Introduction
Spinal fracture is a clinical disease that
frequently occurs, characterized by a wide range of incidence and
wide population distribution, which has the highest incidence rate
in the elderly (1,2). Spinal fractures caused by osteoporosis
and trauma can generally be diagnosed by clinical medical history
combined with imaging examination, and surgery dominates in its
treatment (3). The occurrence site
of spinal fracture is closely related to the operation difficulty,
so the operation should be performed as soon as possible under the
anesthesia of patients using rapid-onset anesthetics with good
effects, reducing the pain and anxiety of patients, and increasing
the success rate of the operation (4). Sevoflurane and propofol are two most
commonly-used anesthetics. Cao et al (5) found that sevoflurane has a small
blood-gas partition coefficient, its concentration in blood is easy
to be controlled and it, as a new anesthetic, can exert an
anesthetic effect through inhibition of N-methyl-D-aspartate (NMDA)
receptors, with higher safety, which can provide effective
anesthesia for the elderly and children; at the same time, its poor
solubility of blood tissues leads to rapid onset of induced
anesthesia. Propofol, as a potent general anesthetic, has the
advantages of rapid onset, short recovery time and few
side-effects, and is widely used in preoperative sedation
anesthesia of clinical patients (6).
De Conno et al (7) found that
anesthetics can reduce the patient's pain index and inflammatory
response, so the choice of appropriate anesthetics is essential.
The study of Visvabharathy et al (8) found that propofol can reduce the impact
of operation on patients' cognitive function, but there has been no
research on the differences in effects of propofol and sevoflurane
anesthesia on pain index, inflammatory factors and cognitive
function of patients during operation. In this study, the effects
of propofol and sevoflurane anesthesia on pain index, inflammatory
response and cognitive function of patients with spinal fractures
were analyzed, and the anesthetic effects of propofol and
sevoflurane on patients with spinal fractures were evaluated.
Patients and methods
Patients
A total of 82 patients with spinal fractures treated
in the Orthopedics Department of Jining First People's Hospital
(Jining, China) from January 2015 to January 2017 were selected,
and all patients were diagnosed with spinal compression fractures
[American Society of Anesthesiologists (ASA) grade I–II] via spinal
magnetic resonance (MR) conventional scan. The above eligible
patients were randomly divided into two groups, the propofol group
(Group P, n=41) and the sevoflurane group (Group S, n=41). In Group
P, there were 22 males and 19 females aged (53.7±18.9) years. In
Group S, there were 23 males and 18 females aged (52.1±19.8) years.
The patients enrolled had basically normal liver and kidney
functions, and had no serious auditory, visual or central nervous
system diseases before operation. Patients with mini-mental state
examination (MMSE) score <24 points, other wasting diseases,
chronic inflammation or inadaptation to sevoflurane and propofol
were eliminated. The groups of patients enrolled were given the
same preoperative and postoperative nursing and treatment measures.
The operation was performed by the same physician. Patients signed
the informed consent, and all clinical and pathological data of
patients during hospitalization were retained. The differences in
age, sex and course of disease were not statistically significant
between the groups of patients. This study was approved by the
ethics committee of Jining First People's Hospital. Signed written
informed consents were obtained from all participants before the
study.
Anesthesia process
Before anesthesia, all patients received
intramuscular injection of 0.1 mg/kg midazolam (Jiangsu Nhwa
Pharmaceutical Co., Ltd., Xuzhou, China), and intravenous injection
of 0.5 mg/kg atropine (Dongying Tiandong Pharmaceutical Co., Ltd.,
Dongying, China) and 0.1 g/kg dilantin (New Asiatic Pharmaceutical,
Dongguan, China) and a multi-function monitor (GE Healthcare,
Buckinghamshire, UK) was connected during operation to monitor
physiological indexes of all patients, followed by tracheal
intubation. The anesthesia for patients in Group P was induced with
1 mg/kg propofol (Xi'an Libang Pharmaceutical Co., Ltd., Xi'an,
China) and maintained at a dose of 6 mg/kg/h. Before induced
anesthesia in patients in Group S, the air storage bag was emptied
and the oxygen flow rate was adjusted to 8 l/min, sevoflurane was
filled for 1 min, and patients were asked to take a deep breath,
fasten the mask and keep a deep breath until the disappearance of
eyelash reflex in patients, indicating the successful induced
anesthesia. At 3 min after ventilation, tracheal intubation was
performed and anesthesia machine was connected for mechanical
ventilation for patients. Two groups of patients were treated with
continuous intravenous pumping of 0.2 µg/kg/min remifentanil
(Yichang Humanwell Healthcare, Yichang, China) for induced
anesthesia. During operation, patients in both groups were
intravenously injected with 0.15 mg/kg cisatracurium (Dongying
Tiandong Pharmaceutical) intermittently to maintain muscle
relaxation. The injection of muscle relaxant was terminated half an
hour before the end of the operation, and anesthetics were
withdrawn during suture. During the operation, the depth of
anesthesia of patients was monitored using bispectral index (BIS);
the cannula could be removed when patients could hear and respond
to the doctor's instructions and the spontaneous respiratory rate
had reached 16–22 times/min; patients were sent back to the ward
when they met the requirements of recovery room.
Pain index evaluation in perioperative
period
Visual analogue scale (VAS) was used to evaluate the
degree of pain in patients at 24 and 48 h after operation. VAS
score: 0 point, no pain; 10 points, intense pain; 0–2 points, good
analgesic effect; 2–4 points, better analgesic effect; and more
than 4 points, poor analgesic effect. The extubation time,
eye-opening time and response time of patients in two groups after
operation were recorded in detail used for evaluation of patients'
recovery after anesthesia. Extubation time: duration from using
anesthetics to removing the tracheal cannula out of the mouth of
patients; eye-opening time: duration from withdrawing anesthetics
to the time when patients responded to external stimulus and
instructions with eyes opened; response time: duration from
withdrawing anesthetics to the time when patients could clearly
answer the physician's questions.
Monitoring of inflammatory
response
The expression of inflammatory factors in serum of
patients in each group after operation were detected using
enzyme-linked immunosorbent assay (ELISA) kits. Arterial blood was
drawn from patients in both groups before operation and at 30 min
and 24 h after operation, placed into the anticoagulant tube, and
centrifuged at 2,400 × g for 20 min at 4°C. Then the supernatant
was collected for the serum. The levels of corresponding
inflammatory factors in serum of patients in each group were
detected using interleukin-6 (IL-6), IL-10β, intercellular adhesion
molecule-1 (ICAM-1) and matrix metalloproteinase-9 (MMP-9) kits,
respectively: The standard substances in kits were added into the
sample plate to prepare the standard curve, and Curve Expert was
used to fit and prepare the standard curve, used as a quantitative
criterion; the serum sample was diluted 10 times with diluent in
the kit, and added into each sample well; the operation was
repeated 3 times for each sample. After the plate was sealed with
sealing membrane, the serum sample was incubated at 37°C for 60
min. The liquid in the well was patted dry, the corresponding
biotin-labeled antibodies were added, and the plate was sealed,
followed by incubation at 37°C for 90 min. The liquid in the well
was patted dry, and each well was washed with 300 µl washing liquid
for 3 min; then the washing liquid was discarded, 100 µl
avidin-peroxidase complex was added, and the plate was sealed,
followed by incubation at 37°C for 30 min; the waste liquid was
discarded and 200 µl of washing liquid was added. After that, 50 µl
of stop buffer was added to terminate the reaction. The optical
density value of sample in each group was measured at 465 nm, and
the levels of serum IL-6, IL-1β, ICAM-1 and MMP-9 in each group
were calculated using standard curves.
Evaluation of cognitive function
The cognitive functions of patients in the groups
were evaluated using MMSE scale. Before anesthesia, and at 24 and
48 h after operation, the cognitive functions of patients in the
groups were evaluated, and the scores were analyzed. Compared with
that before operation, MMSE score was decreased, and the difference
of more than 2 points indicated that the cognitive function of
patients had declined. The serum S100β concentration in patients in
each group was detected using the ELISA kit, as above. The serum
S100β level was used to evaluate the cognitive function of patients
in each group.
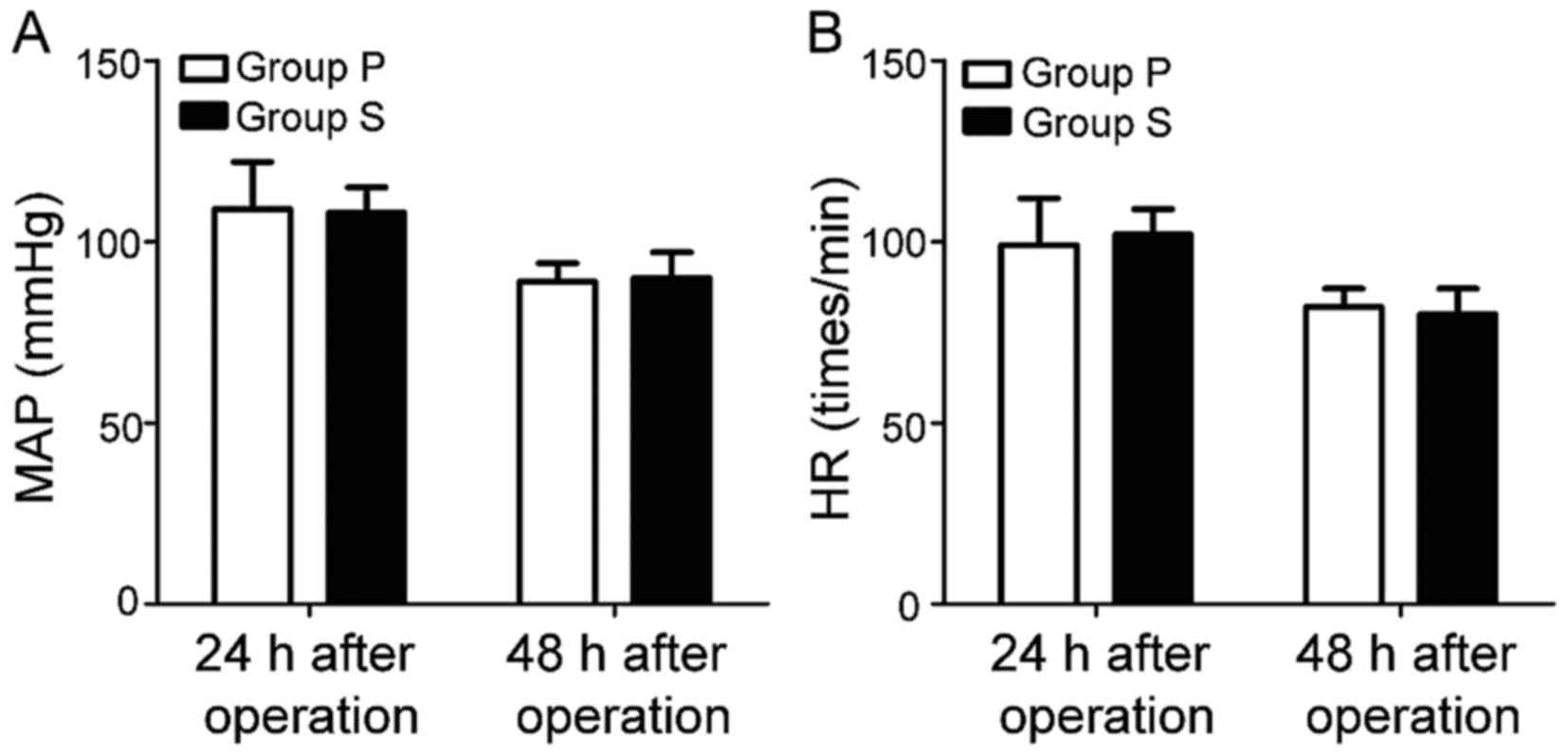
Postoperative evaluation of
physiological indexes
The physiological indexes of patients at 24 and 48 h
after operation were recorded, including mean arterial pressure
(MAP) and heart rate (HR). Changes in physiological indexes of
patients in the two groups after operation were evaluated.
Statistical analysis
Data in the present study are expressed as mean ±
standard deviation, and analyzed using Statistical Product and
Service Solutions 19.0 software (SPSS, Inc., Chicago, IL, USA).
Comparison between groups was done using one-way ANOVA test
followed by post hoc test (least significant difference).
Percentage (%) was used to express the enumeration data and
Chi-square test was used for data analysis. The non-parametric
total rank of independent samples of grade data was used to test. A
value of P<0.05 was considered to indicate a statistically
significant difference.
Results
General data
Each examination was finished for patients in Group
P and Group S within 24 h after admission, and data of patients in
the groups were analyzed. The general data of patients in both
groups are shown in Table I. There
were no statistically significant differences in the sex, age,
years of education, body mass index (BMI) and ASA grade between the
groups of patients (p>0.05). The operations for two groups of
patients were performed by the same doctor, and the operation time,
amount of intraoperative bleeding and anesthesia time of patients
in both groups were recorded in detail. The results showed that the
operation time, amount of intraoperative bleeding and anesthesia
time had no statistically significant difference between the groups
of patients (p>0.05) (Table
II).
 | Table I.General data of patients in each group
(mean ± SD). |
Table I.
General data of patients in each group
(mean ± SD).
| Group | Sex
(male/female) | Age (years) | Years of education
(years) | BMI
(kg/m2) | ASA grade (I/II) |
|---|
| Group P | (22/19) | 53.7±18.9 | 7.5±3.8 | 24.8±2.3 | (28/13) |
| Group S | (23/18) | 52.1±19.8 | 7.3±4.2 | 24.9±2.7 | (30/11) |
| P-value | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 |
| t-test | 0.624 | 0.653 | 0.937 | 0.824 | 0.532 |
 | Table II.Operation conditions (mean ± SD). |
Table II.
Operation conditions (mean ± SD).
| Group | Operation time
(min) | Amount of
intraoperative bleeding (ml) | Anesthesia time
(min) |
|---|
| Group P | 123.6±15.6 | 352.3±73.5 | 159.6±18.8 |
| Group S | 118.9±22.8 | 361.9±50.6 | 155.3±24.2 |
| P-value | >0.05 | >0.05 | >0.05 |
| t-test | 0.530 | 0.852 | 0.735 |
Comparison of recovery time after
operation between two groups of patients
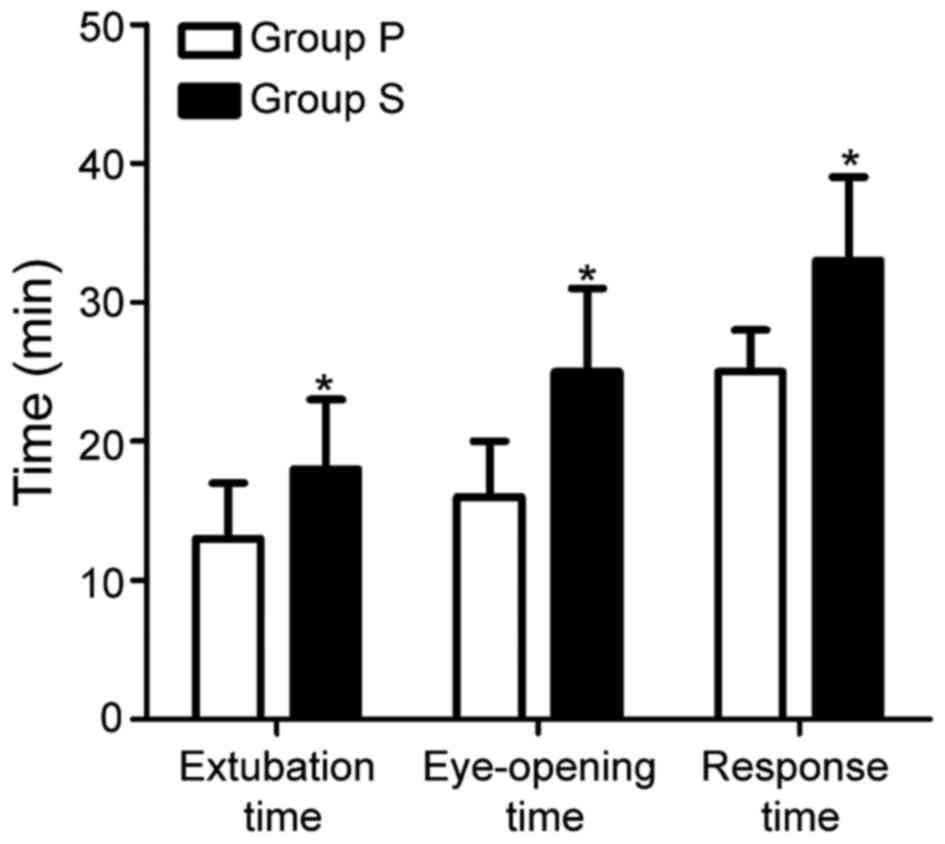
The extubation time, eye-opening time and response
time of patients in the groups after operation were recorded and
analyzed. The results showed that the extubation time, eye-opening
time and response time of patients in Group P were significantly
shorter than those in Group S, and the differences were
statistically significant (p<0.05) (Fig. 1).
Comparison of pain index between two
groups of patients
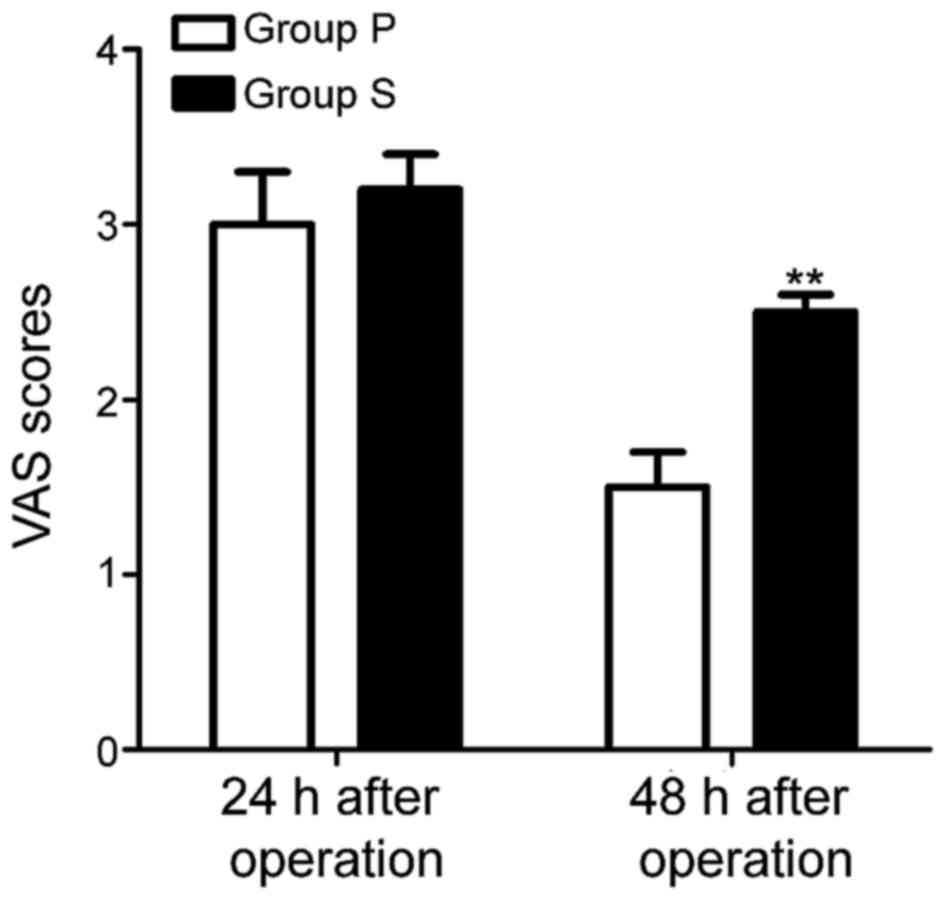
VAS was used to evaluate the pain indexes of
patients in both groups at 24 and 48 h after operation. The results
revealed that there was no statistically significant difference in
VAS score between two groups of patients at 24 h after operation
(p>0.05), and the VAS score of patients in Group P at 48 h after
operation was significantly lower than that in Group S (p<0.05)
(Fig. 2).
Comparison of inflammatory
response
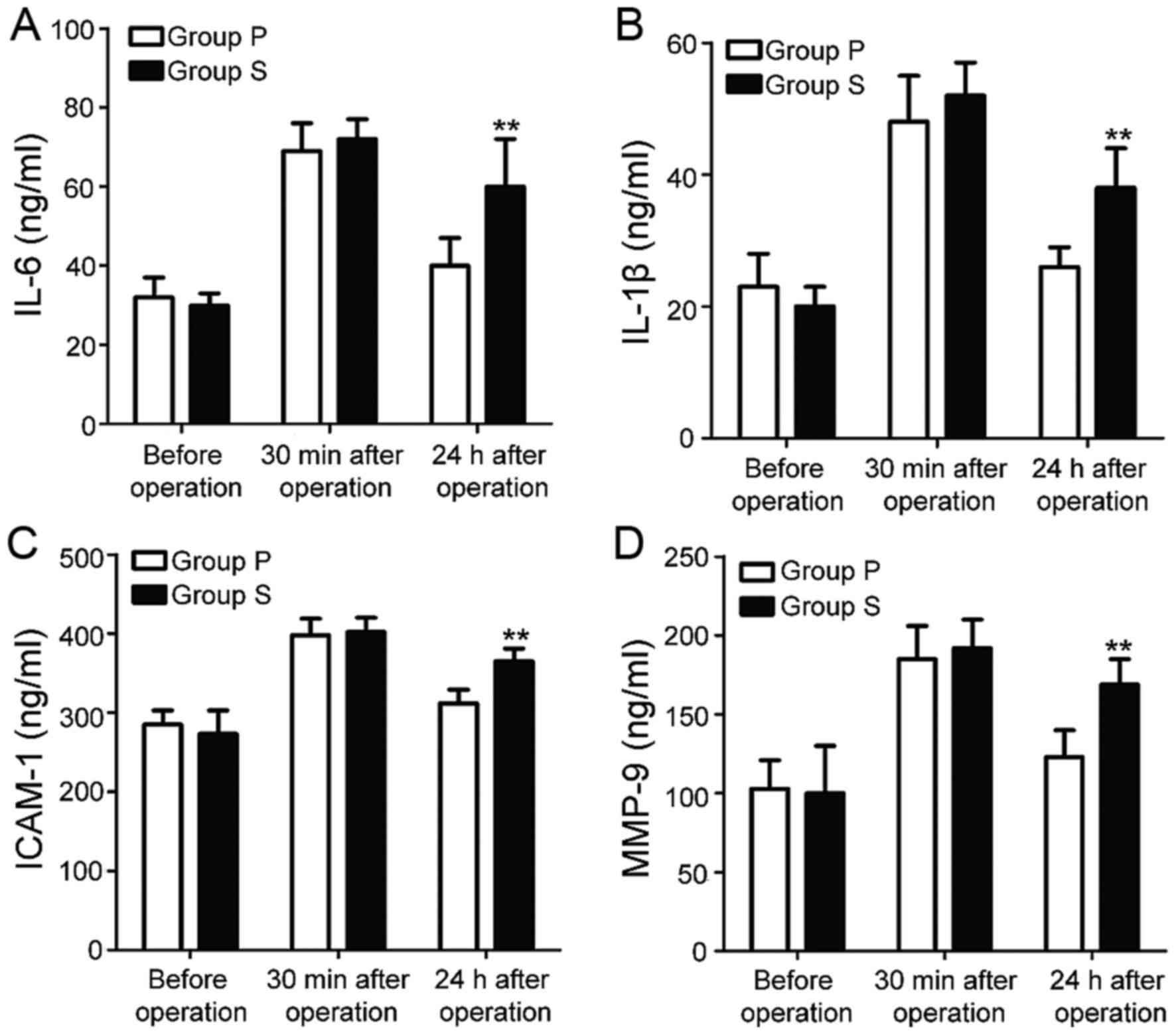
The expression levels of serum inflammatory factors
in patients in the groups were detected before operation and at 30
min and 24 h after operation, respectively. The results revealed
that the levels of serum IL-6, IL-1β, ICAM-1 and MMP-9 in patients
in the groups had no statistically significant differences before
operation and at 30 min after operation (p>0.05); the levels of
serum IL-6, IL-1β, ICAM-1 and MMP-9 in patients in Group P at 24 h
after operation were significantly lower than those in Group S, and
the differences were statistically significant (p<0.01)
(Fig. 3).
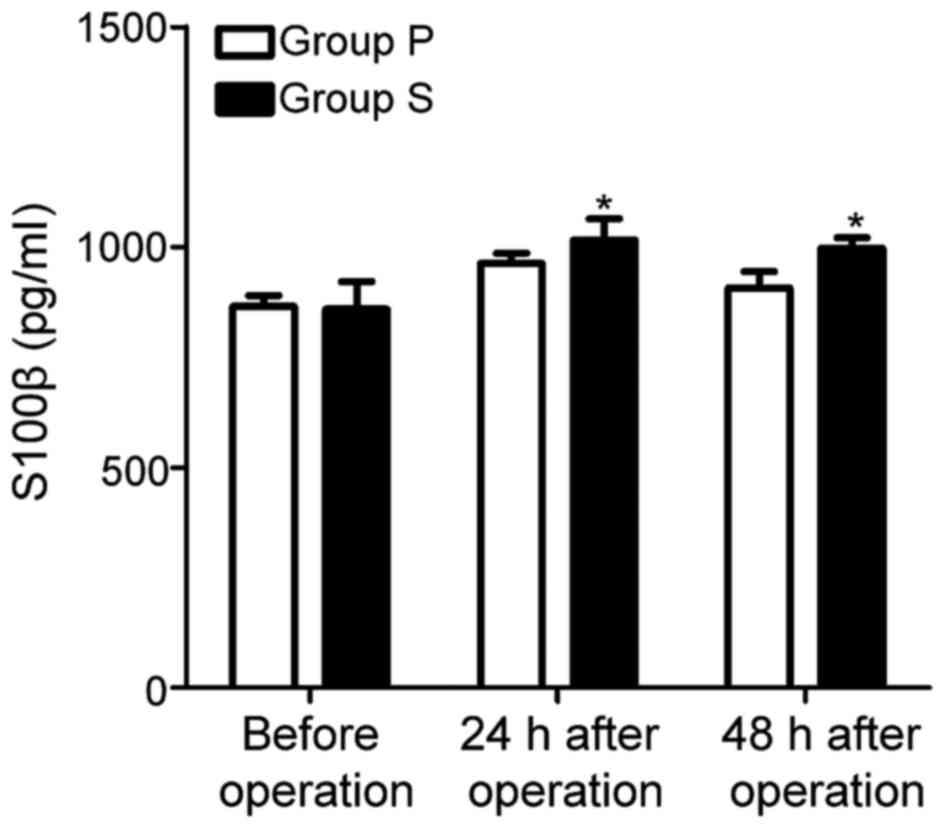
Comparison of cognitive function and
serum S100β concentration after operation
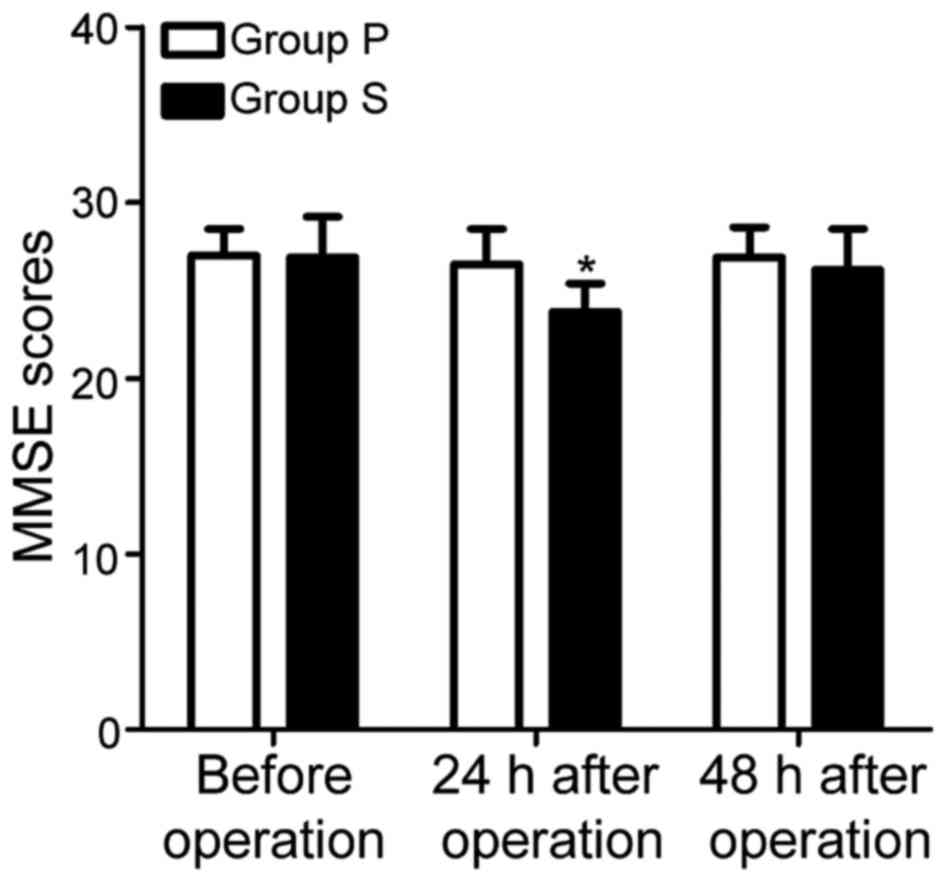
The cognitive functions of patients in two groups
before operation and at 24 and 48 h after operation were evaluated
using MMSE scale. As shown in Fig.
4, there was no statistically significant difference in the
MMSE score between two groups of patients before the operation
(p>0.05); at 24 h after operation, the MMSE score of patients in
Group S was lower than that in Group P (p<0.05), and the
difference was more than 2 points compared with that after
operation; the MMSE scores of patients in Group P and Group S at 48
h after operation had no statistically significant difference
(p>0.05); the serum S100β concentrations in patients in the
groups before operation and at 24 and 48 h after operation were
detected using ELISA kit. The results showed that there was no
statistically significant difference in the serum S100β
concentration between two groups of patients before operation; the
serum S100β concentrations of patients in Group S at 24 and 48 h
after operation were significantly lower than those in Group P
(p<0.05) (Fig. 5).
Postoperative evaluation of
physiological indexes
The physiological indexes of patients in the groups
were recorded at 24 and 48 h after operation, respectively. The
results showed that there were no statistically significant
differences in MAP and HR at 24 and 48 h after operation between
two groups of patients (p>0.05) (Fig.
6).
Discussion
Surgical operation has become the most common and
effective treatment for spinal fracture, which can significantly
reduce the trauma and pain in patients due to fracture. However,
patients often have different degrees of cognitive impairment after
operation (9). Waterloo et al
(10) found that choosing the
appropriate anesthetics during operation can effectively reduce the
pain index in patients after operation, and benefit the recovery of
patients' cognitive function after operation. Waterloo et al
(11) found that fracture orthopedic
surgery can cause damage to some soft tissues, leading to
endothelial cell infiltration, producing inflammatory response;
reducing the inflammatory response during operation can
significantly increase the success rate of operation and improve
the prognosis of patients. Zhang et al (12) showed that the propofol-induced
anesthesia can significantly reduce the inflammatory response of
patients during operation, obviously inhibiting the release of
inflammatory factors and reducing the infiltration of neutrophils
and eosinophils. Postoperative cognitive impairment is a common
neurological complication of patients after operation, which often
occurs in elderly patients, causing serious damage to the memory,
attention and orientation of patients, and even affecting the life
quality of patients after operation (13). Wang et al (14) found that the incidence rate of
postoperative cognitive dysfunction in patients undergoing thoracic
surgery under general anesthesia is over 10%.
In this study, the effects of propofol and
sevoflurane anesthesia, combined with remifentanil, were compared
on the pain index, inflammatory factors and cognitive function of
patients with spinal fractures, and it was found that both propofol
and sevoflurane had good effects of induced anesthesia, which could
make patients enter the anesthesia state quickly, and reduce the
pain of patients caused by fracture; besides, there was no effect
on physiological indexes of patients after operation with a high
safety factor; however, the VAS score of patients after operation
showed that propofol had a better analgesic effect. Sevoflurane is
characterized by no stimulation against upper respiratory tract as
well as stable and safe anesthetic effect, and propofol has the
advantages of rapid onset of action and good analgesic effect
(15). Moreover, remifentanil
combined with sevoflurane or propofol can significantly reduce the
drug concentration in anesthesia and the incidence rate of adverse
reactions, which can also obtain a good anesthetic effect with
rapid recovery (16). Compared with
sevoflurane, propofol has a strong inhibitory effect on
inflammatory response, which can significantly reduce the levels of
serum inflammatory factors (IL-6 and IL-1β). MMP-9, through
increasing the activity of elastase, can promote the adhesion of
neutrophils and vascular endothelium, and hydrolyze the adhesion
protein and connexin, causing damage to the lung tissues (17). ICAM-1, an intercellular adhesion
molecule, exerts its biological activity by binding to specific
receptors on the surface of vascular endothelial cells, which plays
an important role in promoting the endothelial cell migration. The
study of Zhu et al (18)
found that the serum ICAM-1 and MMP-9 levels in patients with
pneumonia are significantly increased. It was found in this
experiment that the serum ICAM-1 and MMP-9 levels in patients in
Group P were significantly lower than those in Group S, indicating
that propofol can significantly reduce the inflammatory response
caused by the operation. Moreover, this study found that MMSE
scores of patients in both groups were decreased to some degree
after operation, and the concentration of S100β was increased. The
above results suggested that both sevoflurane and propofol
anesthesia can cause a certain degree of cognitive impairment.
Fracture surgery will lead to decreased ratio of ventilation volume
to blood flow in the body of patients to some extent, resulting in
hypoxemia and certain damage to cognitive function in patients;
sevoflurane will block the synaptic transmission of postsynaptic
cholinergic neuron and inhibits the long-term potentiation of
hippocampal synapses, further impairing the cognitive function in
patients (19). Propofol can
directly activate γ-aminobutyric acid receptors, weaken the
synaptic activity, and reduce the cerebrovascular blood flow, thus
causing some damage to cognitive function (20). It was found in this evaluation that
the MMSE score of patients in Group P was significantly higher than
that in Group S, indicating that propofol anesthesia causes less
damage to the cognitive function in patients after operation.
In conclusion, compared with sevoflurane, propofol
has a better analgesic effect used in the induced anesthesia in
operation of patients with spinal fractures, which can effectively
reduce the inflammatory response of patients during operation with
little damage to the cognitive function, so its safety is
significantly higher than that of sevoflurane, and propofol is
worthy of extensive promotion in clinical operation.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
YZ designed the study, collected the data and
prepared the manuscript. HZ analysed the data and revised the
study. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Jining First People's Hospital (Jining, China). Signed written
informed consents were obtained from all participants before the
study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Health Quality Ontario, . Vertebral
augmentation involving vertebroplasty or kyphoplasty for
cancer-related vertebral compression fractures: A systematic
review. Ont Health Technol Assess Ser. 16:1–202. 2016.
|
|
2
|
Yu WY, Lou C, Liu FJ and He DW: Clinical
efficacy of one stage posterior debridement joint graft fixation
for lumbar vertebral fractures in spinal tuberculosis patients with
compression. Eur Rev Med Pharmacol Sci. 20:3161–3167.
2016.PubMed/NCBI
|
|
3
|
Malgo F, Hamdy NAT, Ticheler CHJM, Smit F,
Kroon HM, Rabelink TJ, Dekkers OM and Appelman-Dijkstra NM: Value
and potential limitations of vertebral fracture assessment (VFA)
compared to conventional spine radiography: Experience from a
fracture liaison service (FLS) and a meta-analysis. Osteoporos Int.
28:2955–2965. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Cawthon PM, Schousboe JT, Harrison SL,
Ensrud KE, Black D, Cauley JA, Cummings SR, Le Blanc ES, Laughlin
GA, Nielson CM, et al: Osteoporotic fractures in men (MrOS) study
research group: Sex hormones, sex hormone binding globulin, and
vertebral fractures in older men. Bone. 84:271–278. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cao J, Xie H, Sun Y, Zhu J, Ying M, Qiao
S, Shao Q, Wu H and Wang C: Sevoflurane post-conditioning reduces
rat myocardial ischemia reperfusion injury through an increase in
NOS and a decrease in phopshorylated NHE1 levels. Int J Mol Med.
36:1529–1537. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhou L, Wang Z, Zhou H, Liu T, Lu F, Wang
S, Li J, Peng S and Zuo Z: Neonatal exposure to sevoflurane may not
cause learning and memory deficits and behavioral abnormality in
the childhood of Cynomolgus monkeys. Sci Rep. 5:111452015.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
De Conno E, Steurer MP, Wittlinger M,
Zalunardo MP, Weder W, Schneiter D, Schimmer RC, Klaghofer R, Neff
TA, Schmid ER, et al: Anesthetic-induced improvement of the
inflammatory response to one-lung ventilation. Anesthesiology.
110:1316–1326. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Visvabharathy L, Xayarath B, Weinberg G,
Shilling RA and Freitag NE: Propofol increases host susceptibility
to microbial infection by reducing subpopulations of mature immune
effector cells at sites of infection. PLoS One. 10:e01380432015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Katzman WB, Vittinghoff E, Kado DM, Lane
NE, Ensrud KE and Shipp K: Thoracic kyphosis and rate of incident
vertebral fractures: The fracture intervention trial. Osteoporos
Int. 27:899–903. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Waterloo S, Nguyen T, Ahmed LA, Center JR,
Morseth B, Nguyen ND, Eisman JA, Søgaard AJ and Emaus N: Important
risk factors and attributable risk of vertebral fractures in the
population-based Tromsø study. BMC Musculoskelet Disord.
13:1632012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Waterloo S, Søgaard AJ, Ahmed LA, Damsgård
E, Morseth B and Emaus N: Vertebral fractures and self-perceived
health in elderly women and men in a population-based
cross-sectional study: The Tromsø Study 2007–08. BMC Geriatr.
13:1022013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhang JQ, Xu WY and Xu CQ: Neonatal
propofol and etomidate exposure enhance inhibitory synaptic
transmission in hippocampal cornus ammonis 1 pyramidal neurons.
Chin Med J (Engl). 129:2714–2724. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mu DL, Li LH, Wang DX, Li N, Shan GJ, Li
J, Yu QJ and Shi CX: High postoperative serum cortisol level is
associated with increased risk of cognitive dysfunction early after
coronary artery bypass graft surgery: A prospective cohort study.
PLoS One. 8:e776372013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang R, Chen J and Wu G: Variable lung
protective mechanical ventilation decreases incidence of
postoperative delirium and cognitive dysfunction during open
abdominal surgery. Int J Clin Exp Med. 8:21208–21214.
2015.PubMed/NCBI
|
|
15
|
Papadopoulos G, Karanikolas M,
Liarmakopoulou A, Papathanakos G, Korre M and Beris A: Cerebral
oximetry and cognitive dysfunction in elderly patients undergoing
surgery for hip fractures: A prospective observational study. Open
Orthop J. 6:400–405. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sclar DA: Remifentanil, fentanyl, or the
combination in surgical procedures in the United States: Predictors
of use in patients with organ impairment or obesity. Clin Drug
Investig. 35:53–59. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kim YH, Kwon HJ and Kim DS: Matrix
metalloproteinase 9 (MMP-9)-dependent processing of βig-h3 protein
regulates cell migration, invasion, and adhesion. J Biol Chem.
287:38957–38969. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zhu PP, Yuan SG, Liao Y, Qin LL and Liao
WJ: High level of intercellular adhesion molecule-1 affects
prognosis of patients with hepatocellular carcinoma. World J
Gastroenterol. 21:7254–7263. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhang X, Zhou Y, Xu M and Chen G:
Autophagy is involved in the sevoflurane anesthesia-induced
cognitive dysfunction of aged rats. PLoS One. 11:e1535052016.
|
|
20
|
Sato C, Sekiguchi A, Kawai M, Kotozaki Y,
Nouchi R, Tada H, Takeuchi H, Ishida T, Taki Y, Kawashima R and
Ohuchi N: Postoperative structural brain changes and cognitive
dysfunction in patients with breast cancer. PLoS One.
10:e1406552015. View Article : Google Scholar
|