Introduction
Supraventricular tachycardia (SVT) is one of the
most common types of arrhythmias in clinical practice, especially
in children (1). SVT mainly develops
from the regions above ventricles, and the increased heart rate is
usually not accompanied with organic changes in heart tissue, and
RR interval and QRS wave detected by ECG were usually normal
(2). The pathogenesis of VST
includes atrioventricular reentrant tachycardia (AVRT) and
atrioventricular nodal reentrant tachycardia (AVNRT). SVT can cause
chest tightness, palpitations embolism and severe tachycardia
ventricular fibrillation, or even life-threatening complications
(3).
As a safe and effective intervention strategy,
radiofrequency ablation has been proven to be effective in the
treatment of arrhythmia (4). With
the improvement of the quality of catheter materials,
radiofrequency ablation is becoming more and more mature, and has
been gradually applied to the radical treatment of SVT (5). However, recurrence after radiofrequency
ablation, can cause physical and mental pain, and increase medical
expenses, and constitutes a great challenge for the application of
this technique (6).
In the present study, the outcomes of radiofrequency
ablation in the treatment of children with SVT were evaluated, and
risk factors for postoperative recurrence were analyzed to provide
references for the reduction of recurrence.
Materials and methods
General information
A total of 312 patients with pediatric SVT were
selected from April, 2011 to March, 2017. The clinical data of the
patients were retrospectively analyzed. The patients were subjected
to radiofrequency ablation, and no organic heart disease was
observed. Family members of the patients signed informed consent.
The study was approved by the Ethics Committee of the Affiliated
Children's Hospital of Xuzhou Medical University (Xuzhou, China).
General information of the patients is listed in Table I.
 | Table I.General information of the
patients. |
Table I.
General information of the
patients.
| Items | Patients n=312 |
|---|
| Male n (%) | 166 (53.21) |
| Female n (%) | 146 (46.79) |
| Age (years) | 3–13 |
| Average age
(years) | 8.36±2.47 |
| Average weight
(kg) | 33.54±3.73 |
| AVRT n (%) | 158 (50.64) |
| AVNRT n (%) | 154 (49.36) |
Preoperative preparation
Preoperative routine examinations, including chest
X-ray, electrocardiogram, echocardiography, coagulation examination
and other tests were performed for the patients. Treatment with
antiarrhythmic drugs was stopped at 5 half-life before the study,
and treatment with anticoagulant drugs was stopped 3 days before
surgery. The patients were not allowed to eat or drink for 6 h
prior to surgery. The puncture sites were cleaned, and antibiotics
were used to prevent infection 30 min prior to surgery. Tilt table
test was performed in a room with soft lights. Heart rate, blood
pressure and other parameters were recorded.
Radiofrequency ablation
For AVNRT mapping and radiofrequency ablation,
anesthesia was performed by sevoflurane inhalation. ECG and the
back electrode plate were connected. After conventional
disinfection, the right internal jugular and the right femoral vein
were punctured to place the sheath, and the catheter was sent to
the right atrium. Discharge (25 w) was performed for 5–10 sec on
the position of 1/3 below the connection live of hex beam electrode
and coronary sinus electrode. The appearance of junctional and
sinus rhythm indicated an effective discharge. The discharge was
extended approximately to 3 min. If the ablation was not
successful, discharge was performed on another target. Heart rate
was monitored during ablation, and intravenous injection of
dexamethasone was administered in case of atrioventricular block.
Discharge was stopped when heart rate returned to normal.
AVRT mapping and radiofrequency ablation: After
conventional disinfection, the right femoral vein and internal
jugular vein were punctured to place the sheath, and ablation
catheter was sent to the left ventricle or right atrium to hook on
the tricuspid annulus. Small A large V wave was mapped to serve as
an ablation target, and discharge (25 v) was performed for 10 sec.
VA separation and disappearance of bypass or reverse transmission
function indicated an effective discharge. Discharge was extended
to 3 min, and heart rhythm was monitored, and appropriate treatment
was performed.
Evaluation indicators
Tilt table test was performed on the first day
before and the second day after radiofrequency ablation. Heart
rate, systolic and diastolic blood pressure in children were
observed. Plasma levels of D-dimer (D-D), platelet α-granule
membrane protein (GMP-140) and thrombin-antithrombin III complex
(TAT) were detected by enzyme-linked immunosorbent assay using kits
provided by Shanghai Sun Biotech Co., Ltd. (Shanghai, China). The
success rate of radiofrequency ablation and recurrence rate of SVT
were measured by intracardiac electrophysiology, and the incidence
of surgical related complications including severe hematoma, severe
pleural effusion, hemothorax and atrioventricular block were
recorded.
Statistical analysis
SPSS 19.0 (SPSS Inc., Chicago, IL, USA) software was
used. Measurement data were expressed as mean ± standard deviation
(false), and comparisons between pre- and post-operative levels
within a group were performed using ANOVA and the post hoc test was
Dunnett's test. Countable data were expressed as rate, and
processed using χ2 test. Comparisons among multiple data
within a group were performed by repeated measurements of variance
analysis. Influencing factors were performed by Logistic regression
analysis. P<0.05 was considered to indicate a statistically
significant difference.
Results
Comparison of heart rate of supine and
upright position before and after treatment
After treatment, the heart rate of the supine
position was not significantly different from that before treatment
(P>0.05), while the heart rate of the upright position was
significantly increased after treatment (P<0.05) (Table II).
 | Table II.Changes in heart rate before and after
ablation (bpm). |
Table II.
Changes in heart rate before and after
ablation (bpm).
| Variables | Before | After | t-value | P-value |
|---|
| Supine position | 71.29±7.43 | 71.84±7.04 | 0.949 | 0.343 |
| Upright position | 80.83±7.34 | 86.78±7.35 | 10.118 | <0.001 |
| 5 min | 82.98±7.15 | 87.43±7.48 | 7.596 | <0.001 |
| 10 min | 83.09±7.27 | 87.67±7.26 | 7.874 | <0.001 |
| 15 min | 81.24±7.46 | 86.87±7.38 | 9.477 | <0.001 |
Comparison of systolic blood pressure
of supine and upright position before and after treatment
Compared with preoperative levels, systolic blood
pressure of supine and upright position were significantly reduced
(Table III).
 | Table III.Comparison of systolic blood pressure
before and after treatment. |
Table III.
Comparison of systolic blood pressure
before and after treatment.
| Variables | Before | After | t-value | P-value |
|---|
| Supine position | 128.26±8.43 | 121.85±8.04 | 9.719 | <0.001 |
| Upright position | 117.85±6.36 | 110.72±6.37 | 13.991 | <0.001 |
| 5 min | 116.98±6.15 | 110.23±6.05 | 13.820 | <0.001 |
| 10 min | 118.46±6.23 | 112.62±6.19 | 11.746 | <0.001 |
| 15 min | 120.56±6.45 | 115.27±6.38 | 10.299 | <0.001 |
Comparison of diastolic blood pressure
of supine and upright position before and after treatment
Compared with preoperative levels, no significant
changes in diastolic blood pressure of supine and upright position
were found after treatment (Table
IV).
 | Table IV.Comparison of diastolic blood pressure
before and after treatment. |
Table IV.
Comparison of diastolic blood pressure
before and after treatment.
| Variables | Before | After | t-value | P-value |
|---|
| Supine position | 77.23±5.43 | 76.87±5.54 | 0.820 | 0.413 |
| Upright position | 75.87±5.32 | 75.78±5.36 | 0.211 | 0.833 |
| 5 min | 75.68±5.19 | 75.43±5.28 | 0.596 | 0.551 |
| 10 min | 76.59±5.24 | 76.67±5.36 | 0.189 | 0.850 |
| 15 min | 77.36±5.48 | 77.87±5.52 | 1.158 | 0.247 |
Comparison of efficacy and recurrence
rate
No significant differences in immediate success
rate, recurrence rate and the incidence of complications were found
between the AVRT and AVNRT groups (P>0.05) (Table V).
 | Table V.Comparison of efficacy and recurrence
rate between AVRT and AVNRT group, n (%). |
Table V.
Comparison of efficacy and recurrence
rate between AVRT and AVNRT group, n (%).
| Groups | Cases | Immediate success
rate | Recurrence rate | Incidence of
complications |
|---|
| AVRT | 158 | 155 (98.10) | 7 (4.43) | 0 (0.00) |
| AVNRT | 154 | 150 (97.40) | 8 (5.19) | 1 (0.65) |
| χ2 |
| 0.001 | 0.003 | 0.001 |
| P-value |
| 0.927 | 0.959 | 0.990 |
Comparison of coagulation function
before and after radiofrequency ablation
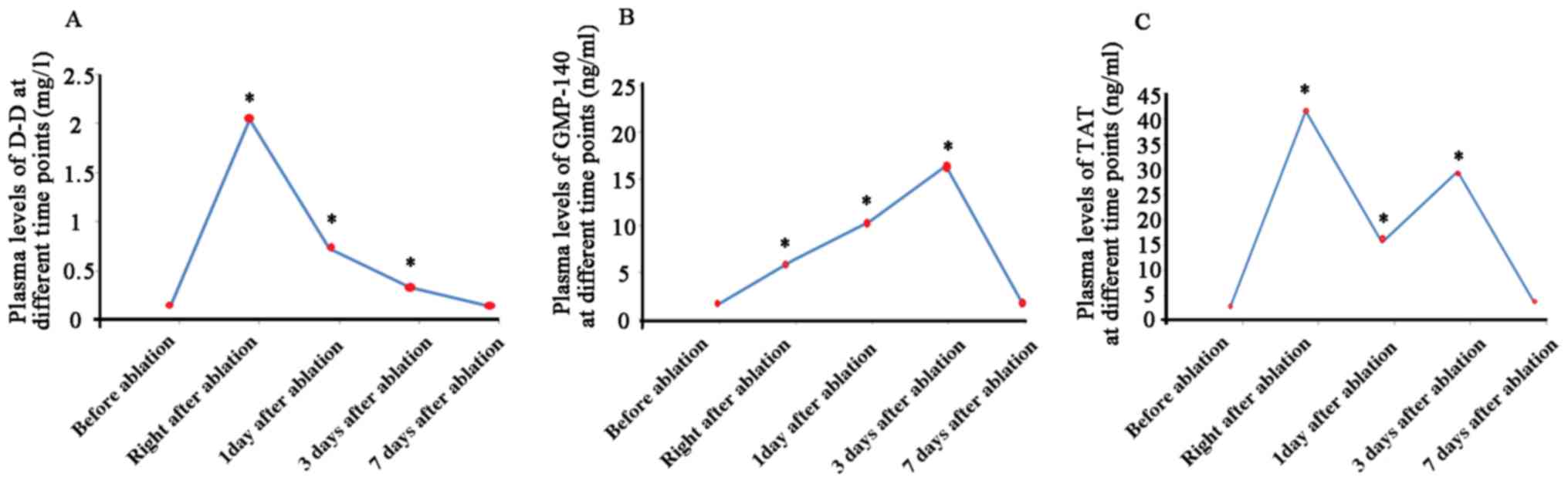
Plasma levels of D-D, GMP-140 and TAT significantly
increased at 1 and 3 days after ablation compared with preoperative
levels. The levels of those factors were decreased on day 7 to
reach normal level (Fig. 1).
Analysis of risk factors for
postoperative recurrence
With postoperative recurrence as a dependent
variable, sex, ablation time, radio frequency current power,
residual slow path and inaccurate targeting were used as
independent variables. Residual slow path (OR=6.718, P=0.005) and
inaccurate targeting (OR=2.815, P=0.007) were proved to be
independent risk factors for the recurrence (Table VI).
 | Table VI.Logistic regression analysis of
factors affecting recurrence after ablation. |
Table VI.
Logistic regression analysis of
factors affecting recurrence after ablation.
| Factors | β | SE | Wald | OR | 95%CI | P-value |
|---|
| Sex | 0.718 | 0.374 | 2.421 | 0.312 | 0.106–0.854 | 0.105 |
| Ablation time | 0.605 | 0.504 | 4.427 | 0.706 | 0.496–0.842 | 0.216 |
| Residual slow
path | 0.567 | 0.636 | 7.703 | 6.718 | 2.075–9.212 | 0.005 |
| Inaccurate
targeting | 0.637 | 0.518 | 5.568 | 2.815 | 1.103–4.046 | 0.007 |
| Radio frequency
current power | 0.156 | 0.442 | 2.713 | 0.783 | 0.275–0.912 | 0.356 |
Discussion
SVR is mostly caused by the reentry mechanism.
Reentrance usually occurs in atrioventricular node, atrium, sinus
node and atrioventricular junction and other parts. As a cause of
rapid arrhythmia, AVRT is caused by the presence of reentry ring
between bypass and normal conduction pathway, and accounts for
approximately 60% of SVT. AVNRT is the formation of AVNRT caused by
the presence of double atrioventricular junction, and AVNRT
accounts for approximately 30% of SVT (7–9).
SVT is usually treated with drugs, such as digitalis
and propafenone injection, and DC shock, but the recurrence rate is
high (10). As a minimally invasive
treatment, radiofrequency ablation has been applied to the
treatment of SVT since 1990s. With the high safety, SVT now has
become a first-line treatment for SVT (11). The principle of radiofrequency
ablation is to heat myocardial tissue through the radio frequency,
so as to destroy focal myocardium (12). In the present study, no significant
differences in immediate success rate, recurrence rate and the
incidence of complications were found between AVRT and AVNRT groups
(P>0.05). This is because radiofrequency ablation can map the
causes of arrhythmia (abnormal reentry and ectopic discharge)
through electrode, and the release of high-frequency current to the
target was performed through ablation catheter to heat the target
tissue (43 to 60°C), so as to denature proteins in myocardial
tissues to cause coagulation necrosis, thus reducing electrical
conduction and achieve the purpose of treatment (13). With the advantages of no radioactive
damage, easy operation and high safety, radiofrequency ablation
will not cause air pressure injury and damages to surrounding
normal myocardial tissue. In addition, the incidence of
postoperative complications and postoperative recurrence rate of
this method are also relatively low (14).
The results of the present study showed that there
was no significant difference in heart rate of the supine position
before and after radiofrequency ablation (P>0.05), while heart
rate of the upright position was significantly increased after
treatment (P<0.05). After treatment, systolic pressures of both
supine and upright position were significantly reduced compared
with the levels before treatment (P<0.05), while no significant
changes in diastolic blood pressure of supine and the upright
position were found (P>0.05). This is because radiofrequency
ablation can easily cause damage to autonomic nerves close to the
endocardium. The autonomic nerves, especially vagus nerve is close
to the myocardial wall and is more sensitive to radiofrequency
ablation, and heart rate usually increases during treatment, and
decline in peripheral vascular resistance and systolic blood
pressure can also occur. By contrast, the area of ablation is
limited, and the impact on blood pressure is not serious (15).
Although radiofrequency ablation is a minimally
invasive surgery, it inevitably causes damage to the body's
coagulation system, leading to the incidence of postoperative
thromboembolism; thus, detection of some markers to diagnose and
prevent thromboembolism is required (16). D-D is a degradation product of
cross-linked fibrin. The content of D-D increases when blood is in
a hypercoagulable state and fibrinolytic activity increases
(17). GMP-140 is a particle surface
membrane protein that is dependent on platelet activation and is
the most sensitive indicator of platelet activation (18). TAT is the product of the link of
serine residue of thrombin to the arginine residue of AT-III
through ester bond. TAT can reflect the coagulation condition in
vivo (19). Results of the
present study showed that the levels of D-D, GMP-140 and TAT
increased at 1 and 3 days after treatment, and decreased 7 days
after treatment to reach normal level. This is because the thermal
effect of radiofrequency ablation can increase local temperature
and activate platelets. Local myocardial necrosis can cause the
release of coagulation factors to accelerate platelet activation.
The presence of radiofrequency ablation can cause damage to
endothelium, leading to platelet aggregation and adhesion, and thus
activate the body's coagulation system. Thus, levels of D-D,
GMP-140 and TAT rapidly increase (20).
Atrioventricular node can be divided into fast and
slow functional pathways. Radiofrequency ablation mainly targets
the slow pathway to improve the success rate of treatment and
reduce recurrence rate (3 to 5%) (21). In the present study, postoperative
recurrence was observed in 15 of 312 cases. Logistic regression
analysis showed that residual slow pathway (OR=6.718, P=0.005) and
inaccurate targeting (OR=2.815, P=0.007) were two independent risk
factors for postoperative recurrence (P<0.05). After
radiofrequency ablation, residual slow pathway can cause shortening
of the refractory period, leading to AVNRT (22). The mapping of bypass pathway is the
key for the success of radiofrequency ablation. Without accurate
targeting, bypass pathway can be damaged by radiofrequency
ablation, so necrosis will happen and recurrence rate will increase
(23).
In summary, the efficacy of radiofrequency ablation
in the treatment of pediatric SVT is clear. Although this treatment
can damage cardiac vagal nerve; thus, the heart rate after ablation
during the course of the tilt table test will increase, but it will
return to normal after a week. Residual slow pathway and inaccurate
targeting were two independent risk factors for postoperative
recurrence.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
CL wrote the manuscript and helped with preoperative
preparation. LJ and ZW performed radiofrequency ablation. LN
contributed to tilt table test. XA analyzed and interpreted ELISA.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
the Affiliated Children's Hospital of Xuzhou Medical University
(Xuzhou, China) and informed consents were signed by the patients
and/or guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bánhidy F, Ács N, Puhó EH and Czeizel AE:
Paroxysmal supraventricular tachycardia in pregnant women and birth
outcomes of their children: A population-based study. Am J Med
Genet A. 167A:1779–1786. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Brembilla-Perrot B, Olivier A, Villemin T,
Manenti V, Vincent J, Moulin-Zinsch A, Lethor JP, Tisserant A,
Marçon F and Marc Jean S: Follow-up of children or teenagers with
paroxysmal supraventricular tachycardia but without preexcitation
syndrome. Arch Cardiovasc Dis. 110:599–606. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chou CP, Lin IC and Kuo KC: A male infant
had subdural effusion and paroxysmal supraventricular tachycardia
during the febrile episode of Kawasaki disease: A case report and
literature review. BMC Pediatr. 16:712016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bends R, Brössner A, Felberbaum R and
Römer T: Myoma in statu nascendi after transcervical radiofrequency
ablation of a transmural uterine leiomyoma. Gynakologische
Endokrinologie. 14:291–294. 2016. View Article : Google Scholar
|
|
5
|
Kuck KH, Brugada J, Fürnkranz A, Metzner
A, Ouyang F, Chun KR, Elvan A, Arentz T, Bestehorn K, Pocock SJ, et
al: FIRE AND ICE Investigators: Cryoballoon or radiofrequency
ablation for paroxysmal atrial fibrillation. N Engl J Med.
374:2235–2245. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhao QX, Zhao YM, Mao L, Shen DL and Zhao
XY: Atrial fibrillation prevalence and atrial vulnerability
analysis in paroxysmal supraventricular tachycardia patients after
radiofrequency ablation. Eur Rev Med Pharmacol Sci. 21:584–589.
2017.PubMed/NCBI
|
|
7
|
Al-Zaiti SS and Magdic KS: Paroxysmal
supraventricular tachycardia: Pathophysiology, diagnosis, and
management. Crit Care Nurs Clin North Am. 28:309–316. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Spanò F, Cereda A, Moreo A, Bonacina E,
Peritore A, Roghi A, Giannattasio C and Pedrotti P: Paroxysmal
supraventricular tachycardia as first manifestation of right atrial
hemangioma during endovascular treatment of intracranial
arteriovenous fistulas. Oncotarget. 6:14060–14064. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kruchina T, Gordeev O, Pushkareva I and
Novik G: P1795 Presyncope and syncope events in pediatric patients
with paroxysmal supraventricular tachycardia. Europace. 19:3972017.
View Article : Google Scholar
|
|
10
|
Shaker H, Jahanian F, Fathi M and Zare M:
Oral verapamil in paroxysmal supraventricular tachycardia
recurrence control: A randomized clinical trial. Ther Adv
Cardiovasc Dis. 9:4–9. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sung JY, Baek JH, Jung SL, Kim JH, Kim KS,
Lee D, Kim WB and Na DG: Radiofrequency ablation for autonomously
functioning thyroid nodules: A multicenter study. Thyroid.
25:112–117. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Han J, Xu J and He Y: Anterior mitral
leaflet perforation: A rare complication of radiofrequency ablation
for paroxysmal supraventricular tachycardia. Clin Case Rep.
5:1414–1415. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Qian LY, Zou H, Che XD, Wang LH, Cen XX,
Xu Q and Qu BM: Comparison of radiofrequency catheter ablation for
paroxysmal supraventricular tachycardia guided by three dimensional
navigation with X-ray. Zhonghua Yi Xue Za Zhi. 96:2821–2824.
2016.(In Chinese). PubMed/NCBI
|
|
14
|
Seizer P, Bucher V, Frische C, Heinzmann
D, Gramlich M, Müller I, Henning A, Hofbeck M, Kerst G, Gawaz M and
Schreieck J: Efficacy and safety of zero-fluoroscopy ablation for
supraventricular tachycardias. Use of optional contact force
measurement for zero-fluoroscopy ablation in a clinical routine
setting. Herz. 41:241–245. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yu M, Yi K, Zhou L and Tan X: Pregnancy
increases heart rates during paroxysmal supraventricular
tachycardia. Can J Cardiol. 31:820.e52015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Menéndez JJ, Verdú C, Calderón B,
Gómez-Zamora A, Schüffelmann C, de la Cruz JJ and de la Oliva P:
Incidence and risk factors of superficial and deep vein thrombosis
associated with peripherally inserted central catheters in
children. J Thromb Haemost. 14:2158–2168. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Man YN, Wang YN, Hao J, Liu X, Liu C, Zhu
C and Wu XZ: Pretreatment plasma D-dimer, fibrinogen, and platelet
levels significantly impact prognosis in patients with epithelial
ovarian cancer independently of venous thromboembolism. Int J
Gynecol Cancer. 25:24–32. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cenni E, Granchi D, Verri E, Cavedagna D,
Gamberini S, Falsone G and Pizzoferrato A: CD62, thromboxane B2,
and beta-thromboglobulin: A comparison between different markers of
platelet activation after contact with biomaterials. J Biomed Mater
Res. 36:289–294. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Csuka D, Veszeli N, Imreh É, Zotter Z,
Skopál J, Prohászka Z, Varga L and Farkas H: Comprehensive study
into the activation of the plasma enzyme systems during attacks of
hereditary angioedema due to C1-inhibitor deficiency. Orphanet J
Rare Dis. 10:1322015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Izumi N, Asahina Y, Noguchi O, Uchihara M,
Kanazawa N, Itakura J, Himeno Y, Miyake S, Sakai T and Enomoto N:
Risk factors for distant recurrence of hepatocellular carcinoma in
the liver after complete coagulation by microwave or radiofrequency
ablation. Cancer. 91:949–956. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kovalev A, Filatov A, Bockeria O and
Bockeria L: P317 The usefulness of radiofrequency ablation of
atrial tachycardias in young patients with significant paroxysmal
atrial fibrillation. Europace. 19:512017. View Article : Google Scholar
|
|
22
|
Reddy CD, Silka MJ and Bar-Cohen Y: A
comparison of AV nodal reentrant tachycardia in young children and
adolescents: Electrophysiology, ablation, and outcomes. Pacing Clin
Electrophysiol. 38:1325–1332. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cooper RM, Shahzad A, Hasleton J,
Digiovanni J, Hall MC, Todd DM, Modi S and Stables RH:
Radiofrequency ablation of the interventricular septum to treat
outflow tract gradients in hypertrophic obstructive cardiomyopathy:
A novel use of CARTOSound® technology to guide ablation.
Europace. 18:113–120. 2016. View Article : Google Scholar : PubMed/NCBI
|