Introduction
Increases in blood pressure are always accompanied
with the elevated risks in cardiovascular diseases, such as
myocardial infarction, heart failure and stroke. Aging of
population in China increases the risk of hypertension and its
cardiovascular (1). In diabetes
mellitus (DM) patients, risk of cardiovascular complications,
coronary artery disease (CAD), cerebral stroke and peripheral
arterial diseases are two to four times higher than that in people
without DM (2,3). DM is always accompanied with
hypertension, and, thus, DM patients complicated with hypertension
usually suffer from an increased risk of cardiovascular
complications (4). Corresponding
studies have reported that during the follow-up period of DM
patients without cardiovascular diseases, the risk of
cardiovascular diseases is almost equivalent to non-DM patients
with history of cardiovascular diseases (5,6). Serum
cystatin C is a kind of kidney-secreted enzyme that is widely
distributed in the body, and can reflect the filtrating function of
glomerulus (7). Diabetes and
hypertension often affect kidneys. However, there is no report on
the serum levels of cystatin C in patients with diabetes mellitus
combined with hypertension. We hypothesized that serum cystatin C
may have some predictive value in detecting renal damage in
patients with hypertension or diabetes without clinical renal
impairments (proteinuria and renal insufficiency), whereas those
with diabetes mellitus combined with hypertension are more likely
to have renal damage in the early stage, and serum cystatin C
levels may be higher in these patients than in patients with only
diabetes. Substance P refers to a kind of neuropeptide widely
distributed in fine nerve fibers. When the nerve is stimulated,
substance P can be released through the central end and peripheral
end, and bind to neurokinin-1 receptor (NK1) to exert the
physiological function. Peripheral neuropathy is one of the common
complications of DM. There is usually an increase in substance P in
patients with diabetes mellitus combined peripheral neuropathy.
However, there is no report on the effect of hypertension on
substance P in patients with diabetes mellitus. In order to measure
the concentration of serum cystatin C and substance P in peripheral
blood of DM patients with hypertension, DM patients, hypertension
patients and DM patients with hypertension were selected from
December 2015 to February 2017. There were 60 patients with only DM
(control group), 60 patients with only hypertension (control group)
and 60 DM patients with hypertension (observation group). We
measured levels of serum cystatin C and substance P in peripheral
blood of all the patients.
Patients and methods
General data of patients
DM patients with or without hypertension who were
admitted to No. 215 Hospital of Shaanxi Nuclear Industry (Xianyang,
China) between December 2015 and February 2017 were enrolled in
this study. Inclusion criteria: i) Patients aged between 40 and 80
years; ii) patients met the Diagnostic Criteria of Diabetes
Mellitus (2010 edition, American Diabetes Association): i)
glycosylated hemoglobin (HbA1c) ≥6.5%; ii) fasting plasma glucose
(FPG) ≥7.0 mmol/l (patients fasted for 8 h); iii) 2 h plasma
glucose in oral glucose tolerance test ≥11.1 mmol/l; iv) random
blood sugar ≥11.1 mmol/l for patients with the typical symptoms or
crisis of high glucose; c) patients whose systolic pressure reached
or exceeded 21.3 kPa (160 mmHg) and diastolic pressure reached or
exceeded 12.7 kPa (95 mmHg). Hypertension classification was based
on the 1999 WHO/ISH guidelines for the treatment of hypertension
(8). Exclusion criteria: a) patients
with type I DM; b) patients complicated with renal insufficiency,
hematuresis or proteinuria; c) patients complicated with severe
infections; d) patients complicated with tumors. Among these
patients, we selected 60 DM patients complicated with hypertension
as observation group. Those patients included 26 males and 35
females and the age ranged from 46 to 80 years, with an average of
65.3±5.6 years. For hypertension grading, there were 16 with
hypertension of grade I, 18 of grade II and 26 of grade III. Sixty
patients with simple diabetes (28 males and 32 females, aged 48–82
years, mean age 66.2±5.2 years and simple hypertension in 60
patients (30 males and 30 females, aged 44–79 years, mean age
65.8±6.1 years as the control group in this study. There were 28
males and 32 females, and the age ranged from 48–82 years with an
average of 66.2±5.2 years. No statistical significance was found in
comparisons of age and sex among groups. This study was approved by
the Ethics Committee of Baoji Central Hospital (Baoji, China), and
all the patients or their family signed the informed consent.
Detection of serum cystatin C
Fasting venous (3 ml) blood was extracted from each
patient in the morning to detect serum cystatin C by particle
reinforcement particle-enhanced turbidimetric immunoassay (PETIA)
using Olympus AU 2700 automatic biochemical analyzer (Ningbo
Purebio Biotechnology Co., Ltd., Ningbo, China) in accordance with
the instructions of kit and apparatus.
Detection of substance P level in
peripheral blood
Enzyme-linked immunosorbent assay (ELISA) was
performed using an ELISA kit (R&D Systems, Inc., Minneapolis,
MN, USA) to detect substance P in peripheral blood of each patient
in strict accordance with the instruction of the kit. Elbow venous
blood (3 ml) was collected, followed by centrifugation at 2,500 × g
at 4°C for 15 min, and the separated plasma was stored at −70°C
before use. OD values at 492 nm were detected to calculate the
content of substance P in peripheral blood.
Statistical analysis
SPSS 22.0 (IBM Corp., Armonk, NY, USA) software was
used. All measurement data were expressed as mean ± standard
deviation, and independent sample t-test. Comparison between groups
was done using one-way ANOVA test followed by post hoc test (Least
Significant Difference). Enumeration data were expressed as No.
(case) or percentage, and Chi-square test was performed for
intergroup comparisons. Spearman's correlation analysis was adopted
for correlation analyses. P<0.05 was considered to indicate a
statistically significant difference.
Results
Comparison of the levels of serum
cystatin C and substance P in peripheral blood of patients in three
groups
There was no significant difference in serum
cystatin C and peripheral blood substance P levels between diabetes
control group and hypertension control group. Average level of
serum cystatin C was significantly higher in observation group than
in the two control groups. The level of substance P in peripheral
blood in the observation group was lower than that in the diabetic
control group (P<0.05), but there was no difference between the
observation group and the hypertension control group (P>0.05).
Average levels of serum cystatin C and substance P in peripheral
blood of observation group were 1.18±0.53 mg/l and 112.65±28.37
ng/l, respectively, and those in diabetes control group were
1.04±0.48 mg/l and 145.28±27.06 ng/l, respectively. Significant
differences were found between two groups (t=2.185, t=1.028,
P<0.05) (Table I).
 | Table I.Comparison of the levels of serum
cystatin C and substance P in peripheral blood of patients in two
groups (mean ± SD). |
Table I.
Comparison of the levels of serum
cystatin C and substance P in peripheral blood of patients in two
groups (mean ± SD).
| Groups | No. | Serum cystatin C
(mg/l) | Substance P in
peripheral blood (ng/l) |
|---|
| Observation | 60 | 1.18±0.53 | 112.65±28.37 |
| Diabetes control | 60 | 1.04±0.48 | 145.28±27.06 |
| Hypertension
control | 60 | 0.98±0.38 | 113.08±27.13 |
| at value |
| 2.185 | 1.028 |
| bt value |
| 2.062 | 0.978 |
| aP value |
| <0.05 | <0.05 |
| bP value |
| <0.05 | >0.05 |
Comparison of the levels of serum
cystatin C and substance P in peripheral blood in patients with
different grades of hypertension in observation group
There was no statistically significant difference
between the distributions of patients with grade I, II and III
hypertension in the hypertension-only control and the observation
groups (P>0.05). In observation group, level of serum cystatin C
was significantly higher, while substance P level in peripheral
blood was significantly lower in patients with grade III
hypertension than those in the patients with grade I or II
hypertension (P<0.05). Comparisons of the serum cystatin C level
and substance P level in peripheral blood between patients with
grade I and II hypertension showed no statistical significance
(P>0.05). In control group, serum levels of cystatin C in
patients with level III hypertension were significantly higher than
those in patients with level II and I, while no significant
difference was found between level II and I in serum levels of
cystatin C and levels of substance P in peripheral blood
(P>0.05). No significant differences were found between patients
in observation group and control group with the same level of
hypertension (P>0.05) (Tables II
and III).
 | Table II.Comparison of serum cystatin C levels
between patients in observation group and hypertension-only control
group with different levels of hypertension (mean ± SD). |
Table II.
Comparison of serum cystatin C levels
between patients in observation group and hypertension-only control
group with different levels of hypertension (mean ± SD).
|
| Observation |
| Hypertension-only
control |
|---|
|
|
|
|
|
|---|
| Levels | Cases | Serum cystatin C
(mg/l) | Cases | Serum cystatin C
(mg/l) | P-value |
|---|
| III | 28 | 1.24±0.34 | 26 | 1.38±0.64 | >0.05 |
| II | 17 |
1.11±0.54a | 18 |
1.17±0.51b | >0.05 |
| I | 15 |
1.01±0.44a | 16 |
1.06±0.43b | >0.05 |
| F-value |
| 8.889 |
| 9.024 |
|
| P-value |
| <0.05 |
| <0.05 |
|
 | Table III.Comparison of levels of P substance in
peripheral blood between patients in observation group and
hypertension-only control with different levels of hypertension
(mean ± SD). |
Table III.
Comparison of levels of P substance in
peripheral blood between patients in observation group and
hypertension-only control with different levels of hypertension
(mean ± SD).
|
| Observation |
| Hypertension-only
control |
|---|
|
|
|
|
|
|---|
| Levels | Cases | P substance in
peripheral blood (ng/l) | Cases | P substance in
peripheral blood (ng/l) | P-value |
|---|
| III | 28 | 102.93±26.67 | 26 | 100.43±25.67 | >0.05 |
| II | 17 |
117.28±27.95a | 18 |
112.25±26.91b | >0.05 |
| I | 15 |
125.57±29.31a | 16 |
126.57±27.31b | >0.05 |
| F value |
| 10.326 |
| 11.453 |
|
| P-value |
| <0.05 |
| <0.05 |
|
Correlation of the systolic pressure
with the levels of serum cystatin C and substance P in peripheral
blood of patients in the observation group
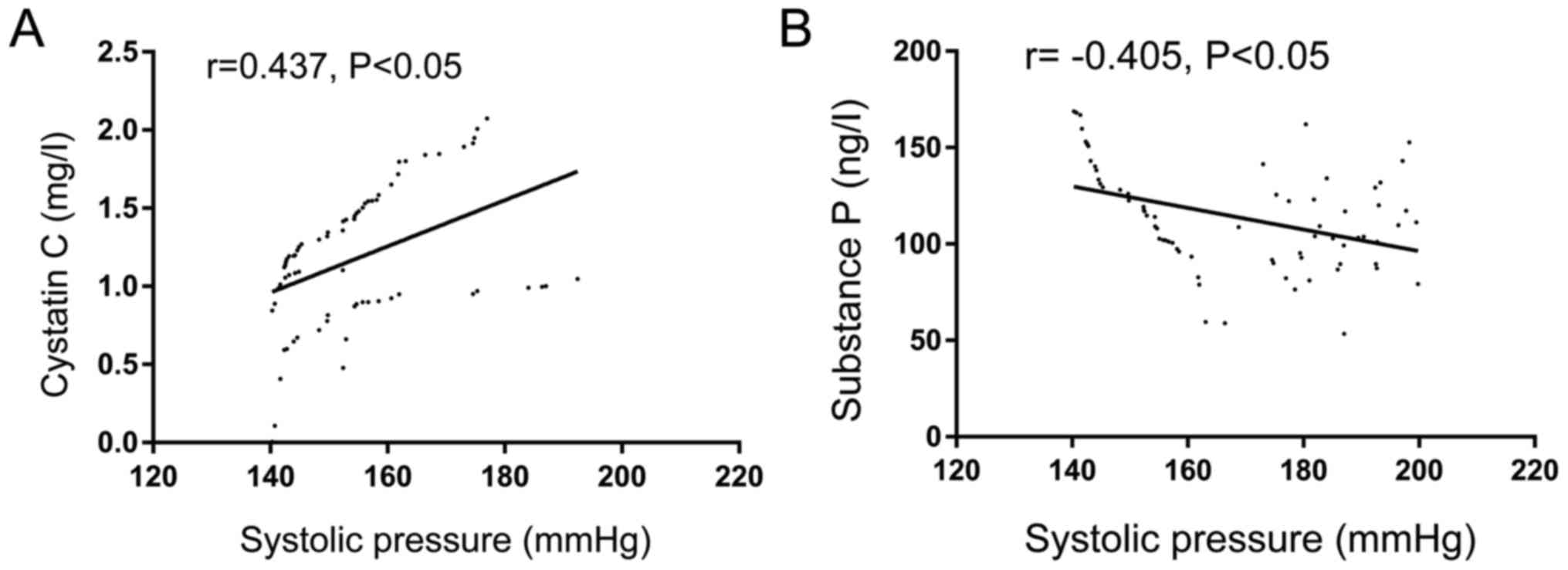
Correlation analysis showed that systolic pressure
of patients in the observation group was significantly positively
correlated with level of serum cystatin C (r=0.437, P<0.05), but
significantly negatively correlated with the level of substance P
in peripheral blood (r= −0405, P<0.05) (Fig. 1).
Discussion
Type II DM is a kind of metabolic disease with
chronic hyperglycemia, in which insufficient secretion of insulin
or insulin-resistance leads to the metabolic disturbance of
nutrients, such as glucose, fat and protein. Long-term
hyperglycemia and metabolic disturbance usually result in damage to
multiple organs, including eyes, kidney, nerve, heart and vessels
(9,10). However, in DM patients, the risk of
cardiovascular complications is equivalent to that of patients with
CAD, and, thus, similar treatment methods should be adopted to
improve the prognosis of cardiovascular diseases (11,12). DM
is usually accompanied with hypertension, which is a key risk
factor for cardiovascular complications in DM patients (13,14).
Previous studies reported that approximately 20–60% of DM patients
were also suffering hypertension, and 25–50% of hypertension
patients were combined with DM, and patients with DM and
hypertension were usually more susceptible to the cardiovascular
diseases (15,16). Rodrigues et al reported that
in DM patients complicated with hypertension, risk of
cardiovascular complications was almost twice of that in people
without DM or hypertension (17). In
this study, we compared the levels of serum cystatin C and
substance P in peripheral blood between the DM patients and DM
patients combined with hypertension for the first time, and our
results suggested the clinical significance of serum cystatin C and
substance P levels in DM and hypertension.
Serum cystatin C, also known as γ-trace protein, is
a cysteine proteinase inhibitor widely distributed in tissues and
body fluid (18). Cystatin C in
blood can only be filtrated and eradicated by glomerulus, and,
thus, can indicate the changes in glomerular filtration rate (GFR)
(19). Previous studies have shown
that serum cystatin C is conducive to the evaluation of GFR, and
can increase the detection rate of renal function damage in early
stage of DM (20–22). Patients complicated with renal
insufficiency, hematuresis or proteinuria were excluded from this
study, and we found that average level of serum cystatin C in DM
patients with hypertension was significantly higher than that in
control group, suggesting that serum cystatin C has a significant
predictive value for hypertension. Furthermore, we found that serum
level of cystatin C was higher in DM patients with grade III
hypertension than in patients with grade I or II, indicating that
serum cystatin C level is correlated with hypertension.
Silva-E-Oliveira et al (23)
found that level of serum cystatin C is correlated with the
flow-mediated vasodilation. Bhavsar et al (24) also found that serum cystatin C in
patients with pregnancy-induced hypertension syndrome was
significantly higher than that in normal control group. Compared
with the patients with only DM, level of serum cystatin C in DM
patients complicated with hypertension was significantly increased,
suggesting that those patients were more susceptible to renal
damage and refractory hypertension.
As a kind of brain-gut peptide, substance P is not
only the neurotransmitter or neuromodulator, but also a kind of key
chemokine in modulating the immune system and endocrine system
(25). Menzies et al
(26) found that complications of
DM, such as CAD, neuropathic pain or gastrointestinal dysfunction,
were correlated with content of substance P in peripheral blood.
Grover et al (27) also
reported that in type II DM patients, content of substance P level
in plasma was significantly lower than that in healthy people, and
a much lower level was found in the DM patients combined with
gastroesophageal reflux. Iwasaki et al (28) found that in DM patients, decrease in
substance P level in peripheral blood may be associated with the
onset of diabetes gastroparesis. In addition, decreased level of
substance P in peripheral blood contributes to the significant
increase in cytokines secreted by immune competent cells and
improvement in bone metabolism. In this study, compared with DM
patients, substance P level in peripheral blood in DM patients
combined with hypertension was significantly reduced, which in turn
affect the major organs of patients, including heart and lungs.
Correlation analysis also revealed that systolic pressure of DM
patients complicated with hypertension was significantly negatively
correlated with substance P level in peripheral blood (P<0.05).
Thus, compared with DM patients, substance P level in peripheral
blood was relatively lower, and blood pressure was negatively
correlated with the substance P level in peripheral blood of DM
patients complicated with hypertension.
In conclusion, we detected the levels of serum
cystatin C and substance P in peripheral blood of DM patients
complicated with hypertension, and found that content of serum
cystatin C was relatively high and level of substance P in
peripheral blood was relatively low in DM patients with
hypertension, and blood pressure was positively correlated with the
serum cystatin C level and negatively correlated with the substance
P level in peripheral blood in these patients. Our findings
provided references for further investigations on the
mechanism.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
WZ conceived and designed the study, and drafted the
manuscript. XG, CL and JL collected, analyzed and interpreted the
patient data, and revised the manuscript critically for important
intellectual content. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Baoji Central Hospital (Baoji, China). Signed informed consents
were obtained from the patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ranpise N, Jamkar P and Langote H: Do
fixed dose combinations play an important role in the management of
coexistent type two diabetes mellitus and hypertension? Ind J Pharm
Edu Res. 49:190–199. 2015.https://pdfs.semanticscholar.org/bb29/cc69f43e2026d0e6b8e1b107782de8c0b51b.pdf
View Article : Google Scholar
|
|
2
|
Hill MD: Stroke and diabetes mellitus.
Handb Clin Neurol. 126:167–174. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Janghorbani M and Amini M: Progression
from optimal blood glucose and pre-diabetes to type 2 diabetes in a
high risk population with or without hypertension in Isfahan, Iran.
Diabetes Res Clin Pract. 108:414–422. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Guo K, Zhou Z, Jiang Y, Li W and Li Y:
Meta-analysis of prospective studies on the effects of nut
consumption on hypertension and type 2 diabetes mellitus. J
Diabetes. 7:202–212. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lan J, Zhao Y, Dong F, Yan Z, Zheng W, Fan
J and Sun G: Meta-analysis of the effect and safety of berberine in
the treatment of type 2 diabetes mellitus, hyperlipemia and
hypertension. J Ethnopharmacol. 161:69–81. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Danquah I, Dobrucky CL, Frank LK, Henze A,
Amoako YA, Bedu-Addo G, Raila J, Schulze MB, Mockenhaupt FP and
Schweigert FJ: Vitamin A: Potential misclassification of vitamin A
status among patients with type 2 diabetes and hypertension in
urban Ghana. Am J Clin Nutr. 102:207–214. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chung JO, Cho DH, Chung DJ and Chung MY:
Serum cystatin C levels are positively associated with
cardiovascular autonomic neuropathy in patients with type 2
diabetes. Exp Clin Endocrinol Diabetes. 123:627–631. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kjeldsen SE, Farsang C, Sleigh P and
Mancia G: World Health Organization; International Society of
Hypertension: 1999 WHO/ISH hypertension guidelines - highlights and
ESH update. J Hypertens. 19:2285–2288. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Li N, Beck T, Chen J, Biermann C, Guo L,
Sun H, Gao F and Liu C: Assessment of thoracic aortic elasticity: A
preliminary study using electrocardiographically gated dual-source
CT. Eur Radiol. 21:1564–1572. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Edelman D, Dolor RJ, Coffman CJ, Pereira
KC, Granger BB, Lindquist JH, Neary AM, Harris AJ and Bosworth HB:
Nurse-led behavioral management of diabetes and hypertension in
community practices: A randomized trial. J Gen Intern Med.
30:626–633. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kamoi K: Usefulness of morning home blood
pressure measurements in patients with type 2 diabetes mellitus:
Results of a 10-year, prospective, longitudinal study. Clin Exp
Hypertens. 37:122–127. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hara Y, Kawagishi N, Nakanishi W, Tokodai
K, Nakanishi C, Miyagi S and Ohuchi N: Prevalence and risk factors
of obesity, hypertension, dyslipidemia and diabetes mellitus before
and after adult living donor liver transplantation. Hepatol Res.
45:764–770. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Liang S, Cai GY and Chen XM: Clinical and
pathological factors associated with progression of diabetic
nephropathy. Nephrology (Carlton). 22 Suppl 4:14–19. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mozafari M, Nekooeian AA, Mashghoolozekr E
and Panjeshahin MR: The cardioprotective effects of resveratrol in
rats with simultaneous type 2 diabetes and renal hypertension. Nat
Prod Commun. 10:335–338. 2015.PubMed/NCBI
|
|
15
|
Zhou J, Liu C, Shan P, Zhou Y, Xu E and Ji
Y: Prevalence and distinguishing features of masked hypertension in
type 2 diabetic patients. J Diabetes Complications. 27:82–86. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ito WD, Lund N, Sager H, Becker W and
Wenzel U: Differential impact of diabetes mellitus type II and
arterial hypertension on collateral artery growth and concomitant
macrophage accumulation. Vasa. 44:31–41. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rodrigues KF, Pietrani NT, Bosco AA,
Campos FMF, Sandrim VC and Gomes KB: IL-6, TNF-α, and IL-10
levels/polymorphisms and their association with type 2 diabetes
mellitus and obesity in Brazilian individuals. Arch Endocrinol
Metab. 61:438–446. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Matsushita K, Sang Y, Ballew SH, Astor BC,
Hoogeveen RC, Solomon SD, Ballantyne CM, Woodward M and Coresh J:
Cardiac and kidney markers for cardiovascular prediction in
individuals with chronic kidney disease: The Atherosclerosis Risk
in Communities study. Arterioscler Thromb Vasc Biol. 34:1770–1777.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yan PJ, Xu Y, Wan Q, Feng J, Li H, Gao CL,
Yang J, Zhong HH and Zhang ZH: Decreased plasma neuregulin 4
concentration is associated with increased high-sensitivity
C-reactive protein in newly diagnosed type 2 diabetes mellitus
patients: A cross-sectional study. Acta Diabetol. 54:1091–1099.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Chuengsamarn S, Rattanamongkolgul S,
Sittithumcharee G and Jirawatnotai S: Association of serum
high-sensitivity C-reactive protein with metabolic control and
diabetic chronic vascular complications in patients with type 2
diabetes. Diabetes Metab Syndr. 11:103–108. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Li X, Wu TT, Chen J and Qiu W: Elevated
expression levels of serum insulin-like growth factor-1, tumor
necrosis factor-α and vascular endothelial growth factor 165 might
exacerbate type 2 diabetic nephropathy. J Diabetes Investig.
8:108–114. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Murai T, Takebe N, Nagasawa K, Todate Y,
Nakagawa R, Nakano R, Hangai M, Hasegawa Y, Takahashi Y, Yoshioka
K, et al: Association of epicardial adipose tissue with serum level
of cystatin C in type 2 diabetes. PLoS One. 12:e01847232017.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Silva-E-Oliveira J, Amélio PM, Abranches
ILL, Damasceno DD and Furtado F: Heart rate variability based on
risk stratification for type 2 diabetes mellitus. Einstein (Sao
Paulo). 15:141–147. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bhavsar NA, Appel LJ, Kusek JW, Contreras
G, Bakris G, Coresh J and Astor BC: AASK Study Group: Comparison of
measured GFR, serum creatinine, cystatin C, and beta-trace protein
to predict ESRD in African Americans with hypertensive CKD. Am J
Kidney Dis. 58:886–893. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sun W, Tadmori I, Yang L, Delgado M and
Ganea D: Vasoactive intestinal peptide (VIP) inhibits TGF-beta1
production in murine macrophages. J Neuroimmunol. 107:88–99. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Menzies JR, McKee R and Corbett AD:
Differential alterations in tachykinin NK2 receptors in isolated
colonic circular smooth muscle in inflammatory bowel disease and
idiopathic chronic constipation. Regul Pept. 99:151–156. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Grover M, Farrugia G, Lurken MS, Bernard
CE, Faussone-Pellegrini MS, Smyrk TC, Parkman HP, Abell TL, Snape
WJ, Hasler WL, et al: NIDDK Gastroparesis Clinical Research
Consortium: Cellular changes in diabetic and idiopathic
gastroparesis. Gastroenterology. 140(1575–85): e82011.
|
|
28
|
Iwasaki H, Kajimura M, Osawa S, Kanaoka S,
Furuta T, Ikuma M and Hishida A: A deficiency of gastric
interstitial cells of Cajal accompanied by decreased expression of
neuronal nitric oxide synthase and substance P in patients with
type 2 diabetes mellitus. J Gastroenterol. 41:1076–1087. 2006.
View Article : Google Scholar : PubMed/NCBI
|