Introduction
Chronic obstructive pulmonary disease (COPD)
represents a frequently occurring chronic respiratory condition,
with its primary pathological manifestation exhibited characterized
by expiratory airflow limitation (1). Clinical statistical data has indicated
that COPD ranks fourth worldwide in regard to its mortality rate
and fifth with in relation to the future burden of disease (by
2020) (2). COPD generally observed
amongst older individuals aged ≥75 years. Furthermore, the
exacerbation of COPD remains a large risk factor resulting in
hospitalization and increasing mortality rates (3). It is widely accepted in concert with
literature, that COPD is caused by chronic airway inflammation with
a strong correlation to tobacco smoking as well as inhalation of
foreign particles (4). COPD
awareness is growing, educating people about airway inflammation as
the foremost cause of COPD, with the markers of systemic
inflammation being entirely responsible for the deaths amongst COPD
patients, including that of tumor necrosis factor (TNF)-α,
interleukin 6 (IL-6) and IL-8 (5).
COPD patients commonly experience both physiological and
pathological changes, including increases in respiratory center
drive, gastric and negative intrathoracic pressure, as well as
abnormally high levels of pulmonary inflammation (6). Interestingly, recent years have brought
with them several symptoms of gastroesophageal reflux (GER) in
combination in patients suffering from chronic respiratory diseases
(7).
GER is one of the most common
gastrointestinal-related outpatient diagnoses, associated with a
series of symptoms including, chest pain, acid regurgitation,
heartburn and food reflux (8). The
gold standard in regard to the diagnosis of GERD, is comprised of a
24 h esophageal pH monitoring system which is applied in a variety
of approaches (9). At present, the
general GER treatment approach revolves around acid suppression,
anti-reflux drug, maintenance therapy, and antacids (10). Furthermore, anti-secretion represents
the chief treatment tool for GER, comprised of H2 receptor
antagonists (H2RA) and proton pump inhibitors drug (PPI) (11). Several previous studies have
demonstrated the significant association shared between GER and the
exacerbation of COPD (11,12), indicating that GER as a potential
complication of COPD. However, insignificant research has been
performed investigating the impact of anti-reflux treatment for
patients with stable COPD in combination with GER from a pulmonary
ventilation function and inflammatory cytokine level perspective.
Hence, the present study aimed to investigate the effects of the
anti-reflux treatment on pulmonary ventilation function and
inflammatory cytokines in patients with stable COPD and GER.
Materials and methods
Ethical statement
All participating subjects signed written informed
consent documents. The present study was performed with the
approval of the Ethical Committee of the People's Hospital of
Guangxi Zhuang Autonomous Region.
Study subjects
Between July 2014 and November 2015, a total of 136
patients suffering from both COPD and GER (100 males and 36
females; mean age: 55.85±8.29 years; mean course of disease:
6.46±1.54 years) who had been admitted to the People's Hospital of
Guangxi Zhuang Autonomous Region were recruited for the purposes of
the study. The patients were randomly divided into either the
routine treatment group (receiving conventional treatment) or the
anti GER group (receiving conventional treatment and anti-reflux
treatment). The routine treatment group comprised of 70 subjects
(53 males and 17 females) with a mean age of 54.89±8.23 years,
while the anti GER group comprised of 66 subjects (47 males and 19
females) with a mean age of 56.86±8.29 years. The subject inclusion
criteria was as follows: patients diagnosed with stable COPD based
on the Global Initiative for Chronic Obstructive Lung Disease
(http://www.goldcopd.com); patients with positive
GER, namely reflux esophagitis (RE); patients with Barrett
esophagus; patients with typical symptoms such as heartburn or acid
reflux (13,14); or patients with a DeMeester score
>14.72 following a 24-h gastric esophageal pH monitoring
(15); The exclusive criteria for
subjects were as below: Patients of Chinese Han ethnicity; patients
with stable or mild symptoms of cough, sputum and dyspnea; patients
who had previously recovered from an acute exacerbation of COPD.
The exclusion criteria for subjects were as follows: Minority and
foreign patients; patients with other lung and heart diseases,
including disease like lung tumor, asthma, congestive heart failure
(CHF), bronchiectasis, tuberculosis; patients with upper and lower
respiratory tract infections in the first 2 months before the date
of study; patients with PPI treatment at 2 weeks prior to the
visit; or patients with steroid hormone treatment 4 weeks prior to
the visit.
Routine treatment
Patients in the routine treatment group received
conventional treatments, including anti infection, eliminating
phlegm and airway dilatation. Non-drug therapy: All patients were
required to comply with an smoking cessation policy, take part in
physical activity and pulmonary rehabilitation, and avoid personal
exposure to occupational dust, smoke and air pollution. Drug
therapy: Patients were treated with β2 receptor agonist salbutamol
(Changzhou Yabang Pharmaceutical Co., Ltd., Changzhou, China), were
asked to inhale corticosteroids (ICS) and fluticasone propionate
(GlaxoSmithKline Company, London, UK); salbutamol administration
was controlled and administered at a dosage of 0.1~0.2 mg 4~6 times
a day; the dosage for fluticasone propionate was 500 ug 2 times a
day.
Anti-reflux treatment
Patients in the anti GER group received additional
anti-reflux treatment in conjunction with their conventional
treatment programs. The primary regimen involved a combination of
acid suppression and prokinetics. The patients were administrated
oral antacid (PPI omeprazole; Harbin Pharmaceutical Pharmaceutical
Group Sanjing Pharmaceutical Nuojie Co., Ltd., Harbin, China), at a
dosage of 40 mg per day over a 6-month period, along with oral
prokinetics mosapride (Shanghai Sine Pharmaceutical Co., Ltd.,
Shanghai, China), 5 mg per day.
Detection of pulmonary ventilation
function
All patients underwent a pulmonary ventilation
function examination before and 6 months after treatment using a
spirograph (Jeager Company, Germany). Patients were placed in a
seated position and were asked to inhale 400 µg of ventolin, 15 min
after which they were examined between 3 and 5 times repeatedly.
The optimal value obtained was used for analysis. The measured
parameters included forced vital capacity (FVC), forced expiratory
volume in one second (FEV1), the ratio of FVC in the normal
reference value (FVC%) and the ratio of FEV1 in the normal
reference value (FEV1%). The results were presented in the form of
percentages in relation to the recorded values as well as reference
values.
Enzyme-linked immunosorbent assay
(ELISA)
Sputum was collected 6 months before and after
treatment, and shaken at 3,000 rpm for 15 min. The supernatant was
retrieved for inflammatory cytokine detection. IL-13 and TGF-β1
ELISA kits were acquired from Shanghai Bio-Tech Co., Ltd.
(Shanghai, China), while tumor necrosis factor α (TNF-α) and IL-18
ELISA kits were acquired from Shenzhen Juying Biotechnology Co.,
Ltd. (Shenzhen, China). EILSA application processes were conducted
in accordance with the instructions, with the intra- and
inter-assays maintained within a range of 10%. Finally, the
absorbance value was read by a spectrophotometer (Thermo Fisher
Scientific, Inc., Waltham, MA, USA) at the wavelength of 450 nm
with a wavelength of 620 nm employed as the reference value.
Collection of bronchoalveolar lavage
fluid and inflammatory cell detection
All patients were intramuscularly injected with 0.5
mg of atropine prior to bronchoscopy and bronchoalveolar lavage
applications, 6 months before and after treatment. Local anesthesia
of the airway was conducted using a 1% lydocaine solution. A total
of 20 ml sterile normal saline was used to lavage the third or
fourth sub-segmental bronchus. The lavage fluid was removed as much
as possible (the recovery was about 50%). Bronchoalveolar lavage
was processed gently and carefully in order minimizes the pain
experienced by the patients. Sputum, blood and carbon foam samples
were unqualified. The qualified lavage fluid was placed in an ice
box and was quickly sent to laboratory for centrifugation. After
centrifugation at 2,000 r/min for 15 min, the supernatant was
removed and the subsided cells were kept for subsequent
experiments. The subsided cells were re-suspended above 1 ml normal
saline. Using a small amount of subsided cells, the total numbers
of cells were then counted using a blood cell counting plate.
Meanwhile, smear and Wright's staining methods were conducted using
a small amount of cells. According to their morphological
characteristics, 500 cells were counted respectively at high
magnification as monocyte, lymphocyte, eosinophil and neutrophil
cells. After counting, the respective percentages were also
calculated.
Test of 6-minute walking distance
(6MWD)
In accordance with the American Thoracic Society
guidelines (16), using a 30 meters
long straight aisle with three chairs in the middle and the ends of
the aisle (as a marked position or resting place for subjects),
patients were asked to walk back and forth in order to record 6MWD
after becoming familiar with the test environment and process.
During the test procedure, the respiratory rate, heart rate, as
well as blood pressure of the subjects were carefully monitored.
The test was immediately terminated in the event that any symptoms
of dizziness, along with anhelation and other symptoms were
observed among the subjects.
Acute exacerbation of COPD
(AECOPD)
AECOPD was confirmed in patients who suffered from
short-term continuous deterioration beyond daily conditions along
with the following symptoms, including cough and wheezing, purulent
sputum, increased sputum secretion, severe fever, insomnia,
fatigue, depression or sleepiness, mental disorders, and body
discomfort. A decline in exercise tolerance and (or) chest image
abnormalities were deemed to be significant signs of AECOPD. The
diagnosis criteria of AECOPD were as follows: 1) patients with
aggravated anhelation; 2) patients with increased sputum secretion:
3) patients with purulent sputum. Patients diagnosed with at least
two conditions of the aforementioned criteria were subsequently
diagnosed with AECOPD.
Body mass index (BMI), obstruction,
dyspnea, exercise (BODE) index
The BODE index has been demonstrated to be a crucial
indicator in the evaluation of the prognosis of patients with COPD.
A greater BODE index indicated a worse prognosis of patients.
Patient BODE indexes were monitored (17) before and after 6 months of treatment
among the COPD patients. The grading criteria were as follows: The
value of BMI (B) >21 kg/m2 recorded as 0 point, ≤21
kg/m2 as 1 point; airflow obstruction (O) FEV1% ≥65%
recorded as 0 point, 50–64% as 1 point, 36–49% as 2 points and ≤35%
as 3 points; 6-m in walking distance ≥350 m recorded as 0 point,
250–349 m as 1 point, 150–249 m as 2 points and ≤149 m as 3 points;
dyspnea index (D) 0–1 recorded as 0 point, 2 as 1 point, 3 as 2
points and 4 as 3 points.
Statistical analysis
Data were analyzed using SPSS v21.0 (IBM Corp.,
Armonk, NY, USA). Data that was continuously measured data was
presented as mean ± standard deviation, and one-way ANOVA followed
by the LSD test was performed for multiple group comparisons.
Categorical data was presented in terms of specific numerical
cases, and analyzed by chi-square test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Baseline characteristics of patients
with COPD between the routine treatment group and anti GER
group
As shown in Table I,
no significant differences were observed in terms of age, gender,
course of disease, smoke, BMI, PaCO2, PaO, plasma
albumin and AECOPD incidents between the routine treatment group
and anti GER group and the results of both groups were comparable
(all P>0.05). The routine treatment group consisted of 70
patients, including 50 smokers, among whom 49 individuals were
confirmed to have adhered to the smoking cessation requirement of
the study. The anti GER group comprised of 66 patients, including
48 smokers, among whom 42 people were able to maintain the smoking
cessation status during the test. There was no significant
difference detected in relation to the number of smokers between
the two groups at baseline. Out of the 136 patients, 25 experienced
esophagitis, while 3 patients suffered from Barrett esophagus. No
adverse reaction in the routine treatment group was observed, and
only 1 patient experienced symptoms of nausea and vomiting in the
anti GER group.
 | Table I.Baseline characteristics of COPD
patients in the routine treatment and anti GER groups. |
Table I.
Baseline characteristics of COPD
patients in the routine treatment and anti GER groups.
| Variables | Routine treatment
group (n=70) | Anti GER group
(n=66) | P-value |
|---|
| Age (years) |
|
| 0.835 |
| ≤55 | 38 | 37 |
|
|
>55 | 32 | 29 |
|
| Sex |
|
| 0.595 |
| Male | 53 | 47 |
|
|
Female | 17 | 19 |
|
| Course of disease
(years) | 6.39±1.61 | 6.53±1.48 | 0.598 |
| Smoke (yes/no) | 50/20 | 48/18 | 0.866 |
| BMI |
|
| 0.308 |
| ≤21 | 39 | 31 |
|
|
>21 | 31 | 35 |
|
| PaCO2
(mmHg) |
|
| 0.118 |
| ≤40 | 36 | 32 |
|
|
>40 | 34 | 34 |
|
| PaO (mmHg) |
|
| 0.636 |
| ≤60 | 27 | 22 |
|
|
>60 | 43 | 44 |
|
| Plasma albumin
(g/l) | 34.30±0.53 | 34.20±0.51 | 0.265 |
| Times of AECOPD
(times/year) | 3.0±1.3 | 2.6±1.2 | 0.065 |
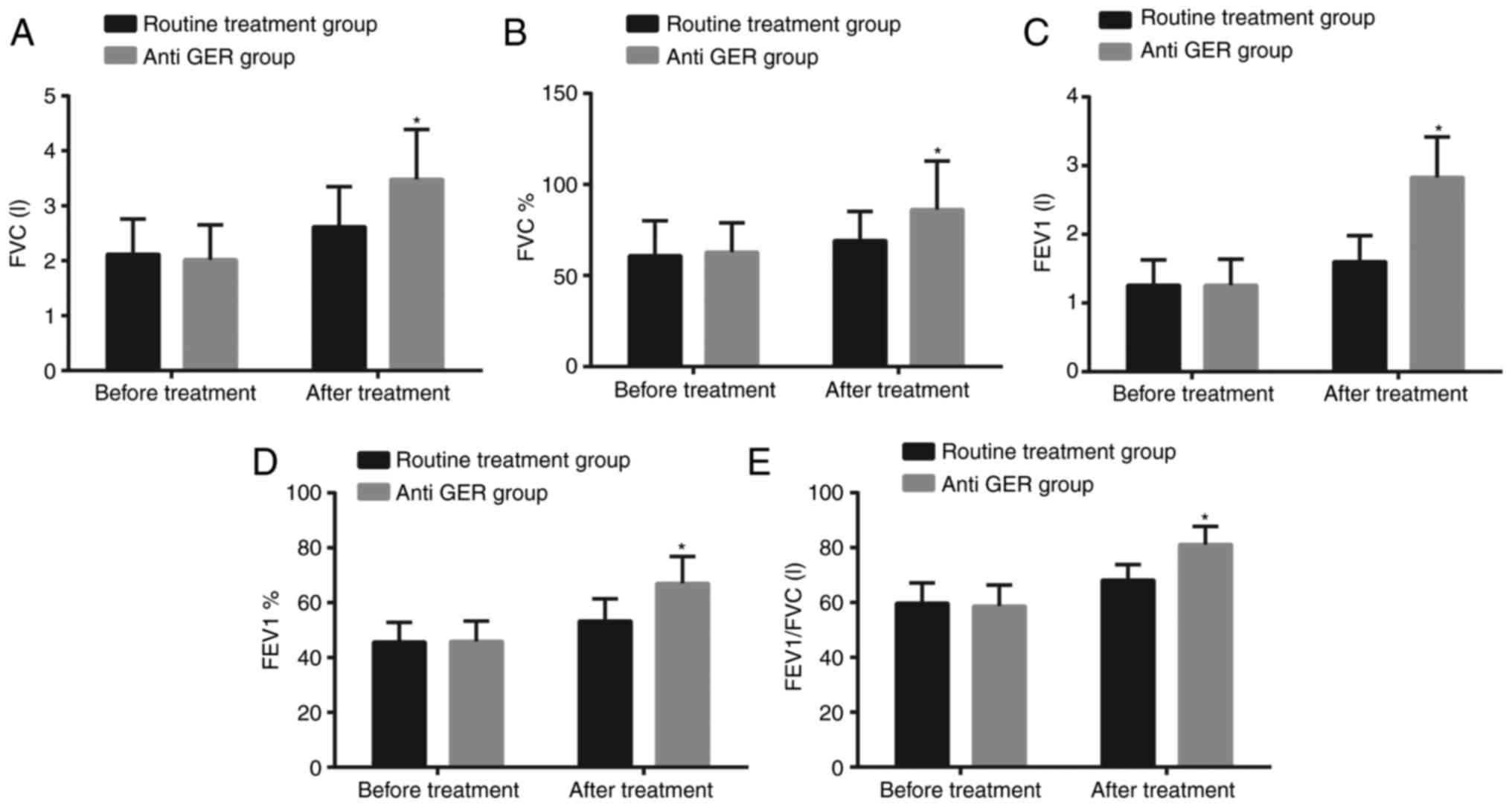
Pulmonary ventilation function of
patients in the anti GER group was higher than in the routine
treatment group after treatment
Pulmonary ventilation function was examined before
treatment and 6 months after treatment (Fig. 1). Prior to treatment, no significant
differences were observed in parameters [FVC (L), FVC%, FEV1 (L),
FEV1% and FEV1/FVC (L)] of pulmonary ventilation function between
the routine treatment group and anti GER group (all P>0.05). Six
months after treatment, all the aforementioned parameters increased
in both the routine treatment and anti GER groups; and these
parameters in the anti GER group were significantly higher compared
to the value of the routine treatment group (all P<0.05).
Anti GER treatment reduced
inflammatory cytokines
Prior to the treatment, there was no significant
difference detected in regard to the levels of inflammatory
cytokines IL-13, IL-18, transforming growth factor-β1 (TGF-βl) and
TNF-α between the routine treatment group and anti GER group (all
P>0.05). Six months after treatment, the levels of IL-13, IL-18,
TGF-βl and TNF-α decreased in both the routine treatment and anti
GER groups; and the levels of IL-13, IL-18, TGF-βl and TNF-α in the
anti GER group were significantly lower compared to the levels
observed in the routine treatment group (all P<0.05; Fig. 2).
Anti GER treatment relieved
inflammation
The total number of cells determined in the
respective bronchoalveolar lavage fluid as well as the percentage
of inflammatory cells between the two groups was compared (Table II). Before treatment, there was no
significant difference observed in regard to the total number of
cells in bronchoalveolar lavage fluid and percentage of
inflammatory cells (monocyte, lymphocyte, eosinophil and neutrophil
cells) (all P>0.05). Compared with situation before treatment,
the total number of inflammatory cells and the percentage of
eosinophil cells significantly decreased with remarkable increases
of monocyte, lymphocyte, and neutrophil cells observed in both
groups 6 months after treatment (all P<0.05). The total number
of inflammatory cells and percentage of eosinophil cells in the
anti GER group were remarkably lower than in the routine treatment
group; however the percentages of monocyte, lymphocyte, and
neutrophil cells were noticeably higher than in the routine group
(all P<0.05).
 | Table II.The total number of inflammatory
cells and percentage of eosinophil cells of patients were lower
with higher percentages of monocyte, lymphocyte, and neutrophil
cells in the anti GER group after treatment. |
Table II.
The total number of inflammatory
cells and percentage of eosinophil cells of patients were lower
with higher percentages of monocyte, lymphocyte, and neutrophil
cells in the anti GER group after treatment.
|
|
| Cell percentage
(%) |
|---|
|
|
|
|
|---|
| Group | Total inflammatory
cells (10–8) | Lymphocyte | Neutrophil | Eosinophil | Monocyte |
|---|
| Routine treatment
group |
|
|
|
|
|
| Before
treatment | 4.64±0.36 | 3.91±0.24 | 20.25±1.15 | 8.89±0.46 | 49.12±2.97 |
| 6
months after treatment |
2.85±0.15a |
5.76±0.46a |
28.34±1.61a |
6.74±0.51a |
56.75±3.30a |
| Anti GER group |
|
|
|
|
|
| Before
treatment | 4.53±0.37 | 3.82±0.29 | 20.48±2.02 | 8.56±0.54 | 50.13±3.18 |
| 6
months after treatment |
2.41±0.19a,b |
7.49±0.63a,b |
36.11±2.27a,b |
4.21±0.32a,b |
65.33±4.82a,b |
6MWD increased and times of AECOPD
decreased of patients in the anti GER group
Prior to treatment, the patients in the routine
treatment group and anti GER group displayed no significant
differences in relation to 6MWD and AECOPD incidents (both
P>0.05). Six months after treatment, the patients in the routine
treatment and anti GER groups exhibited increased 6MWD and
decreased number of AECOPD incidents (both P<0.05); while the
patients in the anti GER group had longer 6MWD and lesser AECOPD
incidents compared to the routine treatment group (both P<0.05;
Table III).
 | Table III.Comparison of 6MWD and the times of
AECOPD between the routine treatment and anti GER groups before and
6 months after treatment. |
Table III.
Comparison of 6MWD and the times of
AECOPD between the routine treatment and anti GER groups before and
6 months after treatment.
|
| Routine treatment
group |
| Anti GER group |
|
|---|
|
|
|
|
|
|
|---|
| Index | Before
treatment | 6 months after
treatment | P-value | Before
treatment | 6 months after
treatment | P-value |
|---|
| 6MWD (m) | 766.22±110.78 | 983.24±115.61 | <0.001 | 701.37±113.64 |
1159.45±115.23a | <0.001 |
| AECOPD (times) | 4.64±0.89 | 2.61±0.82 | <0.001 | 4.56±0.86 |
2.03±0.66a | <0.001 |
BODE index of patients decreased in
the anti GER
The respective BODE indexes were evaluated for
determination of the prognosis of patients with COPD (Table IV). There was no significant
difference in the BODE index in the routine treatment group and the
anti GER group prior the treatment (P>0.05). Six months after
treatment, the BODE indexes had decreased significantly in both the
routine treatment and anti GER groups (both P<0.05); the BODE
index was significantly lower in the anti GER group compared to the
routine treatment group (P<0.05).
 | Table IV.BODE index between the routine
treatment and anti GER groups before and 6 months after
treatment. |
Table IV.
BODE index between the routine
treatment and anti GER groups before and 6 months after
treatment.
|
| BODE index |
|---|
|
|
|
|---|
| Group | Before
treatment | 6 months after
treatment | P-value |
|---|
| Routine treatment
group | 2.47±0.50 | 1.89±0.58 | <0.001 |
| Anti GER group | 2.52±0.81 |
1.15±0.73a | <0.001 |
BODE index of patients was higher in
the anti GER group with a longer course of disease and more AECOPD
incidents
To further evaluate the relationship between the
treatment effects and clinicopathological characteristics, the
relationship between BODE index as well as the clinicopathological
characteristics after treatment in the anti GER group were all
analyzed, shown in Table V. The BODE
index was found to be associated with the course of the disease and
AECOPD incidents after treatment (both P<0.05). The BODE index
was confirmed to be higher with a longer course of disease and more
AECOPD incidents. No significant difference was observed between
the BODE index after treatment and parameters including age,
gender, smoke, BMI, PaCO2, PaO and plasma albumin.
 | Table V.Relationship between BODE index and
clinical pathology after treatment in the anti GER group. |
Table V.
Relationship between BODE index and
clinical pathology after treatment in the anti GER group.
| Variables | 0 | 1 | 2 | 3 | P-value |
|---|
| Age (years) |
|
|
|
| 0.198 |
|
≤55 | 4 | 21 | 9 | 3 |
|
|
>55 | 5 | 21 | 2 | 1 |
|
| Sex |
|
|
|
| 0.612 |
|
Male | 6 | 29 | 8 | 4 |
|
|
Female | 3 | 13 | 3 | 0 |
|
| Course of disease
(years) | 5.60±0.92 | 6.42±1.54 | 7.30±1.25 | 7.64±0.96 | <0.001 |
| Smoke (yes/no) | 5/4 | 31/11 | 10/1 | 2/2 | 0.237 |
| BMI |
|
|
|
| 0.525 |
|
≤21 | 3 | 19 | 6 | 3 |
|
|
>21 | 6 | 23 | 5 | 1 |
|
| PaCO2
(mmHg) |
|
|
|
| 0.677 |
|
≤40 | 5 | 19 | 5 | 3 |
|
|
>40 | 4 | 23 | 6 | 1 |
|
| PaO (mmHg) |
|
|
|
| 0.375 |
|
≤60 | 1 | 16 | 3 | 2 |
|
|
>60 | 8 | 26 | 8 | 2 |
|
| Plasma albumin
(g/l) | 34.27±0.71 | 34.20±0.47 | 34.15±0.54 | 34.18±0.50 | 0.654 |
| Times of AECOPD
(times/years) | 2.22±1.48 | 2.60±1.06 | 2.73±1.27 | 3.00±2.45 | <0.001 |
Discussion
COPD is a widespread chronic disease associated with
negative intra-thoracic pressure, increased respiratory center
drive, as well as flat diaphragm. Exacerbation of COPD is widely
considered to be the primary factor responsible for lowering the
quality of life in patients and can contribute to deteriorating
lung function. GER has more recently, been earmarked as a potential
risk factor contributing to the exacerbation of COPD (18). There exists a high prevalence of GER
among COPD patients. Likewise, patients with more GER symptoms are
at a higher risk of suffering from COPD (19,20). GER
symptoms have been linked to COPD diagnoses and patients with GER
suffered from increased frequency of exacerbations every year
(21). Thus, the study investigated
the relationship between anti-reflux treatment and inflammatory
cytokines as well as the lung function change among patients with
stable COPD along with GER.
Initially, the research successfully confirmed that
pulmonary ventilation function in patients with COPD significantly
improved after anti-reflux treatment. The overall results primarily
demonstrated that FEV1, FEV1% and FEV1/FVC remarkably decreased
after anti-reflux treatment. Continuous gastric reflux material and
aspiration can trigger lower airway inflammation and bronchospasm,
and the reflux content has been shown to damage the respiratory
epithelium, which can lead to various clinical manifestations
associated with inflammatory effects (22). Phulpoto et al (23), reported that FEV1 had a significant
association on the severity of airway obstruction with frequent
gastroesophageal symptoms. These results were in concert with
former findings that anti-reflux medication to be an important
factor for objective tests and diagnostic confirmation of GER in
patients with COPD. Another significant result suggested that the
levels of IL-13, IL-18, TGF-βl, and TNF-α in the sputum of patients
with COPD significantly reduced. By evaluating the difference and
the total number and distribution of inflammatory cells in
bronchoalveolar lavage fluid before and 6 months after treatment, I
found that anti GER treatment decreased the total number, with
higher percentages of monocyte, lymphocyte, and neutrophil cells
and lower percentage of eosinophil cells. As previously described,
inflammation was the largest factor responsible for the occurrence
and progression of COPD (5). IL-13
is a key element in the stimulation of airway inflammation
(24). During the progression of
airway inflammation and structural remodeling, IL-13 was shown to
cause reduplicated airway hyper-reactivity and chronic inflammation
(25). The level of IL-13
significantly increased lung tissue based on a conducted by Crosby
et al (26). IL-18 is mainly
produced by monocytes and macrophages, which activates the release
of toxic oxygen in neutrophils and macrophages (27). A previous study found that IL-18 was
associated with the pathogenesis of COPD and played a crucial role
in the inflammation in patients with COPD (28). Airway remodeling is characterized by
continuous asthma, including increased airway smooth muscle (ASM)
mass and altered extracellular matrix (ECM) deposition.
Interestingly, a significant association between TGF-βl and airway
remodeling on patients with COPD was observed, which might be
induced by high-expression of TGF-βl consequently increased the
thickness of airway and basement membrane, which furthermore
promoted fibronectin from human ASM cells and deposition of ECM
proteins (29). TNF-α, as a
pro-inflammatory cytokine operating at an early stage of the
inflammatory cascade, has been reported to be a central player in
the occurrence of COPD and is again increased when patients are in
the process of suffering from an acute exacerbation attack
(30). Eagan et al (31), highlighted that higher TNF-α level in
patients with COPD was responsible for the pathogenesis of COPD and
associated comorbidities. The protection against GORD has also been
reported to result in the inhibition of the pro-inflammatory
process (32). The aforementioned
information highlighted that anti-reflux treatment could reduce the
incidence of airway inflammation, which significantly reduced the
levels of the inflammatory cytokines IL-13, IL-18, TGF-βl, TNF-α
amongst patients with COPD as well as the total number of
inflammatory cells.
Another significant observation of the study was
that anti-reflux treatment improved the prognosis of patients with
COPD. The 6MWT is a simple test for patients with COPD, which could
be potentially employed as a useful reference in lung function and
depression (33). After anti-reflux
treatment, the pulmonary ventilation function improved amongst
patients with COPD, along with a reduction in the amount of acute
attacks, which consequently increased 6MWD. BMI, airflow
obstruction, dyspnoea and patient exercise capacity index belong to
the multidimensional grading system to predict the risk of death in
patients with COPD and reflect disease severity (34). Hence, the BODE index relatively
decreased due to improved lung function of patients and decreased
levels of inflammatory cytokines.
To conclude, the study presented evidence providing
verification that anti-reflux treatment could improve pulmonary
ventilation function and prognosis of patients with COPD combined
with GER, and decrease the levels of IL-13, IL-18, TGF-βl and
TNF-α, which was indicative of the effectiveness of anti-reflux
treatment in COPD therapy. However, more prospective studies with
causation in the future are needed to focus on developing new
therapeutic strategies for treating COPD with GER. There were some
limitations faced during the study. This study did not include a
well-devised follow-up plan. Therefore, I intended to perform a 2–5
years follow-up to further investigate the long-term prognosis
after GER treatment. The details of the follow-up plan are as
follows: Follow-up method is an outpatient visit; follow-up
contents include follow-up rate and lost follow-up rate of all
patients, and basic safety indexes including vital signs, hematuria
routine, blood biochemistry and pulmonary function test; asking
adverse reactions and combined use of drugs over a period of 2
years. The present study had a relatively small sample size, and as
a result a larger sample size study is required in order to confirm
the reliability of the results.
Acknowledgements
The author wishes to express his gratitude to
reviewers for their critical comments.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Author contribution
HL conceived and designed the study, was involved in
data collection, performed the statistical analysis and preparation
of figures and drafted the paper. HL also contributed substantially
to its revision.
Ethics approval and consent to
participate
All participating subjects signed informal written
consent documents. The present study was performed with the
approval of the Ethical Committee of the People's Hospital of
Guangxi Zhuang Autonomous Region.
Consent for publication
Consent for publication was obtained from the
participants.
Competing interests
The author declares that they have no competing
interests.
References
|
1
|
Delzell JE Jr: Common lung conditions:
Chronic obstructive pulmonary disease. FP Essent. 409:23–31.
2013.PubMed/NCBI
|
|
2
|
Vestbo J, Hurd SS, Agusti AG, Jones PW,
Vogelmeier C, Anzueto A, Barnes PJ, Fabbri LM, Martinez FJ,
Nishimura M, et al: Global strategy for the diagnosis, management,
and prevention of chronic obstructive pulmonary disease: GOLD
executive summary. Am J Respir Crit Care Med. 187:347–365. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Parameswaran Iyer G and Murphy TF: Chronic
obstructive pulmonary disease: Role of bacteria and updated guide
to antibacterial selection in the older patient. Drugs Aging.
26:985–995. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lee H, Kim J and Tagmazyan K: Treatment of
stable chronic obstructive pulmonary disease: The GOLD guidelines.
Am Fam Physician. 88(655–663): 663B–F. 2013.
|
|
5
|
Gan WQ, Man SF, Senthilselvan A and Sin
DD: Association between chronic obstructive pulmonary disease and
systemic inflammation: A systematic review and a meta-analysis.
Thorax. 59:574–580. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Casanova C, Baudet JS, del Valle Velasco
M, Martin JM, Aguirre-Jaime A, de Torres JP and Celli BR: Increased
gastro-oesophageal reflux disease in patients with severe COPD. Eur
Respir J. 23:841–845. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rogha M, Behravesh B and Pourmoghaddas Z:
Association of gastroesophageal reflux disease symptoms with
exacerbations of chronic obstructive pulmonary disease. J
Gastrointestin Liver Dis. 19:253–256. 2010.PubMed/NCBI
|
|
8
|
Liang BM and Feng YL: Association of
gastroesophageal reflux disease symptoms with stable chronic
obstructive pulmonary disease. Lung. 190:277–282. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wang AJ, Liang MJ, Jiang AY, Lin JK, Xiao
YL, Peng S, Chen J, Wen WP and Chen MH: Gastroesophageal and
laryngopharyngeal reflux detected by 24-hour combined impedance and
pH monitoring in healthy Chinese volunteers. J Dig Dis. 12:173–180.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yeh AM and Golianu B: Integrative
treatment of reflux and functional dyspepsia in children. Children
(Basel). 1:119–133. 2014.PubMed/NCBI
|
|
11
|
Ingebrigtsen TS, Marott JL, Vestbo J,
Nordestgaard BG, Hallas J and Lange P: Gastro-esophageal reflux
disease and exacerbations in chronic obstructive pulmonary disease.
Respirology. 20:101–107. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Benson VS, Müllerová H, Vestbo J, Wedzicha
JA, Patel A and Hurst JR: Evaluation of COPD Longitudinally to
Identify Predictive Surrogate Endpoints (ECLIPSE) Investigators:
Associations between gastro-oesophageal reflux, its management and
exacerbations of chronic obstructive pulmonary disease. Respir Med.
109:1147–1154. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lundell LR, Dent J, Bennett JR, Blum AL,
Armstrong D, Galmiche JP, Johnson F, Hongo M, Richter JE, Spechler
SJ, et al: Endoscopic assessment of oesophagitis: Clinical and
functional correlates and further validation of the Los Angeles
classification. Gut. 45:172–180. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Holub JL, Silberg DG, Michaels LC,
Williams JL, Morris CD and Eisen G: Acid-related upper endoscopy
findings in patients with diabetes versus non-diabetic patients.
Dig Dis Sci. 55:2853–2859. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kumbhari V, Familiari P, Bjerregaard NC,
Pioche M, Jones E, Ko WJ, Hayee B, Cali A, Ngamruengphong S, Mion
F, et al: Gastroesophageal reflux after peroral endoscopic myotomy:
A multicenter case-control study. Endoscopy. 49:634–642. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Calik-Kutukcu E, Savci S, Saglam M,
Vardar-Yagli N, Inal-Ince D, Arikan H, Aribas Z, Ozer O,
Bosnak-Guclu M and Coplu L: A comparison of muscle strength and
endurance, exercise capacity, fatigue perception and quality of
life in patients with chronic obstructive pulmonary disease and
healthy subjects: A cross-sectional study. BMC Pulm Med. 14:62014.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Williams JE, Green RH, Warrington V,
Steiner MC, Morgan MD and Singh SJ: Development of the i-BODE:
Validation of the incremental shuttle walking test within the BODE
index. Respir Med. 106:390–396. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kim J, Lee JH, Kim Y, Kim K, Oh YM, Yoo
KH, Rhee CK, Yoon HK, Kim YS, Park YB, et al: Association between
chronic obstructive pulmonary disease and gastroesophageal reflux
disease: A national cross-sectional cohort study. BMC Pulm Med.
13:512013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gadel AA, Mostafa M, Younis A and Haleem
M: Esophageal motility pattern and gastro-esophageal reflux in
chronic obstructive pulmonary disease. Hepatogastroenterology.
59:2498–2502. 2012.PubMed/NCBI
|
|
20
|
Takada K, Matsumoto S, Kojima E, Iwata S,
Okachi S, Ninomiya K, Morioka H, Tanaka K and Enomoto Y:
Prospective evaluation of the relationship between acute
exacerbations of COPD and gastroesophageal reflux disease diagnosed
by questionnaire. Respir Med. 105:1531–1536. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sakae TM, Pizzichini MM, Teixeira PJ,
Silva RM, Trevisol DJ and Pizzichini E: Exacerbations of COPD and
symptoms of gastroesophageal reflux: A systematic review and
meta-analysis. J Bras Pneumol. 39:259–271. 2013.(In English,
Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Pacheco-Galván A, Hart SP and Morice AH:
Relationship between gastro-oesophageal reflux and airway diseases:
The airway reflux paradigm. Arch Bronconeumol. 47:195–203. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Phulpoto MA, Qayyum S, Rizvi N and
Khuhawar SM: Proportion of gastroesophageal reflux symptoms in
patients with chronic obstructive pulmonary disease. J Pak Med
Assoc. 55:276–279. 2005.PubMed/NCBI
|
|
24
|
Oh CK, Geba GP and Molfino N:
Investigational therapeutics targeting the IL-4/IL-13/STAT-6
pathway for the treatment of asthma. Eur Respir Rev. 19:46–54.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hashimoto K, Sheller JR, Morrow JD,
Collins RD, Goleniewska K, O'Neal J, Zhou W, Ji S, Mitchell DB,
Graham BS and Peebles RS Jr: Cyclooxygenase inhibition augments
allergic inflammation through CD4-dependent, STAT6-independent
mechanisms. J Immunol. 174:525–532. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Crosby LM and Waters CM: Epithelial repair
mechanisms in the lung. Am J Physiol Lung Cell Mol Physiol.
298:L715–L731. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
van de Veerdonk FL, Netea MG, Dinarello CA
and Joosten LA: Inflammasome activation and IL-1β and IL-18
processing during infection. Trends Immunol. 32:110–116. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Dima E, Koltsida O, Katsaounou P, Vakali
S, Koutsoukou A, Koulouris NG and Rovina N: Implication of
Interleukin (IL)-18 in the pathogenesis of chronic obstructive
pulmonary disease (COPD). Cytokine. 74:313–317. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Johnson PR, Burgess JK, Ge Q, Poniris M,
Boustany S, Twigg SM and Black JL: Connective tissue growth factor
induces extracellular matrix in asthmatic airway smooth muscle. Am
J Respir Crit Care Med. 173:32–41. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
von Haehling S, Hopkinson NS, Polkey MI,
Niethammer M, Anker SD and Genth-Zotz S: Elevated TNFalpha
production in whole blood in patients with severe COPD: The
potential link to disease severity. Wien Klin Wochenschr.
121:303–308. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Eagan TM, Ueland T, Wagner PD, Hardie JA,
Mollnes TE, Damås JK, Aukrust P and Bakke PS: Systemic inflammatory
markers in COPD: Results from the Bergen COPD cohort study. Eur
Respir J. 35:540–548. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Shahabi S, Rasmi Y, Jazani NH and Hassan
ZM: Protective effects of Helicobacter pylori against
gastroesophageal reflux disease may be due to a neuroimmunological
anti-inflammatory mechanism. Immunol Cell Biol. 86:175–178. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Polkey MI, Spruit MA, Edwards LD, Watkins
ML, Pinto-Plata V, Vestbo J, Calverley PM, Tal-Singer R, Agusti A,
Bakke PS, et al: Six-minute-walk test in chronic obstructive
pulmonary disease: Minimal clinically important difference for
death or hospitalization. Am J Respir Crit Care Med. 187:382–386.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Hernandes NA, Wouters EF, Meijer K,
Annegarn J, Pitta F and Spruit MA: Reproducibility of 6-minute
walking test in patients with COPD. Eur Respir J. 38:261–267. 2011.
View Article : Google Scholar : PubMed/NCBI
|