Introduction
At present, intraoperative computed tomography and
magnetic resonance imaging (MRI) examination results are used as
objective evidence for evaluating the presence of a residual tumor
during pituitary adenoma resection surgery via the
trans-nasal-sphenoidal approach, especially for the pituitary
macroadenomas that have invaded the upper sella turcica or
cavernous sinus. These examinations improve tumor resection and
cure rates. However, intraoperative MRI images may be influenced by
blood clots, collapsed tumor cavities and hemostatic materials;
which affects the evaluation of residual tumors, especially for
small residual tumors within the sella turcica. In addition,
special surgical instruments and an operating room are needed for
intraoperative MRI, which is expensive; therefore, this is not
commonly conducted (1–9). Following trans-nasal-sphenoidal
pituitary tumor resection, it may not be possible to observe the
internal structure of the tumor cavity under microscopy and
conventional endoscopy due to the depression of the diaphragma
sellae or bleeding from the tumor cavity; therefore it may not be
clearly and accurately evaluated whether residual tumors are
present in the tumor cavity (9).
In the last decade, the application of routine
endoscopic techniques in surgery for pituitary adenoma has been
rapidly developed due to its characteristics of close lighting,
wide field of vision and production of high quality images, as well
as improved outcomes and fewer complications; traits which have
been recognized by many neurosurgeons (10–18). The
extended transsphenoidal endoscopic technique has certain
advantages in processing lesions in the midline of the skull base
such as clival chordoma, cystic craniopharyngioma and tuberculum
sellae meningiomas (19–23). It has previously been reported that
the use of endoscopic techniques in the treatment of lesions in the
region of the lateral skull base such as Meckel's cavity and the
petroclival region also achieved satisfactory results (24–27). An
endoscope is often used to accommodate for the blind spots of the
microscope, and a microscope may also make up for shortcomings of
the endoscope, such as the two-dimensional image, image deformation
and the space occupied by the endoscope itself. The application of
the diving endoscopic technique in surgery for pituitary adenoma
has been reported previously (28,29).
This makes up for the shortcomings of the microscope and
conventional endoscope, in which, due to tumor cavity bleeding or
hemorrhage of the cavernous sinus, microstructures in the tumor
cavity may not be clearly observed under microscopy or conventional
endoscopy. This combined technique may directly determine the
presence of residual tumors in the tumor cavity, providing an
objective basis in evaluating the resection extent of pituitary
adenoma. In the present study, the diving endoscopic technique has
been applied in 37 patients who underwent pituitary adenoma
resection surgery via the trans-nasal-sphenoidal approach, which is
reported below.
Materials and methods
Clinical data
From October 2011 to July 2014, a total of 37
patients (17 male, 20 female; age range 28–70 years) with pituitary
adenoma from the Department of Neurosurgery in Beijing Boai
Hospital (Beijing, China) were treated by applying the diving
endoscopic technique. The inclusion criteria for using
trans-nasal-sphenoidal approach were as follows: i) Tumors that had
developed above the suprasellar level did not exceed the level of
the interventricular foramen; ii) tumors that had developed above
the suprasellar level did not exceed 2 cm in midline; and iii) the
advancing tumor did not exceed the tuberculum sellae level.
Among these 37 patients, according to the
pre-opration pituitary related hormone levels, 15 patients
exhibited prolactin-secreting adenoma, 14 patients exhibited
nonfunctioning pituitary adenoma, 3 patients exhibited
adrenocorticotropic hormone-secreting adenoma, and 5 patients
exhibited growth hormone (GH)-secreting adenoma. Among the 5
patients with GH type, 4 patients had recurrent pituitary adenoma,
whereas 1 patient exhibited pituitary adenoma apoplexy.
Furthermore, among the 37 patients with pituitary adenoma, 3
patients had micro pituitary adenoma, 29 patients had large
pituitary adenoma, and 5 patients had giant pituitary adenoma.
Furthermore, 5 patients underwent tumor resection via the extended
trans-nasal-sphenoidal approach.
The clinical symptoms exhibited by patients are as
follows: Simple headache (n=2), simple amenorrhoea and lactation
(n=2), simple decreased visual acuity (n=12), simple acromegalic
face change (n=3), headache with decreased visual acuity (n=4),
headache with acromegalic face changes (n=1), headache and eye
movement disorder with decreased visual acuity (n=1), decreased
visual acuity with amenorrhea and lactation (n=4), decreased visual
acuity with acromegaly (n=1), progressive obesity and elevated
blood pressure (n=2), obesity and breast development (n=1),
asymptomatic (n=1) and sexual function decline (n=3) The present
study was approved by the Beijing Boai Hospital, China
Rehabilitation Research Centre. Written informed consent was
provided by all patients.
Surgical methods
Initially, a unilateral trans-nasal-sphenoidal
approach was set under a surgical microscope, and tumor resection
was conducted under microscope or endoscope. The structure in the
tumor cavity was observed by applying the diving endoscopic
technique following confirmation of complete resection of the
tumor.
This approach was typically set at the left side of
the nasal cavity, however, if the tumor is clearly at the left
side, the right side was selected. For tumors that had obviously
invaded the cavernous sinus, extended trans-nasal-sphenoidal
approach for tumor resection was set at the ipsilateral nasal
cavity, and part of the middle turbinate was removed for lateral
expansion. The patient was placed in the supine position, the
surgeon stood at the right side of the patient, the patient's body
was situated close to one side of the surgeon and the head was
slightly turned to the right. The scopes of the lateral wall of the
sphenoidal sinus, the bone and dura of the sellar base, and the
cavernous sinus, which were to be opened, were determined according
to the size and location of the tumor; thus, resection surgery was
conducted under microscopy or endoscopy. When the effect of the
resection under endoscope-assisted microscopy was satisfactory,
observation was conducted by applying the diving endoscopic
technique.
A KARL STORZ LOTTA high-definition endoscope (KARL
STORZ GmbH & Co. KG., Tuttlingen, Germany) was used. Images
were acquired by applying a hard observing endoscope of 0 and 30°,
with a diameter of 2.7 mm and a length of 18 cm. The flow-operating
sheath was externally connected with a 500-ml sterile saline
infusion bag. An infusion pressure bag was used to provide
pressure, which was set at 100 mmHg, in order to provide a
relatively large injection speed and injection pressure. If the
flow-operating sheath was not connected with any suction device,
turbulence would occur and affect the definition of the visual
field. The attractor was directly placed in the nasopharynx to
prevent any disruptions on the imaging effect provided by the
diving endoscopic technique. A cavity was formed following tumor
resection, the endoscope was placed in the tumor cavity, and the
saline bag was pressurized to rapidly fill-up the tumor cavity;
thus, enabling the visual field to clear. Due to the difference in
refractive index between water and air, reducing the focal length
was required at this point.
Patients were followed up for 3 months, and assessed
for visual acuity, transient diabetes insipidus, hypopituitarism,
cerebrospinal fluid leakage and tumor recurrence.
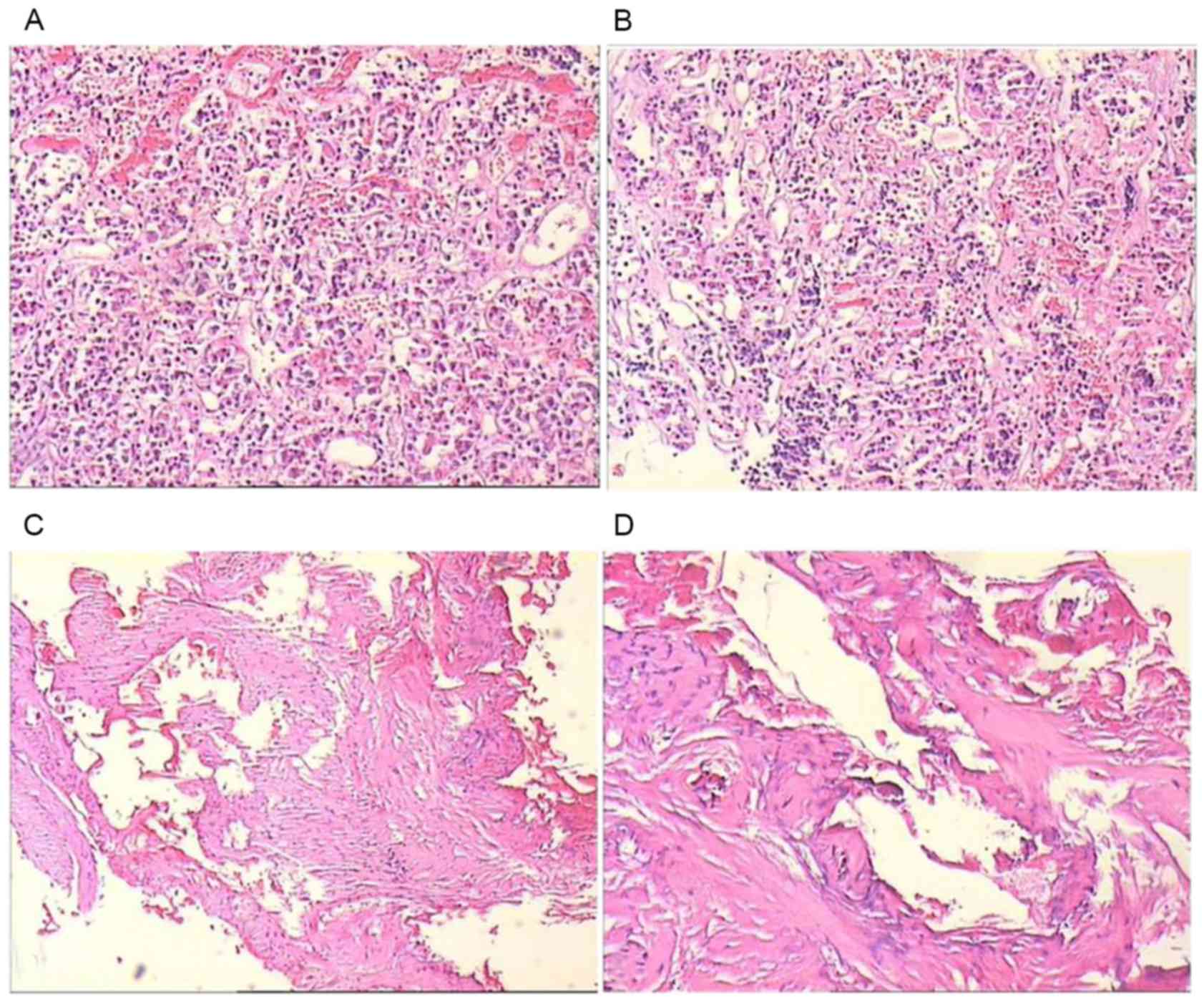
Histopathology
Following resection, suspected tumor specimens were
fixed with 4% formalin at room temperature for ≥6 h. Specimens were
subsequently cut into 3 µm sections and stained with hematoxylin
for 10 min at room temperature, and eosin for 3 min at room
temperature. Samples were then viewed under light microscopy at ×40
and ×100 magnification.
Results and Discussion
The diving endoscopic technique allows surgeons to
directly observe the structure inside the tumor cavity in
high-definition. In the present study, 24 patients had pituitary
macroadenomas or microadenomas that did not invade the cavernous
sinus, and were considered to have undergone successful total
resection; and no tumor residues were observed through the diving
endoscopic technique in any of these patients. It was initially
considered that some of the white lichenoid and fibrous cord-like
tissues in the tumor cavity were remnants of tumors. However,
pathology confirmed that this was not the case. For tumors that
invaded the cavernous sinus, which occurred in 13 patients,
observation was only able to be conducted under an angulation
endoscope through the diving endoscopic technique; i.e., surgery
could not be conducted under an endoscope.
Of the total 37 patients, 1 developed cerebrospinal
leakage following surgery, which was ameliorated via lumbar cistern
drainage for 5 days. No patients developed intracranial infection.
Furthermore, among these patients, 1 had visual acuity of
hand-motion prior to surgery, which did not improve following
surgery; whereas short-term symptoms, such as headache and impaired
vision, were improved in other patients. The mean duration of
surgery was ~1.5 h, which was approximately twice as long than by a
microscope alone. In the present study, it was found that the
application of the diving endoscopic technique did not increase the
incidence of postoperative cerebrospinal leakage and intracranial
infection.
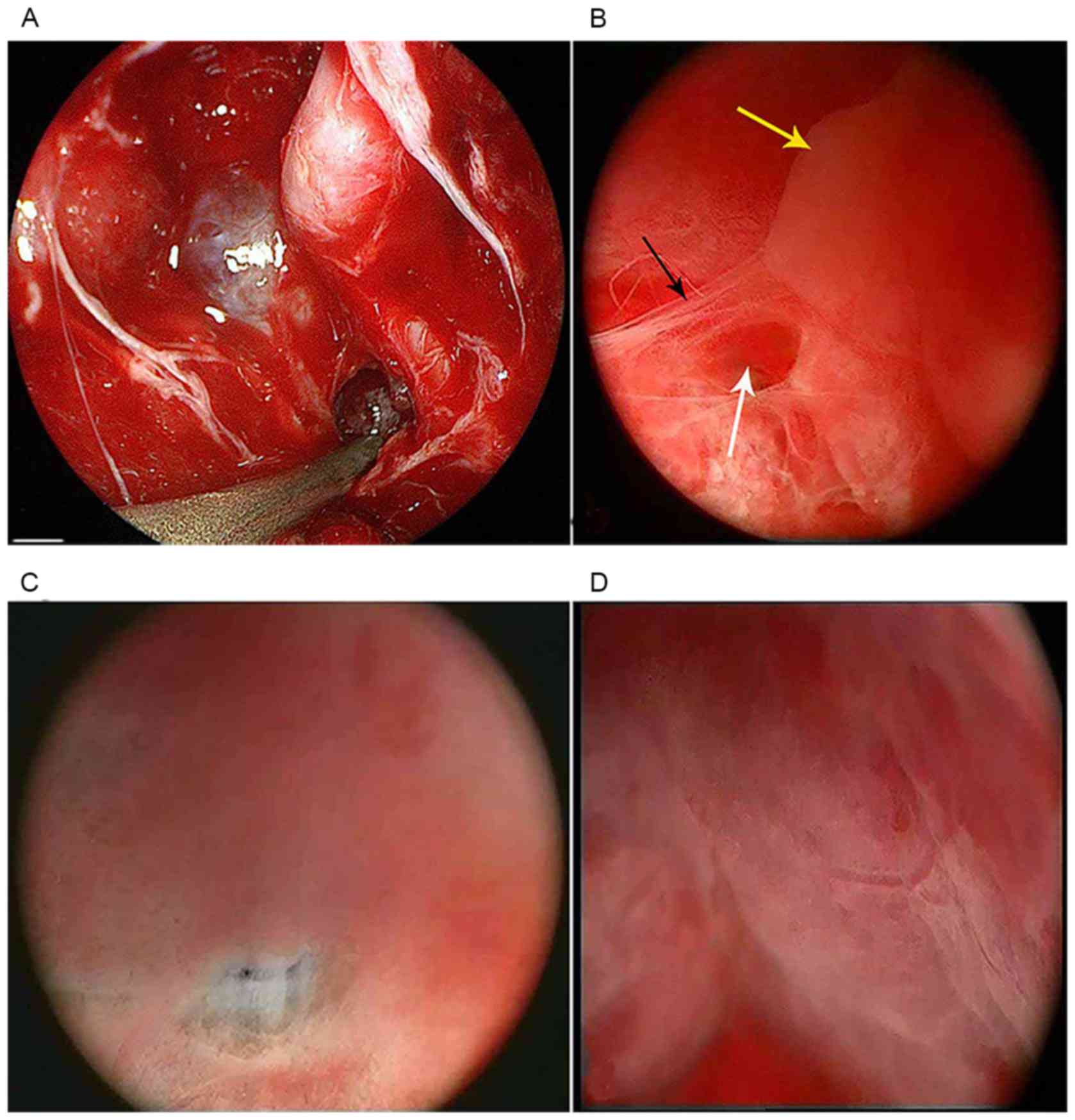
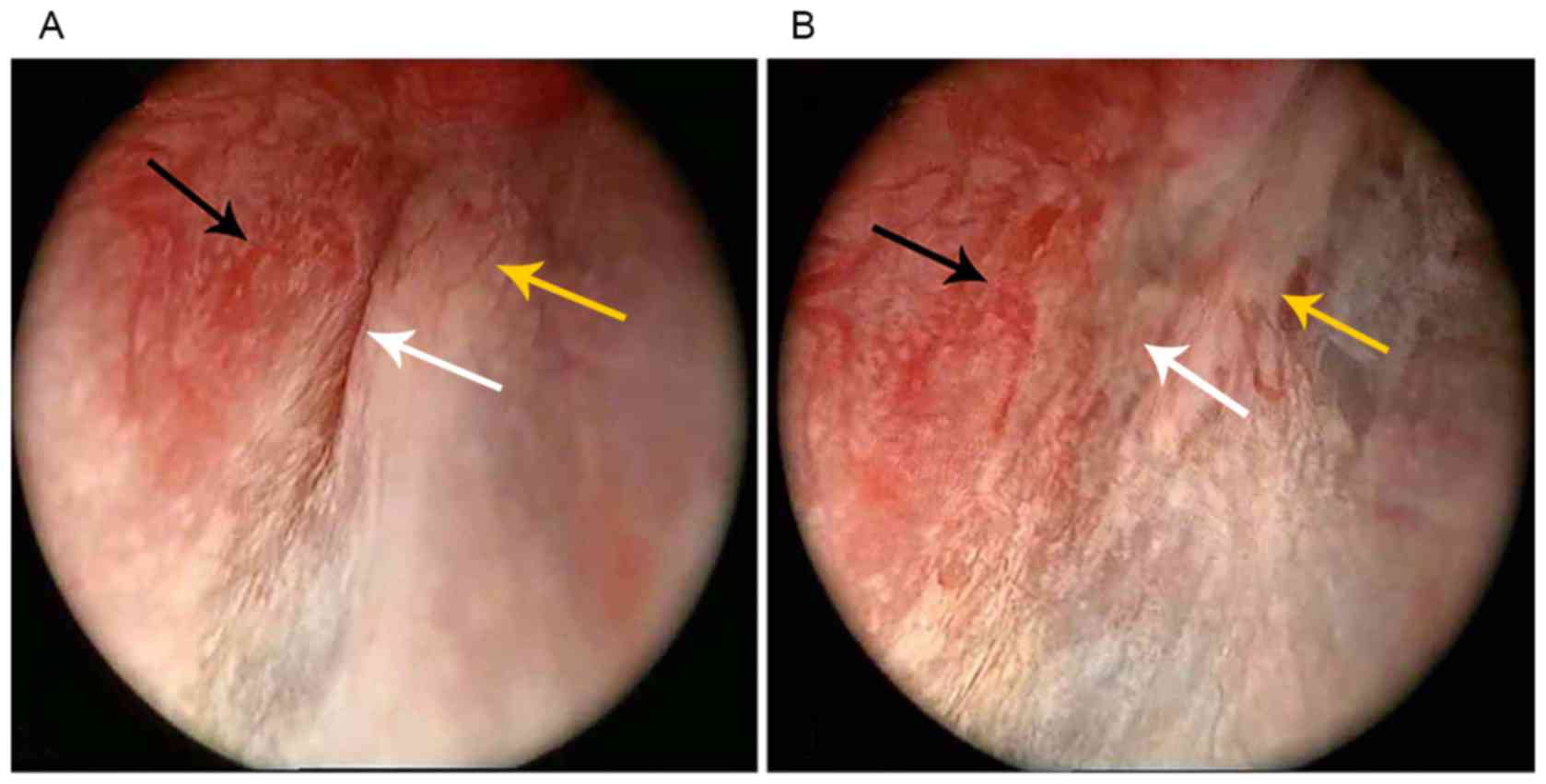
The application of the diving endoscopic technique
in surgery for pituitary adenoma has increased the exposure of the
surgical field. In particular, the application of an angulation
endoscope is able to increase the exposure of the lateral line
(Fig. 1), However, due to continuous
bleeding of the tumor cavity or hemorrhage of the cavernous sinus,
the observation of the local structure of tumor cavity through
conventional endoscopic techniques could not be conducted. Although
there was no active bleeding in the tumor cavity, due to the
reflection effect of blood clots that cover the wound surface and
liquid on the structure surface, the visual field was not clear. In
addition, it was impossible to clearly determine the presence of
residual tumors under direct vision as the sinking diaphragma
sellae was blocked following tumor resection. Senior et al
(29) reported the application of
the diving endoscopic technique in pituitary adenomas in 2005. This
technique allows the endoscope to more clearly present local subtle
structures in tumor cavities.
At present, the objective basis is to determine the
degree of pituitary adenoma resection, which is primarily obtained
through intraoperative MRI. MRI is beneficial, particularly in the
evaluation of residual tumors in the lateral side of the internal
carotid artery within the cavernous sinus, as hemorrhage, collapse
of the tumor cavity and the application of hemostatic material may
affect MRI imaging, which may affect the evaluation of residual
tumors in the sella turcica (1,2,5,8). The
application of the diving endoscopic technique may allow the
surgeon to directly observe the structure in the tumor cavity, and
clearly determine the presence of residual tumors in the sella
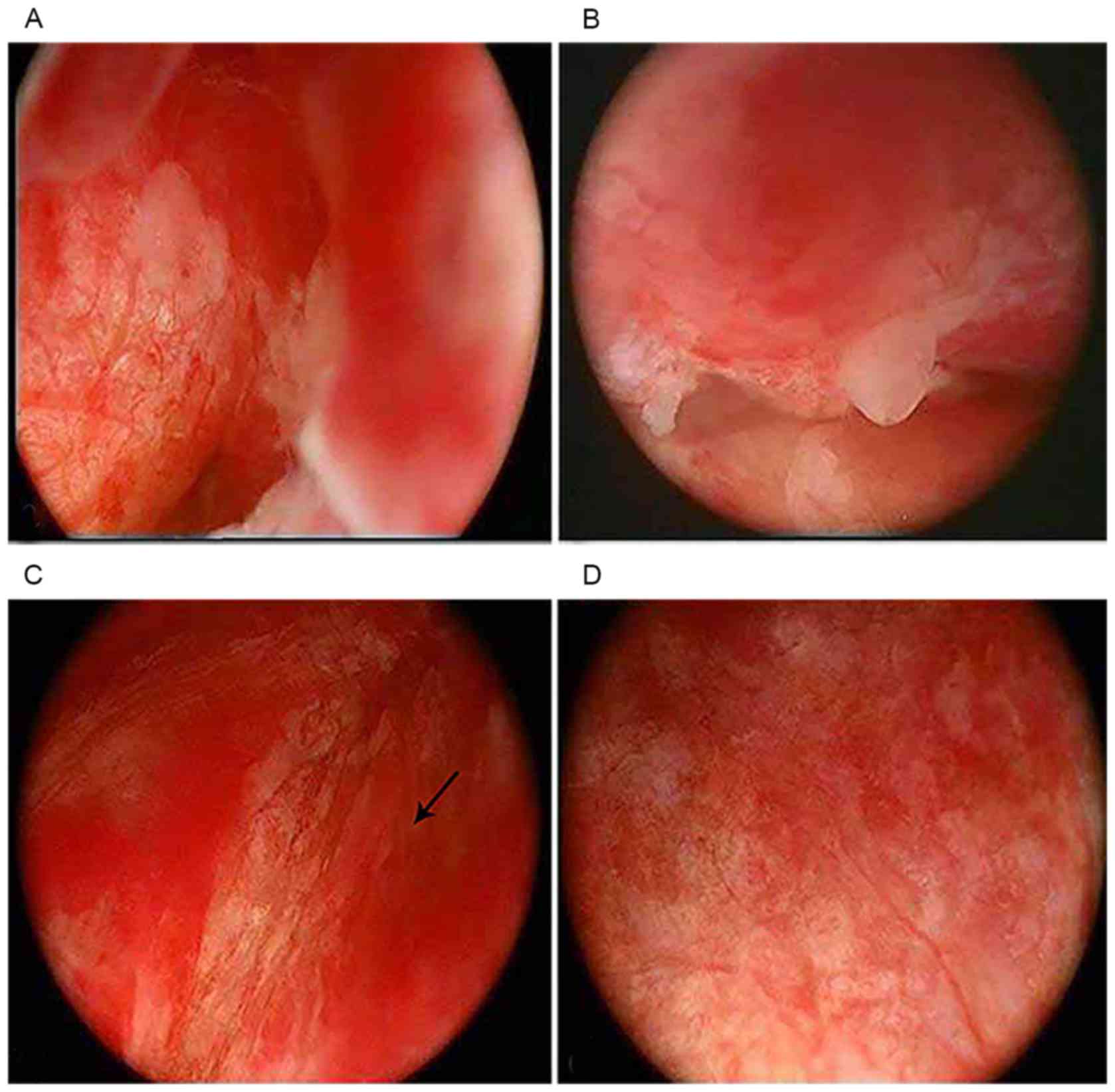
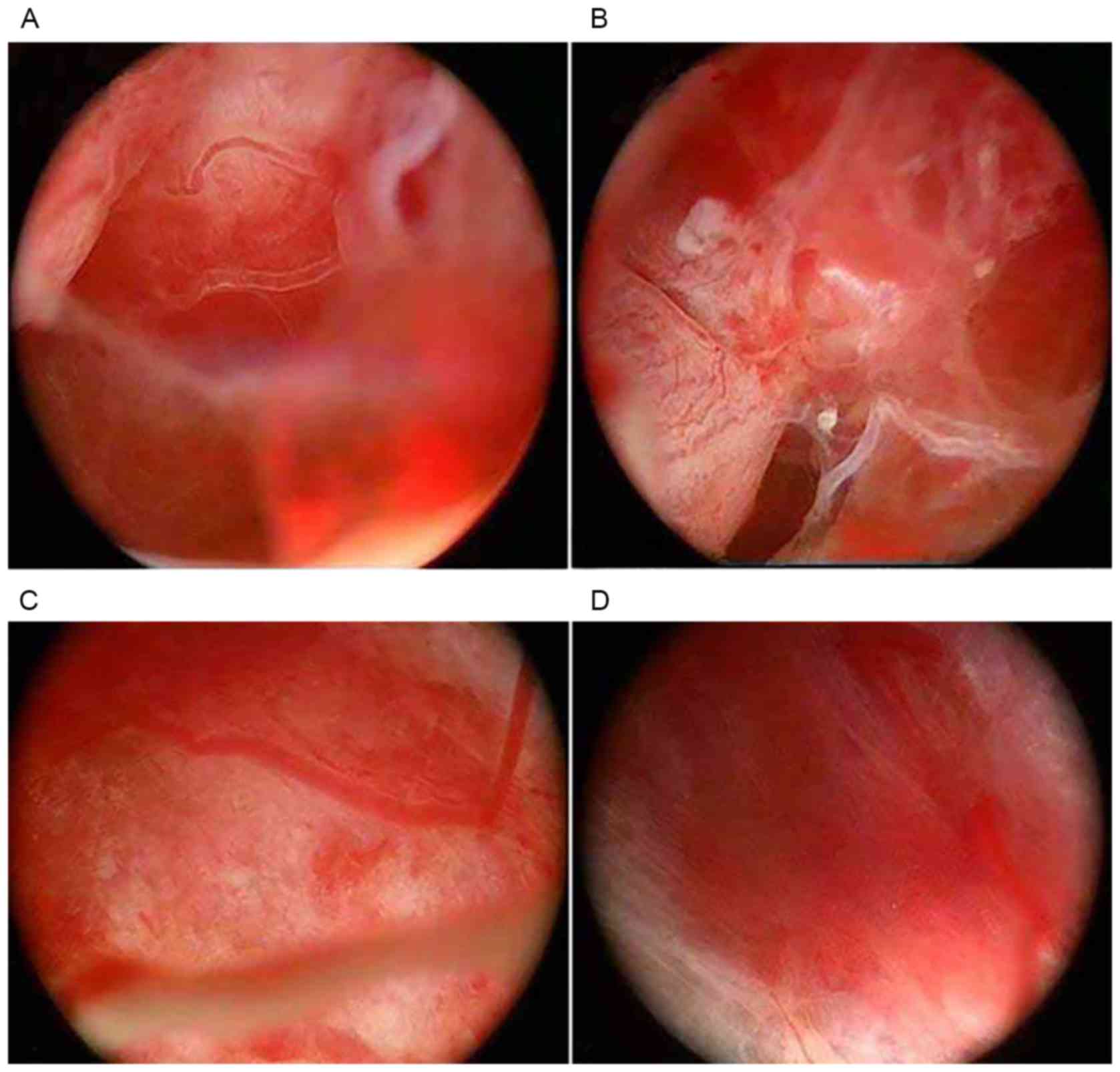
turcica under direct view. In the present study, following the
surgical resection of tumors under a microscope or endoscope, some
white lichenoid or fibrous cord-like structures were observed in
the medial wall of the cavernous sinus, diaphragma sellae fold
returns and suprasellar tissues in some patients (n=6; Fig. 2), through the application of the
diving endoscopic technique. Initially, these were considered to be
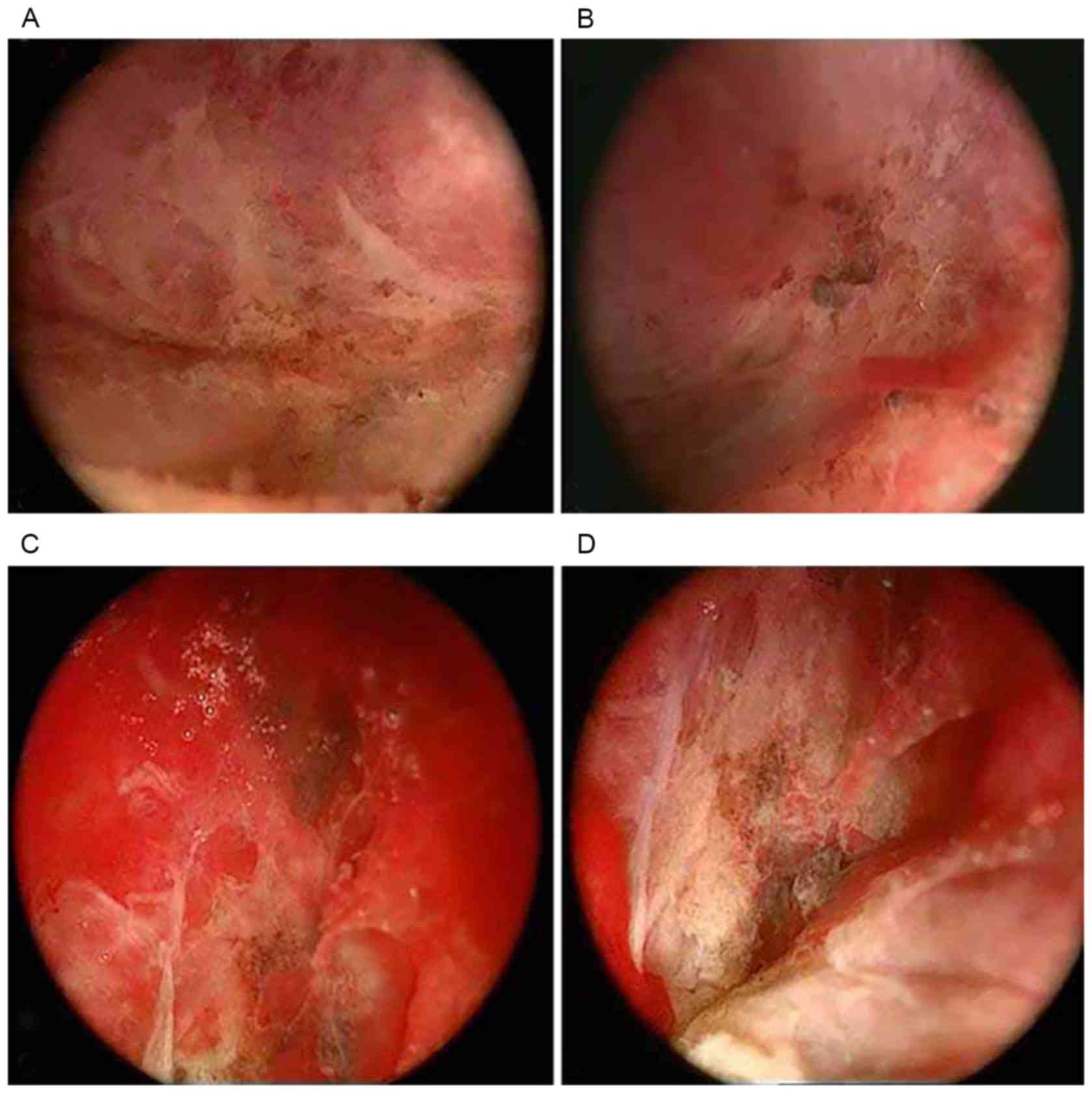
remnants of tumors, and were resected with a straight or elbow
bipolar elctrocoagulation forcep (Fig.
3). Histopathological examination of these specimens was
performed, and confirmed that these were not tumor tissues, but
were venous sinus-like structures formed by small amounts of
pituitary tissues and dense fibrous connective tissues (Fig. 4).
It is possible to determine the extent of tumor
resection under direct vision by applying the diving endoscopic
technique. In addition, this study has identified the following
advantages: i) It is known that the collapse of the diaphragma
sellae into the sella is one of the important factors that
influence tumor resection, and tumor residues often occur in fold
returns of the diaphragma sellae (16). By using changes in water pressure,
the diving endoscopic technique is able to elevate the diaphragma
sellae, in order to observe whether residual tumors in the fold
returns of the diaphragma sellae are present, especially the fold
returns between the diaphragma sellae and medial wall of the
cavernous sinus (Fig. 5). ii) The
pressure of the water injection also has an effect in controlling
bleeding. iii) In reparatory surgery of cerebrospinal leakage, the
endoscope may be used to search for leaks (Fig. 1C). Furthermore, the endoscope may
also be used to explore bleeding points, particularly in the sella
turcica. During the resection of tumors located in the sella
turcica, it is possible to cause intracranial hemorrhage due to
damage to the suprasellar blood vessels. Surgeons are able to
search bleeding points along the surgical channel and decide
whether active measures should be taken (Fig. 6).
In the present study, the following disadvantages of
the diving endoscopic technique were observed. i) Local microscopic
anatomy is complex, and the surgery must be conducted by surgeons
who are familiar to the anatomical structures in the sellar region.
ii) Imaging lacks stereo feeling. When tumors were removed under
the endoscope, they were relatively close to the endoscope, which
led to the difficult operation of the scraper ring and elbow
bipolar electric coagulation under the microscope.
Furthermore, it has been realized through this study
that the following surgical conditions are required for the
application of the diving endoscopic technique. i) First, a tumor
cavity ≥1 cm2 is needed, in which an endoscope may be
placed and the tumor cavity to be observed may be filled up with
physiological saline in a short time. ii) The maintenance of a
clear field of vision requires the rapid replacement of normal
saline for lavage in tumor cavity. The tumor cavity may be rapidly
filled with saline thus quickly replacing cerebrospinal fluid. iii)
Rapid bleeding in the tumor cavity must be prevented; that is, the
replacement of blood-water in the tumor cavity must be faster than
the bleeding.
Endoscopic techniques have increased the present
understanding of the surgery of pituitary adenomas, and have also
lead to some questions. It was detected that during tumor
resection, parts of the medial wall of the cavernous sinus and
pituitary around the tumors were smooth in some patients (Fig. 1D). In addition, the medial wall of
the cavernous sinus around the tumor was rough, uneven, and even
presented with defects in some patients (Fig. 1B). Further studies are required to
determine whether this is associated with tumor invasion.
In conclusion, the diving endoscopic technique
enables the further understanding of the intrasellar local subtle
anatomy in vivo, allows the direct and clear view of the
intrasellar structure and provides more convenient, economical,
objective evidences for determining the resection extent of
intrasellar tumors during the operation.
References
|
1
|
Li J, Cong Z, Ji X, Wang X, Hu Z, Jia Y
and Wang H: Application of intraoperative magnetic resonance
imaging in large invasive pituitary adenoma surgery. Asian J Surg.
38:168–173. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cao L, Chen H, Hong J, Ma M, Zhong Q and
Wang S: Magnetic resonance imaging appearance of the medial wall of
the cavernous sinus for the assessment of cavernous sinus invasion
by pituitary adenomas. J Neuroradiol. 40:245–251. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Alimohamadi M, Sanjari R, Mortazavi A,
Shirani M, Moradi Tabriz H, Hadizadeh Kharazi H and Amirjamshidi A:
Predictive value of diffusion-weighted MRI for tumor consistency
and resection rate of nonfunctional pituitary macroadenomas. Acta
Neurochir (Wien). 156:2245–2252. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Fomekong E, Duprez T, Docquier MA, Ntsambi
G, Maiter D and Raftopoulos C: Intraoperative 3T MRI for pituitary
macroadenoma resection: Initial experience in 73 consecutive
patients. Clin Neurol Neurosurg. 126:143–149. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Jiménez P, Brell M, Sarriá-Echegaray P,
Roldán P, Tomás-Barberán M and Ibáñez J: ‘Intrasellar Balloon
Technique’ in intraoperative MRI guided transsphenoidal endoscopic
surgery for sellar region tumors. Usefulness on image
interpretation and extent of resection evaluation. Technical note.
Acta Neurochir (Wien). 158:445–449. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Coburger J, König R, Seitz K, Bäzner U,
Wirtz CR and Hlavac M: Determining the utility of intraoperative
magnetic resonance imaging for transsphenoidal surgery: A
retrospective study. J Neurosurg. 120:346–356. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tabakow P, Czyz M, Jarmundowicz W and
Lechowicz-Głogowska E: Surgical treatment of pituitary adenomas
using low-field intraoperative magnetic resonance imaging. Adv Clin
Exp Med. 21:495–503. 2012.PubMed/NCBI
|
|
8
|
Kuge A, Kikuchi Z, Sato S, Sakurada K,
Takemura S and Kayama T: Practical use of a simple technique,
insertion of wet cotton pledgets into the tumor resection cavity in
transsphenoidal surgery of pituitary tumors, for a better
comparison between pre-and intraoperative high-field magnetic
resonance images. J Neurol Surg A Cent Eur Neurosurg. 74:366–372.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tosaka M, Nagaki T, Honda F, Takahashi K
and Yoshimoto Y: Multi-slice computed tomography-assisted
endoscopic transsphenoidal surgery for pituitary macroadenoma: A
comparison with conventional microscopic transsphenoidal surgery.
Neurol Res. 37:951–958. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kanter AS, Dumont AS, Asthagiri AR,
Oskouian RJ, Jane JA Jr and Laws ER Jr: The transsphenoidal
approach: A historical perspective. Neurosurg Focus. 18:e62005.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Castelnuovo P, Pistochini A and Locatelli
D: Different surgical approaches to the sellar region: Focusing on
the ‘two nostrils four hands technique’. Rhinology. 44:2–7.
2006.PubMed/NCBI
|
|
12
|
Kassam AB, Thomas A, Carrau RL, Snyderman
CH, Vescan A, Prevedello D, Mintz A and Gardner P: Endoscopic
reconstruction of the cranial base using a pedicled nasoseptal
flap. Neurosurgery. 63 (1 Suppl 1):ONS44–ONS53. 2008.PubMed/NCBI
|
|
13
|
de Divitiis E, Cappabianca P and Cavallo
LM: Endospic transsphenoidal approach: Adaptability of the
procedure to different sellar lesions. Neurosurgery. 51:699–706.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Locatelli D, Rampa F, Acchiardi I, Bignami
M, De Bernardi F and Castelnuovo P: Endoscopic endonasal approaches
for repair of cerebrospinal fluid leaks: Nine-year experience.
Neurosurgery. 58 (4 Suppl 2):ONS-246-ONS-257. 2006.PubMed/NCBI
|
|
15
|
Ferreli F, Turri-Zanoni M, Canevari FR,
Battaglia P, Bignami M, Castelnuovo P and Locatelli D: Endoscopic
endonasal management of non-functioning pituitary adenomas with
cavernous sinus invasion: A 10-year experience. Rhinology.
53:308–316. 2015.PubMed/NCBI
|
|
16
|
Xu T, Peng L, Li H, Wang Y, Liu L, Jiang Y
and Gu Y: The safety and efficacy of endoscopic versus microscopic
surgery for transsphenoidal pituitary adenoma in China: An updated
and cumulative meta-analysis. Zhonghua Yi Xue Za Zhi. 95:3378–3381.
2015.PubMed/NCBI
|
|
17
|
Chu J and Oyesiku N: Endoscopic
transsphenoidal pituitary surgery: Recurrent pituitary adenoma:
3-dimensional operative video. Neurosurgery. 11 Suppl 3:S4672015.
View Article : Google Scholar
|
|
18
|
Cappabianca P, Cavallo LM, de Divitiis O,
de Angelis M, Chiaramonte C and Solari D: Endoscopic endonasal
extended approaches for the management of large pituitary adenomas.
Neurosurg Clin N Am. 26:323–331. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Frank G, Sciarretta V, Calbucci F, Farneti
G, Mazzatenta D and Pasquini E: The endoscopic transnasal
transsphenoidal appaoach for the treatment of cranial base
chordomas and chondrosarcomas. Neurosurgery. 59 (1 Suppl
1):ONS50–ONS57. 2006.PubMed/NCBI
|
|
20
|
Locatelli D, Levi D, Rampa F, Pezzotta S
and Castelnuovo P: Endoscopic approach for the treatment of
relapses in cystic craniopharyngiomas. Childs Nerv Syst.
20:863–867. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kassam A, Snyderman CH, Mintz A, Gardner P
and Carrau RL: Expanded endonasal approach: The rostrocaudal axis.
Part I. Crista galli to the sella turcica. Neurosurg Focus.
19:e32005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kassam A, Snyderman CH, Mintz A, Gardner P
and Carrau RL: Expanded endonasal approach: The rostrocaudal axis.
Part II. Posterior clinoids to the foramen magnum. Neurosurg Focus.
19:e42005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Frank G, Pasquini E, Doglietto F,
Mazzatenta D, Sciarretta V, Farneti G and Calbucci F: The
endoscopic extended transsphenoidal approach for
craniopharyngiomas. Neurosurgery. 59 (1 Suppl 1):NS75–NS83.
2006.
|
|
24
|
Kassam AB, Prevedello DM, Carrau RL,
Snyderman CH, Gardner P, Osawa S, Seker A and Rhoton AL Jr: The
front door to meckel's cave: An anteromedial corridor via expanded
endoscopic endonasal approach-technical considerations and clinical
series. Neurosurgery. 64 (3 Suppl):ONS71–ONS83. 2009.PubMed/NCBI
|
|
25
|
Raza SM, Donaldson AM, Mehta A, Tsiouris
AJ, Anand VK and Schwart TH: Surgical management of trigeminal
schwannomas:defining the role for endoscopic endonasal approaches.
Neurosurg Focus. 37:E172014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Mesquita Filho PM, Ditzel Filho LF,
Prevedello DM, Martinez CA, Fiore ME, Dolci RL, Otto BA and Carrau
RL: Endoscopic endonasal surgical management of chondrosarcomas
with cerebellopontine angle extension. Neurosurg Focus. 37:E132014.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zanation AM, Snyderman CH, Carrau RL,
Gardner PA, Prevedello DM and Kassam AB: Endoscopic endonasal
surgery for petrous apex lesions. Laryngoscope. 119:19–25. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Locatelli D, Canevarl FR, Acchiardl I and
Castelnuovo P: The endoscopic diving technique in pituitary and
cranial base surgery: Technical note. Neurosurgery. 66:E400–E401.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Senior BA, Dubin MG, Sonnenburg RE, Melroy
CT and Ewend MG: Increased role of the otolaryngologist in
endoscopic pituitary surgery: Endoscopic hydroscopy of the sella.
Am J Rhinol. 19:181–184. 2005.PubMed/NCBI
|