Introduction
The cardiovascular disease is one of major diseases
threatening human health, among which acute myocardial infarction
(AMI) posses a higher incidence rate when compared with other
diseases in China even the whole world as well, and it features
rapid onset, fast development and high mortality due to
life-threatening severe arrhythmia and cardiogenic shock.
Myocardial infarction (MI) is ischemic necrosis of cardiac muscle.
Based on coronary artery disease, MI manifests a drastic reduction
or suspension of the coronary artery blood supply, which causes
severely and lastingly acute ischemia of corresponding cardiac
muscle, thus leading to myocardial necrosis (1,2). Current
literatures showed that bundle branch block (BBB) often expressed
by wide infarct size. The rate of cardiac failure, malignant
arrhythmia and fatality has been increasing significantly;
therefore, more and more attentions have been paid to BBB's
clinical significance (3–5).
Recent study (6)
showed that MI will cause myocardial ischemia or infarct which may
affect the conducting system of heart, and it always results in
various heart blocks, among which the occurrence rate of the right
bundle branch block (RBBB) reaches 10–13%. Foreign documents
(7) indicated that the occurrence
rate of AMI patients with left bundle branch block (LBBB) was 3.2%.
Though the incidence rate of AMI patients with LBBB is lower than
that with RBBB, it has been increasing over these years. Thus it
has been a hot issue to study BBB on AMI patients' prognosis.
Studies showed that there was a higher mortality in patients with
AMI combined with LBBB or RBBB than those without bundle-branch
block (8), therefore, the
bundle-branch block simultaneously with AMI had significant meaning
for the symptoms and prognosis of AMI patients.
Previous researches showed that the mortality of
patients with AMI combined with LBBB or RBBB was higher than that
of patients with NBBB; however, current notable guidelines of AMI
treatment only recommended new onset LBBB as the indication for
reperfusion therapy since 1996 (9–11). Our
studying team had repeatedly questioned above phenomena since 2010
(12–14) aiming at exploring the clinical
characteristics and value in early reperfusion therapy of new onset
RBBB in patients with acute myocardial infarction further, and
providing evidence for the treatment of AMI patients with RBBB.
Patients and methods
Patients
A total of 845 patients with AMI subjected to
primary coronary angiographic in Henan Provincial People's Hospital
(Zhengzhou, China) from January 2008 to June 2016 were analyzed
retrospectively according to the diagnostic criteria of AMI
(15) as proposed by ACC/AHA/ESC.
The patient whose document was incomplete and prospective life time
was shorter than one year was excluded. According to the appearance
of ECG in 12 h after onset of symptom, these patients were divided
into three groups: RBBB, LBBBB and non-bundle branch block
(non-BBB). The patients with bifascicular block were excluded.
Ultimately, 845 patients were included in our study. The Ethics
Committee and all the patients agreed to the study as they are
patients in Henan Provincial People's Hospital. All the
experimental processes were carried out as per the standards of the
Ethics Committee.
Data collections
Data of patients' baselines characteristics were
recorded on the admission data on electrocardiographic findings,
and the coronary angiographic findings were documented (Table I). The diagnosis of in-hospital MACE
and in-hospital mortality were recorded. The diagnostic criteria of
the left and right bundle-branch block were all in line with the
standards of bundle-branch block recommended in AHA/ACCF/HRS
guideline for electrocardiogram 2009 (16).
 | Table I.Patients baseline characteristics. |
Table I.
Patients baseline characteristics.
|
|
|
|
| P-value |
|---|
|
|
|
|
|
|
|---|
| Characteristics | New RBBB (n=70) | No BBB (n=719) | New LBBB (n=56) | P1 | P2 |
|---|
| Mean age (years) | 66.50±17.80 | 61.25±11.73 | 64.58±19.24 | 0.102 | 0.158 |
| Sex (males, %) | 52 (74.29) | 552 (76.77) | 29 (51.79) | 0.658 | 0.015a |
| Smoking (%) | 57 (81.43) | 455 (63.28) | 32 (57.14) | 0.002a | 0.003a |
| Hypertension (%) | 51 (72.86) | 362 (50.35) | 41 (73.21) |
<0.001a | 1.000 |
| Diabetes (%) | 35 (50.00) | 229 (31.85) | 31 (55.36) | 0.003a | 0.593 |
| Hyperlipemia (%) | 16 (22.86) | 64 (8.90) | 15 (26.79) | 0.001a | 0.679 |
| Killip ≥2 (%) | 55 (78.57) | 205 (28.51) | 46 (82.14) |
<0.001a | 0.659 |
| Peak level of
CK-MB | 560.00±356.74 | 214.23±187.25 | 630.85±465.89 | 0.001a | 0.023a |
| Symptom to balloon
time (h) | 6.14±3.25 | 4.12±3.87 | 5.69±3.54 | 0.352 | 0.8491 |
LBBB: i) QRS duration is ≥120 msec; ii) broad
notched or slurred R wave in leads I, aVL, V5 and V6 as well as an
occasional RS pattern in V5 and V6 attributed to displaced
transition of QRS complex; iii) absent q waves in leads I, V5, and
V6, but in the lead aVL, a narrow q wave may be present in the
absence of myocardial pathology; iv) R peak time is greater than 60
msec in leads V5 and V6 but normal in leads V1, V2 and V3, when
small initial r waves can be discerned in the above leads; v) ST
and T waves usually opposite in direction to QRS; vi) positive T
wave in leads with upright QRS may be normal (positive
concordance); vii) depressed ST segment and/or negative T wave in
leads with negative QRS (negative concordance) are abnormal.
RBBB: i) QRS duration is ≥120 msec in adults; ii)
rsr', rsR', or rSR' in leads V1 or V2. The R' or r' deflection is
usually wider than the initial R wave. In a minority of patients, a
wide and often notched R wave pattern may be seen in lead V1 and/or
V2; iii) the duration of S wave is greater than R wave or greater
than 40 msec in leads I and V6; iv) normal R peak time in leads V5
and V6 but >50 msec in lead V1. Of the above criteria, the first
three should be present to make the diagnosis. When a pure dominant
R wave with or without a notch is presented in V1, criterion 4
should be satisfied.
MACE: Including cardiac death, re-infraction, acute
left heart failure/deterioration of heart function, cardiac shock,
malignant arrhythmia (e.g., three-degree atrioventricular block,
ventricular fibrillation and sustained ventricular
tachycardia).
Statistical analysis
All the data were analyzed using SPSS 23.0 software
(SPSS, Inc., Tokyo, Japan). Absolute numbers, percentages, means
and SD, median, and upper/lower quartile were computed as
appropriate. Categorical variables were compared by using the
χ2 or Fisher exact test, as appropriate, and the odds
ratio (OR) and the 95% confidence intervals were calculated.
Independent predictors of new onset RBBB, LBBB, peak level of
creatine kinase-MB (CK-MB), level of heart function and occluded
position of IRA in AMI patients were screened by Logistic
regression stepwise method. Independent predictors of MACE during
hospitalization were analyzed by COX regression proportional hazard
model. P<0.05 was considered to indicate a statistically
significant difference. The survival rate was analyzed by
Kaplan-Meier method.
Results
Difference of clinical baselines
characteristics
Seventy patients (8.28%) presented RBBB and 56
(6.63%) patients presented LBBB in 845 patients with AMI, as shown
in Table I. Compared with non-BBB
patients, RBBB patients had a higher incidence of smoking,
hypertension and diabetes, hyperlipidaemia, worse heart function
and higher peak enzyme level (P<0.05). Compared with LBBB
patients, the RBBB patients were almost male, and have a lower
incidence of smoking, hypertension and diabetes, and a lower peak
enzyme level (P<0.05). The heart function between LBBB and RBBB
had no significant difference (P>0.05).
Coronary angiographic (CAG) findings
and percutaneous coronary intervention (PCI) stent
implantation
All of the 845 patients received emergent CAG. The
distribution of IRA between RBBB and non-BBB group had obvious
difference (Table II). IRA was
anterior descending artery (LAD) in 54.29% of RBBB patients and
35.47% in LBBB patients (54.29 vs. 35.47%, P<0.001). 35.47% of
RBBB patients' IRA was right coronary artery (RCA); however, there
was no statistical significance in the difference of IRA's
distribution between RBBB patients and LBBB patients. The incidence
of complete occluded IRA was higher in RBBB patients than that in
non-BBB patients (88.57 vs. 52.16%) (P<0.05) and LBBB patients
(88.57 vs. 62.50%) (P<0.05). The ratio of IRA occluded position
in proximal vessel of RBBB patients is noticeably higher than that
of non-BBB patients (74.29 vs. 19.33%) (P<0.05), and also higher
than that of LBBB patients but without statistical significance.
The Acceptance rate of emergency PCI patients in RBBB group was
prominently higher than that in non-BBB group (87.14 vs. 66.20%)
(P<0.05) and that in LBBB group (55.36 vs. 87.14%)
(P<0.05).
 | Table II.Angiographic findings and reperfusion
therapy. |
Table II.
Angiographic findings and reperfusion
therapy.
|
|
|
|
| P-value |
|---|
|
|
|
|
|
|
|---|
| Variables | New RBBB (n=70) | No BBB (n=719) | New LBBB (n=56) | P1 | P2 |
|---|
| 1-VD (%) | 10 (14.29) | 164 (22.81) | 8 (14.29) | 0.218 | 0.635 |
| 2-VD (%) | 22 (31.43) | 161 (22.39) | 10 (17.86) |
|
|
| 3-VD (%) | 43 (61.43) | 462 (64.26) | 43 (76.79) |
|
|
| IRA-LMCA (%) | 3 (4.29) | 54 (7.51) | 5 (8.93) |
<0.001a | 0.215 |
| IRA-LAD (%) | 38 (54.29) | 255 (35.47) | 24 (42.86) |
|
|
| IRA-LCX (%) | 6 (8.57) | 260 (36.16) | 11 (19.64) |
|
|
| IRA-RCX (%) | 27 (38.57) | 184 (25.59) | 18 (32.14) |
|
|
| Proximal lesion of
IRA (%) | 52 (74.29) | 139 (19.33) | 35 (62.50) |
<0.001a | 0.1235 |
| Proximal lesion-LAD
(%) | 29 (41.43) | 54 (7.51) | 12 (21.43) |
|
|
| Proximal lesion-LCX
(%) | 2 (2.86) | 27 (3.76) | 7 (12.50) |
|
|
| Proximal lesion-RCX
(%) | 19 (27.14) | 29 (4.03) | 10 (17.86) |
|
|
| TIMI=0/1 (%) | 62 (88.57) | 375 (52.16) | 35 (62.50) |
<0.001a | 0.0351a |
| PCI (%) | 61 (87.14) | 476 (66.20) | 31 (55.36) | 0.009a | 0.005a |
Electrocardiographic (ECG)
findings
By analyzing ECG of all patients, we found that the
distribution of infarct sites had obvious difference between RBBB
group and non-BBB group (P<0.05) and difference also existed
between RBBB group and LBBB group (P<0.05). The anterior and
high lateral wall myocardial infarction (58.57%) was common in RBBB
group, followed by the inferior wall and the right ventricular
myocardial infarction (34.29%) (Table
III). In this research, the graphics characteristic of RBBB in
10 patients (14.29%) in RBBB group and in 5 patients (8.93%) in
LBBB group appeared in hyperacute period, but the difference of
ratio between the two groups had no statistical significance.
 | Table III.Position of infarctions. |
Table III.
Position of infarctions.
|
|
|
|
| P-value |
|---|
|
|
|
|
|
|
|---|
| Variables | New RBBB
(n=70) | No BBB (n=719) | New LBBB
(n=56) | P1 | P2 |
|---|
| Anterior and/or
high-lateral wall (%) | 41 (58.57) | 369 (51.32) | 31 (55.36) |
<0.001a | 0.032a |
| Inferior and/or
posterior wall (%) | 3 (4.29) | 240 (33.38) | 16 (28.57) |
|
|
| Inferior and/or
right ventricular (%) | 24 (34.29) | 102 (14.19) | 8 (14.29) |
|
|
Independent predictor of new onset
RBBB
After inducting the clinical baselines
characteristics and CAG findings (such as age, sex, underlying
disease, IRA and occluded position of IRA) into the logistic
equation, we found that the TIM 0/1 of IRA (OR=3.28, P<0.01) and
proximal occlusion of IRA (OR=12.72, P<0.01) were independent
predictors of the new onset RBBB.
In-hospital prognosis
There were 217 cases of in-hospital MACE among the
845 patients, 41 cases in RBBB group, 146 cases in non-BBB group
and 30 cases in LBBB group. The RBBB group was significantly
different with the non-BBB group in aspect of the average days of
stay, left ventricular ejection fraction, pro-BNP, heart failure,
cardiac shock, cardiovascular mortality and the total rate of MACE
(P<0.05); but there was no obvious difference between RBBB group
and LBBB group (P>0.05) (Table
IV). The grade of heart function, peak level of CK-MB, new
onset of RBBB, new onset of LBBB and the occluded position of IRA
were independently associated with the appearance of in-hospital
MACE in the multivariate Cox proportional hazard regression model
(Table V). The new RBBB had a RR
value of 4.682 for the in-hospital MACE event, indicated that the
probability of a MACE incident occurring in patients with AMI
associated with a new RBBB is 4.682 times higher than that in
patients without RBBB.
 | Table IV.In-hospital outcomes. |
Table IV.
In-hospital outcomes.
|
|
|
|
| P-value |
|---|
|
|
|
|
|
|
|---|
| Variables | New RBBB n=70 | No BBB n=719 | New LBBB n=56 | P1 | P2 |
|---|
| Mean in-hospital
time (day) | 20.06±8.50 | 10.23±5.69 |
18.46±10.87 | 0.012a | 0.985 |
| Mean EF (%) |
43.59±17.86 |
64.71±27.51 |
42.18±23.42 | 0.041a | 0.756 |
| Pro-BNP
(pg/ml) |
2,320±1983 |
265±238 | 2,579±1652 |
<0.001a | 0.521 |
| Heart failure
(%) | 10 (14.28) | 15 (2.09) | 7 (12.50) |
<0.001a | 0.800 |
| Malignant
arrhythmia (n, %) | 9 (12.86) | 36 (5.00) | 5 (8.93) | 0.013a | 0.576 |
| Auricular
fibrillation (n, %) | 5 (7.14) | 33 (4.59) | 4 (7.14) | 0.373 | 1.000 |
| Cardiogenic shock
(n, %) | 11 (15.71) | 37 (5.15) | 6 (10.71) | 0.002a | 0.446 |
| Cardic death (n,
%) | 13 (18.57) | 36 (5.00) | 10 (17.86) |
<0.001a | 1.000 |
| All MACE (n,
%) | 41 (58.57) | 146 (20.36) | 30 (53.57) |
<0.001a | 0.169 |
 | Table V.Independent predictors of in-hospital
MACE (adjusting other factors). |
Table V.
Independent predictors of in-hospital
MACE (adjusting other factors).
| Variables | Coefficient | P-value | RR | 95% CI |
|---|
| Peak level of
CK-MB | 0.009 | 0.012a | 2.035 | 0.825–1.689 |
| Level of heart
function | 3.021 |
<0.001a | 41.283 | 1.382–373.468 |
| New RBBB | 1.897 |
<0.001a | 4.682 | 1.025–8.567 |
| New LBBB | 1.123 |
<0.001a | 3.687 | 1.002–6.589 |
| Occluded position
of IRA | 1.259 | 0.038a | 2.037 | 1.258–8.593 |
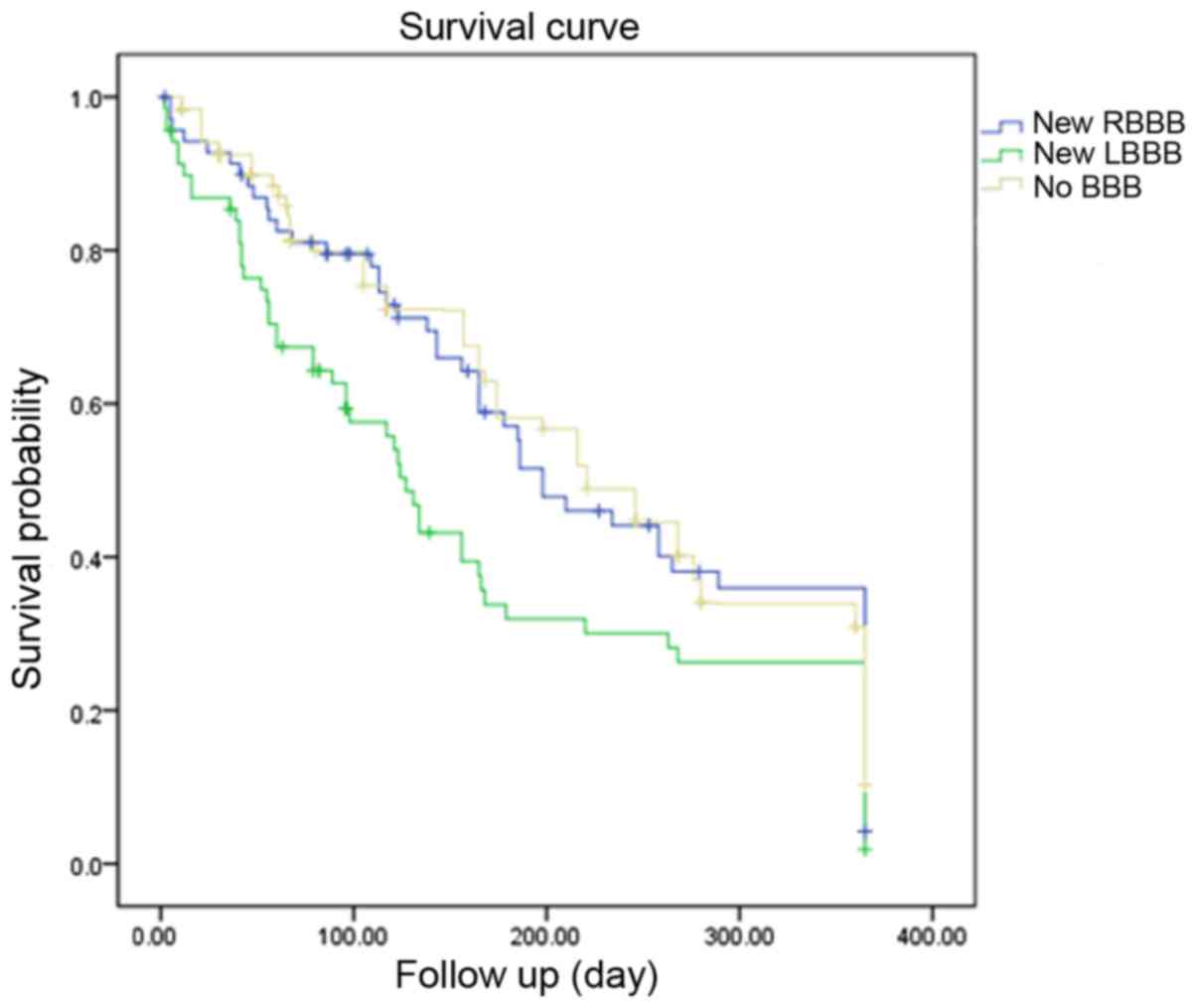
One-year mortality comparison
According to one-year Kaplan-Meier survival
analysis, the cumulative one-year survival rate in RBBB group was
significantly different with that in the no BBB group (P=0.046).
Also, compared with the LBBB group, the RBBB group had a lower
survival rate, and the difference was statistically significant
(P<0.001; Fig. 1).
Discussion
The high mortality of AMI combined with bundle
branch block was confirmed in the 1970s (1); however, authoritative guidelines for
AMI all over the world only recommend new onset LBBB as an
indication of reperfusion therapy but never mention the new onset
RBBB.
Previous reports about AMI combined with new onset
RBBB showed that the incidence of new RBBB in AMI was 4–18%. The
research results showed that the incidence of new RBBB in AMI
patients in the first 12 h was 6.32%, slightly higher than the
incidence in the reports of Wagner et al (17) and Widimsky et al (18), and also higher than the incidence of
new LBBB in this research. There was no obvious difference in the
peak level of CK-MB, the level of heart function, the incidence of
in-hospital MACE and in-hospital mortality between RBBB group and
LBBB group; but all indexes in the former two groups were higher
than those in the non-BBB group. The above results are similar to
previous documentations (4). In RBBB
group, the ratio of that IRA was LAD was 54.29% and the ratio of
that IRA was RCX was 38.57%. Both of the above percentages were
higher than those in non-BBB group significantly but had no
apparent difference in contrast with those in LBBB group. The right
bundle branch is slender and runs through inter-ventricular septum.
The blood supply of proximal end of right bundle branch comes from
inter-ventricular septal anterior artery and atrioventricular nodal
artery, while the middle and distal end of right bundle branch are
supplied by penetrating branches from the left anterior descending
coronary artery independently. Thus, occlusion of the LAD is
associated with the appearance of new RBBB; however, LBBB which has
strong anti-ischemia ability accepts double blood supply from LAD
and the posterior descending branch (19). The incidence of new RBBB in AMI
patients is higher than that of new LBBB; moreover, this research
also showed that the proportion of anterior and/or high lateral
wall myocardial infarction as induced by LAD occlusion in AMI
combined with new RBBB patient was high. This finding can be
supported by previous research (17).
The right coronary artery supplies 90% of the upper
portion of the inter-ventricular septum, including the AV node, the
bundle of His and the upper segments of the two main bundle
branches (20). In this sense, the
occlusion of RCX can not only induce disturbance of AV conduction
but also lead to bundle branch block (21). In 1976, Fukuda et al (22) reported that the interruption of blood
flow at the proximal right coronary artery could result in the
right ventricular dilatation. Chronic damage of RBBB in combination
with mechanical stretching might be the main reasons for the
appearance of new RBBB. In this clinic research, we found that rate
of new RBBB was 38.57% in RBBB patients with occlusion of RCX.
Further analyses indicated that the proportion of proximal
occlusion and TIMI 0/1 of IRA was higher in RBBB group than that in
non-BBB group obviously.
The complete occlusion of RCX can obstruct the blood
supplement of the right ventricular branch which originates from
RCX. Because of disappearance of right ventricular branch's blood
supplement, a large area of the right ventricular myocardial
ischemia can induce the maximum rate of depolarization of 0 phase
to slow down. As a result, the conduction velocity of activation in
the right ventricular myocardium slows down, thus the left and
right ventricular depolarization is not synchronous, which may
contribute to the incidence of MACE.
The findings of this research also showed that the
proportion of proximal occlusion of IRA in RBBB group was obviously
higher than that in non-BBB group; but there was no significant
difference between RBBB group and LBBB group. The proportions of
TIMI 0/1 in IRA and patients conducted primary PCI in RBBB group
were both higher than those in the non-BBBB group and the LBBB
group. These results illustrated that the characteristics of
coronary of AMI patients combined with new onset RBBB were more
accordant with the indication of primary PCI. Additionally, further
logistic regression analysis showed that the proximal occlusion and
TIMI flow 0/1 of IRA were both the independent risk factors of new
onset RBBB in AMI patients. COX regression analysis showed that new
onset RBBB was an independent predictor of in-hospital MACE, the
same as new onset LBBB.
The characteristic of coronary lesion of AMI in
combination with the new onset RBBB is proximal complete occlusion
of LAD or RCX. The essential reason of the appearance of new onset
RBBB in AMI patients are blood supply obstruction of the right
bundle branch and the ischemia or necrosis of a large area in the
right ventricular myocardium. As to these patients, clinical
symptoms are more serious and the prognosis is worse; therefore,
the demand of reperfusion therapy is more urgent; however, at
present, the majority guidelines regarding to the indications of
emergency revascularization in AMI only mention the elevation of ST
segment and the new or presumed new LBBB all over the world
(9–11). Our team has been proposing the query
at the absence of RBBB in these guidelines of AMI since 2010
(12–14). Widimsky et al (18) proposed the recommendation that new
onset RBBB should be included in the indications of emergency
revascularization in AMI European patients. This research confirmed
that AMI patients with new onset RBBB was a group which existed
objectively. In addition, the incidence of new RBBB was higher than
new LBBB in AMI patient and the characteristic of coronary lesion
in new RBBB patients was fitter the indication of primary PCI than
LBBB and non-BBB patients. The reasons mentioned above corroborate
that new onset RBBB in AMI should be listed as indication of
emergency revascularization as new onset LBBB. In fact, both the
guidelines of the American College of Emergency Physicians for the
management of patients with suspected AMI or unstable angina in
2000 (23) contained this standpoint
but not attracted serious concerns.
Currently, the reason supporting the guidelines
which exclude the new onset RBBB is that LBBB influences the first
40 msec of the ventricular depolarization and hide the appearance
of pathological Q wave, hereby further affecting the diagnosis of
AMI; however, RBBB only influences the last 40 msec of ventricular
depolarization without effect on AMI diagnosis. We consider further
researches are needed to explore early phase indicator prompting
ischemic. Pathological Q wave is the electrocardiographic
characteristic of establishing the phase rather than hyperacute or
evolving phase. Thus, early revascularization cannot be
accomplished by depending on the pathological Q waves in AMI
patients. In this research, the incidence of new RBBB in the first
12 h since symptom onset was higher than new LBBB, and 4 cases of
new RBBB were detected in hyperacute phase in RBBB group. In
addition, the detection rate of new RBBB in hyperacute phase had no
obvious difference when compared with the new LBBB's. Apparently,
the value of new onset RBBB in early diagnosis and
revascularization shouldn't be ignored; moreover, if the new onset
RBBB was excluded from the indications of emergency
revascularization in these authoritative guidelines of AMI, these
guidelines would not only transmit the error information that AMI
patients combining with new RBBB were few and the symptom of these
patients was not severe, but also manifest the defect of
theoretical system of electrocardiogram.
Bansilal et al (24) in their long-term follow-up found that
AMI patients with LBBB had increasing possibility of adverse
cardiovascular events including death, sudden death and
revascularization. In this study, the one-year cumulative survival
in RBBB group was obviously lower than that in non-BBB group and
their inter-difference was statistically significant. Study by
Kleemann et al (25)
demonstrated that AMI patients with RBBB had poor prognosis and low
long-term survival. Studies on AMI patients with LBBB or with RBBB
indicated that those patients had wild infarct size and high rate
of adverse cardiovascular events. Longer follow-up might conduct
more accurate results, which still demanded retrospective analyses
on a large scale and for long-term.
In-time unblocking of infarcted vessel can improve
the patients' prognosis. Some study indicated that, with all
contraindications being excluded, AMI patients with BBB should
receive emergency PCI treatment (26). Though thrombolysis can effectively
decrease AMI patients' mortality and features advantage of massive
utility, easy implementation and low coast, thrombolysis therapy
has more contraindications and higher risk of bleeding; as a
result, PCI treatment is more popular at present; moreover,
research by Keeley (27) showed that
it would be better for AMI patients to conduct emergency PCI
treatment than thrombolysis therapy.
The primary limitation of this study is
retrospective characteristics. We cannot determine the onset time
of RBBB in numbers of the acute myocardial infarction patients,
thus presumable RBBB may influence the statistical result of the
research. Another limitation in relation to the fact is that the
coronary angiography analysis was not performed in a blinded
manner.
The characteristic of coronary artery lesion of most
acute myocardial infarction patients accompanying with new onset
RBBB is completely proximal occlusion of LAD or RCX. Compared with
non-BBB patients, the peak level of CK-MB, the level of heart
function and the incidence of in-hospital MACE are higher in the
new onset RBBB patients. The incidence of in-hospital MACE and
detection rate in hyperacute phase between LBBB group and RBBB has
no obvious difference, but the incidence of new onset RBBB is
higher than the new LBBB in acute myocardial infarction patients.
Thus, the new onset RBBB should be considered as indication of
emergency revascularization in the guidelines of acute myocardial
infarction.
Acknowledgements
I thank all authors who have contributed to this
study for advice and comments. This study is supported by Research
on Revascularization of Chinese patients with acute coronary
syndromes, attached to Key Project of Science of Technology
Department of Henan Province in 2012 (grant no. 122102310068).
References
|
1
|
Ross JC and Dunning AJ: Right bundle
branch block and left axis deviation in acute
myocard-ialinfarction. Br Heart J. 32:847–851. 1970. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nguyen BL, Tufano F, De Angelis S,
Tersigni F, Alessandri N and Brugada P: Ventricular fibrillation
induction and diffuse abnormal ST-segment response to ajmaline in a
patient with apparent pre-existing dynamic right bundle branch
block. Eur Rev Med Pharmacol Sci. 18:3115–3119. 2014.PubMed/NCBI
|
|
3
|
Freedman RA, Alderman EL, Sheffield LT,
Saporito M and Fisher LD: Bundle branch block in patients with
chronic coronary artery disease: Angiographic correlates and
prognostic significance. J Am Coll Cardiol. 10:73–80. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Melgarejo-Moreno A, Galcerá-Tomás J,
Garciá-Alberola A, Valdés-Chavarri M, Castillo-Soria FJ,
Mira-Sánchez E, Gil-Sánchez J and Allegue-Gallego J: Incidence,
clinical characteristics, and prognostic significance of right
bundle-branch block in acute myocardial infarction: A study in the
thrombolytic era. Circulation. 96:1139–1144. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wagdy HM, Hodge D, Christian TF, Miller TD
and Gibbons RJ: Prognostic value of vasodilator myocardial
perfusion imaging in patients with left bundle-branch block.
Circulation. 97:1563–1570. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Patanè S, Marte F, Di Bella G and
Chiribiri A: Atrial fibrillation with intermittent right axis
deviation in the presence of complete left bundle branch block. Int
J Cardiol. 129:e1–e2. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
De Sutter J, De Bondt P, Van de Wiele C,
Fonteyne W, Dierckx R, Clement D and Tavernier R: Prevalence of
potential candidates for biventricular pacing among patients with
known coronary artery disease: A prospective registry from a single
center. Pacing Clin Electrophysiol. 23:1718–1721. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
De Sutter J: Incidence of potential
candidates for biventricular pacing in heart failure: Results from
a one year single-centre prospective registry. Eur Heart J.
21:1922000.
|
|
9
|
Wong CK, Stewart RA, Gao W, French JK,
Raffel C and White HD: Prognostic differences between different
types of bundle branch block during the early phase of acute
myocardial infarction: Insights from the Hirulog and Early
Reperfusion or Occlusion (HERO)-2 trial. Eur Heart J. 27:21–28.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ryan TJ, Anderson JL, Antman EM, Braniff
BA, Brooks NH, Califf RM, Hillis LD, Hiratzka LF, Rapaport E,
Riegel BJ, et al: ACC/AHA guidelines for the management of patients
with acute myocardial infarction: Executive summary. A report of
the Amer-ican College of Cardiology/American Heart Association Task
Force on Practice Guidelines (Committee on Management of Acute
Myocardial Infarction). Circulation. 94:2341–2350. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Antman EM, Anbe DT, Armstrong PW, Bates
ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas
GA, et al: American College of Cardiology. American Heart
Association. ACC/AHA guidelines for the management of patients with
ST-elevation myocardial infarction-executive summary: A report of
the American College of Cardiology/American Heart Association Task
Force on Practice Guidelines (Writing Committee to revise the 1999
guidelines for the management of patients with acute myocardial
infarction. J Am Coll Cardiol. 44:671–719. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Task Force on the management of ST-segment
elevation acute myocardial infarction of the European Society of
Cardiology (ESC)1, ; Steg PG, James SK, Atar D, Badano LP,
Blömstrom-Lundqvist C, Borger MA, Di Mario C, Dickstein K, Ducrocq
G, et al: ESC Guidelines for the management of acute myocardial
infarction in patients presenting with ST-segment elevation. Eur
Heart J. 33:2569–2619. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chu YJ: New thinking of acute myocardial
infraction electrocardiogram. J Prac Diag Therap. 24:533–536.
2010.
|
|
14
|
Iwasaki J, Kono K, Katayama Y, Takahashi
N, Takeuchi K, Tanakaya M, Osawa K, Shiraki T and Saito D:
Prognostic significance of right bundle branch block in patients
with acute inferior myocardial infarction. Acta Med Okayama.
63:25–33. 2009.PubMed/NCBI
|
|
15
|
Chu YJ, Wang FF, Liu XY, HE WQ and Wang
YH: Several rare changes in the electro-cardiogram with myocardial
ischemia. Chin J Card Pacing Electro Physio. 25:330–333. 2011.
|
|
16
|
Thygesen K, Alpen JS and White HD; Joint
ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial
Infarction, : Universal definition of myocardial infarction. J Am
Coll Cardiol. 50:2173–2195. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wagner GS, Macfarlane P, Wellens H,
Josephson M, Gorgels A, Mirvis DM, Pahlm O, Surawicz B, Kligfield
P, Childers R, et al: AHA/ACCF/HRS recommendations for the
standardization and interpretation of the electrocardiogram: part
VI: acute ischemia/infarction: a scientific statement from the
American Heart Association Electrocardiography and Arrhythmias
Committee, Council on Clinical Cardiology; the American College of
Cardiology Foundation; and the Heart Rhythm Society. Endorsed by
the International Society for Computerized Electrocardiology. J Am
Coll Cardiol. 53:1003–1011. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Widimsky P, Rohác F, Stásek J, Kala P,
Rokyta R, Kuzmanov B, Jakl M, Poloczek M, Kanovsky J, Bernat I, et
al: Primary angioplasty in acute myocardial infarction with right
bundle branch block: Should new onset right bundle branch block be
added to future guidelines as an indication for reperfusion
therapy? Eur Heart J. 33:86–95. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Brilakis ES, Wright RS, Kopecky SL, Reeder
GS, Williams BA and Miller WL: Bundle branch block as a predictor
of long-term survival after acute myocardial infarction. Am J
Cardiol. 88:205–209. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hadziselimovic H: Vascularization of the
conducting system in the human heart. Acta Anat. 102:105–110. 1978.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
James TN and Burch GE: Blood supply of the
human interventricular septum. Circulation. 17:391–396. 1958.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Fukuda K, Nakata Y, Okada R and Takagi T:
Histopathological studies on the conduction susytem of complete
right bundle branch block wth special reference to configuration of
QRS complex. Jpn Heart J. 20:831–844. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
American College of Emergency Physicians,
. Clinical policy: Critical issues in the evaluation and managent
of adult patients presenting with suspected acute myocardial
infarction or unstable angina. Ann Emerg Med. 35:521–544. 2000.
View Article : Google Scholar
|
|
24
|
Bansilal S, Aneja A, Mathew V, Reeder GS,
Smars PA, Lennon RJ, Wiste HJ, Traverse K and Farkouh ME: Long-term
cardiovascular outcomes in patients with angina pectoris presenting
with bundle branch block. Am J Cardiol. 107:1565–1570. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kleemann T, Juenger C, Gitt AK, Schiele R,
Schneider S, Senges J, Darius H and Seidl K; MITRA PLUS Study
Group, : Incidence and clinical impact of right bundle branch block
in patients with acute myocardial infarction: ST elevation
myocardial infarction versus non-ST elevation myocardial
infarction. Am Heart J. 156:256–261. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gallagher EJ: Which patients with
suspected myocardial ischemia and left bundle-branch block should
receive thrombolytic agents? Ann Emerg Med. 37:439–444. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Keeley EC, Boura JA and Grines CL: Primary
angioplasty versus intravenous thrombolytic therapy for acute
myocardial infarction: A quantitative review of 23 randomised
trials. Lancet. 361:13–20. 2003. View Article : Google Scholar : PubMed/NCBI
|