Introduction
Cimetidine is a drug approved by the Food and Drug
Administration (USA) for the reduction of gastric acid secretion.
It is used to alleviate the symptoms of peptic ulcer, erosive
gastroesophageal reflux and hypersecretory conditions, including
Zollinger-Ellison syndrome, and multiple endocrine adenomas
(1). Cimetidine significantly
inhibits the secretion of gastric acid caused by food, histamine,
pentagastrin, caffeine and insulin. It is an H2 receptor
antagonist and competitively blocks dihydrotestosterone (DHT)
receptors in the pituitary gland, hypothalamus and other tissues
that require DHT (2,3). DHT is a sterol transformed from
testosterone (T), and functions as the so-called real male hormone
in accessory glands, including the prostate and seminal vesicle
gland. It is referred to as a weak nonsteroidal anti-androgen
(4,5). Cimetidine has been demonstrated to have
important immunoregulatory and anticancer effects, which further
broadened its clinical applications (6,7).
Cimetidine is widely distributed in various types of tissue; thus,
its pharmacological action is broad. Adverse effects, including
loss of libido, impotence and decreased sperm, have been reported
by male patients treated with cimetidine (8).
Cimetidine causes a significant reduction of
testicular weight, tubular diameter and seminiferous epithelium
height (9–12). In addition, irregular tubules
exhibiting disorganized epithelium, intraepithelial vacuolization,
loss of germ cells by apoptosis and sloughed germ cells filling the
tubular lumen have been observed (9–14).
França et al (9) identified a
significant reduction of peritubular tissue in testis samples from
cimetidine-treated rats. In addition, the presence of apoptotic
peritubular cells and disordered basal lamina around apparently
normal seminiferous tubules indicated that peritubular cells are
the primary targets of cimetidine (9). Beltrame et al (15) reported that cimetidine causes
testicular vascular atrophy by inducing apoptosis in vascular
cells. The impairment of the testicular microvasculature by
cimetidine may be exerted through a possible antagonist effect of
on H2- and/or androgen receptors in vascular cells
(15). Koshimizu et al
(16) demonstrated that cimetidine
induces significant epithelial damage. It may prevent the
translocation of nuclear factor (NF)-κB to the nucleus and
interfere with NF-κB-mediated control of smooth muscle cell
apoptosis (16). NF-κB is important
in inflammation, immune responses, tumorigenesis and protection
against apoptosis (17–19). It activates the transcription of
numerous genes, several of which directly block the activation of
caspases involved in apoptosis (20); these genes include cyclooxygenase
(COX)-2 and inducible nitric oxide (NO) synthase (iNOS) (21). COX-2 is an inducible form of COX and
has an important role in inflammation and tumor proliferation
(22). iNOS induces NO formation,
leading to cytotoxicity (23).
During infection, NO is detected at high levels in the immune
system and has host-protective effects (24). It may be an important mediator of
acute and chronic inflammatory signals in different forms of
inflammation in humans and animals (25). Studies have demonstrated that NO and
reactive oxygen species trigger cell death. The oxidation products
of NO cause lipid peroxidation (26–28).
Furthermore, iNOS binds specifically to COX-2 and enhances its
catalytic activity (29).
To further understand the mechanisms of reproductive
toxicity induced by cimetidine, the present study evaluated the
effects of a 9-week oral cimetidine treatment on the reproductive
system of male Sprague Dawley (SD) rats, assessing serum levels of
reproductive hormones, the sperm count and histopathologic features
of the testis. In addition, COX-2, iNOS, and NF-κB expression
levels, and apoptosis in testis samples were detected.
Materials and methods
Animals and treatment
A total of 32 male SD rats (weight, 430–530 g; age,
16-weeks) were purchased from SIPPR-B&K Laboratory Animal Corp.
(Shanghai, China; license no. SCXK; 2008-0016). They were housed at
two animals per cage in an animal room kept at 20–26°C with 40–70%
relative humidity, under a 12-h light/dark cycle. The animals had
free access to tap water and food. This study was approved by the
Ethics Committee Shanghai Institute of Planned Parenthood Research
Animal Care (Shanghai, China). Discomfort, distress and pain to the
animals were strictly minimized.
The animals were randomly assigned into 4 groups of
8. Group I served as a control group and was administered 0.5%
sodium carboxymethyl cellulose. Groups II, III and IV received 20,
40 and 120 mg/kg body weight of cimetidine, respectively, by gavage
for 63 consecutive days; 40 mg/kg represents the therapeutic dose
used in humans. The rats were sacrificed on the 64th day (24 h
after the final treatment) under anesthesia with 3% pentobarbital
sodium (35 mg/kg). Cimetidine was supplied by Wuhan Shengtianyu
Biological Technology Co., Ltd (Wuhan, China) and mixed with 0.5%
sodium carboxymethyl cellulose prior to use.
Body and organ weight measurements,
and histopathology
Rats were weighed twice a week and sacrificed on the
64th day as described above. The testis, epididymis, prostate
gland, seminal vesicle, preputial gland, levator ani muscle and
sphincter ani were collected and weighed. Organ weights were
recorded in g and expressed as g/100 g body weight. The testis
samples were then fixed in neutral 10% formalin for 24 h at room
temperature, dehydrated in ethanol, cleared in xylene and embedded
in paraffin. Slices of 4–6 µm thickness were prepared and stained
with hematoxylin (5 min at room temperature) and eosin (2 min at
room temperature). The sections were then examined under a light
microscope.
Sperm parameters
The epididymis was isolated and cleared of adhering
tissues. The cauda epididymis was extracted, minced and incubated
in 4 ml M199 at 37°C for 5 min, to allow sperm cells to leave the
epididymal tubules. A total of 10 µl sperm suspension was then
added to the sperm counting plate. Sperm parameters were collected
by computer-assisted sperm analysis with the HTM-IVOS (Hamilton
Thorne, Beverly, Ma, USA) and evaluated using the HTM-TOXIVOS
Toxicology software program (Rat Head Toxicology, Hamilton-Thorne
Research, Beverly, MA, USA) version 12.
Serum hormone levels
At the end of the experimental period, rats were
anesthetized with 3% pentobarbital sodium. Blood samples were
collected via the abdominal aorta and centrifuged for 15 min (2,095
× g, 4°C). The resulting supernatants were immediately stored at
−80°C until use for hormone level measurements.
Follicle-stimulating hormone (FSH), luteinizing hormone (LH) and
testosterone (T) concentrations were measured by FSH, LH and T
ELISA kits (Hufeng Chemical Co., Ltd, Nantong, China; cat. nos.
F14574-A, F14573-A and F4421-A, respectively) according to the
manufacturer's instructions.
Immunohistochemistry
Paraffin sections of testis samples were
deparaffinized and rehydrated. Antigens were retrieved by
incubating the sections in a microwave oven in sodium citrate
buffer (10 mM; pH 6.0) for 15 min. Sections were brought to room
temperature and rinsed with PBS. Then the sections were blocked
using 5% bovine serum albumin (Boster Biological Technology Co.,
Ltd., Pleasanton, CA, USA) at room temperature for 20 min.
Subsequently, the tissues were incubated with primary antibodies
overnight at 4°C. Antibodies against COX-2 (cat. no. BA0738, Boster
Biological Technology Co., Ltd., China) and NF-κB (p52) (cat. no.
BA1873, Boster Biological Technology Co., Ltd.) were diluted at
1:200, 1:200 and 1:100 in PBS, respectively. After 12 h, the
sections were washed with PBS and incubated for 30 min with biotin
labeled goat anti rabbit IgG secondary antibodies (cat. no. SA1022;
included in a kit SABC-POD (rabbit IgG) kit for immediate use
provided by Boster Biological Technology Co., Ltd.) at room
temperature. Bands were visualized using diaminobenzidine (DAB)
chromogenic agent (Boster Biological Technology Co., Ltd.) at room
temperature for 5–10 min. Sections were counterstained with Mayer's
hematoxylin at room temperature for 5 min. Finally, the mean
optical density values were analyzed with ImageJ software v. 1.47
(National Institutes of Health, Bethesda, MD, USA).
Terminal deoxynucleotidyl transferase
(TdT) deoxyuridine triphosphate nick end labeling (TUNEL)
assay
TUNEL staining was performed using the DeadEnd™
Colorimetric Apoptosis Detection System (cat. no. G3250; Promega
Corp., Madison, WI, USA). Testicular sections were deparaffinized,
hydrated and incubated with 20 µg/ml proteinase K (Promega Corp.)
for 10 min at room temperature. The sections were then equilibrated
with equilibration buffer at room temperature for 10 min.
Subsequently, the TdT reaction mix was added to the tissue sections
on an area no larger than 5 cm2. The slides were
incubated for 60 min at 37°C in a humidified chamber. The reaction
was stopped by transferring the slides to 2X saline-sodium citrate
for 15 min. Endogenous peroxidase was inactivated by incubation
with 0.3% hydrogen peroxide for 5 min at room temperature. The
sections were incubated with streptavidin horseradish peroxidase
(diluted at 1:500 in PBS) for 30 min at room temperature and
developed with DAB at room temperature for 5 min until a brown
background appeared. Finally, the samples were counterstained with
Mayer's hematoxylin. The mean optical density values were analyzed
with ImageJ software v. 1.47.
Statistical analysis
Values are expressed as the mean ± standard
deviation. Statistical analyses were performed using SPSS version
11.5 (SPSS, Inc., Chicago, IL, USA). One-way analysis of variance
followed by Dunnett's test was used to assess statistical
differences between the control and treatment groups. P<0.05 was
considered to indicate a statistically significant difference.
Results
Body and organ weight
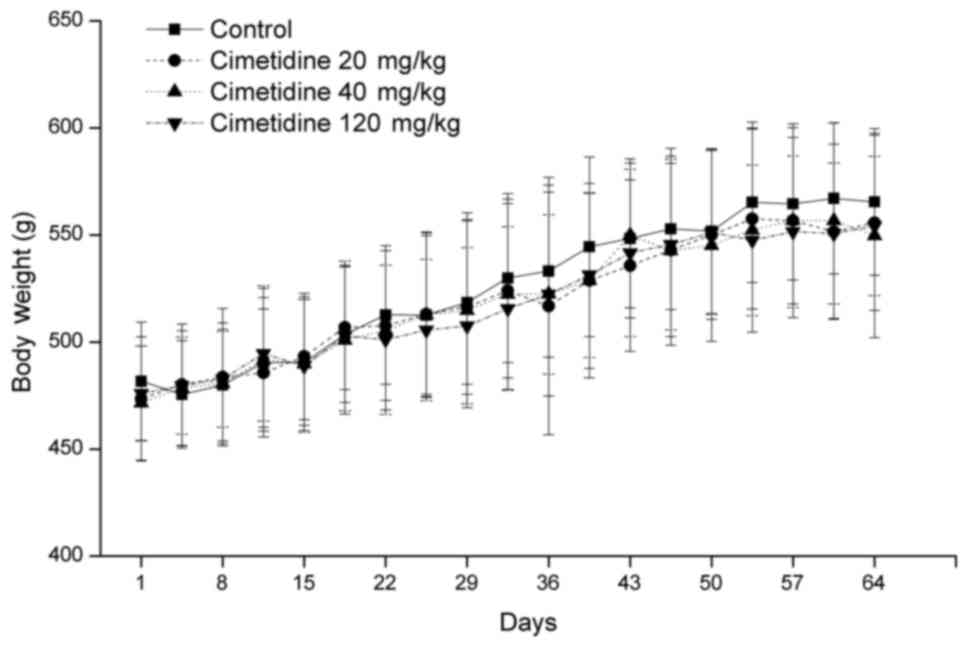
The body weight of treated rats was not
significantly different from that in the control group throughout
the treatment period (Fig. 1). In
addition, testis, epididymis, prostate gland, preputial gland,
levator ani muscle and sphincter ani weights were similar in the
control and treatment groups. Administration of 120 mg/kg
cimetidine significantly increased the seminal vesicle weight
compared with control group. However, no significant difference in
relative seminal vesicle weight (g/100 g body weight) was observed
between the 120 mg/kg cimetidine group and control group (Table I).
 | Table I.Effects of cimetidine on weight of
organs of male rats associated with the reproductive system. |
Table I.
Effects of cimetidine on weight of
organs of male rats associated with the reproductive system.
|
|
| Cimetidine
(mg/kg) |
|---|
|
|
|
|
|---|
| Organ | Control | 20 | 40 | 120 |
|---|
| Testis |
|
|
|
|
|
(g) | 3.384±0.173 | 3.516±0.337 | 3.445±0.269 | 3.466±0.231 |
| (g/100
g b.w.) | 0.601±0.067 | 0.633±0.049 | 0.630±0.074 | 0.628±0.022 |
| Epididymis |
|
|
|
|
|
(g) | 1.298±0.080 | 1.264±0.105 | 1.281±0.100 | 1.274±0.119 |
| (g/100
g b.w.) | 0.231±0.024 | 0.229±0.025 | 0.234±0.027 | 0.230±0.011 |
| Preputial
gland |
|
|
|
|
|
(g) | 0.091±0.015 | 0.092±0.024 | 0.108±0.028 | 0.099±0.018 |
| (g/100
g b.w.) | 0.016±0.003 | 0.017±0.005 | 0.020±0.005 | 0.018±0.003 |
| Prostate gland |
|
|
|
|
|
(g) | 1.495±0.161 | 1.582±0.197 | 1.579±0.178 | 1.542±0.275 |
| (g/100
g b.w.) | 0.266±0.043 | 0.285±0.030 | 0.287±0.024 | 0.278±0.040 |
| Seminal
vesicle |
|
|
|
|
|
(g) | 1.724±0.135 | 1.729±0.296 | 1.856±0.209 |
2.020±0.273a |
| (g/100
g b.w.) | 0.307±0.038 | 0.315±0.072 | 0.338±0.033 | 0.368±0.061 |
| Levator ani
muscle |
|
|
|
|
|
(g) | 0.317±0.048 | 0.310±0.033 | 0.292±0.038 | 0.310±0.036 |
| (g/100
g b.w.) | 0.056±0.008 | 0.056±0.006 | 0.053±0.008 | 0.056±0.006 |
| Sphincter ani |
|
|
|
|
|
(g) | 1.167±0.084 | 1.169±0.134 | 1.171±0.107 | 1.141±0.113 |
| (g/100
g b.w.) | 0.207±0.018 | 0.212±0.034 | 0.214±0.021 | 0.207±0.015 |
High-dose cimetidine causes decreased
sperm average path velocity (VAP), straight line velocity (VSL) and
curvilinear velocity (VCL)
Sperm count, sperm motility, progressive sperm
count, VAP, VSL and VCL are presented in Table II. Administration of 120 mg/kg
cimetidine for 9 weeks significantly decreased sperm VAP, VSL and
VCL compared with the control group (P<0.05). Sperm motilities
were not significantly different between the control and cimetidine
treatment groups.
 | Table II.Effects of cimetidine on sperm
parameters of male rats. |
Table II.
Effects of cimetidine on sperm
parameters of male rats.
|
|
| Cimetidine
(mg/kg) |
|---|
|
|
|
|
|---|
| Parameter | Control | 20 | 40 | 120 |
|---|
| Sperm count
(106/ml) | 9.1±4.5 | 6.9±2.8 | 5.8±3.1 | 6.0±1.8 |
| Sperm motility
(%) | 51.5±20.3 | 60.2±14.5 | 65.3±13.3 | 49.5±11.2 |
| Progressive sperm
count (106/ml) | 1.7±1.1 | 1.4±0.8 | 1.3±0.5 | 0.9±0.6 |
| VAP (µm/sec) | 243.2±40.5 | 240.6±24.5 | 249.5±11.6 |
205.5±15.6a |
| VSL (µm/sec) | 167.1±30.7 | 165.9±18.6 | 161.2±9.8 |
139.6±10.6a |
| VCL (µm/sec) | 417.7±80.5 | 412.0±41.6 | 427.1±25.9 |
348.9±31.8a |
High-dose cimetidine increases LH and
T levels
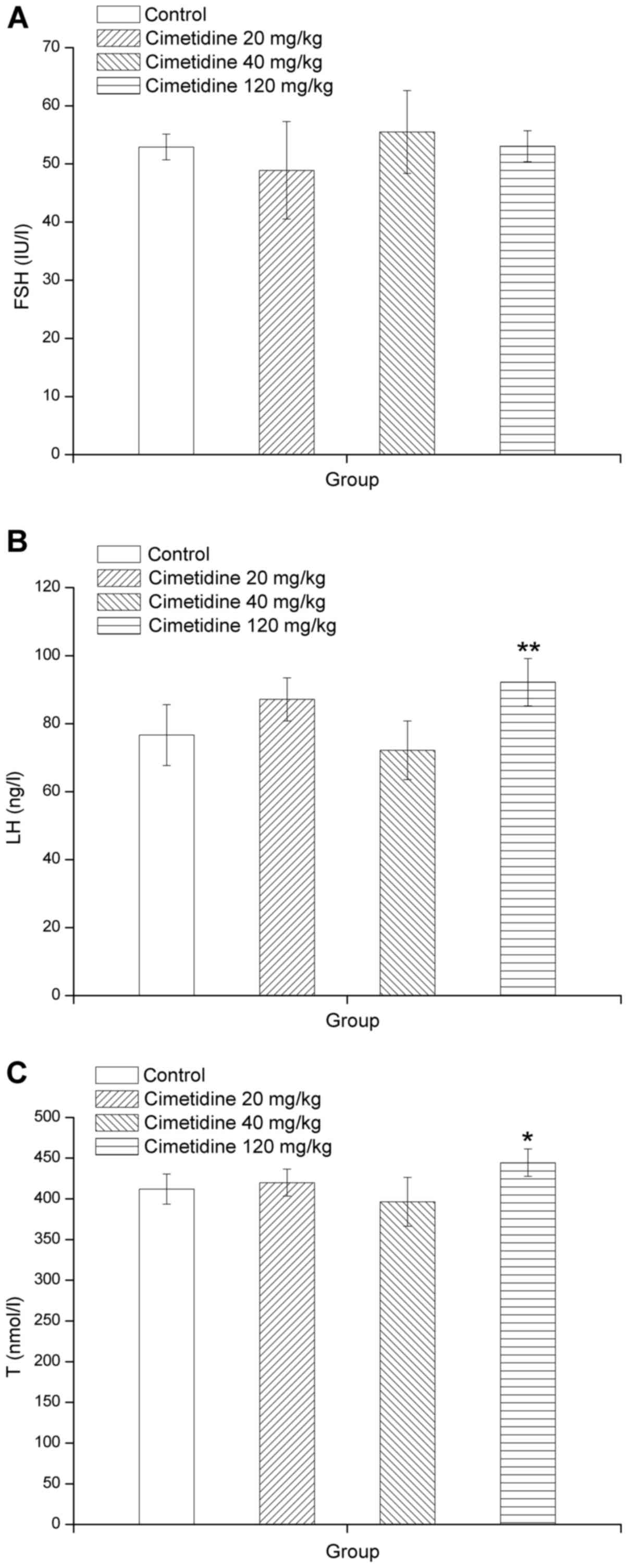
Total serum concentrations of unconjugated FSH, LH
and T are presented in Fig. 2A, B and
C, respectively. LH and T levels were significantly higher in
the 120 mg/kg cimetidine group compared with those in the control
group (P<0.05 or P<0.01). However, serum FSH levels exhibited
no significant differences from those in the control group.
High-dose cimetidine causes testicular
lesions
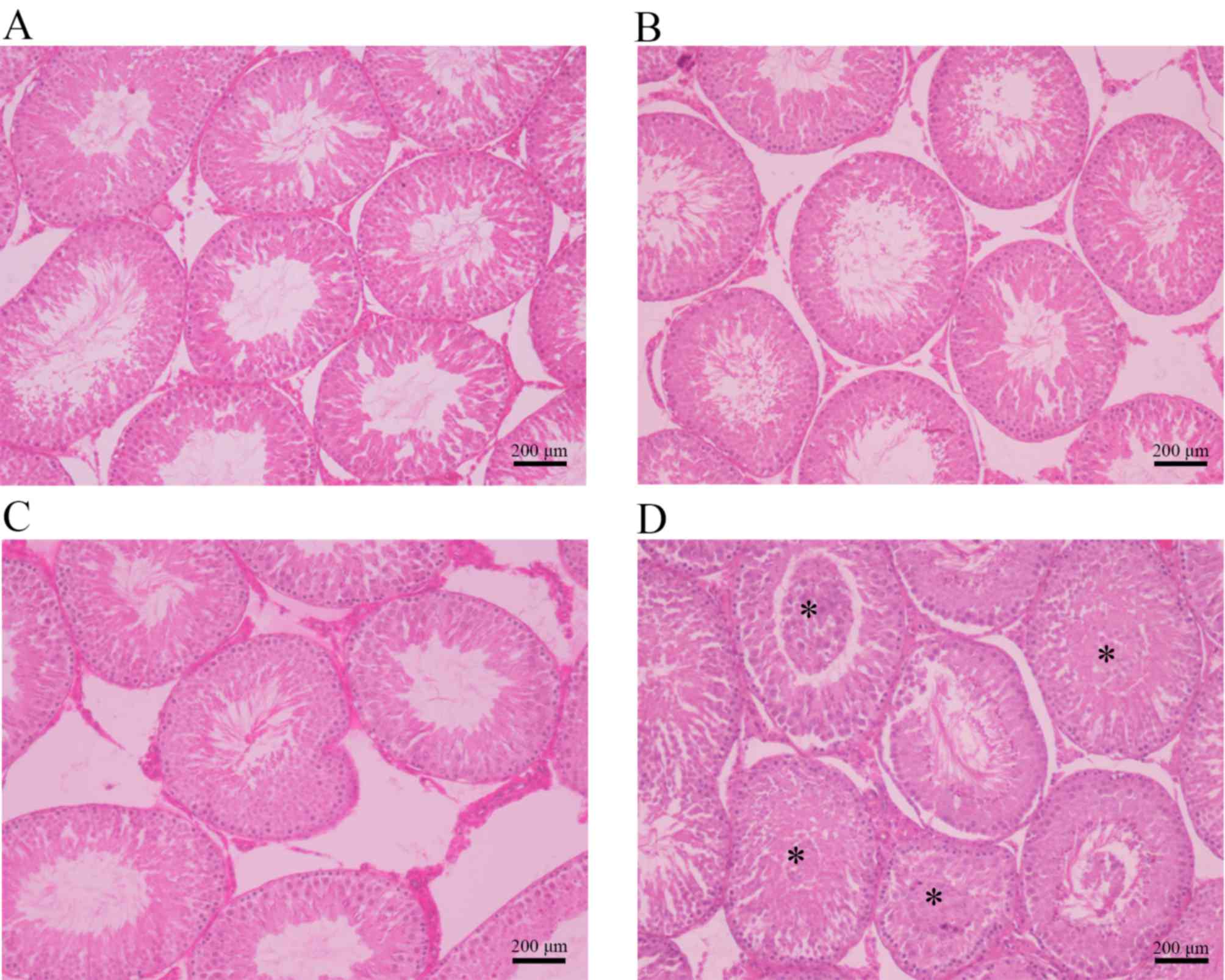
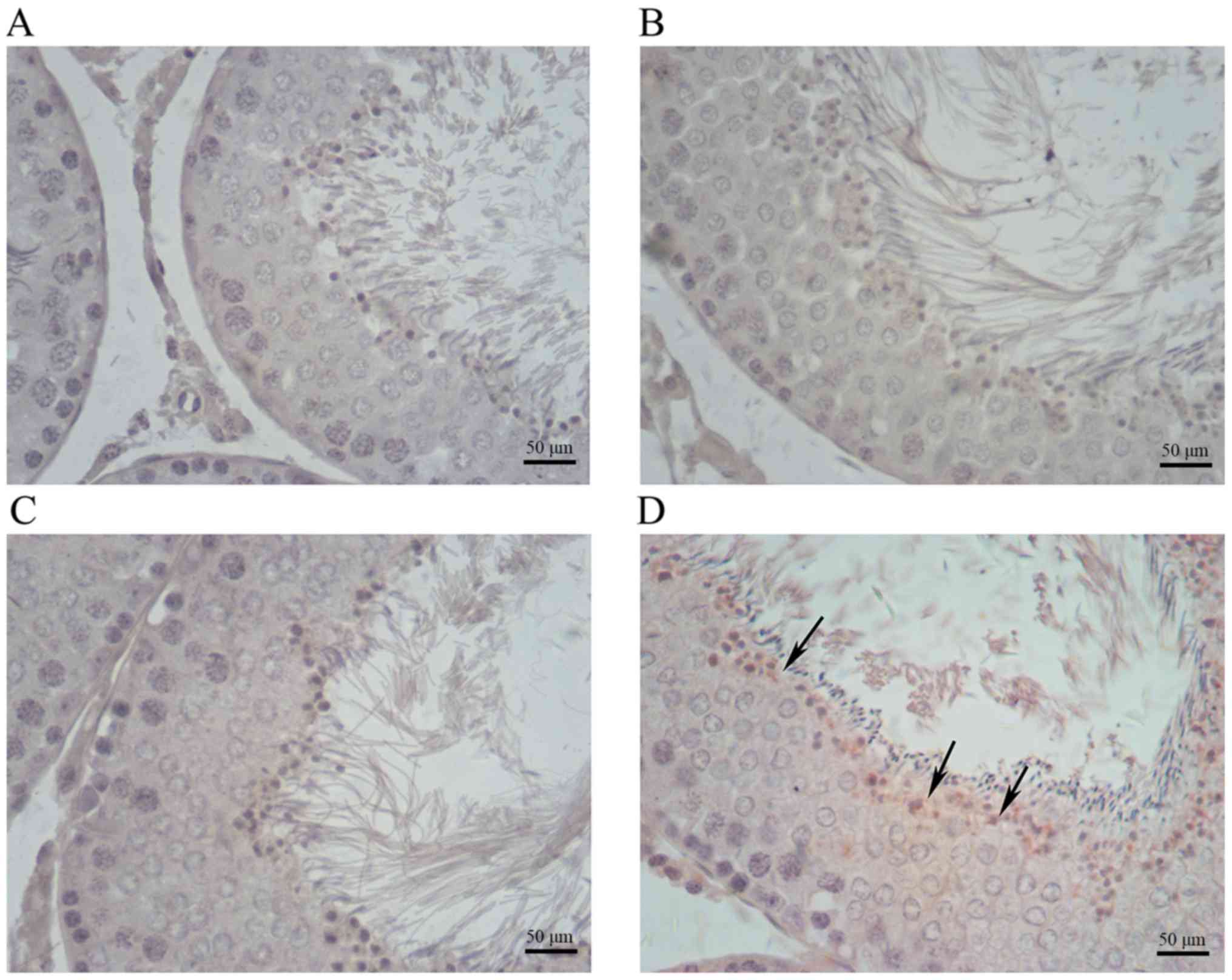
The photomicrographs in Fig. 3 illustrate the different
histopathologic changes observed in testis samples from rats
treated with cimetidine. The control, 20 mg/kg cimetidine and 40
mg/kg cimetidine groups exhibited a compact and regular arrangement
of cells in the seminiferous tubules (Fig. 3A, B and C, respectively). Treatment
with cimetidine at 120 mg/kg caused testicular lesions on
histopathological examination. The 120 mg/kg group displayed cell
material shedding in the lumen of seminiferous tubules (Fig. 3D).
High-dose cimetidine causes increased
expression of COX-2 and NF-κB
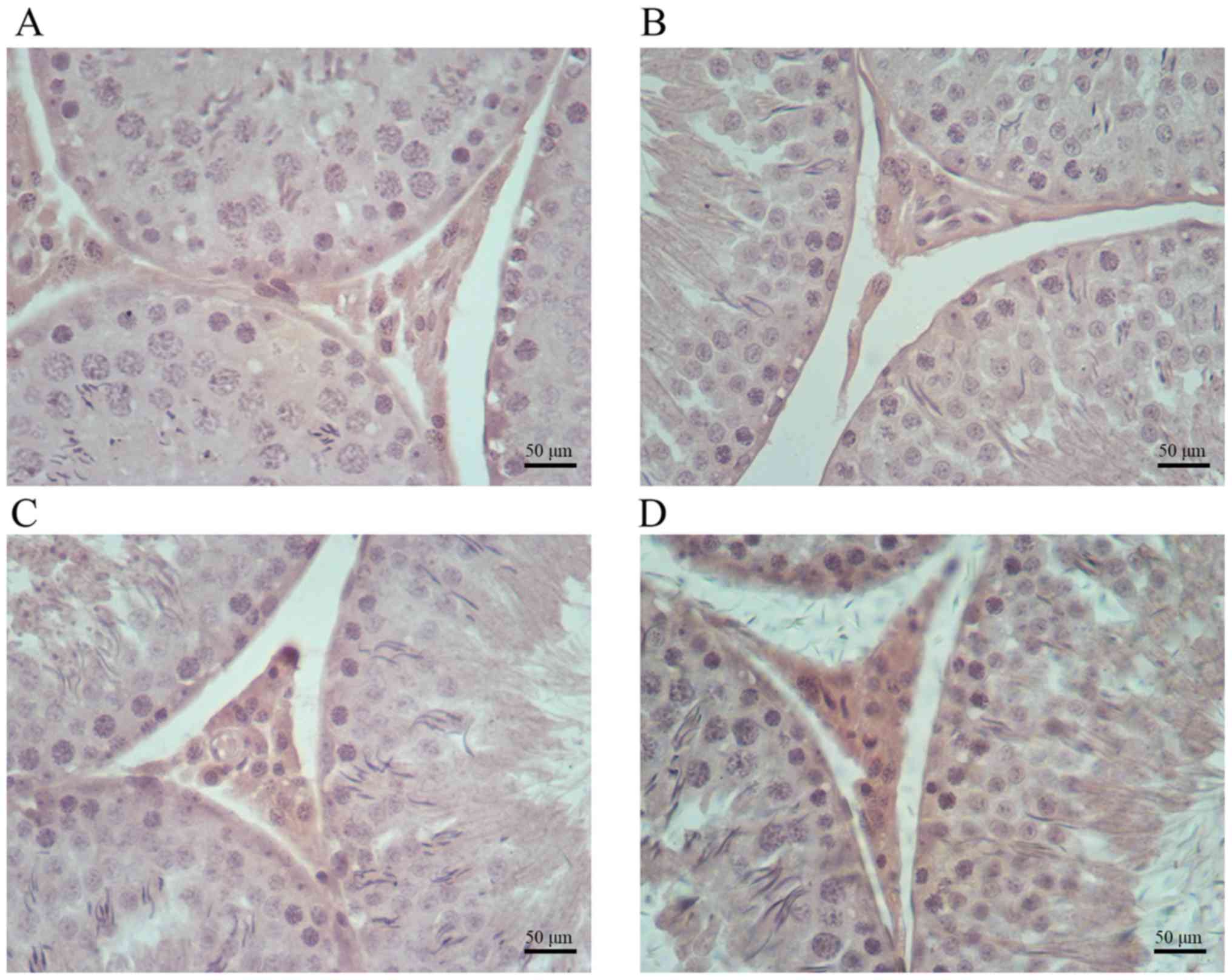
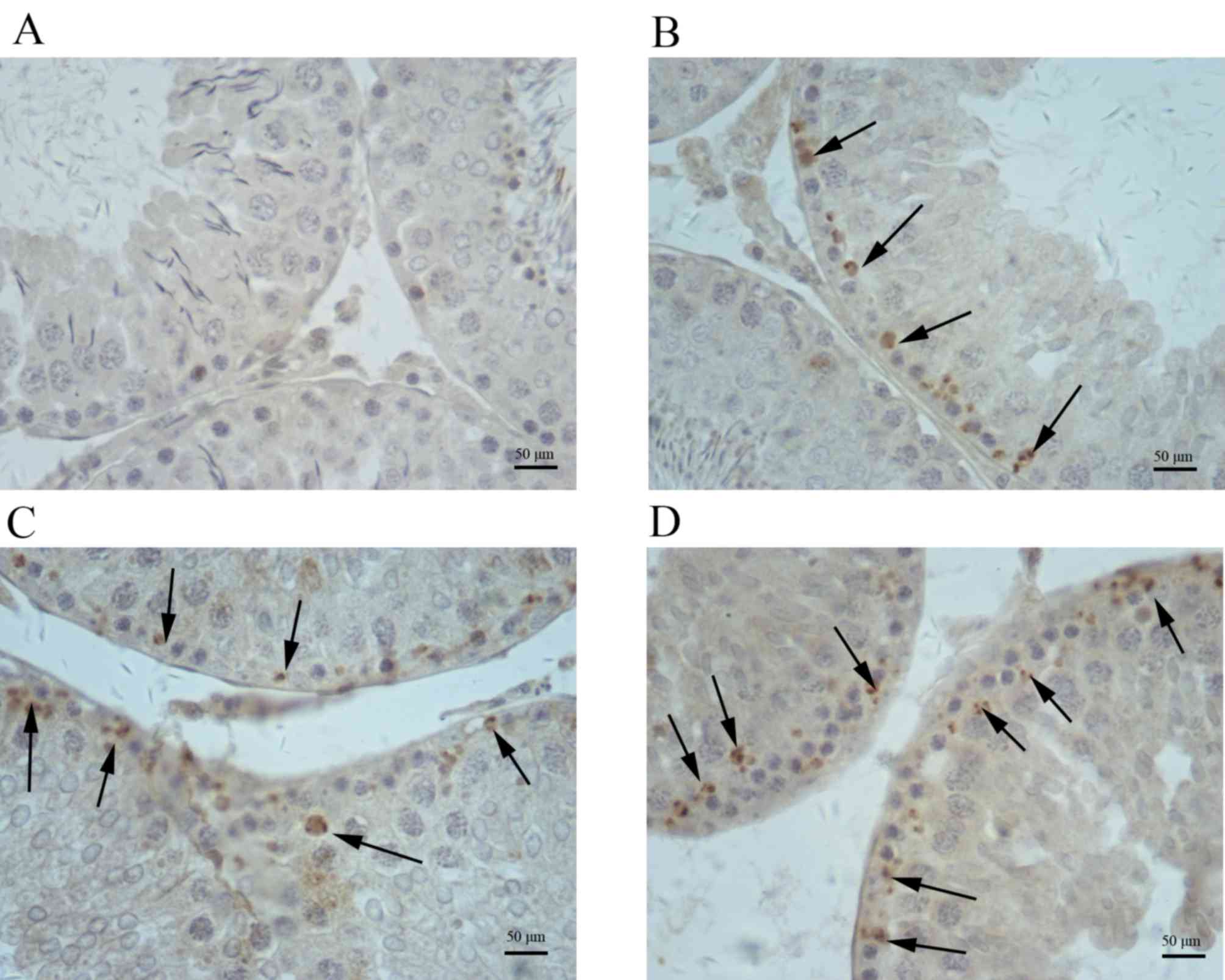
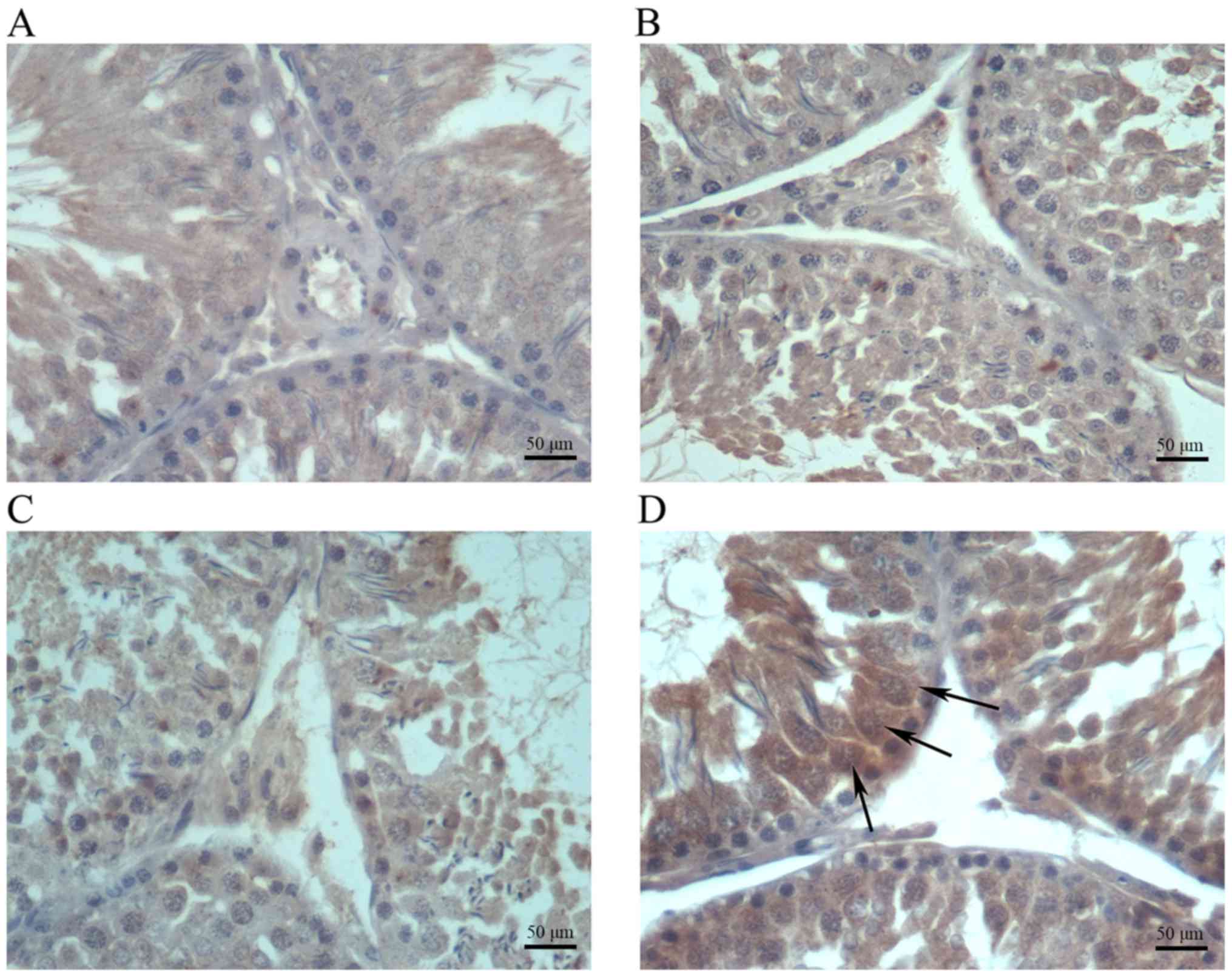
Immunohistochemical analysis indicated increased
amounts of cells positive for COX-2, iNOS and NF-κB in testis
samples from cimetidine-treated rats (Figs. 4–6).
The amount of cells positive for COX-2 and NF-κB was increased in
the 120 mg/kg cimetidine group (Figs.
4D and 6D; Table III) compared with the control
group; furthermore, the amount of cells positive for iNOS was
increased in all cimetidine treatment groups, including the 20, 40
and 120 mg/kg groups (Fig. 5B, C and
D; Table III). Notably, the
cells expressing iNOS were the Sertoli cells, but further research
is required to validate this result. There was no change in the
type of cells with iNOS, COX-2 and NF-κB expression upon
treatment.
 | Table III.Expression of COX-2, iNOS and NF-κB,
and apoptosis in testis of male rats. |
Table III.
Expression of COX-2, iNOS and NF-κB,
and apoptosis in testis of male rats.
|
|
| Cimetidine
(mg/kg) |
|---|
|
|
|
|
|---|
| Protein/item | Control | 20 | 40 | 60 |
|---|
| COX-2 | 0.167±0.011 | 0.169±0.013 | 0.172±0.006 |
0.192±0.009a |
| iNOS | 0.312±0.020 |
0.341±0.009a |
0.334±0.005a |
0.358±0.011b |
| NF-κB | 0.333±0.010 | 0.330±0.011 | 0.338±0.021 |
0.355±0.008a |
| Apoptosis | 0.327±0.016 | 0.319±0.022 | 0.331±0.019 |
0.363±0.013b |
High-dose cimetidine causes apoptosis
in testicles
In testicular sections from the control, 20 mg/kg
cimetidine and 40 mg/kg cimetidine groups, the seminiferous tubules
rarely displayed any TUNEL-stained cells, while obvious
TUNEL-positive cells were idenfied in seminiferous tubules from the
120 mg/kg cimetidine group (Fig. 7)
compared with control group. The results of the semi-quantitative
analysis of the images are displayed in Table III.
Discussion
Cimetidine, a weak nonsteroidal anti-androgenic
drug, induces testis abnormalities in male rats after
intraperitoneal injection (13,16). In
previous studies, it was demonstrated that cimetidine causes
significant structural alterations in the seminiferous tubules,
including intraepithelial vacuolization, loss of germ cells by
apoptosis, decrease in epithelial parameters and the area of the
smooth muscle layer of the vas deferens, and vascular cell
apoptosis (10,13,16).
However, the underlying mechanisms have remained elusive.
In the present study, cimetidine had no adverse
influence on the body and relative weight of reproductive organs
after 9 weeks of treatment by gavage; in another study (9), significant decreases in epididymal,
ventral prostate and combined seminal vesicle, as well as
coagulating gland weights were identified after a 59-day treatment
with a high dose (250 mg/kg) administered by intraperitoneal
injection. The discrepancy may be caused by the differences in
dosage and administration route. The dose of 250 mg/kg is much
higher than the highest dose (120 mg/kg) used in the present study.
In addition, intraperitoneal injection results in higher
bioavailability compared with oral administration used in the
present study.
The sperm count and progressive sperm count had a
decreasing trend with the increasing dosage of the drug, although
no statistical significance was reached. A possible explanation is
that cimetidine has an adverse effect on spermatogenic cells to a
certain degree. VAP, VSL and VCL are valuable parameters reflecting
sperm motility. In the present study, VAP, VSL and VCL were
significantly decreased in the 120 mg/kg cimetidine group compared
with those in the control group. Thus, it was deduced that
cimetidine may have adverse effects on the activation of
spermatozoon motility. The underlying mechanisms require further
exploration.
For hormone signaling, serum T, LH and FSH levels
were assessed after a nine-week treatment. LH and T levels were
significantly increased in the 120 mg/kg cimetidine group compared
with those in the control group. In another study (30), elevated T levels were also detected,
but LH levels remained unchanged. In two other studies on male
patients, increased LH and T levels were also reported (4,5).
Cimetidine competitively blocks DHT receptors and is referred to as
a weak nonsteroidal anti-androgen (2–5). It
increases LH levels, presumably by antagonizing the feedback
control of gonadotrophin secretion by androgens. An alternative
explanation is that cimetidine desensitizes androgen receptors and
inhibits the negative feedback for gonadotrophin secretion.
Subsequent to increased LH levels, an elevation in T levels occurs.
However, in the present study, FSH levels were not changed by
cimetidine. Generally speaking, FSH and LH are synthesized and
secreted by gonadotropic cells in the anterior pituitary gland.
Serum levels of FSH and LH are adjusted by negative feedback. In
the present study, only elevated serum LH levels were detected,
while serum FSH was unchanged after 9 weeks of cimetidine
treatment. From this, it was deduced that FSH is less sensitive to
the effects of cimetidine than LH.
As revealed by histopathology, cimetidine caused
significant structural alterations in seminiferous tubules,
including blocked tubular lumen by deciduous germ cells.
Immunohistochemistry revealed increased amounts of cells positive
for COX-2, iNOS and NF-κB after cimetidine treatment. In a previous
study (16), enhanced NF-κB
expression was detected in the cytoplasm of smooth muscle cells of
the vas deferens. In the present study, Enhanced NF-κB expression
was detected in spermatogenic cells in the 120 mg/kg cimetidine
group.
Oxidative stress and subsequent activation of
signaling kinases may stimulate NF-κB (31,32).
NF-κB is a transcription factor with an important role in inducing
genes involved in physiological processes, and is also activated in
response to injury, infection and inflammation (33,34). It
has a crucial role in regulating cell death by inducing apoptosis
(35). In general, NF-κB is bound to
the NF-κB inhibitor (IκBα) protein and activated after stimulation
by certain effectors (36). IκBα is
phosphorylated by the IκB kinase complex and degraded by
proteasomes. Subsequently, NF-κB translocates to the nucleus and
activates the target genes leading to cell death (37). In the present study, cell death was
detected in the 120 mg/kg cimetidine group.
COX-2 is induced by inflammatory stimuli (38). In the present study, increased
amounts of cells positive for COX-2 were detected in Leydig cells
of the 120 mg/kg cimetidine group. However, the levels of T, which
is secreted by Leydig cells, were elevated in the 120 mg/kg
cimetidine group. Elevated serum levels of T resulted from the
combination of two effects: i) An inductive effect caused by LH and
ii) an adverse effect to Leydig cells associated with COX-2
expression. Thus, it was deduced that the inductive effect of LH is
stronger than the adverse effect caused by COX-2 to yield elevated
serum levels of T.
iNOS is modulated by NF-κB. Excessive NO production
due to elevated iNOS causes cytotoxicity and induces germ cell
apoptosis (39,40). Furthermore, NO is a signaling
molecule that has an important role in the pathogenesis of
inflammation (41). In all
cimetidine treatment groups, iNOS expression was detected. In
addition, the cells with iNOS expression were Sertoli cells. These
results suggested that Sertoli cells are also affected by
cimetidine. Furthermore, 9 weeks of treatment with an excessive
dose of cimetidine led to inflammation in the testis and germ cell
apoptosis, as demonstrated in the TUNEL assay.
In conclusion, the results of the present study
indicated that 9 weeks of oral treatment with cimetidine adversely
affects the reproductive system of male rats by disturbing hormone
secretion and inducing germ cell apoptosis. A possible mechanism is
that toxicity to the testes caused by cimetidine may be associated
with NF-κB, iNOS and COX-2 expression, which requires further
research for confirmation.
References
|
1
|
Scheinfeld N: Cimetidine: A review of the
recent developments and reports in cutaneous medicine. Dermatol
Online J. 9:42003.PubMed/NCBI
|
|
2
|
Knigge U, Dejgaard A, Wollesen F,
Ingerslev O, Bennett P and Christiansen PM: The acute and long term
effect of the H 2-receptor antagonists cimetidine and ranitidine on
the pituitary-gonadal axis in men. Clin Endocrinol (Oxf).
18:307–313. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Winters SJ, banks JL and Loriaux DL:
Cimetidine is an antiandrogen in the rat. Gastroenterology.
76:504–508. 1979.PubMed/NCBI
|
|
4
|
Peden NR, Boyd EJ, Browning MC, Saunders
JH and Wormsley KG: Effects of two histamine H2-receptor blocking
drugs on basal levels of gonadotrophins, prolactin, testosterone
and oestradiol-17βduring treatment of duodenal ulcer in male
patients. Acta Endocrinol (Copenh). 96:564–568. 1981.PubMed/NCBI
|
|
5
|
Wang C, Lai CL, Lam KC and Yeung KK:
Effect of cimetidine on gonadal function in man. Br J Clin
Pharmacol. 13:791–794. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kokhaei P, Barough MS and Hassan ZM:
Cimetidine effects on the immunosuppression induced by burn injury.
Int Immunopharmacol. 22:273–276. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kubecova M, Kolostova K, Pinterova D,
Kacprzak G and Bobek V: Cimetidine: An anticancer drug? Eur J Pharm
Sci. 42:439–444. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Peden NR, Cargill JM, Browning MC,
Saunders JH and Wormsley KG: Male sexual dysfunction during
treatment with cimetidine. Br Med J. 1:6591979. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
França LR, Leal MC, Sasso-Cerri E,
Vasconcelos A, Debeljuk L and Russell LD: Cimetidine (Tagamet) is a
reproductive toxicant in male rats affecting peritubular cells.
Biol Reprod. 63:1403–1412. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gill M, Sareen ML and Sanyal SN: Effect of
H2-receptor antagonists, cimetidine and ranitidine on reproductive
functions in male mice. Indian J Exp Biol. 29:900–906.
1991.PubMed/NCBI
|
|
11
|
Pereira OC: Some effects of cimetidine on
the reproductive organs of rats. Gen Pharmacol. 18:197–199. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sasso-Cerri E, Giovanoni M, Hayashi H and
Miraglia SM: Morphological alterations and intratubular lipid
inclusions as indicative of spermatogenic damage in cimetidine
treated rats. Arch Androl. 46:5–13. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sasso-Cerri E and Miraglia SM: In situ
demonstration of both TUNEL-labeled germ cell and Sertoli cell in
the cimetidine-treated rats. Histol Histopathol. 17:411–417.
2002.PubMed/NCBI
|
|
14
|
Sasso-Cerri E and Cerri PS: Morphological
evidences indicate that the interference of cimetidine on the
peritubular components is responsible for detachment and apoptosis
of Sertoli cells. Reprod Biol Endocrinol. 6:182008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Beltrame FL, Yamauti CT, Caneguim BH,
Cerri PS, Miraglia SM and Sasso-Cerri E: Cimetidine-induced
vascular cell apoptosis impairs testicular microvasculaature in
adult rats. Histol Histopathol. 27:1343–1351. 2012.PubMed/NCBI
|
|
16
|
Koshimizu JY, Beltrame FL, de Pizzol JP
Jr, Cerri PS, Caneguim BH and Sasso-Cerri E: NF-κB overexpression
and decreased immunoexpression of AR in the muscular layer is
related to structural damages and apoptosis in cimetidine-treated
rat vas deferens. Reprod Biol Endocrinol. 11:292013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Karin M, Cao Y, Greten FR and Li ZW:
NF-kappaB in cancer: From innocent bystander to major culprit. Nat
Rev Cancer. 2:301–310. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Li Q and Verma IM: NF-kappaB regulation in
the immune system. Nat Rev Immunol. 2:725–734. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Orlowski RZ and Baldwin AS Jr: NF-kappaB
as a therapeutic target in cancer. Trends Mol Med. 8:385–389. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Deveraux QL and Reed JC: IAP family
proteins-suppressors of apoptosis. Genes Dev. 13:239–252. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Liang Y, Zhou Y and Shen P: NF-kappaB and
its regulation on the immune system. Cell Mol Immunol. 5:343–350.
2004.
|
|
22
|
Subbarmaiah K and Dannenberg AJ:
Cyclooxygenase 2: A molecular target for cancer prevention and
treatment. Trends Pharmacol Sci. 24:96–102. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Bogdan C: The multiplex function of nitric
oxide in (auto) immunity. J Exp Med. 187:1361–1365. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bogdan C: Nitric oxide and the immune
response. Nat Immunol. 2:907–916. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Moncada S: Nitric oxide: Discovery and
impact on clinical medicine. J R Soc Med. 92:164–169. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gong QH, Wu Q, Huang XN, Sun AS, Nie J and
Shi JS: Protective effect of Ginkgo biloba leaf extract on learning
and memory deficit induced by aluminum in model rats. Chin J Integr
Med. 12:37–41. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ilbey YO, Ozbek E, Simsek A, Otunctemur A,
Cekmen M and Somay A: Potential chemoprotective effect of melatonin
in cyclophosphamide- and cisplatin-induced testicular damage in
rats. Fertil Steril. 92:1124–1132. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zaninotto F, La Camera S, Polverari A and
Delledonne M: Cross talk between reactive nitrogen and oxygen
species during the hypersensitive disease resistance response.
Plant Physiol. 141:379–383. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kim SF, Huri DA and Snyder SH: Inducible
nitric oxide synthase binds, S-nitrosylates and activates
cyclooxygenase-2. Science. 310:1966–1970. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Scobie IN, Saunders J, Barnes GD, Hoad J,
Wheeler MJ, Lowry C, Sonksen PH, Amphlett G and Riley AJ: A
comparative study of the effects of ranitidine and cimetidine on
carbohydrate tolerance, growth hormone secretion and the
hypothalamic-pituitary-gonadal axis in man. Curr Med Res Opin.
10:285–290. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kyriakis JM and Avruch J: Mammalian
mitogen-activated protein kinase signal transduction pathways
activated by stress and inflammation. Physiol Rev. 81:807–869.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Bubici C, Papa S, Dean K and Franzoso G:
Mutual cross-talk between reactive oxygen species and nuclear
factor-kappa B: Molecular basis and biological significance.
Oncogene. 25:6731–6748. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Bowie A and O'Neill LA: Oxidative stress
and nuclear factor-kappaB activation: A reassessment of the
evidence in the light of recent discoveries. Biochem Pharmacol.
59:13–23. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Hoesel B and Schmid JA: The complexity of
NF-κB signaling in inflammation and cancer. Mol Cancer. 12:862013.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Erl W, Hansson GK, de Martin R, Draude G,
Weber KS and Weber C: Nuclear factor-kappa B regulates induction of
apoptosis protein-1 expression in vascular smooth muscle cells.
Circ Res. 84:668–677. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Rodriguez MS, Thompson J, Hay RT and
Dargemont C: Nuclear retention of IkappaBalpha protects it from
signal-induced degradation and inhibits nuclear factor kappaB
transcriptional activation. J Biol Chem. 274:9108–9115. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Karin M: How NF-kappaB is activated: The
role of the IkappaB kinase (IKK) complex. Oncogene. 18:6867–6874.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ricciotti E and FitzGerald GA:
Prostaglandins and inflammation. Arterioscler Thromb Vasc Biol.
31:986–1000. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Lue Y, Hikim Sinha AP, Wang C, Leung A and
Swerdloff RS: Functional role of inducible nitric oxide synthase in
the induction of male germ cell apoptosis, regulation of sperm
number and determination of testes size: Evidence from null mutant
mice. Endocrinology. 144:3092–3100. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Napli C, Paolisso G, Casamassimi A,
Al-Omran M, Barbieri M, Sommese L, Infante T and Ignarro LJ:
Effects of nitric oxide on cell proliferation: novel insights. J Am
Coll Cardiol. 62:89–95. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Sharma JN, Al-Omran A and Parvathy SS:
Role of nitric oxide in inflammatory diseases.
Inflammopharmacology. 15:252–259. 2007. View Article : Google Scholar : PubMed/NCBI
|