Introduction
Acute lung injury (ALI) and acute respiratory
distress syndrome (ARDS) are two serious forms of diffuse lung
disease, which impose a substantial health burden worldwide
(1). They usually occur in
association with severe diseases, such as serious infection, burns,
trauma and shock, and can be clinically characterized by
progressive hypoxemia and respiratory distress, which contributes
to alveolar and diffuse pulmonary interstitial edema that is caused
by injury to alveolar epithelial cells and pulmonary capillary
endothelial cells (2). ALI/ARDS is a
major clinical challenge with a high mortality rate of 30–40%
(3). In the past, various
interventions and intensive care strategies have been applied to
patients with ALI/ARDS. However, only certain supportive treatments
utilizing a fluid conservative strategy and lung protective
ventilation have been demonstrated to be effective for reducing
morbidity and mortality (4). Thus,
the development of a novel therapeutic strategy to improve the
outcome of ALI/ARDS is required (5).
Despite the intensive research conducted in animals
and patients, the etiology and mechanisms of ALI/ARDS have not yet
been completely clarified. In previous studies, it has been
reported that the systemic inflammatory response caused by multiple
pathogenic factors, such as lipopolysaccharide (LPS), plays a vital
role (1,3). However, the specific cellular and
molecular mechanisms of ALI/ARDS are not completely known (6). Autophagy is a conserved cellular
process for the disposal of denatured proteins and damaged
organelles through a lysosomal degradation pathway that occurs in
almost all cells having mitochondria (7). Autophagy executes a homeostatic
function in cells when occurring at low basal levels. However,
autophagy is rapidly upregulated when intracellular nutrition
and/or energy are deficient, such as during starvation, growth
factor depletion and in hypoxia (8).
It has been indicated that autophagy is associated with a number of
pulmonary diseases, including ALI (9). Therefore, the inhibition of autophagy
may potentially protect against ALI. 3-methyladenine (3-MA), is a
phosphoinositide 3-kinase (PI3K) inhibitor that has been well
established as an autophagy inhibitor. Previous studies have
indicated that dexmedetomidine (DEX) has protective effects on
pulmonary functions in ALI and ventilator-induced lung injury
(10).
In the present study, an ALI model was constructed
by exposing experimental mice to LPS. The protective effect and
underlying therapeutic mechanism of 3-MA and DEX on ALI were
subsequently evaluated in this model.
Materials and methods
Animals and treatments
BALB/c mice (n=120; 60 male and 60 female; 20–25 g;
5 weeks) were purchased from the Animal Experimental Center of
Southern Medical University (Guangzhou, China). All BALB/c mice
were bred in a stainless steel isolation box with free feeding and
drinking water. They were kept at a constant temperature (25±2°C)
and humidity (50–60%) and exposed to 12-h light/dark cycles. The
mice were randomly divided into four groups: Blank group (n=30),
intratracheally injected with 1.00 ml/kg 0.9% saline solution;
model group (n=30), intratracheally injected with 0.2% LPS (L2630;
Sigma-Aldrich; Merck KGaA, Darmstadt, Germany; 3 mg/kg); 3-MA group
(n=30), intraperitoneally injected with 0.2% LPS (3 mg/kg), and
then intravenously injected with 3-MA (cat no. M9281;
Sigma-Aldrich; Merck KGaA) solution (30 mg/kg) 1 h later; and DEX
(cat no. SML0956; Sigma-Aldrich; Merck KGaA) group (n=30),
intratracheally injected with 0.2% LPS solution (3 mg/kg), and then
intravenously injected with DEX solution (50 µg/kg) 1 h later.
The surviving mice in each group were observed at
three observation time points: 1, 3 and 5 days after injection, and
10 mice from each group were sacrificed under anesthesia at each of
these time points. All animal procedures were conducted following
the National Institutes of Health guidelines for the care and use
of laboratory animals, and the Institutional Animal Care and Use
Committee of Zhujiang Hospital approved all the experimental
protocols.
Arterial blood gas analysis and lung
wet-dry weight ratio (W/D)
Carotid arterial blood was immediately collected
from the BALB/c mice in each group following sacrifice on days 1, 3
and 5. Moreover, an automated blood gas analyzer (PL1000A; Wincom
Co., Ltd., Changsha, China) was used to measure the partial
pressure of carbon dioxide (PaCO2), partial pressure of
oxygen (PaO2) and pH value. In addition, the right upper
lung was separated and its wet weight was measured. The right upper
lung was then dried in a convection oven (DHG-9030A; Bluepard
Instruments Co., Ltd., Shanghai, China) until a constant weight was
achieved, and the dry weight was measured. Each example was
measured in triplicate. Finally, the W/D was calculated.
Albumin and cytokine content
determination in bronchoalveolar lavage fluid (BALF)
On days 1, 3 and 5, sacrificed BALB/c mice were
intratracheally injected with 0.5 ml PBS (4°C) three times. The
three BALF samples that were obtained were mixed and then
centrifuged at 500 × g (4°C) for 10 min. Albumin, tumor necrosis
factor (TNF)-α and interleukin (IL)-6 contents in the supernatant
were measured using ELISA kits (ab108792; Abcam, Cambridge, MA,
USA; MTA00B and M6000B; R&D Systems, Inc., Minneapolis, MN,
USA), respectively, according to the manufacturer's instructions.
Each example was performed in triplicate.
Myeloperoxidase (MPO) assay
MPO content in lung tissue was quantified using a
mouse MPO ELISA kit (cat no. ab155458; Abcam). This assay employed
a specific antibody against mouse MPO coated on 96-well plates.
Crushed lung tissue was centrifuged at 1,000 × g for 10 min at 4°C
and the supernatant and standards were added to the wells and MPO
in the sample was bound into the wells by the immobilized antibody.
After washing, biotinylated anti-mouse antibody was added and the
plate was incubated at room temperature for 1 h. The unbound
biotinylated antibody was then washed away, and horseradish
peroxidase (HRP)-conjugated streptavidin was added to the wells.
After washing three times, 3,3′,5,5′-tetramethylbenzidine substrate
solution was added and color developed in proportion to the content
of MPO. The addition of stop solution terminated the color
development, and the intensity of the color was measured at 450 nm
using a microplate reader (Biotek Instruments, Inc., Winooski, VT,
USA). Each example was performed in triplicate.
Hematoxylin and eosin (H&E)
staining
The lung tissue was fixed in 4% paraformaldehyde for
10 min and then cut into 5-µm sections. The sections were stained
as follows: 70% ethanol for 10 sec, diethyl pyrocarbonate-treated
water for 5 sec, and then hematoxylin with RNAase inhibitor for 20
sec, 70% ethanol for 30 sec, eosin Y in 100% ethanol for 20 sec,
followed by dehydration with a series of ethanol for 30 sec each,
and finally xylenes for 2 min. The morphometric analysis of
alveolar collapse, alveolar hemorrhage, perivascular hemorrhage,
vascular congestion, perivascular edema, alveolar edema, alveolar
polymorphonuclear leukocytes and macrophages was conducted, as
previously described (11). All HE
staining experiments were repeated three times.
Western blot analysis
The expression levels of the
autophagy-related-proteins microtubule-associated protein
1A/1B-light chain 3 (LC3)-I, LC3-II, autophagy protein 5 (ATG5),
Rab7 and lysosome-associated membrane protein 1 (LAMP1) were
detected using western blotting. The lung tissue was lysed in
radioimmunoprecipitation assay buffer (Beyotime Institute of
Biotechnology, Haimen, China) for 2 h at 4°C. After centrifugation
at 10,000 × g for 10 min at room temperature, the protein
concentration was determined using a BCA protein assay kit. A total
of 80 µg per lane of the protein lysates were separated by 12%
gradient sodium dodecyl sulfate-polyacrylamide gel electrophoresis
and then transferred to PVDF membranes (EMD Millipore, Billerica,
MA, USA). The PVDF membranes were blocked with 5% (w/v) skimmed
milk in TBS with 0.05% Tween-20 at room temperature for 2 h. After
washing three times with TBST, the PVDF membranes were incubated
with rabbit polyclonal anti-LC3 (cat no. L8918; Sigma-Aldrich;
Merck KGaA; 1:1,000), ATG5 (cat no. ab109490; 1:1,000), Rab7 (cat
no. ab50533; 1:2,000) and LAMP1 (cat no., ab25630; 1:10,000; all
Abcam) in PBS (0.25% Triton X and 1% BSA) at 37°C for 2 h. The
membranes were then incubated with anti-rabbit or anti-mouse
HRP-conjugated secondary antibody (cat no. BA1054; Wuhan Boster
Biological Technology, Ltd., Wuhan, China; 1:5,000) for 2 h at
37°C. The control GAPDH (Abcam; cat no. ab181602; 1:10,000) levels
were used for the normalization. Visualization with ECL detection
reagents (Pierce; Thermo Fisher Scientific, Inc.). The protein
bands were scanned with a ChemiDoc image analysis system (Bio-Rad
Laboratories, Inc., Hercules, CA, USA) and quantified with Image J
2× software (National Institutes of Health, Bethesda, MD, USA). All
western blot experiments were repeated three times.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total RNA was extracted from lung tissue using an
RNA Extraction kit (Invitrogen; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA). The concentration of total RNA was determined by
measuring the absorbance at 260 nm. The total RNA (0.5 µg) was
employed for cDNA synthesis using a cDNA Synthesis kit (cat no.
6210A; Takara, Biotechnology Co., Ltd., Dalian, China) according to
the manufacturer's protocols and subsequently the cDNA was diluted
using nuclease-free water to a concentration of 10 ng/µl. The
primers used for PCR are shown in Table
I. PCR was accomplished by a hotstart SYBR-green-based method
(VeriQuest SYBR-Green qPCR Master Mix, Invitrogen; Thermo Fisher
Scientific, Inc.). Gene fold-changes were determined using the ΔΔCq
method (12) and utilizing 18S rRNA
for normalization. DNA was amplified at 94°C for 3 min, followed by
35 cycles of 94°C for 15 sec and at 60°C for 15 sec. All RT-qPCR
experiments were performed in triplicate and repeated twice.
 | Table I.Primers used in the quantitative
polymerase chain reaction. |
Table I.
Primers used in the quantitative
polymerase chain reaction.
| Primer | Forward (5′-3′) | Reverse (5′-3′) |
|---|
| NF-κB |
CTGAACAAAATGCCCCACGG |
TTCCTCCTTTGGGACGATGC |
| TLR4 |
AGCCGGAAGGTTATTGTGGT |
CAGCAGGGACTTCTCAACCT |
| 18S |
GAATTCCCAGTAAGTGCGGGTCAT |
CGAGGGCCTCACTAAACCATC |
Statistical analysis
Data are presented as the mean ± standard error of
the mean and were analyzed using SPSS 13.0 statistical software
(SPSS Inc., Chicago, IL, USA). Data from multiple groups were
analyzed using analysis of variance with repeated measures. The
post-hoc test of least significant difference was used where equal
variances were assumed and Dunnett's T3 test was used when equal
variances were not assumed. A value of P<0.05 was considered to
indicate a statistically significant difference.
Results
Arterial blood gas analysis and lung
W/D
The results of arterial blood gas analysis, pH
analysis and W/D calculations are presented in Table II. In the model group, W/D and
PaCO2 were elevated and PaO2 was reduced
compared with those in the blank group (both P<0.05). These
results implied that the ALI model was successfully established. At
each time point, PaCO2 and W/D in the 3-MA and DEX
groups were lower compared with those in the model group (both
P<0.05), and the PaO2 values in the 3-MA and DEX
groups were higher compared with those in the model group
(P<0.05). No significant difference was identified in pH value
among the four groups (all P>0.05).
 | Table II.Comparison of PaO2,
PaCO2, pH value and W/D among the groups on days 1, 3
and 5 following the intratracheal injection of
lipopolysaccharide. |
Table II.
Comparison of PaO2,
PaCO2, pH value and W/D among the groups on days 1, 3
and 5 following the intratracheal injection of
lipopolysaccharide.
| Group | Day | n | PaO2
(mmHg) | PaCO2
(mmHg) | pH value | W/D |
|---|
| Blank group | 1 | 10 |
115.34±2.35 |
33.25±1.20 |
7.38±0.06 |
5.74±0.29 |
|
| 3 | 10 |
116.04±1.86 |
34.21±1.25 |
7.35±0.05 |
5.76±0.31 |
|
| 5 | 10 |
114.95±2.31 |
33.86±1.37 |
7.34±0.07 |
5.77±0.25 |
| Model group | 1 | 10 |
82.50±1.67a |
50.35±1.85a |
7.28±0.05a |
7.68±0.56a |
|
| 3 | 10 |
85.38±2.58a |
51.34±1.36a |
7.22±0.06a |
7.88±0.65a |
|
| 5 | 10 |
88.85±3.12a |
49.37±2.01a |
7.30±0.07a |
7.84±0.63a |
| 3-MA group | 1 | 10 |
109.75±1.65b |
38.56±1.76b |
7.35±0.05b |
6.35±0.27b |
|
| 3 | 10 |
110.68±2.30b |
39.86±1.48b |
7.36±0.07b |
6.32±0.28b |
|
| 5 | 10 |
112.45±1.60b |
40.25±2.34b |
7.37±0.04b |
6.28±0.31b |
| DEX group | 1 | 10 |
98.55±1.86b |
42.35±1.86b |
7.36±0.06b |
6.64±0.35b |
|
| 3 | 10 |
99.35±2.75b |
41.35±2.05b |
7.37±0.05b |
6.62±0.44b |
|
| 5 | 10 |
100.25±2.65b |
40.55±1.88b |
7.38±0.04b |
6.58±0.30b |
Albumin, cytokine and MPO
contents
The ELISA results for albumin and cytokines (TNF-α
and IL-6) in BALF and MPO in lung tissue are shown in Table III. The levels of albumin, TNF-α
and IL-6 in the BALF were significantly increased in the model
group compared with the blank group (P<0.05). Furthermore, the
levels of TNF-α, IL-6, MPO and albumin were significantly decreased
in the BALF in the 3-MA or DEX groups when compared with the model
group (P<0.05).
 | Table III.Comparison of TNF-α, IL-6 and albumin
content in BALF and MPO content in lung tissue among the groups on
day 1, 3 and 5 following the intratracheal injection of
lipopolysaccharide. |
Table III.
Comparison of TNF-α, IL-6 and albumin
content in BALF and MPO content in lung tissue among the groups on
day 1, 3 and 5 following the intratracheal injection of
lipopolysaccharide.
| Group | Day | n | TNF-α (pg/ml) | IL-6 (pg/ml) | MPO (ng/ml) | Albumin
(ng/ml) |
|---|
| Blank group | 1 | 10 |
101.06±4.32 |
90.25±4.65 |
20.34±1.35 |
48.67±3.35 |
|
| 3 | 10 |
102.34±3.86 |
91.34±4.85 |
21.38±1.42 |
49.35±5.26 |
|
| 5 | 10 |
103.34±2.65 |
92.37±3.65 |
20.24±1.37 |
50.31±4.96 |
| Model group | 1 | 10 |
612.35±5.63a |
402.36±5.67a |
80.34±1.65a |
183.24±6.68a |
|
| 3 | 10 |
604.35±5.84a |
398.36±5.34a |
82.35±2.47a |
180.27±5.48a |
|
| 5 | 10 |
593.68±4.67a |
390.25±6.31a |
81.35±2.36a |
173.26±6.04a |
| 3-MA group | 1 | 10 |
204.63±3.64b |
200.45±5.28b |
41.25±2.32b |
98.34±5.55b |
|
| 3 | 10 |
201.32±2.86b |
192.24±4.67b |
42.15±2.41b |
94.31±5.22b |
|
| 5 | 10 |
195.75±3.68b |
188.57±4.35b |
40.85±1.33b |
90.38±6.33b |
| DEX group | 1 | 10 |
285.64±4.56b |
300.35±5.86b |
51.58±2.46b |
152.39±5.28b |
|
| 3 | 10 |
279.49±5.36b |
286.34±5.26b |
50.22±1.41b |
143.37±6.24b |
|
| 5 | 10 |
268.42±5.26b |
275.31±6.74b |
49.85±1.37b |
132.27±5.64b |
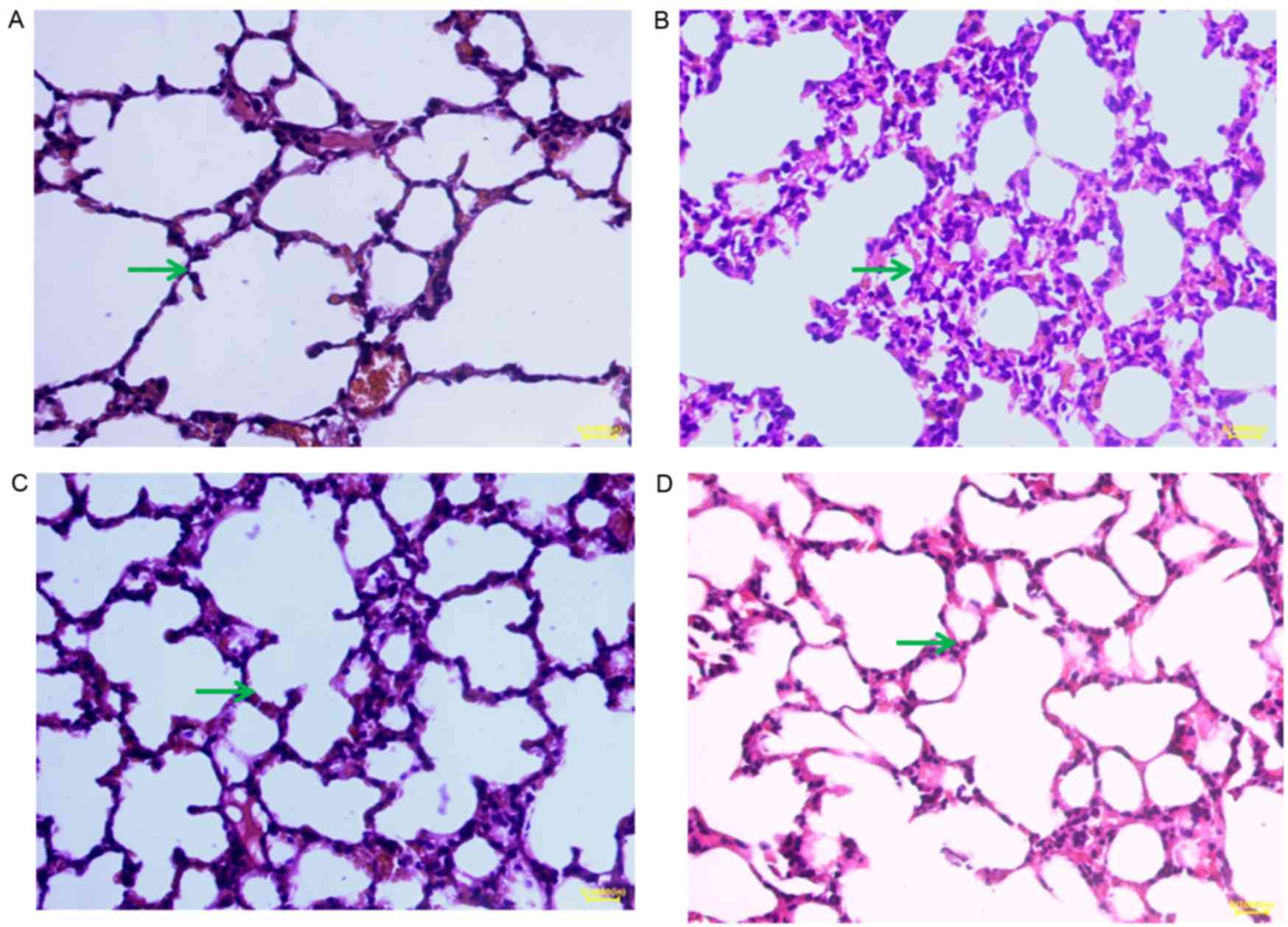
H&E staining
H&E staining images for samples from day 1 are
displayed in Fig. 1. In the blank
group, H&E staining revealed thin alveolar walls and clear
alveolar structures. Moreover, no hyperemia or widening was
observed in the alveolar septum and no symptoms of bleeding and
inflammatory cell infiltration were detected (Fig. 1A). In the model group, pulmonary
interstitial and alveolar edema progressed rapidly, and alveolitis
was clearly observed. Diffuse pulmonary hemorrhage, vascular
endothelial cell injury, the formation of hyaline membranes and
alveolar collapse occurred, and a heavy infiltration of
inflammatory cells was visible in the alveolar space, accompanied
by slight hemorrhage and edema (Fig.
1B). In the 3-MA and DEX groups, pulmonary lesions were
comparable. It was observed macroscopically that the lung was
slightly enlarged and the bleeding points and ecchymosis were
visible in sections of the lung. The surface of the lung tissues
was uneven locally, with a scattering of small white nodules.
However, observation of the images in Fig. 1C and D indicates that the protective
effect of 3-MA was particularly evident. The H&E staining
results for samples taken on days 3 and 5 were similar to those on
day 1. The H&E staining demonstrated that 3-MA and DEX are able
to alleviate the pathological changes of acute alveolitis in
mice.
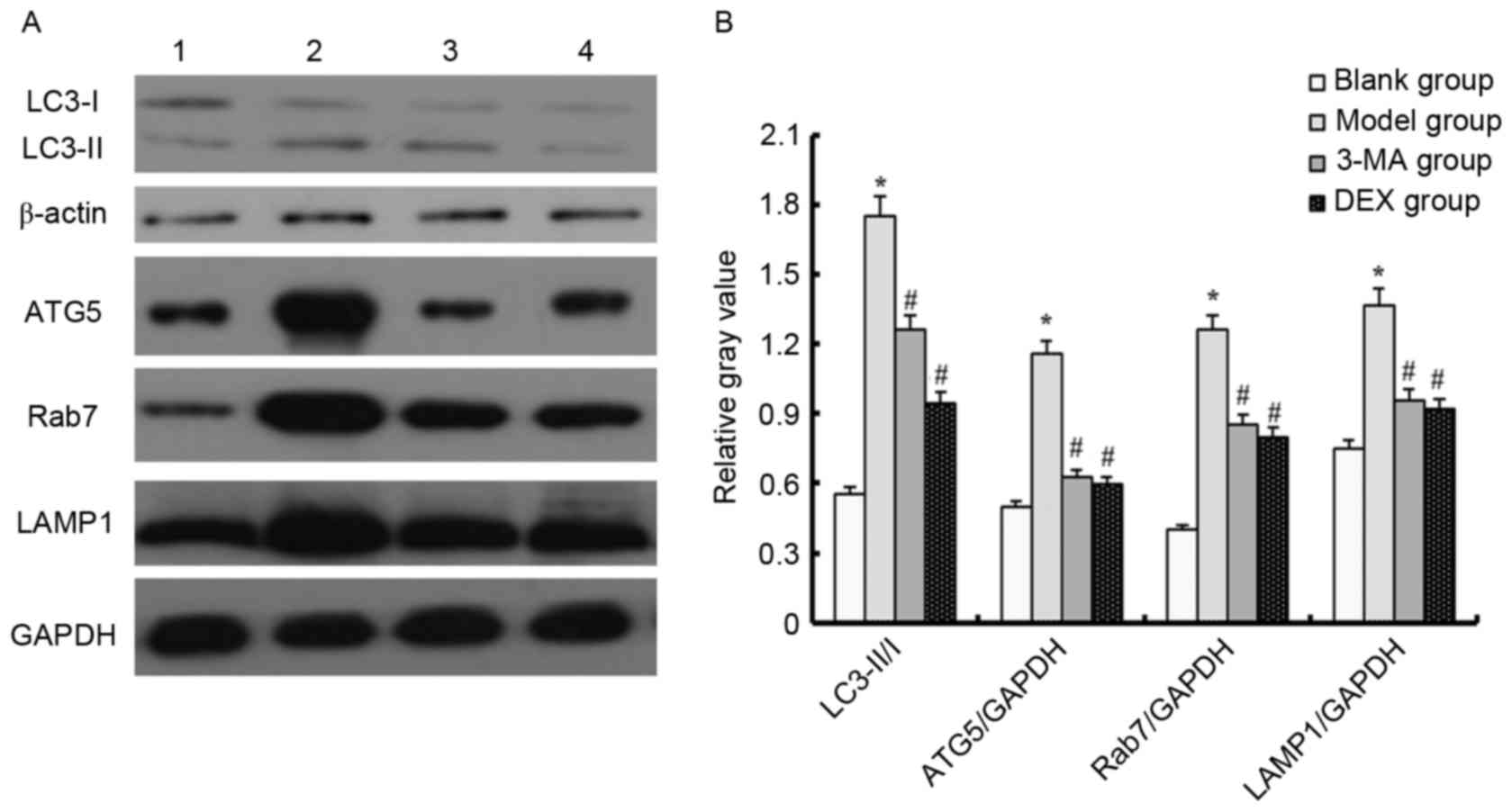
Western blot analysis
Western blotting was used to detect changes in the
LC3-II/I ratio in order to evaluate the occurrence of autophagy. A
higher LC3-II/I ratio is indicative of a higher level of autophagy
(13). The LC3-II/I ratio was higher
in the model group compared with the blank group. In addition,
compared with the blank group, the expression levels of ATG5, Rab7
and LAMP1 were upregulated in the model group (P<0.05). This
indicates that LPS increased the level of autophagy in mice.
However, when the ALI model mice were treated with 3-MA or DEX, the
LC3-II/I ratio, and ATG5, Rab7 and LAMP1 expression levels were
downregulated (P<0.05). These results indicate that 3-MA and DEX
are able to reduce autophagy (Fig.
2). The results shown in Fig. 2
are those for samples taken on day 1; the results for samples taken
on days 3 and 5 (data not shown) were similar to those on day
1.
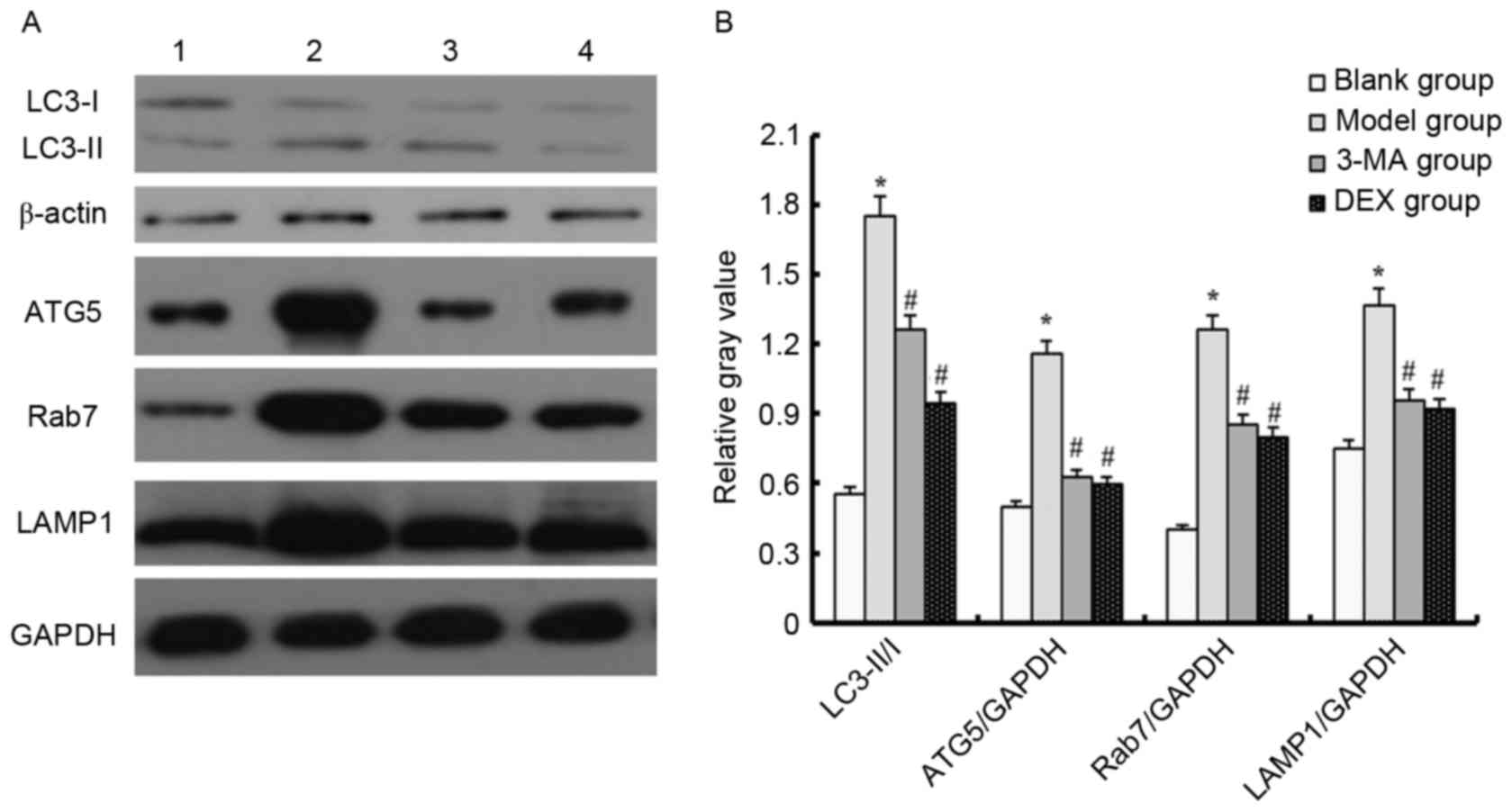 | Figure 2.Autophagy related-protein expression
level in each group as determined by western blotting. (A)
Representative western blots are shown. Lane 1, blank group; lane
2, model group; lane 3, 3-MA group; lane 4, DEX group. (B) Relative
gray values for LC3-II/I, ATG5/GAPDH, Rab7/GAPDH and LAMP1/GAPDH.
*P<0.05 vs. the blank group; #P<0.05 vs. the model
group. LC3, microtubule-associated protein 1A/1B-light chain 3;
ATG5, autophagy protein 5; LAMP1, lysosome-associated membrane
protein 1; 3-MA, 3-methyladenine; DEX, dexmedetomidine. |
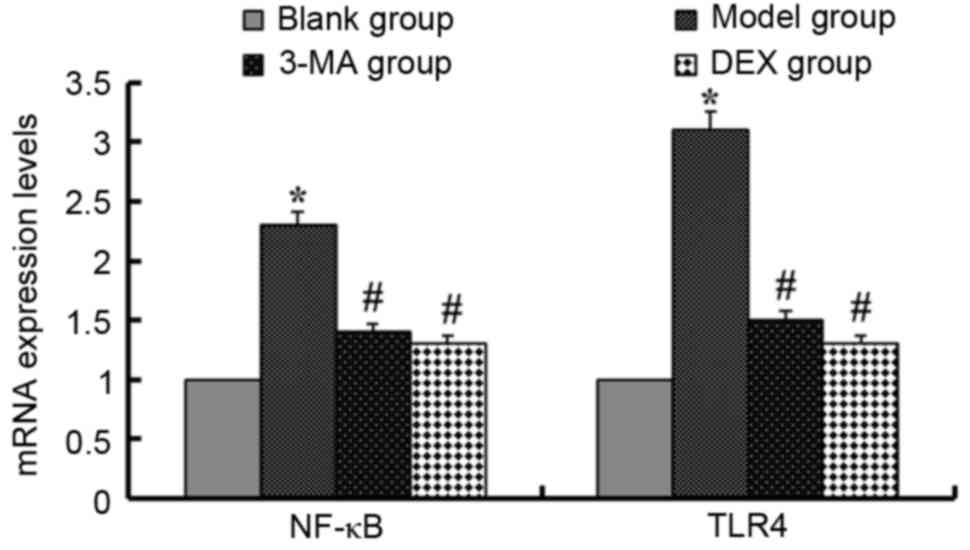
RT-qPCR analysis
In order to detect the effect of 3-MA and DEX on the
autophagy-related signaling pathway, this experiment evaluated the
expression levels of nuclear factor-κB (NF-κB) and Toll-like
receptor 4 (TLR4) using RT-qPCR (Fig.
3). In the LPS-induced ALI model mice, the mRNA expression
levels of NF-κB and TLR4 were upregulated compared with those in
the blank group (P<0.05). Following treatment of the mice with
3-MA, the mRNA expression levels of NF-κB and TLR4 were
downregulated (P<0.05). The mice in the DEX group exhibited
similar downregulation of these mRNAs (P<0.05). The results
shown in Fig. 3 are those for
samples taken on day 1; the results for samples taken on days 3 and
5 (data not shown) were similar to those on day 1.
Discussion
The pathogenesis of ALI is considered to involve
injury of the alveolar epithelium and vascular endothelium.
Neutrophils and leukocytes serve a vital role in the pathogenesis
of ALI/ARDS (2). The high expression
of pro-inflammatory mediators (for example, TNF, IL-1, IL-8 and
IL-6) is considered a direct manifestation of cellular injury
(14). Furthermore, numerous studies
have indicated that NF-κB is activated following the exposure of an
animal or human body to LPS and activated NF-κB is important in the
regulation of inflammatory mediator transcription (15,16).
Under the stimulation of LPS or TNF-α, neutrophils exhibit
activation of NF-κB, Akt and p38, and this early activation of
neutrophils has been shown to be associated with ventilator time
and treatment modality in patients with ALI (17). MPO is characteristic of neutrophils;
the content of MPO reflects the antioxidant ability of neutrophils
(18). Alveolar macrophages are also
very important in the inflammatory response that leads to cell
damage in ALI; a variety of cytokines are produced by macrophages
that contribute to the initiation of ALI, including TNF-α, IL-6,
IL-1β, IL-8 and interferon-γ (14).
In a previous study of ALI, 3-MA reduced the lung weight
coefficient and content of TNF-α in the BALF, and increased
PaO2 (9). The
anti-inflammatory effect of DEX has been demonstrated in previous
experimental animal models (19,20). The
present study confirmed the anti-inflammatory effects of 3-MA and
DEX.
3-MA, as a PI3K inhibitor, Liu et al
(9) found that 3-MA partly
ameliorated seawater-induced ALI through the inhibition of
autophagy. DEX is a selective α2-adrenergic agonist used for
analgesia and sedation in critically ill patients (21). The mechanism of the protective effect
of DEX on ALI is not clear; however, Xie et al (22) demonstrated that DEX ameliorated
intestinal I/R-induced lung injury via the reduction of autophagy
and apoptosis. Furthermore, Zhang et al (23) revealed that DEX inhibited neuronal
autophagy mediated by activation of the PI3K/Akt/mechanistic target
of rapamycin (mTOR) pathway in the hippocampus. In the present
study, 3-MA and DEX treatment decreased the expression of
autophagy-related proteins and inhibited autophagy.
TLR4 activity participates in cytoplasmic
sequestration and subsequent recycling or degradation by connecting
autophagy to phagocytosis so that autophagy acts as an effector of
TLR4 signaling to eliminate invasive pathogens, apoptotic/dead
cells and debris (24). In a
previous study, TLR4 was demonstrated to act as a negative
regulator of noninfectious lung inflammation induced by
low-molecular-weight hyaluronic acid (25). Furthermore, Doi et al
(26) established an ALI model using
TLR4-mutant (C3H/HeJ) mice and TLR4-wild-type (C3H/HeN) mice, and
the results indicated that C3H/HeJ mice had significantly decreased
expression levels of inflammatory cytokines and were protected
against ALI. It has been reported that TLR4 deficiency not only
inhibits the formation of autophagosomes, but also results in
decreased numbers of autophagosomes in lung tissue (24). On the basis of the present study and
other observations (27), it appears
that activation of TLR4 induces autophagy by inhibiting the
PI3K-Akt-mTOR pathway. Thus, the present study supports the notion
that basal TLR4 activity, particularly TLR4-induced autophagy, is
required for the early and effective clearance of injured or dead
cells, unfolded/misfolded proteins, or debris in injured lung
tissue and for the resolution of chronic inflammation and fibrosis
following tissue injury (24). In
the present study, 3-MA and DEX decreased TLR4 expression, and
resulted in a reduction in autophagosomes, as indicated by the
decreased expression of autophagy-related proteins.
In summary, the present study confirmed that 3-MA
and DEX have comparable effects on ALI; both of them protect
against ALI through reducing the inflammatory response and
inhibiting autophagy-related proteins and the autophagy-related
signaling pathway. The efficacy of 3-MA and DEX in attenuating the
LPS-induced ALI was similar. The results indicate that LPS-induced
ALI was effectively reversed with 3-MA or DEX through the reduction
of inflammation and autophagy, and inhibition of the TLR 4-NF-κB
pathway.
Acknowledgements
The present study was funded by the National Natural
Science Foundation of China (grant no. 81271390) and the Science
and Technology Project of Shenzhen (grant no.
JCYJ20140416122812032).
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
3-MA
|
3-methyladenine
|
|
DEX
|
dexmedetomidine
|
|
LPS
|
lipopolysaccharide
|
|
ALI
|
acute lung injury
|
|
MPO
|
myeloperoxidase
|
References
|
1
|
Wang L, Chen JM, Wang B, Wu DQ, Li H, Lu
H, Wu H and Chai Y: Protective effect of quercetin on
lipopolysaccharide-induced acute lung injury in mice by inhibiting
inflammatory cell influx. Exp Biol Med (Maywood). 239:1653–1662.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Herold S, Gabrielli NM and Vadász I: Novel
concepts of acute lung injury and alveolar-capillary barrier
dysfunction. Am J Physiol Lung Cell Mol Physiol. 305:L665–L681.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Matthay MA and Howard JP: Progress in
modelling acute lung injury in a pre-clinical mouse model. Eur
Respir J. 39:1062–1063. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
de Haro C, Martin-Loeches I, Torrents E
and Artigas A: Acute respiratory distress syndrome: Prevention and
early recognition. Ann Intensive Care. 3:112013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Griet M, Zelaya H, Mateos MV, Salva S,
Juarez GE, de Valdez GF, Villena J, Salvador GA and Rodriguez AV:
Soluble factors from Lactobacillus reuteri CRL1098 have
anti-Inflammatory effects in acute lung injury induced by
lipopolysaccharide in mice. PLoS One. 9:e1100272014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhao LL, Hu GC, Zhu SS, Li JF and Liu GJ:
Propofol pretreatment attenuates lipopolysaccharide-induced acute
lung injury in rats by activating the phosphoinositide-3-kinase/Akt
pathway. Braz J Med Biol Res. 47:1062–1067. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ryter SW, Nakahira K, Haspel JA and Choi
AM: Autophagy in pulmonary diseases. Annu Rev Physiol. 74:377–401.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Levine B and Kroemer G: Autophagy in the
pathogenesis of disease. Cell. 132:27–42. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Liu QP, Zhou DX, Lin P, Gao XL, Pan L and
Jin FG: Participation of autophagy in acute lung injury induced by
seawater. Exp Lung Res. 39:441–452. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sen V, Güzel A, Şen HS, Ece A, Uluca U,
Söker S, Doğan E, Kaplan İ and Deveci E: Preventive effects of
dexmedetomidine on the liver in a rat model of acid-induced acute
lung injury. Biomed Res Int. 2014:6218272014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wu Q, Li R, Soromou L, Chen N, Yuan X, Sun
G, Li B and Feng H: p-Synephrine suppresses
lipopolysaccharide-induced acute lung injury by inhibition of the
NF-kB signaling pathway. Inflamm Res. 63:429–439. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Karim M, Kanazawa T, Daigaku Y, Fujimura
S, Miotto G and Kadowaki M: Cytosolic LC3 ratio as a sensitive
index of macroautophagy in isolated rat hepatocytes and H4-II-E
cells. Autophagy. 3:553–560. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yang KY, Arcaroli JJ and Abraham E: Early
alterations in neutrophil activation are associated with outcome in
acute lung injury. Am J Respir Crit Care Med. 167:1567–1574. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Minhajuddin M, Fazal F, Bijli KM, Amin MR
and Rahman A: Inhibition of mammalian target of rapamycin
potentiates thrombin-induced intercellular adhesion molecule-1
expression by accelerating and stabilizing NF-kappa B activation in
endothelial cells. J Immunol. 174:5823–5829. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wang S, Li Y, Fan J, Wang Z, Zeng X, Sun
Y, Song P and Ju D: The role of autophagy in the neurotoxicity of
cationic PAMAM dendrimers. Biomaterials. 35:7588–7597. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hu Y, Liu J, Wu YF, Lou J, Mao YY, Shen HH
and Chen ZH: mTOR and autophagy in regulation of acute lung injury:
A review and perspective. Microbes Infect. 16:727–734. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Xiao H, Heering P, Hu P, Liu Z, Zhao M,
Aratani Y, Maeda N, Falk RJ and Jennette JC: Antineutrophil
cytoplasmic autoantibodies specific for myeloperoxidase cause
glomerulonephritis and vasculitis in mice. J Clin Invest.
110:955–963. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yang CL, Tsai PS and Huang CJ: Effects of
dexmedetomidine on regulating pulmonary inflammation in a rat model
of ventilator-induced lung injury. Acta Anaesthesiol Taiwan.
46:151–159. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Can M, Gul S, Bektas S, Hanci V and
Acikgoz S: Effects of dexmedetomidine or methylprednisolone on
inflammatory responses in spinal cord injury. Acta Anaesthesiol
Scand. 53:1068–1072. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gertler R, Brown C, Mitchell DH and
Silvius EN: Dexmedetomidine: A novel sedative-analgesic agent. Proc
(Bayl Univ Med Cent). 14:pp. 13–21. 2001; View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Xie C, Li Y, Liang J, Xiao J, Zhao Z and
Li T: The effect of dexmedetomidine on autophagy and apoptosis in
intestinal ischemia reperfusion-induced lung injury. Zhonghua Jie
He He Hu Xi Za Zhi. 38:761–764. 2015.(In Chinese). PubMed/NCBI
|
|
23
|
Zhang MH, Zhou XM, Gao JL, Wang KJ and Cui
JZ: PI3K/Akt/mTOR pathway participates in neuroprotection by
dexmedetomidine inhibits neuronic autophagy following traumatic
brain injury in rats. Int J Res Med Sci. 2:1569–1575. 2014.
View Article : Google Scholar
|
|
24
|
Yang HZ, Wang JP, Mi S, Liu HZ, Cui B, Yan
HM, Yan J, Li Z, Liu H, Hua F, et al: TLR4 activity is required in
the resolution of pulmonary inflammation and fibrosis after acute
and chronic lung injury. Am J Pathol. 180:275–292. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhao H, Leu SW, Shi L, Dedaj R, Zhao G,
Garg HG, Shen L, Lien E, Fitzgerald KA, Shiedlin A, et al: TLR4 is
a negative regulator in noninfectious lung inflammation. J Immunol.
184:5308–5314. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Doi K, Ishizu T, Tsukamoto-Sumida M,
Hiruma T, Yamashita T, Ogasawara E, Hamasaki Y, Yahagi N, Nangaku M
and Noiri E: The high-mobility group protein B1-Toll-like receptor
4 pathway contributes to the acute lung injury induced by bilateral
nephrectomy. Kidney Int. 86:316–326. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yen YT, Yang HR, Lo HC, Hsieh YC, Tsai SC,
Hong CW and Hsieh CH: Enhancing autophagy with activated protein C
and rapamycin protects against sepsis-induced acute lung injury.
Surgery. 153:689–698. 2013. View Article : Google Scholar : PubMed/NCBI
|