Introduction
Most cardiovascular diseases develop to heart
failure in their advanced stages, and thus lead to death. Although
various clinical means currently used for the treatment of heart
failure show certain clinical effects, the most common cause of
death in patients in cardiovascular medicine department is still
heart failure (1). At present, the
most commonly used and the most effective method for clinical
diagnosis of heart failure is echocardiogram combined with
radionuclide imaging examination, but not all hospitals and
patients have access to this diagnostic method (2). Especially in primary hospitals, most
clinical diagnoses are performed based on clinical manifestations
and physicians' experience, and error diagnoses and misdiagnoses
cannot be avoided, so both false-positive and false-negative rates
are high (3). Therefore, a
diagnostic method with high positive rate and specificity is needed
in clinical practices for early diagnosis and prognosis prediction
of patients with heart failure (4).
Yu et al (5)
reported that soluble growth stimulation expressed gene 2 (sST2),
which was correlated with ischemic heart disease and heart failure,
can be used to predict the prognosis of heart failure. However,
this method is expensive and complex, so clinical popularization is
difficult, especially for primary hospitals. N-terminal pro-brain
natriuretic peptide (NT-proBNP) is a kind of B-type natriuretic
peptide that is secreted and produced by the heart when heart
failure occurs and ventricular and atrial pressure and volume loads
were obviously increased (5). In the
diagnosis of heart failure, NT-proBNP has advantages of being
economic, simple and reproducible in clinical detections, and
especially fits the need of a primary hospital (6). Matrix metalloproteinase-9 (MMP-9) is
the most important cytokine that mediates myocardial remodeling and
left ventricular dilatation, and plays important roles in the
occurrence and development of heart failure (7). Yan et al (6) reported that MMP-9 could change the
extracellular matrix of cardiomyocytes to promote the development
of heart failure and provide important prognostic information for
left ventricular remodeling in patients with heart failure.
Vorovich et al (7) concluded
that NT-proBNP was more clinically valuable than MMP-9 in
diagnosing ventricular remodeling and predicting prognosis in
patients with congestive heart failure. In this study, changes in
MMP-9 and left ventricular ejection fraction (LVEF) in heart
failure patients were analyzed, and NT-proBNP levels of heart
failure patients with different cardiac function classifications
were measured and values of risk factors of the occurrence of heart
failure in evaluating the prognosis were analyzed.
Patients and methods
General data
A total of 80 heart failure patients with different
cardiac functions who received treatment in Yixing People's
Hospital from January 2016 to June 2017 were chosen. All patients
met the diagnostic criteria for heart failure established by the
Chinese Medical Association in 2015, and were divided into two
groups (group with cardiac function in class II and below and group
with cardiac function in class III and above) in accordance with
the cardiac function classification of New York Heart Association
(NYHA). NYHA I patients have cardiac disease but without the
resulting limitations of physical activity. Ordinary physical
activity does not cause undue fatigue, palpitation, dyspnoea or
anginal pain. NYHA II patients have cardiac disease resulting in
slight limitation of physical activity. They are comfortable at
rest. Ordinary physical activity results in fatigue, palpitation,
dyspnoea or anginal pain. NYHA III patients have cardiac disease
resulting in marked limitation of physical activity. They are
comfortable at rest. Less than ordinary physical activity causes
fatigue, palpitation, dyspnoea or anginal pain. NYHA IV patients
have cardiac disease resulting in inability to carry on any
physical activity without discomfort. Symptoms of cardiac
insufficiency or of the anginal syndrome may be present even at
rest (8). If any physical activity
is undertaken, discomfort is increased. Before enrollment, all
patients signed the informed consent or this was done by their
authorized person, and this study obtained approvals from the
Ethics Committee of Yixing People's Hospital (Yixing, China). Group
with cardiac function in class II and below included 23 males and
17 females, age ranged from 45 to 75 years, with a mean age of
65.3±2.3 years old, of which 18 patients were combined with
diabetes mellitus, and 15 patients were combined with hypertension;
the group with cardiac function in class III and above consisted of
22 males and 18 females, and age ranged from 45 to 75 years, with
an average age of 65.4±2.4 years, of which 17 patients were
combined with diabetes mellitus and 15 patients were combined with
hypertension. There were no statistically significant differences
in sex, age, ratios of patients with diabetes mellitus and
hypertension, levels of NT-proBNP, MMP-9 and LVEF between the two
groups (p>0.05).
Methods for study and
investigation
Blood biochemical test and outcome analysis were
conducted. Elbow venous blood was extracted from all patients in
the morning for measurement of serum NT-proBNP and MMP-9 levels.
Echocardiogram examination was carried out, and correlations
between NT-proBNP and MMP-9 levels in patients with different
cardiac functions with LVEF level were analyzed at the same time.
In terms of the analysis of risk factors, univariate analysis was
first performed to process general data, such as sex, age, cardiac
function, MMP-9, NT-proBNP and LVEF levels, incidence of diabetes
mellitus and hypertension; then, multivariate logistic regression
analyses were applied to identify independent risk factors for
heart failure in patients with different cardiac functions. All
researchers were trained, and a total of 160 questionnaires were
sent to all patients and their attending physicians. The contents
of questionnaires filled in by patients and their physicians were
synthesized, analyzed and summarized.
Assessment methods
Serum samples of all patients were derived from
fasting elbow venous blood extracted from patients on the day of
diagnosis. For detection of MMP-9 and NT-proBNP, ethylenediamine
tetraacetic acid dipotassium anti-coagulant and Sysmex XS-500i
automatic blood biochemical analyzer were used, and all samples
were sent for detection within 30 min after collection. The
detection was performed via bi-directional lateral flow
immunosorbent assay with reagents provided by ReLIA
Biotechnologies, Inc. (Shenzhen, China), and physicians with >5
years of working experience in clinical laboratory were in strict
accordance with instructions. Normal reference range of NT-proBNP
was from 0 to 300. Normal reference range of MMP-9 was from 1.15 to
4.53 µg/l. Color Doppler echocardiography was performed using Sonos
5500 color Doppler ultrasound system with a frequency of 2.5–3.0
MHz. Calibration was performed automatically before measurement.
Left ventricular end-diastolic diameter (LVEDD), left ventricular
end-systolic diameter (LVESD), LVEF (%) and data relating to
cardiac ultrasound were continuously measured 3 times and averaged
by the same physician who had >5 years of working experience in
ultrasonic diagnosis.
Statistical analysis
Statistical treatment was performed via Statistical
Product and Service Solutions (SPSS) 21.0. Measurement data were
expressed as mean ± standard deviation (SD), and t-test was used
for comparisons between the two groups, and χ2 test was
used for intragroup comparisons. Univariate and multivariate
logistic regression analyses were used to analyze relevant risk
factors for heart failure in patients with different cardiac
functions. Correlations between LVEF and NT-proBNP, and between
LVEF and MMP-9, were analyzed using Spearman's rank method.
P<0.05 indicates that the difference was statistically
significant.
Results
Comparison of serum NT-proBNP and
MMP-9 levels in patients with different cardiac functions
The levels of serum NT-proBNP and MMP-9 in the group
with cardiac function in class II and below were significantly
lower than those in the group with cardiac function in class III
and above (p<0.05) (Table I).
 | Table I.Comparison of serum NT-proBNP and
MMP-9 levels in patients with different cardiac functions
(x±s). |
Table I.
Comparison of serum NT-proBNP and
MMP-9 levels in patients with different cardiac functions
(x±s).
| Different cardiac
functions | NT-proBNP
(pg/ml) | MMP-9 (µg/l) |
|---|
| Cardiac function in
class II and below |
156.8±25.1a |
2.02±0.06a |
| Cardiac function in
class III and above | 458.9±56.3 | 4.11±0.12 |
| t | 30.996 | 98.524 |
| P-value | <0.001 | <0.001 |
Comparison of levels of detected data
relating to echocardiogram between the two groups
Compared with the group with cardiac function in
class III and above, group with cardiac function in class II and
below had obviously lower LVEDD and LVESD (p<0.05), but higher
LVEF (p<0.05) in echocardiogram indexes (Table II).
 | Table II.Comparison of LVEDD, LVESD and LVEF in
patients with different cardiac functions (x±s). |
Table II.
Comparison of LVEDD, LVESD and LVEF in
patients with different cardiac functions (x±s).
| Different cardiac
functions | LVEDD (mm) | LVESD (mm) | LVEF (%) |
|---|
| Cardiac function in
class II and below | 46.8±3.6a | 43.5±2.9a | 46.5±2.9a |
| Cardiac function in
class III and above | 65.6±5.3 | 63.3±5.0 | 35.6±1.9 |
| t | 18.558 | 21.665 | 19.884 |
| P-value | <0.001 | <0.001 | <0.001 |
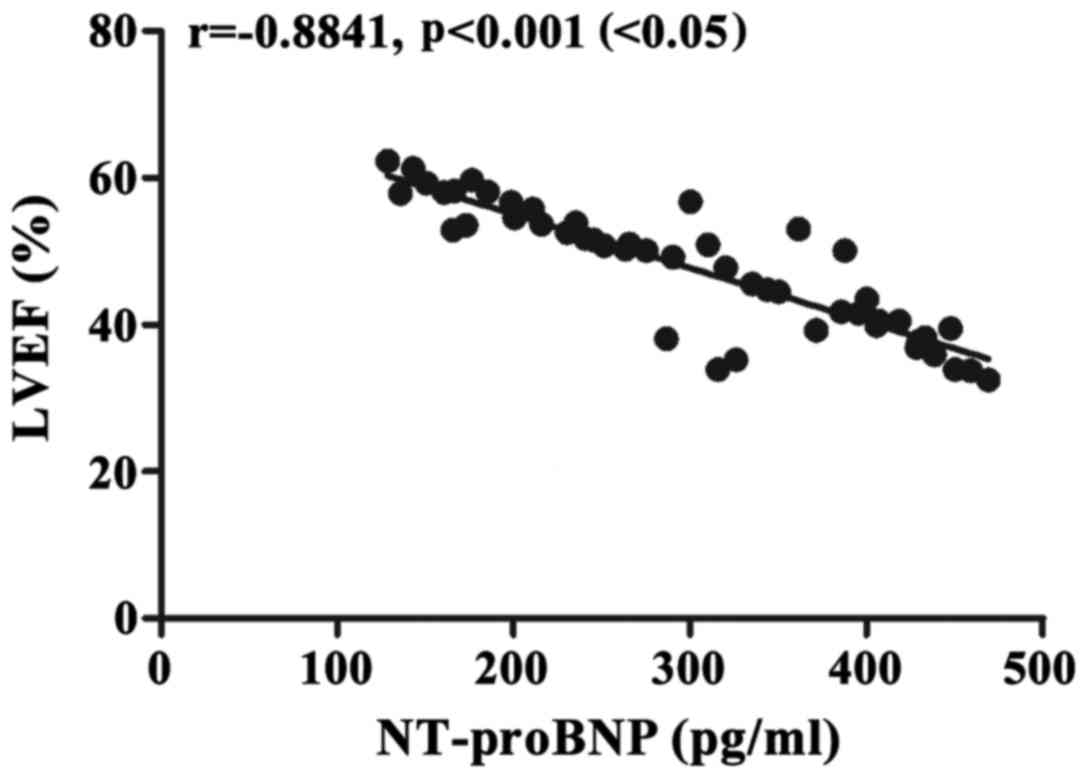
Analysis of correlation between
NT-proBNP and LVEF levels in patients with different cardiac
functions
The analysis showed that there was a negative
correlation between NT-proBNP and LVEF levels [r=−0.8517,
p<0.001 (<0.05)] (Fig. 1).
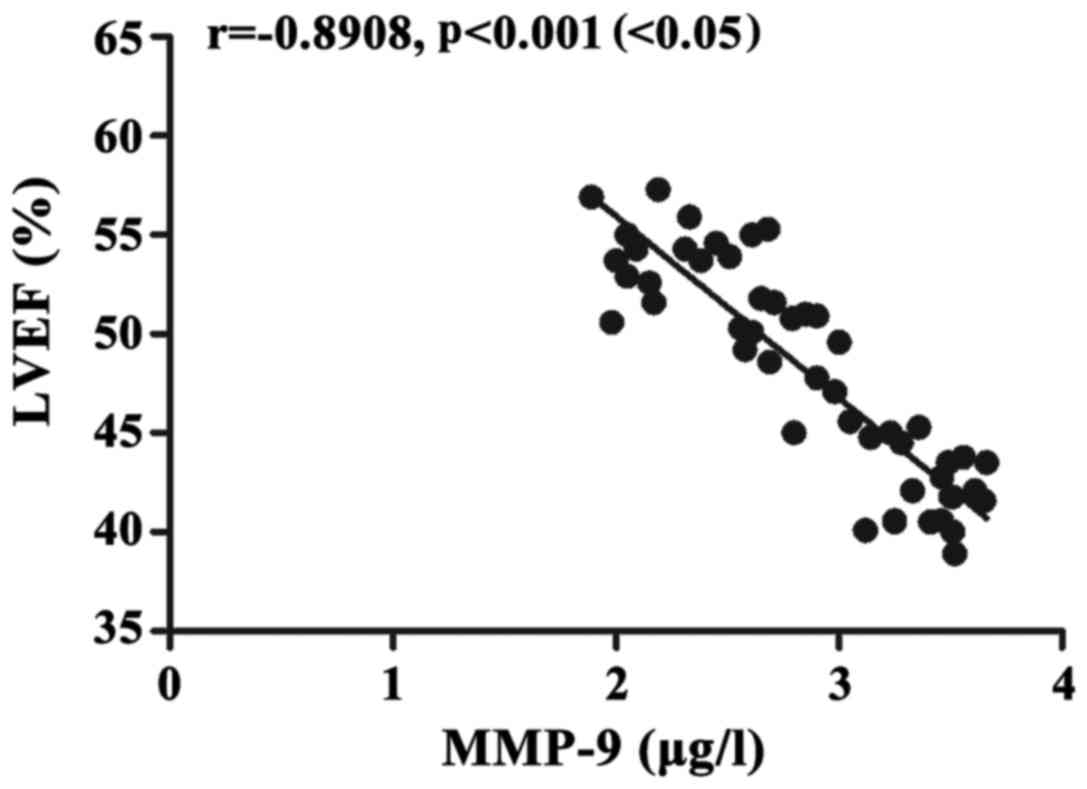
Analysis on correlation of MMP-9 level
with LVEF level in patients with different cardiac functions
The analysis revealed that MMP-9 level had a
negative relation with LVEF level [r=−0.8517, p<0.001
(<0.05)] (Fig. 2).
Univariate analysis identified
relevant factors for heart failure in patients with different
cardiac functions
Univariate analysis showed that cardiac function in
class III and above, increased NT-proBNP, upward MMP-9 and downward
LVEF were relevant risk factors of the occurrence of heart failure
in patients with different cardiac functions (Table III).
 | Table III.Univariate analysis on relevant
factors of the occurrence of heart failure in patients with
different cardiac functions. |
Table III.
Univariate analysis on relevant
factors of the occurrence of heart failure in patients with
different cardiac functions.
| Relevant factors | Case | Heart failure | t or
χ2 | P-value |
|---|
| Sex |
|
|
|
|
| Male | 45 | 25 | 0.020 | 0.887 |
|
Female | 35 | 20 |
|
|
| Age (years) |
|
|
|
|
|
>60 | 55 | 32 | 2.557 | 0.110 |
| ≤60 | 25 | 13 |
|
|
| Cardiac function |
|
|
|
|
| Cardiac
function |
|
|
|
|
| in class
II and below | 40 | 7 | 45.741 | <0.001 |
| Cardiac
function |
|
|
|
|
| in class
III and above | 40 | 38 |
|
|
| MMP-9 (µg/l) |
|
|
|
|
|
Normal | 35 | 5 | 44.525 | <0.001 |
|
Upward | 45 | 40 |
|
|
| NT-proBNP |
|
|
|
|
|
Normal | 20 | 1 | 27.280 | <0.001 |
|
Upward | 60 | 45 |
|
|
| LVEF (%) |
|
|
|
|
|
Normal | 30 | 3 | 38.769 | <0.001 |
|
Downward | 50 | 42 |
|
|
| Combined with
diabetes |
|
|
|
|
| Yes | 35 | 21 | 0.356 | 0.551 |
| No | 45 | 24 |
|
|
| Combined with
hypertension |
|
|
|
|
| Yes | 30 | 15 | 0.762 | 0.383 |
| No | 50 | 30 |
|
|
Multivariate logistic regression
analysis of the occurrence of heart failure in patients with
different cardiac functions
Multivariate logistic regression analysis showed
that cardiac function in class III and above, increased NT-proBNP,
increased MMP-9 and decreased LVEF were independent risk factors of
the occurrence of heart failure in patients with different cardiac
functions (Table IV).
 | Table IV.Multivariate logistic regression
analysis of patients with cardiac function in class III and
above. |
Table IV.
Multivariate logistic regression
analysis of patients with cardiac function in class III and
above.
| Different cardiac
functions | Wald test
value | OR | Degree of
freedom | SE | P-value |
|---|
| Cardiac function in
class III and above | 5.288 | 0.949 | 0.937 | 2.014 | 0.011 |
| Increased
NT-proBNP | 10.653 | 2.620 | 0.964 | 0.057 | 0.025 |
| Increased
MMP-9 | 6.215 | 1.363 | 0.311 | 0.153 | 0.047 |
| Decreased LVEF | 6.625 | 1.669 | −0.512 | 0.199 | 0.010 |
Discussion
Heart failure is a clinical disease with increased
pre- and post-loading volumes of the heart, stasis of blood flow,
and insufficient supply of blood and oxygen to main organs because
of the dysfunctions of systolic and diastolic capacities and
reduced pumping capability of the heart (9). In recent years, with changes in
people's lifestyle and diet structure, the occurrence and
development of cardiovascular diseases show an increasing trend,
and onset age is also becoming younger (10). In addition, there are increasing
number of inducements of heart failure, so the morbidity of heart
failure is getting higher and higher, seriously threatening the
life and health of humans (11).
Patients with early heart failure only have complaints such as
fatigue, decreased exercise tolerance and increased heart rate,
which can easily be ignored (12),
but with the prolonged course of disease and the aggravation of
disease, patients may show manifestations including dyspnea on
exertion, orthopnea, lung rale and even pink frothy sputum, which
can reduce cardiac function and increase difficulties in treatment
(13). Therefore, how to realize
rapid and effective early diagnosis of heart failure in clinical
practices and evaluate the prognosis of patients at the same time
is the focus and hotspot of current studies (14). Previous study has shown (5) that plasma NT-proBNP level, which is
positively correlated with the severity of heart failure, can be
used as a sensitive index in assessing changes of cardiac
function.
In this study, patients with different cardiac
functions were divided into a group with cardiac function of class
II and below and a group with cardiac function of class III and
above. Comparisons of serum NT-proBNP and MMP-9 levels between the
two groups revealed that the group with cardiac function in class
II and below had significantly lower serum NT-proBNP and MMP-9
levels than the group with cardiac function in class III and above,
suggesting that NT-proBNP and MMP-9 levels are relatively low in
patients with lower class of cardiac function. At the same time,
the results of the echocardiogram were compared between the two
groups, and showed that LVEDD and LVESD were obviously lower in the
group with cardiac function in class II and below than those in
group with cardiac function in class III and above. LVEF in the
group with cardiac function in class II and below was higher than
that in the group with cardiac function in class III and above,
indicating that patients with cardiac function in class II and
below have both lower LVEDD and LVESD, but higher LVEF than
patients with cardiac function in class III and above. Furthermore,
analyses on correlations of NT-proBNP and MMP-9 levels with LVEF
level in patients with different cardiac functions showed that
NT-proBNP and MMP-9 levels were negatively related to LVEF level,
which was consistent with the finding of Yan et al (6), indicating that LVEF declined with
increase in NT-proBNP and MMP-9 levels, and Vorovich et al
(7) suggested that NT-proBNP is
superior to MMP-9 in the diagnosis and prognosis of heart failure.
Moreover, analyses of factors related to the occurrence of heart
failure in patients with different cardiac functions suggested that
class III and above cardiac function, increased NT-proBNP and MMP-9
levels and decreased LVEF level were the relevant and independent
risk factors for heart failure.
NT-proBNP, mainly synthesized by cardiomyocytes, is
a biological natural hormone with the highest expression in cardiac
ventricles, and is secreted mainly in the case of passive
ventricular dilatation and volume overload (15). With the longer half-time and
expression time, and higher detection sensitivity than type-B
natriuretic peptide in patients with heart failure, NT-proBNP is
considered to be one of the specific markers of early cardiac
dysfunction, and can be used for early diagnosis of heart failure
in clinical practice (16). When
patients suffer from heart failure caused by various degrees of
decompensation, the level of NT-proBNP secreted into ventricular
cells is increased distinctly (17).
High class of cardiac function reflects poor cardiac function, and
is the cause of increased ventricular end-diastolic pressure, left
ventricular enlargement, decreased ejection fraction (18), and increased NT-proBNP level.
Although many studies on the relationship between the level of
NT-proBNP and the development of heart failure have been reported
(19), most patients were diagnosed
based on clinical manifestations or New York Heart Function scores,
and objective data were not used, especially for the LVEF evaluated
by color Doppler echocardiography. In this study, correlation
between NT-proBNP levels and LVEF was analyzed. Combined with the
New York Heart Function assessment, we found that NT-proBNP and
MMP-9 levels were elevated and LVEF levels decreased in patients
with grade III cardiac function or beyond. These patients have
high-risk of heart failure and prognosis is poor. Attention should
be paid to these patients during clinical treatment (20).
In conclusion, patients with cardiac function in
class II and below have relatively lower NT-proBNP and MMP-9
levels; NT-proBNP and MMP-9 levels are negatively correlated with
LVEF in patients with different degrees of cardiac function;
attention should be paid to patients with cardiac function in class
III and above, increased NT-proBNP and MMP-9 levels and decreased
LVEF in clinical practice, so as to actively prevent and treat
heart failure.
Acknowledgements
Not applicable.
Funding
This study was supported by the Scientific Research
Project of Wuxi Health Bureau (MS201535).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
LX and YC conceived and designed the study. YJ
collected the patient data. SY was responsible for the analysis and
interpretation of the data. LX drafted and revised the manuscript
critically for important intellectual content. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Yixing People's Hospital (Yixing, China). Signed informed consents
were obtained from the patients or the guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Isah IA, Sadoh WE and Iduoriyekemwen NJ:
Usefulness of amino terminal pro-B-type natriuretic peptide in
evaluating children with cardiac failure. Cardiovasc Diagn Ther.
7:380–388. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Raedle-Hurst T, Mueller M, Meinitzer A,
Maerz W and Dschietzig T: Homoarginine-A prognostic indicator in
adolescents and adults with complex congenital heart disease? PLoS
One. 12:e01843332017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Darkner S, Goetze JP, Chen X, Henningsen
K, Pehrson S and Svendsen JH: Natriuretic propeptides as markers of
atrial fibrillation burden and recurrence (from the AMIO-CAT
Trial). Am J Cardiol. 120:1309–1315. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jiang R, Zhao QH, Wu WH, Zhang R, Yuan P,
Gong SG, He J, Luo CJ, Qiu HL, Wang L, et al: Efficacy and safety
of a calcium sensitizer, levosimendan, in patients with right heart
failure due to pulmonary hypertension. Clin Respir J. 12:1518–1525.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yu J, Oh PC, Kim M, Moon J, Park YM, Lee
K, Suh SY, Han SH, Byun K, Ahn T, et al: Improved early risk
stratification of patients with ST-segment elevation myocardial
infarction undergoing primary percutaneous coronary intervention
using a combination of serum soluble ST2 and NT-proBNP. PLoS One.
12:e01828292017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yan AT, Yan RT, Spinale FG, Afzal R,
Gunasinghe HR, Arnold M, Demers C, McKelvie RS and Liu PP: Plasma
matrix metalloproteinase-9 level is correlated with left
ventricular volumes and ejection fraction in patients with heart
failure. J Card Fail. 12:514–519. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Vorovich EE, Chuai S, Li M, Averna J,
Marwin V, Wolfe D, Reilly MP and Cappola TP: Comparison of matrix
metalloproteinase 9 and brain natriuretic peptide as clinical
biomarkers in chronic heart failure. Am Heart J. 155:992–997. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Raphael C, Briscoe C, Davies J, Whinnett
Ian Z, Manisty C, Sutton R, Mayet J and Francis DP: Limitations of
the New York Heart Association functional classification system and
self-reported walking distances in chronic heart failure. Heart.
93:476–482. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chang KW, Fox S, Mojaver S and Maisel AS:
Using biomarkers to guide heart failure management. Expert Rev
Cardiovasc Ther. 15:729–741. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Felker GM, Anstrom KJ, Adams KF, Ezekowitz
JA, Fiuzat M, Houston-Miller N, Januzzi JL Jr, Mark DB, Piña IL,
Passmore G, et al: Effect of natriuretic peptide-guided therapy on
hospitalization or cardiovascular mortality in high-risk patients
with heart failure and reduced ejection fraction: A randomized
clinical trial. JAMA. 318:713–720. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dai Y, Yang J, Takagi A, Konishi H,
Miyazaki T, Masuda H, Shimada K, Miyauchi K and Daida H:
In-hospital and long-term outcomes of congestive heart failure:
Predictive value of B-type and amino-terminal pro-B-type
natriuretic peptides and their ratio. Exp Ther Med. 14:1715–1721.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Clerico A, Zaninotto M, Passino C and
Plebani M: New issues on measurement of B-type natriuretic
peptides. Clin Chem Lab Med. 56:32–39. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mozzini C, Di Dio Perna M, Pesce G, Garbin
U, Pasini Fratta AM, Ticinesi A, Nouvenne A, Meschi T, Casadei A,
Soresi M, et al: Lung ultrasound in internal medicine efficiently
drives the management of patients with heart failure and speeds up
the discharge time. Intern Emerg Med. 13:27–33. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kang CK, Pope M, Lang CC and Kalra PR:
Iron deficiency in heart failure: Efficacy and safety of
intravenous iron therapy. Cardiovasc Ther. 35:59–62. 2017.
View Article : Google Scholar
|
|
15
|
Shou X, Lin J, Xie C, Wang Y and Sun C:
Plasma IL-37 elevated in patients with chronic heart failure and
predicted major adverse cardiac events: A 1-year follow-up study.
Dis Markers. 2017:91340792017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Iacoviello L, Bonaccio M, Di Castelnuovo
A, Costanzo S, Rago L, De Curtis A, Assanelli D, Badilini F, Vaglio
M, Persichillo M, et al: Moli-sani study Investigators: Frontal
plane T-wave axis orientation predicts coronary events: Findings
from the Moli-sani study. Atherosclerosis. 264:51–57. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Luedde M, Winkler T, Heinsen FA, Rühlemann
MC, Spehlmann ME, Bajrovic A, Lieb W, Franke A, Ott SJ and Frey N:
Heart failure is associated with depletion of core intestinal
microbiota. ESC Heart Fail. 4:282–290. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Toma M, Mak GJ, Chen V, Hollander Z,
Shannon CP, Lam KKY, Ng RT, Tebbutt SJ, Wilson-McManus JE,
Ignaszewski A, et al: Differentiating heart failure phenotypes
using sex-specific transcriptomic and proteomic biomarker panels.
ESC Heart Fail. 4:301–311. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Darche FF, Baumgärtner C, Biener M,
Müller-Hennessen M, Vafaie M, Koch V, Stoyanov K, Rivinius R, Katus
HA and Giannitsis E: Comparative accuracy of NT-proBNP and
MR-proANP for the diagnosis of acute heart failure in dyspnoeic
patients. ESC Heart Fail. 4:232–240. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Medvedeva EA, Berezin II and Shchukin YV:
Galectin-3, markers of oxidative stress and renal dysfunction in
patients with chronic heart failure. Kardiologiia. 57:46–50.
2017.(In Russian). PubMed/NCBI
|