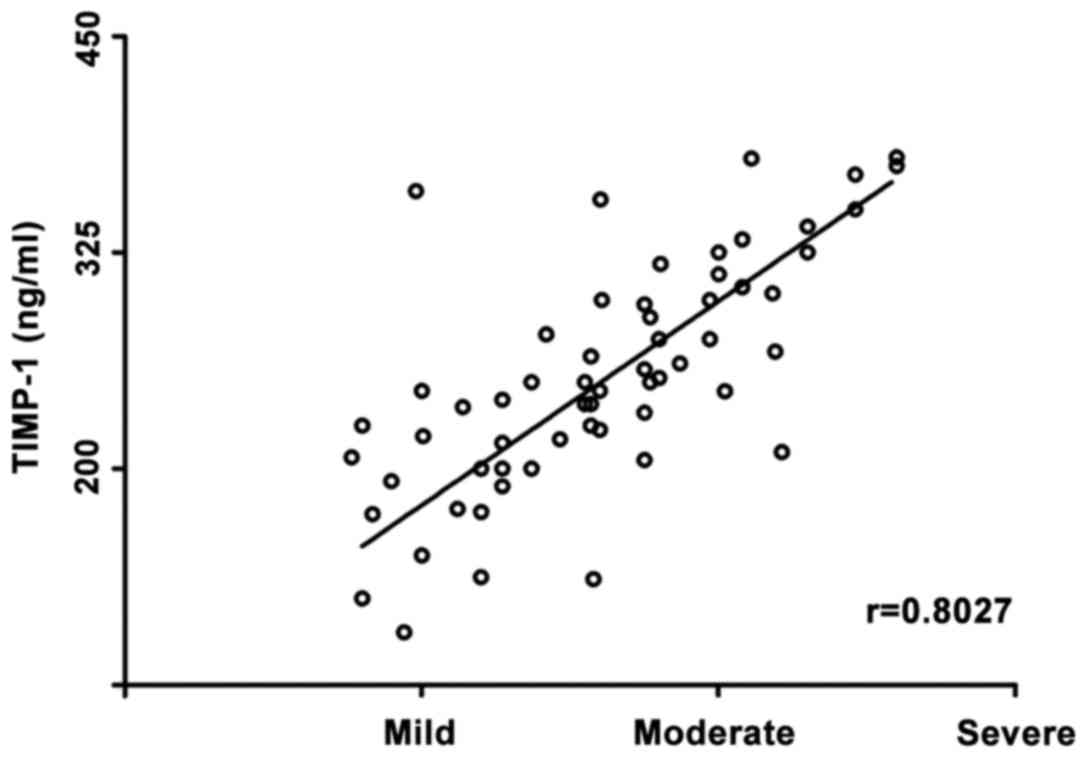
Correlation between expression levels
of TIMP-1 and Bcl-2 and KOA
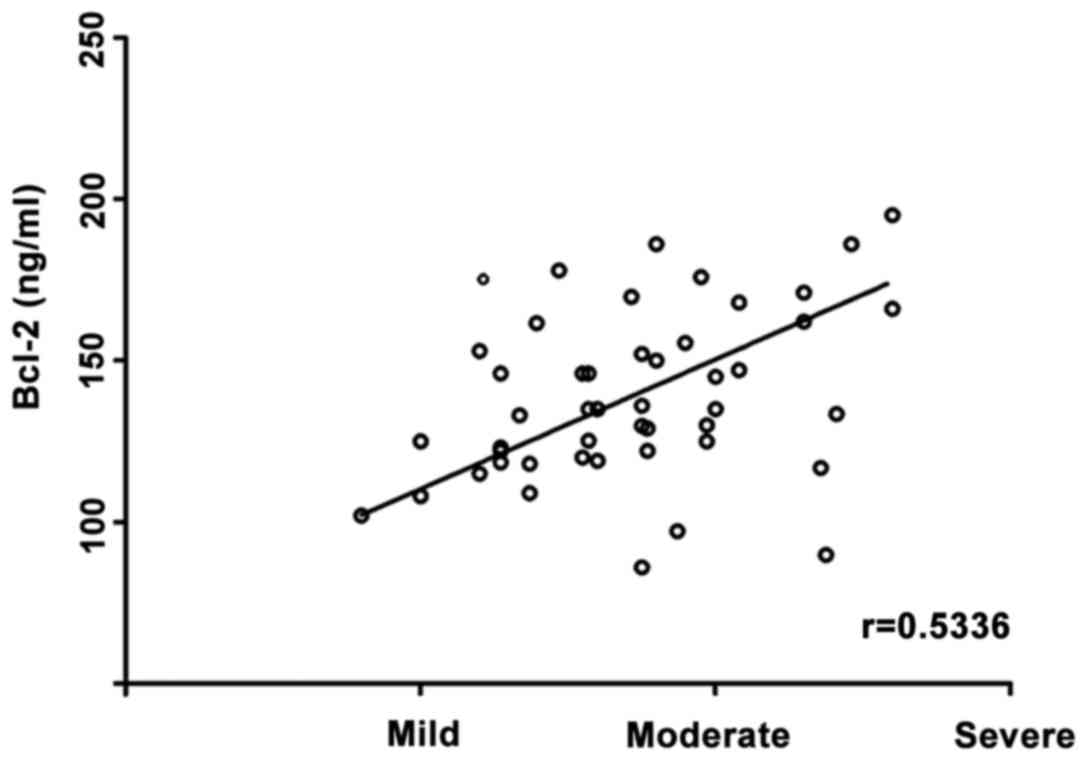
We next performed Pearson's correlation analysis to
analyze the relationship between the expression levels of TIMP-1
and Bcl-2 and the severity of KOA. The expression level of TIMP-1
was positively correlated with the severity of KOA (r=0.8027,
P<0.05) (Fig. 4). The expression
level of Bcl-2 was also positively correlated with the severity of
KOA (r=0.5336, P<0.05) (Fig.
5).
Statistical analysis was performed on the expression
levels of TIMP-1 and Bcl-2 in the synovial tissues of KOA patients.
When the expression level was higher in KAO patients than that of
controls, it was considered as high expression. If expression in
KAO patients was equal to or lower than that of controls, it was
considered normal or low expression. The expression levels of
TIMP-1 and Bcl-2 in the synovial tissues of KOA patients were not
mutually correlated (r=−0.658, P>0.05) (Table III).
 | Table III.Correlation between expressions of
MMP-2 and TIMP-3 in KOA. |
Table III.
Correlation between expressions of
MMP-2 and TIMP-3 in KOA.
|
| TIMP-1 |
|
|
|---|
|
|
|
|
|
|---|
| Bcl-2 | High expression | Normal or low
expression | r-value | P-value |
|---|
| High expression | 12 | 58 | −0.658 | 0.081 |
| Normal expression or
low expression | 49 | 21 |
|
|
Discussion
The onset of KOA is a dynamic, progressive process
in which subchondral bone and articular cartilage influence each
other. The pathogenesis of KOA often leads to changes in stress
stimulation of subchondral bone on articular cartilage and,
eventually, causes destruction of articular cartilage, inducing the
onset of osteoarthritis (11).
Currently the diagnosis for KOA is fairly delayed and patients
cannot be treated in a timely manner. Furthermore, with the
progressive aging of the population, the KOA patients and the
society as a whole are facing huge economic pressures. With the
continuous progress of molecular biology and genetic engineering,
scholars in China and other countries have made in-depth analyses
on osteoarthritis from the perspective of pathogenesis, providing
new approaches for the treatment and diagnosis of KOA (12,13).
MMPs are calcium- and zinc-dependent proteases that
can degrade almost all the components of extracellular matrix.
Studies published in the past few years indicate that MMPs are
related to onset of KOA (14). For
instance, MMPs and TIMP plays a crucial role in the pathogenesis of
KOA (15). TIMP can hydrolyze the
glycoproteins in the articular cartilage, destroy the cartilaginous
skeleton, and accelerate the progression of KOA. TIMP-1 plays an
important role in the pathogenesis of several inflammatory
conditions (16). Here, we found
that the levels of TIMP-1 mRNA and protein were significantly
increased in the synovial tissues of KOA patients compared with
those in controls. We also found that the expression level of
TIMP-1 in patients with severe KOA was significantly higher than
that in patients with milder KOA. Our analysis showed positive
correlation between the expression level of TIMP-1 and the severity
of osteoarthritis. Our results indicate that TIMP-1 is closely
related to the onset and development of KOA. Batra et al
found that TIMP regulated the metabolic processes of the
extracellular matrix by inhibiting MMPs (7). When TIMP was expressed at high levels,
the TIMP-1/MMPs ratio aggravated cartilage injury and affected the
development of osteoarthritis. In a normal cartilage, there is a
balance between MMPs and MMPs inhibitors: the imbalance between
MMPs and MMPs inhibitors may lead to cartilage degeneration
(17). Therefore, early diagnosis of
KOA can be realized by detecting the expression level of TIMP-1 in
the synovial membrane of KOA patient.
Bcl-2 is known to be the most important
anti-apoptotic cellular factor. Bcl-2 is mainly distributed in the
serosal surface of outer mitochondrial membrane, nuclear membrane,
and endoplasmic reticulum surface. Bcl-2 stabilizes the
mitochondrial membranes and maintains transmembrane potentials in
the mitochondria (17). Some studies
also find that Bcl-2 can reduce chondrocyte apoptosis by
maintaining the integrity of the extracellular matrix and
regulating the activity of telomerase (18). A study found that the expression
level of Bcl-2 adjacent to the fissure of cartilage was higher than
that in cartilage without a fissure and higher expression level was
detected in areas with severe injury (19). Here, we showed that the expression
levels of Bcl-2 were significantly higher in synovial tissues of
KOA patients than those in controls. The expression level of Bcl-2
was closely related to the severity of arthritis, but there was no
correlation between the expression levels of Bcl-2 and TIMP-1 in
KOA patients. These results suggest that Bcl-2 participates in the
occurrence and development of KOA, and that Bcl-2 may be involved
in the regulation of articular chondrocyte apoptosis in KOA
patients. The pathogenesis of KOA may be closely related to
chondrocyte apoptosis and the expression level of Bcl-2 can be used
as one of the indicators for diagnosing KOA.
In conclusion, both TIMP-1 and Bcl-2 are closely
related to the occurrence and development of KOA. Thus, they can be
used as the indicators for clinical diagnosis of KOA. However,
there are still some limitations to our study. The sample size is
small and all the patients were enrolled in one hospital. We did
not perform mechanistic studies to determine the causative role of
TIMP-1 and Bcl-2 on the pathogenesis of KOA. Nevertheless, TIMP-1
and Bcl-2 may be valuable for clinical diagnosis of KOA, and TIMP-1
and Bcl-2 can bring about new breakthroughs for clinical diagnosis
and treatment of KOA.
References
|
1
|
Kuyinu EL, Narayanan G, Nair LS and
Laurencin CT: Animal models of osteoarthritis: Classification,
update, and measurement of outcomes. J Orthop Surg. 11:192016.
View Article : Google Scholar
|
|
2
|
Bruyère O, Cooper C, Arden N, Branco J,
Brandi ML, Herrero-Beaumont G, Berenbaum F, Dennison E, Devogelaer
JP, Hochberg M, et al: Can we identify patients with high risk of
osteoarthritis progression who will respond to treatment? A focus
on epidemiology and phenotype of osteoarthritis. Drugs Aging.
32:179–187. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Arden N, Richette P, Cooper C, Bruyère O,
Abadie E, Branco J, Brandi ML, Berenbaum F, Clerc C, Dennison E, et
al: Can we identify patients with high risk of osteoarthritis
progression who will respond to treatment? A focus on biomarkers
and frailty. Drugs Aging. 32:525–535. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Moreau M, Pelletier JP, Lussier BV,
d'Anjou MA, Blond L, Pelletier JM, del Castillo JR and Troncy E: A
posteriori comparison of natural and surgical destabilization
models of canine osteoarthritis. BioMed Res Int. 33:851–855.
2013.
|
|
5
|
Heijink A, Gomoll AH, Madry H, Drobnič M,
Filardo G, Espregueira-Mendes J and Van Dijk CN: Biomechanical
considerations in the pathogenesis of osteoarthritis of the knee.
Knee Surg Sports Traumatol Arthrosc. 20:423–435. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Musumeci G, Castrogiovanni P, Trovato FM,
Weinberg AM, Al-Wasiyah MK, Alqahtani MH and Mobasheri A:
Biomarkers of chondrocyte apoptosis and autophagy in
osteoarthritis. Int J Mol Sci. 16:20560–20575. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Batra J, Robinson J, Mehner C, Hockla A,
Miller E, Radisky DC and Radisky ES: PEGylation extends circulation
half-life while preserving in vitro and in vivo activity of tissue
inhibitor of metalloproteinases-1 (TIMP-1). PLoS One. 7:e500282012.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Foight GW and Keating AE: Locating
herpesvirus Bcl-2 homologs in the specificity landscape of
anti-apoptotic Bcl-2 proteins. J Mol Biol. 427:2468–2490. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rother S, Samsonov SA, Moeller S,
Schnabelrauch M, Rademann J, Blaszkiewicz J, Köhling S,
Waltenberger J, Pisabarro MT, Scharnweber D, et al: Sulfate
hyaluronan alters endothelial cell activation in vitro by
controlling the biological activity of the angiogenic factors
vascular endothelial growth factor-A and tissue inhibitor of
metalloproteinase-3. ACS Appl Mater Interfaces. 9:9539–9550. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
McConnell S, Kolopack P and Davis AM: The
Western Ontario and McMaster Universities Osteoarthritis Index
(WOMAC): A review of its utility and measurement properties.
Arthritis Rheum. 45:453–461. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Valverde-Franco G, Lussier B, Hum D, Wu J,
Hamadjida A, Dancause N, Fahmi H, Kapoor M, Pelletier JP and
Martel-Pelletier J: Cartilage-specific deletion of ephrin-B2 in
mice results in early developmental defects and an
osteoarthritis-like phenotype during aging in vivo. Arthritis Res
Ther. 18:652016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lourenço S, Lucas R, Araújo F, Bogas M,
Santos RA and Barros H: Osteoarthritis medical labelling and
health-related quality of life in the general population. Health
Qual Life Outcomes. 12:1462014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim C, Nevitt MC, Niu J, Clancy MM, Lane
NE, Link TM, Vlad S, Tolstykh I, Jungmann PM, Felson DT, et al:
Association of hip pain with radiographic evidence of hip
osteoarthritis: Diagnostic test study. BMJ. 351:h59832015.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Adamson A, Ghoreschi K, Rittler M, Chen Q,
Sun HW, Vahedi G, Kanno Y, Stetler-Stevenson WG, O'Shea JJ and
Laurence A: Tissue inhibitor of metalloproteinase 1 is
preferentially expressed in Th1 and Th17 T-helper cell subsets and
is a direct STAT target gene. PLoS One. 8:e593672013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tency I, Verstraelen H, Kroes I,
Holtappels G, Verhasselt B, Vaneechoutte M, Verhelst R and
Temmerman M: Imbalances between matrix metalloproteinases (MMPs)
and tissue inhibitor of metalloproteinases (TIMPs) in maternal
serum during preterm labor. PLoS One. 7:e490422012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hire JM, Evanson JL, Johnson PC, Zumbrun
SD, Guyton MK, McPherson JC III and Bojescul JA: Variance of matrix
metalloproteinase (MMP) and tissue inhibitor of metalloproteinase
(TIMP) concentrations in activated, concentrated platelets from
healthy male donors. J Orthop Surg. 9:292014. View Article : Google Scholar
|
|
17
|
Dhar A, Gardner J, Borgmann K, Wu L and
Ghorpade A: Novel role of TGF-β in differential astrocyte-TIMP-1
regulation: Implications for HIV-1-dementia and neuroinflammation.
J Neurosci Res. 83:1271–1280. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lee SY, Kwok SK, Son HJ, Ryu JG, Kim EK,
Oh HJ, Cho ML, Ju JH, Park SH and Kim HY: IL-17-mediated Bcl-2
expression regulates survival of fibroblast-like synoviocytes in
rheumatoid arthritis through STAT3 activation. Arthritis Res Ther.
15:R312013. View
Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kernt M, Neubauer AS, Eibl KH, Wolf A,
Ulbig MW, Kampik A and Hirneiss C: Minocycline is cytoprotective in
human trabecular meshwork cells and optic nerve head astrocytes by
increasing expression of XIAP, survivin, and Bcl-2. Clin
Ophthalmol. 4:591–604. 2010. View Article : Google Scholar : PubMed/NCBI
|