Introduction
The incidence of atherosclerosis (AS) has been on
the increase in recent years. As is a chronic inflammatory disease
of blood vessels, which poses a great threat to human health
(1–4). The process from the hyperlipidemia at
first to AS involves the accumulation of lipid on the arterial
intima, occurrence of fibrous lesions and formation of
atherosclerotic plaques, resulting in vascular stenosis, decreased
elasticity and increased thickness of vascular wall, ultimately
causing other serious complications, such as thrombotic disease,
cerebrovascular disease and coronary heart disease. The
pathogenesis is the aggregation of a large number of cytokines,
macrophage-derived foam cells and a variety of chemokines on the
intimal surface, causing endothelial cell lesions and ultimately
leading to the occurrence of AS (5).
Vascular endothelial cell damage is a key factor in inducing
atherosclerotic disease. Under physiological conditions, vascular
endothelial cells can prevent the accumulation of inflammatory
factors on the vascular wall, and reduce the pathological migration
and proliferation of smooth muscle cells, ultimately improving the
occurrence and development of the disease (6). At present, the progression mechanism of
atherosclerotic disease is not fully clarified, but the
inflammatory response of vascular endothelial cells caused by
intravascular lipid accumulation and metabolic disorders is closely
related to the occurrence and development of AS (7,8).
Statins, such as the hydroxymethylglutaryl coenzyme
A reductase inhibitor, can effectively suppress the synthesis of
cholesterol and reduce the serum cholesterol content (9). Rosuvastatin is a new type of statin,
which, not only reduces the content of blood lipids, but also
improves the physiological effect of vascular endothelium (10). However, there is little research on
its effect on the expression of candidate gene polypeptide
N-acetylgalactosaminyltransferase 3 (GALNT3). This study aimed to
investigate the effect of rosuvastatin on the expression of AS
candidate gene GALNT3, to lay a foundation for the clinical
treatment of AS with rosuvastatin.
Materials and methods
Materials and reagents
Rosuvastatin (5 mg/tablet; Lunan Beite
Pharmaceutical Co., Ltd., Linyi, China); nitric oxide (NO),
triglyceride (TG) and total cholesterol (TC) detection kits
(Nanjing Jiancheng Biotechnology Institute, Nanjing, China); rabbit
anti-rat GALNT3 polyclonal antibody and goat anti-rabbit
horseradish peroxidase (HRP)-labeled secondary polyclonal antibody
(cat. nos. 16716-1-AP and SA00001-2; Proteintech; Wuhan Institute
of Biological Products Co., Lts., Wuhan, China); GALNT3 antibody
and horseradish peroxidase (HRP)-labeled secondary antibody
(Proteintech; Wuhan Institute of Biological Products Co., Lts.);
primer synthesis, reverse transcription kit and quantitative PCR
kit (Takara, Dalian, China); bicinchoninic acid (BCA) protein
quantification kit and cell lysis buffer (Beyotime Biotechnology
Research Institute, Nantong, China) were used in this study.
Experimental animals and grouping
Sixty clean Wistar rats weighing 180±10 g, were
randomly divided into the control (n=20), model (AS group, n=20)
and administration (rosuvastatin group, n=20) groups. The rats were
injected with D3.6 million units of vitamin per kilogram of body
weight first, and then fed with high-fat diet (87.8% basal feed,
10% lard oil, 2% cholesterol) for 6 weeks. The rats in the
administration group were fed with high-fat diet every day and
treated with gavage using 1 mg/kg rosuvastatin calcium at the same
time. The study was approved by the Ethics Committee of Jinan
Zhangqiu District Hospital of Traditional Chinese Medicine (Jinan,
China).
Detection of TC, TG and NO levels
After modeling, the blood was taken from the orbital
cavity of rats under anesthesia using the capillary tube. After
coagulation, the blood was centrifuged at 8,000 × g for 10 min, the
upper serum was taken and the serum TG, TC and NO levels were
detected according to the protocol of the kit.
Morphological observation of vascular
tissues
After modeling, the vascular tissues were taken from
the thoracic aorta of rats, and immediately fixed with 4%
paraformaldehyde solution for 48 h, followed by dehydration and
transparency, paraffin embedding, cutting and sticking, dewaxing
and staining, sealing, and preparation into hematoxylin and eosin
(H&E) staining sections. The effect of rosuvastatin on the
morphology of vascular tissues was observed under a microscope
(Olympus Corporation, Tokyo, Japan).
Detection of mRNA expression of GALNT3
via RT-PCR
The vascular tissues were taken from the thoracic
aorta of rats, and the total RNA was extracted. The qualified total
RNA was used as the template to synthesize cDNA via reverse
transcription. The specific reaction conditions were as follows:
Incubation at 42°C for 15 min, incubation at 95°C for 3 min,
cooling on ice and stored at −80°C for subsequent experiment.
Routine amplification was performed according to the primer
sequence in Table I.
 | Table I.RT-PCR primer sequences of GALNT3
mRNA. |
Table I.
RT-PCR primer sequences of GALNT3
mRNA.
| Gene name | Primer sequences |
|---|
| GALNT3 |
F:5′-GTTGCTAGGAGCAACAGTCGCA-3′ |
|
| R:
5′-AGTTCACCGTGGTAGTATTGTAGT-3′ |
| GAPDH | F:
5′-CTCAACTACATGGTCTACATG-3′ |
|
| R:
5′-TGGCATGGACTGTGGTCATGAG-3′ |
Western blot analysis
The vascular tissues were taken from the thoracic
aorta of rats, and the total protein was extracted. Then the
protein concentration was determined and the samples to be tested
were treated. Protein (50 µg) was taken for sodium dodecyl sulfate
polyacrylamide gel electrophoresis (SDS-PAGE) and transferred onto
the membrane. The isolated protein was electronically transferred
onto the polyvinylidene fluoride (PVDF) membrane. The membrane was
sealed using blocking solution at room temperature for 1 h,
followed by incubation with primary antibody overnight at 4°C.
After the membrane was washed with TTBS, the secondary antibody
(1:2,000) was added for incubation at room temperature for 1 h. The
membrane was washed again with TTBS, followed by color development
using developing solution and photographed.
Statistical analysis
Data were expressed as mean ± standard deviation and
processed using SPSS 17.0 (SPSS, Inc., Chicago, IL, USA). One-way
analysis of variance (ANOVA) and the SNK post hoc test were used
for the statistical analysis of data obtained. P<0.05 was
considered to indicate a statistically significant difference.
Results
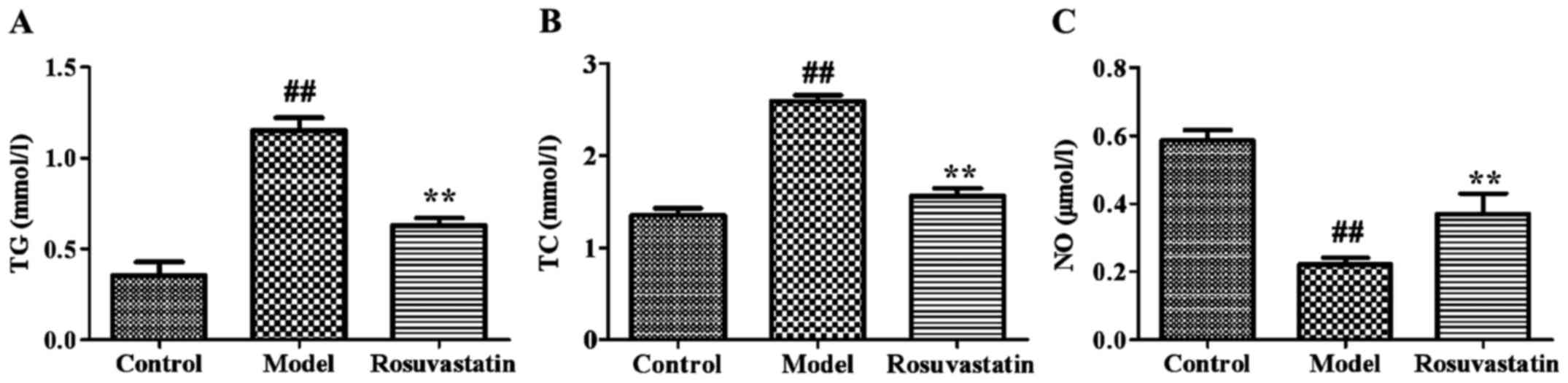
Effect of rosuvastatin on blood lipids
in AS rats
As shown in Fig. 1,
the contents of TG and TC in the model group were significantly
higher than those in the control group at 6 weeks after modeling,
suggesting that the early AS model was successfully established.
After administration of rosuvastatin, the contents of TG and TC in
serum were significantly decreased (P<0.01).
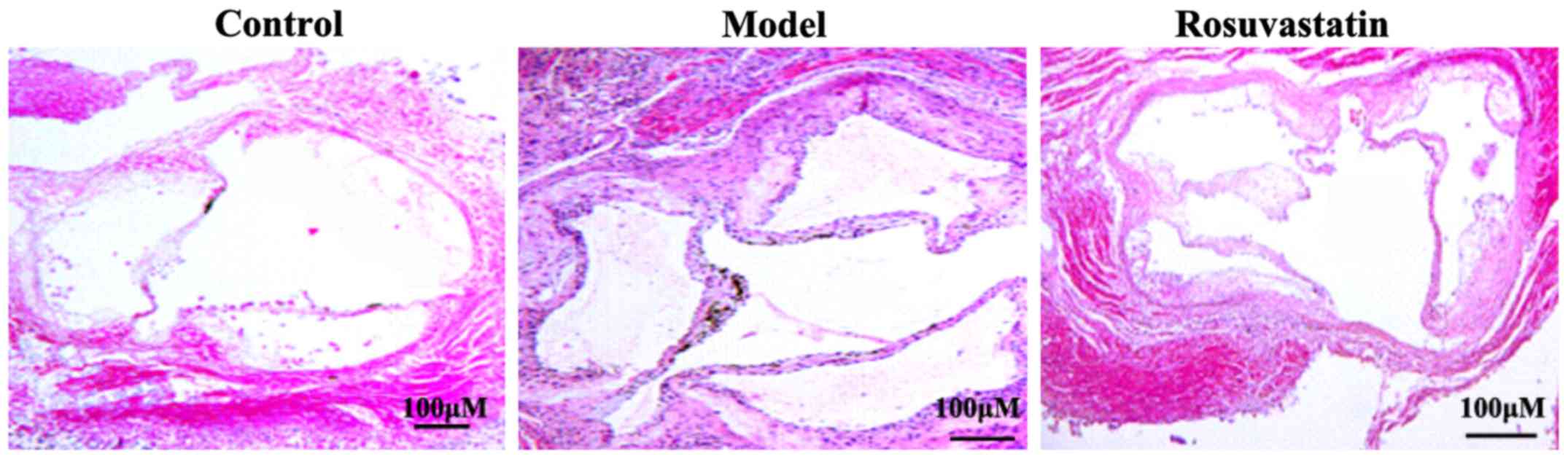
Effect of rosuvastatin on the vascular
morphology of rats
As shown in Fig. 2,
the results of H&E staining showed that in the control group,
the vascular intima was smooth, medial smooth muscle cells and
elastic fibers were arranged regularly without obvious
proliferation. In the model group, the vascular surface was not
smooth with endothelial shedding and irregular arrangement, the
nuclear staining was deep, and the intercellular matrix and
thickness of vascular wall were increased.
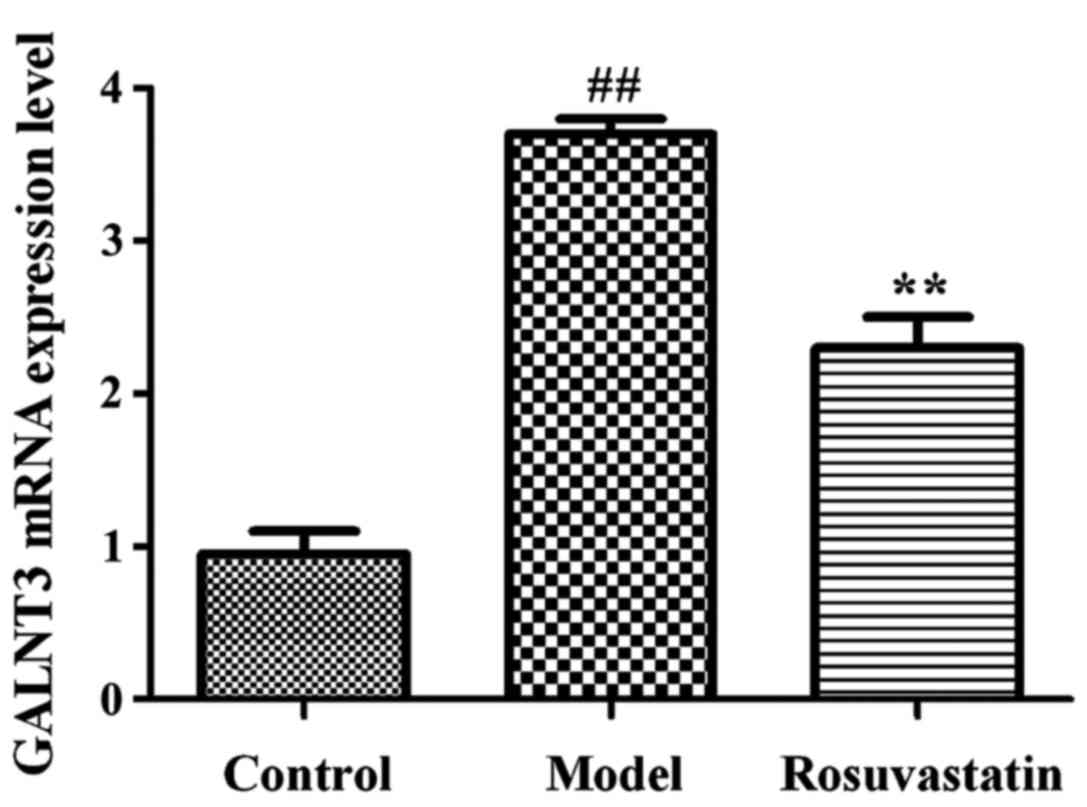
Effect of rosuvastatin on the mRNA
expression of GALNT3
As shown in Fig. 3,
the mRNA expression level of GALNT3 in model group was
significantly increased compared with that in the control group
(P<0.01). By contrast, the mRNA expression level of GALNT3 in
the administration group was significantly decreased (P<0.01),
indicating that rosuvastatin can significantly reduce the mRNA
expression of GALNT3 in AS rats.
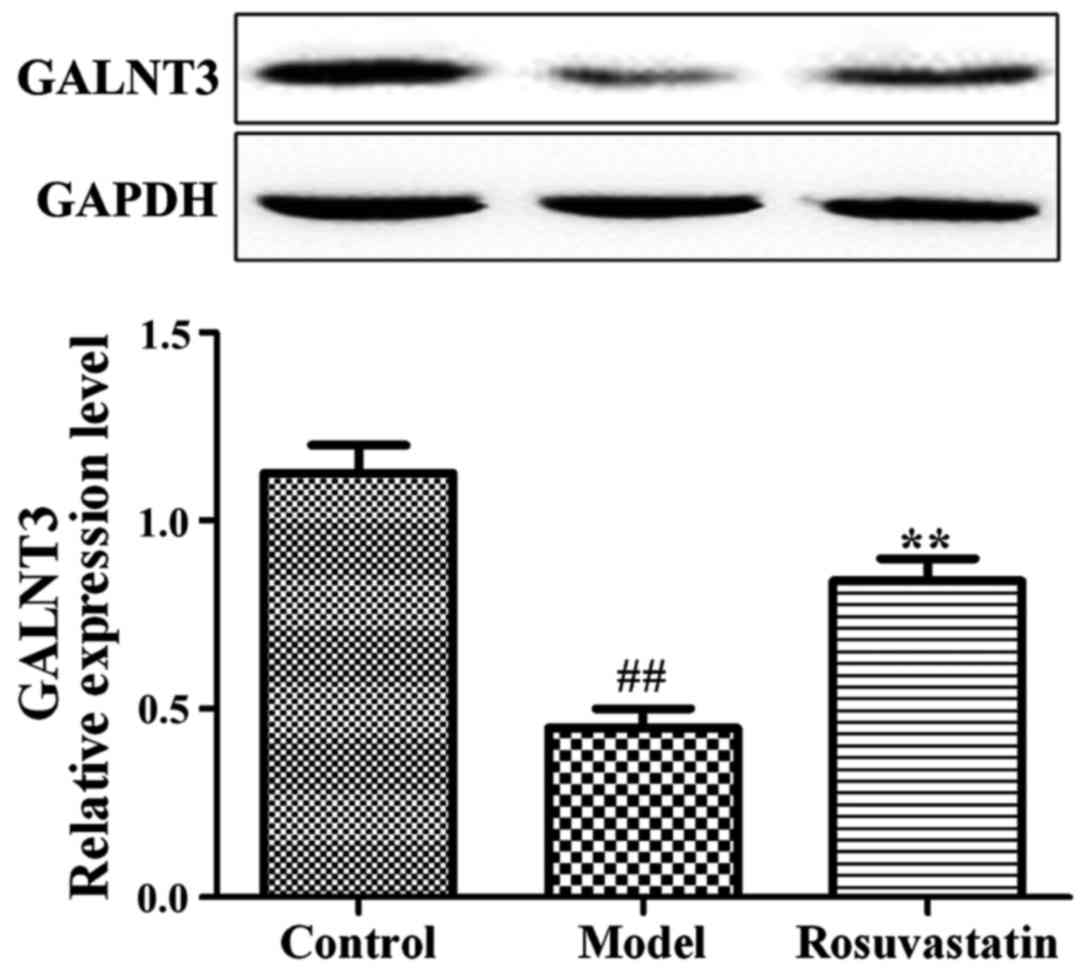
Effect of rosuvastatin on the protein
expression of GALNT3
As shown in Fig. 4,
the protein expression level of GALNT3 in the model group was
significantly decreased compared with that in the control group,
and the protein expression level of GALNT3 in the administration
group was also significantly decreased (P<0.01), indicating that
rosuvastatin can significantly downregulate the protein expression
of GALNT3 in AS.
Discussion
The complex pathogenesis of AS is due to the
combined effects of external and genetic factors, which involves a
variety of genes and other factors. Although some achievements have
been made in the study on AS, there is still a lack of effective
treatment means. Therefore, finding an effective therapeutic target
and mechanism of AS is of groundbreaking medical significance for
the clinical treatment and intervention of AS.
Vascular endothelium can secrete a variety of
bioactive substances, among which NO derived from endothelium has a
strong cardiovascular protection and anti-AS effect. NO is a kind
of gas signaling molecule produced by vascular endothelium under
the action of endothelial nitric oxide synthase (eNOS). NO, not
only has a strong vasodilatory effect, but can also inhibit
platelet aggregation and adhesion, prevent thrombosis, inhibit the
expression of inflammatory factors, low-density lipoprotein
oxidation and foam cell formation, and prevent the occurrence of
early AS. In addition, NO can inhibit the proliferation and
migration of vascular smooth muscle cells, and protect and prevent
progression in the late stage of AS. Therefore, NO is an essential
protective factor that resists AS and thrombosis, and maintains the
normal vasomotor response in cardiovascular system. Clinical and
experimental data show that glycoprotein is a key factor that
maintains the steady state of endothelial cells and blood vessels,
which is also an important signal regulator of cardiovascular
function (11). In sugar complexes,
the role of glycoprotein is very significant, which, not only
includes the regulation of cell growth and differentiation, but
also plays an important role in the identification, signal
transduction and immune response, carrying and transmitting a large
number of biological information (12). The O-linked glycoprotein is mainly
distributed on the cell surface, and the catalytic response of
O-glycosylation reaction is involved in the formation of this
important skeleton. The members of UDP-GalNAc are the performers
and participants in this biochemical process, and the expression of
each member in the ppGalNAc-Ts family has a certain periodic
functional specificity, and many members, such as the rate-limiting
enzymes, participate in the process of post-translational
processing of a variety of proteins, which have irreplaceable
physiological activities (13,14).
Additionally, GALNT3 gene has an important role in protecting
vascular endothelial cells, and the damage to vascular endothelial
cells is considered an important factor in the incidence of AS
(15). Shibao et al reported
that compared with that in normal breast tissues, the ppGALNT3
expression level in the differentiated malignant adenocarcinoma is
significantly increased, and it is not expressed in normal breast
tissues, but in breast cancer cells (16). In addition, the study on
GALNT3 gene showed that the levels of vitamin D and
Ca2+ can affect the expression of ppGALNT3 (17). However, there are few reports on the
relationship between GALNT3 gene and coronary heart disease.
It was found in this study to the best of our knowledge for the
first time that rosuvastatin has a significant effect on the
expression level of ppGALNT3 gene in AS, providing a new
perspective for the treatment of AS.
In this study, the AS rat model was established
using high-fat diet. The contents of serum TG, TC and NO in AS rats
after intervention with rosuvastatin were investigated in this
study. Compared with those in model group, the contents of TG and
TC were significantly decreased after drug administration, but the
serum NO content was significantly increased. The results of
H&E staining showed that in model group, the vascular intima of
thoracic aorta was not smooth with endothelial shedding, and the
smooth muscle cells were arranged irregularly with proliferation;
but the conditions were significantly improved after the
administration of rosuvastatin. The results of RT-PCR and western
blot analysis revealed that compared with those in model group, the
mRNA and protein expressions of GALNT3 were significantly increased
in the administration group. Similar research showed that the
proliferation of vascular endothelial cells can be significantly
inhibited through intervention in the GALNT3 expression in human
umbilical vein endothelial cells (HUVECs), while the proliferation
of vascular endothelial cells is significantly increased and the
arterial plaques are obviously reduced after the upregulation of
GALNT3 (18,19). In addition, findings have also shown
that consistent results are observed in the detection of vascular
endothelial cell apoptosis using a flow cytometer. In other words,
the endothelial cell apoptosis is aggravated when the GALNT3
gene expression is inhibited, but the upregulation of GALNT3 can
significantly inhibit apoptosis of endothelial cells and alleviate
AS (20,21). In conclusion, rosuvastatin can
significantly increase the expression of AS candidate gene
GALNT3, thereby improving atherosclerotic lesions.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
YL contributed significantly to writing the
manuscript and cell culture. TC analyzed and interpreted western
blot analysis. JX recorded and analysed orthological observation of
vascular tissues and RT-PCR. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Jinan Zhangqiu District Hospital of Traditional Chinese Medicine
(Jinan, China).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
van Gils JM, Ramkhelawon B, Fernandes L,
Stewart MC, Guo L, Seibert T, Menezes GB, Cara DC, Chow C, Kinane
TB, et al: Endothelial expression of guidance cues in vessel wall
homeostasis dysregulation under proatherosclerotic conditions.
Arterioscler Thromb Vasc Biol. 33:911–919. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kriszbacher I, Koppán M and Bódis J:
Inflammation, atherosclerosis, and coronary artery disease. N Engl
J Med. 353:429–430. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ross R: Atherosclerosis - an inflammatory
disease. N Engl J Med. 340:115–126. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gregersen I, Holm S, Dahl TB, Halvorsen B
and Aukrust P: A focus on inflammation as a major risk factor for
atherosclerotic cardiovascular diseases. Expert Rev Cardiovasc
Ther. 14:391–403. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Barton M: Obesity and aging: Determinants
of endothelial cell dysfunction and atherosclerosis. Pflugers Arch.
460:825–837. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Gotlieb AI: Smooth muscle and endothelial
cell function in the pathogenesis of atherosclerosis. Can Med Assoc
J. 126:903–908. 1982.PubMed/NCBI
|
|
7
|
Ross R and Glomset JA: The pathogenesis of
atherosclerosis (first of two parts). N Engl J Med. 295:369–377.
1976. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ross R and Glomset JA: The pathogenesis of
atherosclerosis (second of two parts). N Engl J Med. 295:420–425.
1976. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Vale N, Nordmann AJ, Schwartz GG, de Lemos
J, Colivicchi F, den Hartog F, Ostadal P, Macin SM, Liem AH, Mills
E, et al: Statins for acute coronary syndrome. Cochrane Database
Syst Rev. 9:CD0068702011.
|
|
10
|
Durán WN, Breslin JW and Sánchez FA: The
NO cascade, eNOS location, and microvascular permeability.
Cardiovasc Res. 87:254–261. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Tian XY, Wong WT, Xu A, Chen ZY, Lu Y, Liu
LM, Lee VW, Lau CW, Yao X and Huang Y: Rosuvastatin improves
endothelial function in db/db mice: Role of angiotensin II type 1
receptors and oxidative stress. Br J Pharmacol. 164:598–606. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tsuiji H, Takasaki S, Sakamoto M, Irimura
T and Hirohashi S: Aberrant O-glycosylation inhibits stable
expression of dysadherin, a carcinoma-associated antigen, and
facilitates cell-cell adhesion. Glycobiology. 13:521–527. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sørensen T, White T, Wandall HH,
Kristensen AK, Roepstorff P and Clausen H:
UDP-N-acetyl-alpha-D-galactosamine:polypeptide
N-acetylgalactosaminyltransferase. Identification and separation of
two distinct transferase activities. J Biol Chem. 270:24166–24173.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ten Hagen KG, Fritz TA and Tabak LA: All
in the family: The UDP-GalNAc:polypeptide
N-acetylgalactosaminyltransferases. Glycobiology. 13:1R–16R. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Vita JA and Keaney JF Jr: Endothelial
function: A barometer for cardiovascular risk? Circulation.
106:640–642. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shibao K, Izumi H, Nakayama Y, Ohta R,
Nagata N, Nomoto M, Matsuo K, Yamada Y, Kitazato K, Itoh H, et al:
Expression of UDP-N-acetyl-alpha-D-galactosamine-polypeptide galNAc
N-acetylgalactosaminyl transferase-3 in relation to differentiation
and prognosis in patients with colorectal carcinoma. Cancer.
94:1939–1946. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chefetz I, Kohno K, Izumi H, Uitto J,
Richard G and Sprecher E: GALNT3, a gene associated with
hyperphosphatemic familial tumoral calcinosis, is transcriptionally
regulated by extracellular phosphate and modulates matrix
metalloproteinase activity. Biochim Biophys Acta. 1792:61–67. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ramakrishnan P, Clark PM, Mason DE, Peters
EC, Hsieh-Wilson LC and Baltimore D: Activation of the
transcriptional function of the NF-κB protein c-Rel by O-GlcNAc
glycosylation. Sci Signal. 6:ra752013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gill DJ, Tham KM, Chia J, Wang SC,
Steentoft C, Clausen H, Bard-Chapeau EA and Bard FA: Initiation of
GalNAc-type O-glycosylation in the endoplasmic reticulum promotes
cancer cell invasiveness. Proc Natl Acad Sci USA. 110:E3152–E3161.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Bakhashab S, Lary S, Ahmed F, Schulten HJ,
Bashir A, Ahmed FW, Al-Malki AL, Jamal HS, Gari MA and Weaver JU:
Reference genes for expression studies in hypoxia and hyperglycemia
models in human umbilical vein endothelial cells. G3 (Bethesda).
4:2159–2165. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Saffi MA, Furtado MV, Polanczyk CA,
Montenegro MM, Ribeiro IW, Kampits C, Haas AN, Rösing CK and
Rabelo-Silva ER: Relationship between vascular endothelium and
periodontal disease in atherosclerotic lesions: Review article.
World J Cardiol. 7:26–30. 2015. View Article : Google Scholar : PubMed/NCBI
|