Introduction
Hypertensive disease developed in pregnancy is
called pregnancy-induced hypertension (PIH), including chronic
hypertension, pre-eclampsia, eclampsia, hypertension in pregnancy
and pre-eclampsia complicated by chronic hypertension, which is a
disease occurring in the specific period of pregnancy (1). Hypertensive disease during pregnancy
brings great harm to the health of parturients and infants, which
is an important cause of neonatal and maternal deaths (2). It is common worldwide that hypertensive
disease occurs in the pregnancy period with an incidence rate of
10%. The incidence rate in other countries is slightly higher than
that in China, which may be related to the dietary differences
between them (3). There are four
causes of PIH. First, it is believed that the occurrence of
hypertension in pregnancy is associated with oxidative stress,
which can lead to the production of inflammatory factors so as to
cause hypertension. Second, it is considered that PIH is related to
heredity, and people with genetic predisposition are susceptible to
the disease. Third, it is held that this disease is associated with
adverse immune response. Immunologic abnormality can lead to
hypertension in pregnancy, and it is considered that the occurrence
of hypertension in pregnancy is related to placental ischemia. It
has been confirmed by many scholars that the immunological theory
is involved in the development of PIH (4–7).
Endothelial injury and cytokines are involved in the process of
immune activation. In recent years, increased number of studies on
cytokines have been carried out (8–10).
Interleukin-6 (IL-6) is a 26 kDa cytokine with complex
physiological functions. It is produced by activated macrophages,
monocytes and T lymphocytes (T cells) (11). The role of IL-6 is to induce the
differentiation and growth of cells and factors in different types,
levels and organs (12–15). Some scholars have found that the IL-6
level in patients with PIH is higher than that in patients with
normal pregnancy. Maternal and infant prognoses in patients with
high level of IL-6 are worse than those in the pregnant women with
normal IL-6 level, indicating that IL-6 exerts effects on the
prognosis of patients with PIH (16). Activated natural killer (NK) cells, T
cells and macrophages can secrete a large number of tumor necrosis
factors (TNFs) (17). TNF-α has
multiple functions, as it not only has an anti-infection effect,
but also can promote proliferation and differentiation of cells.
Moreover, it has side effects damaging endothelial cells or causing
vascular dysfunction. Since PIH is closely associated with vascular
endothelium injury, it is believed that TNF-α is related to PIH.
C-reactive protein (CRP) is a protein produced under stress of the
body, which can help the body combat against external invasion and
clean up the ‘garbage’ generated inside the body so as to provide
protective effects (18). Therefore,
CRP plays an important role in the organism when it receives
external invasion, namely the effect of anti-inflammation. It has
been recognized by scholars for many years that CRP is a
non-specific inflammatory marker. However, recent studies have
found a certain correlation between CRP and atherosclerosis. In
addition, studies have shown that CRP is one of the strongest
predictors and risk factors of cardiovascular disease. Thus it is
inferred that CRP is associated with PIH. In this study, the
expression of TNF-α, IL-6 and high-sensitivity C-reactive protein
(hs-CRP) in patients with PIH were examined to investigate the
relationship between the poor pregnancy outcomes, such as
stillbirth, and PIH.
Patients and methods
General data
The expression levels of TNF-α, IL-6 and hs-CRP in
100 patients with PIH treated in Jining First People's Hospital
(Jining, China) from January 2012 to October 2017 as well as the
correlation between the expression levels of these factors in
patients with PIH and fetal adverse outcomes were studied and
analyzed. One hundred normal pregnant women at the same period were
selected as the control group. The average age of these 200
pregnant women was 27.1±3.0 years and the average gestational age
was 39.3±1.9 weeks. This study was approved by the Ethics Committee
of Jining First People's Hospital. Signed informed consents were
obtained from all participants before the study.
Standard collection
Elbow venous blood (5 ml) of patients were taken and
left to stand. Then, supernatants were removed. IL-6 and TNF-α in
serum were detected through enzyme-linked immunosorbent assay
(ELISA) and hs-CRP level was determined through immunological
transmission turbidimetry.
Judgement of adverse pregnancy
outcomes
The adverse pregnancy outcomes include preterm
birth, stillbirth, fetal death, neonatal asphyxia and death.
Statistical analysis
Whether there was a correlation between the two
variables was analyzed. The odds ratio (OR) and the 95% confidence
interval were used to select variables related to each other in the
univariate logistic regression analysis. The data analysis was
conducted through Statistical Product and Service Solutions (SPSS)
19.0 software (IBM SPSS, Armonk, NY, USA). The data calculated in
this study were expressed by the mean ± standard deviation.
P<0.05 were considered to indicate statistically significant
differences.
Results
Comparisons of the inflammatory
factors IL-6, TNF-α and hs-CRP between normal pregnancy and
PIH
One hundred normal pregnant women and
100 patients with PIH were compared
The levels of IL-6, TNF-α and hs-CRP in patients
with PIH were much higher than those in normal pregnant women. The
differences were statistically significant (p<0.01) (Table I).
 | Table I.Comparison of the inflammatory factors
IL-6, TNF-α and hs-CRP between normal pregnancy and PIH. |
Table I.
Comparison of the inflammatory factors
IL-6, TNF-α and hs-CRP between normal pregnancy and PIH.
| Factors | Normal pregnancy
(n=100) | PIH (n=100) |
|---|
| Inflammatory factor
IL-6 (pg/ml) | 1.79±0.37 | 3.42±0.45a |
| Inflammatory factor
TNF-α (µg/ml) | 1.13±0.41 | 4.98±1.25a |
| Inflammatory factor
hs-CRP (mg/ml) | 1.33±0.89 | 5.12±1.88a |
Relationships between the grade of
hypertension in patients with PIH and the inflammatory factors
IL-6, TNF-α and hs-CRP
The inflammatory factors IL-6, TNF-α and hs-CRP at
grades I–III hypertension were compared in each two groups and the
differences were significant (Table
II).
 | Table II.The relationships between the grade of
hypertension in patients with PIH and the inflammatory factors
IL-6, TNF-α and hs-CRP. |
Table II.
The relationships between the grade of
hypertension in patients with PIH and the inflammatory factors
IL-6, TNF-α and hs-CRP.
| Factors | Grade I
hypertension | Grade II
hypertension | Grade III
hypertension |
|---|
| Inflammatory factor
IL-6 (pg/ml) | 1.98±0.39 | 2.30±0.41b | 4.73±0.50a |
| Inflammatory factor
TNF-α (µg/ml) | 1.77±0.75 | 2.96±1.34b | 5.16±1.87a |
| Inflammatory factor
hs-CRP (mg/ml) | 1.92±0.77 | 3.18±1.32b | 6.76±1.97a |
Correlation between the pregnancy
outcome of patients with PIH and inflammatory factors IL-6, TNF-α
and hs-CRP
According to the aforementioned diagnostic criteria,
the adverse pregnancy outcomes include preterm birth, stillbirth,
intrauterine fetal death, neonatal asphyxia and death. Based on
this standard, the levels of inflammatory factors TNF-α and hs-CRP
in patients with good pregnancy outcomes were significantly lower
than those in patients with adverse pregnancy outcomes (p<0.01).
The level of inflammatory factor IL-6 in patients with good
pregnancy outcomes was also lower than that in patients with
adverse pregnancy outcomes (p<0.05) (Table III).
 | Table III.Correlation between pregnancy outcome
of patients with PIH and inflammatory factors IL-6, TNF-α and
hs-CRP. |
Table III.
Correlation between pregnancy outcome
of patients with PIH and inflammatory factors IL-6, TNF-α and
hs-CRP.
|
| PIH (n=100) |
|---|
|
|
|
|---|
| Factors | Good pregnancy
outcomes (54) | Adverse pregnancy
outcomes (46) |
|---|
| Inflammatory factor
IL-6 (pg/ml) | 2.13±0.56 | 3.72±0.87b |
| Inflammatory factor
TNF-α (µg/ml) | 2.15±0.77 | 4.99±1.56a |
| Inflammatory factor
hs-CRP (mg/ml) | 3.11±0.68 | 5.42±1.12a |
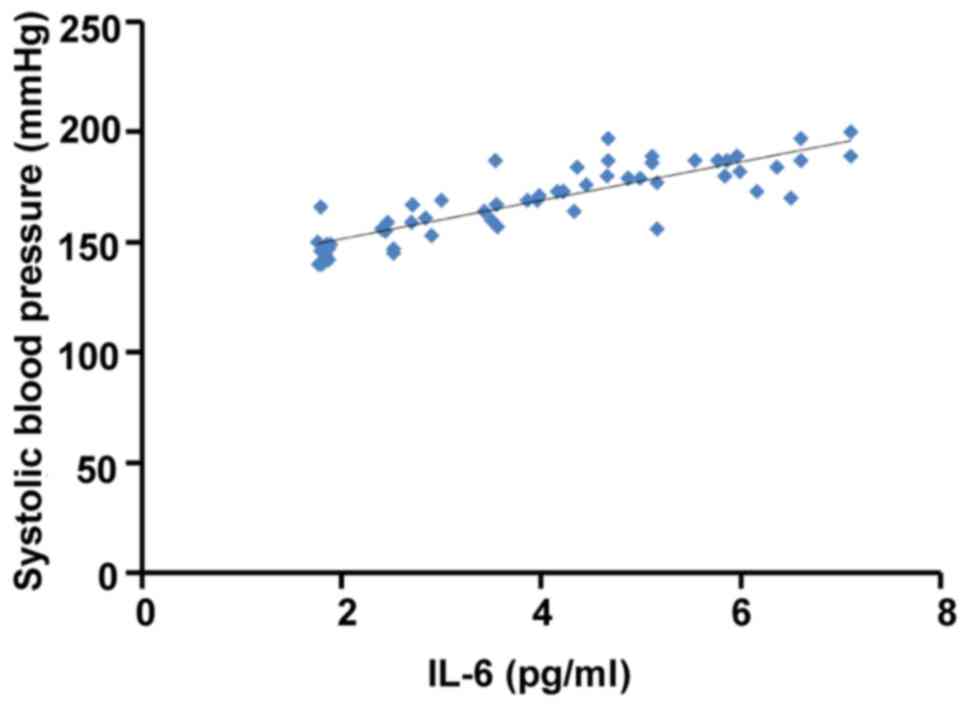
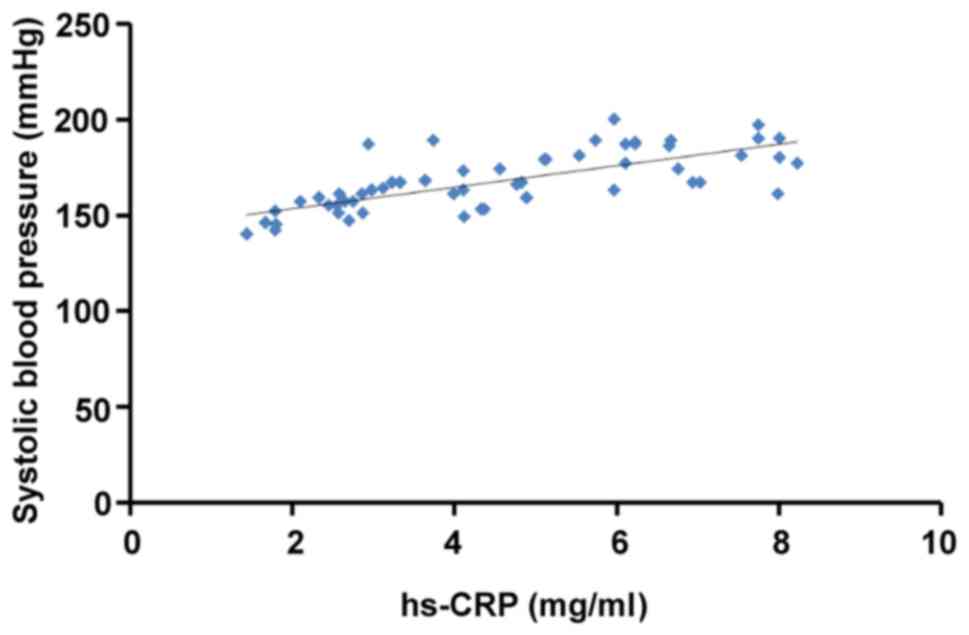
Correlation between the expression of
IL-6, TNF-α and hs-CRP and the levels of systolic blood pressure in
patients
The expression of IL-6, TNF-α and hs-CRP in patients
was linearly positively correlated with systolic blood pressure of
patients with PIH (r=0.646, r=0.711, r=0.692) (Figs. 1–3).
Logistic regression analysis for risk
factors of the adverse pregnancy outcomes in patients with PIH
Analysis of univariate logistic correlation found
that there were no correlations of age, height and weight with the
adverse pregnancy outcomes of patients with PIH (p>0.05).
Inflammatory factors TNF-α, CRP, IL-6 and blood pressure levels
were correlated to the adverse pregnancy outcomes of patients with
PIIH (p<0.05) and they were positively correlated with the
adverse pregnancy outcomes (OR value >1) (Table IV).
 | Table IV.Logistic regression analysis for risk
factors of the adverse pregnancy outcomes in patients with PIH. |
Table IV.
Logistic regression analysis for risk
factors of the adverse pregnancy outcomes in patients with PIH.
| Risk factors | P-value | OR value | 95% CI |
|---|
| Age (years) | 0.134 | 1.074 | 0.887, 1.256 |
| Height | 0.647 | 0.712 | 0.109, 6.226 |
| Weight | 0.616 | 5.954 | 1.217, 23.156 |
| TNF-α | 0.019 | 1.301 | 0.923, 1.509 |
| CRP | 0.035 | 1.521 | 0.689, 2.562 |
| IL-6 | 0.041 | 2.452 | 1.734, 3.058 |
| Blood pressure | 0.005 | 4.347 | 1.718, 15.152 |
Discussion
PIH is an important complication during the
perinatal period, which is a very important cause of maternal and
fetal death or neonatal death (19).
For normal pregnancy, the placental trophoblasts will break through
the spiral artery of the placental bed and then conduct the
retrograde infiltration along the vessel wall to destroy elastic
fibers of vessel wall until they reach the myometrium of spiral
artery. This change reduces the resistance of maternal blood
flowing to fetal blood which makes it easier for the fetus to
obtain blood and the nutrients dissolved in blood from the mother.
However, when PIH occurs, the physiological changes of spiral
artery cannot reach the myometrium, which will result in the
fibrinoid necrosis of the muscular layer and acute atherosclerosis.
This result will reduce the blood flow to the placenta, thereby
affecting the amount of blood received by the fetus, and then
further affecting the growth of the fetus. Neonatal asphyxia and
premature delivery are the frequent consequences of these causes,
and in severe cases stillbirth will be caused (20).
In recent years, it has been generally believed that
PIH is associated with immune imbalance, and cytokines, especially
inflammatory factors, play important roles in immune regulation.
Therefore, in this study, the relationship between three common
cytokines and the adverse pregnancy outcomes of patients with PIH
was investigated in order to find new methods for the diagnosis and
treatment of PIH in patients. In this study, the levels of IL-6,
TNF-α and hs-CRP in patients with PIH were significantly higher
than those in the normal pregnant women (p<0.01);. The
inflammatory factors IL-6, TNF-α and hs-CRP at grades I–III
hypertension were compared in each two groups and the differences
were significant. The expression of IL-6 in PIH patients with good
pregnancy outcomes was significantly lower than that in patients
with poor pregnancy outcomes (p<0.05). Therefore, the expression
of these inflammatory factors in patients with PIH were related to
the pregnancy outcomes, and they were linearly positively
correlated with the systolic blood pressure level in patients with
PIH. Age, height and weight were not related to the adverse
pregnancy outcomes of patients with PIH (p>0.05), while the
inflammatory factors TNF-α, CRP, the level of blood pressure and
IL-6 were correlated with the adverse pregnancy outcomes of
patients with PIH (p<0.05). In addition, they were positively
associated with adverse pregnancy outcomes (OR value >1).
Therefore, it is concluded that the expression of IL-6, TNF-α and
hs-CRP in patients with PIH can be used to predict the occurrence
of the adverse pregnancy outcomes in this period.
In conclusion, IL-6, TNF-α and hs-CRP in patients
with PIH are positively correlated with the systolic blood pressure
level and the adverse outcomes of neonatal asphyxia and stillbirth,
can be used as indicators of prognosis evaluation for patients with
PIH. In subsequent studies, it will be further analyzed whether the
reduction of the inflammatory factors IL-6, TNF-α and hs-CRP by a
series of drug interventions can improve the pregnancy outcomes in
patients with PIH, hence finding the new treatment options for
PIH.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors contributions
DK and HW designed the study. YL and HL collected
the patient data. HW and PZ analyzed the patient data. All authors
have read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Jining First People's Hospital (Jining, China). Signed informed
consents were obtained from all participants before the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ames M, Rueda J and Caughey AB: Ambulatory
management of chronic hypertension in pregnancy. Clin Obstet
Gynecol. 55:744–755. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mustafa R, Ahmed S, Gupta A and Venuto RC:
A comprehensive review of hypertension in pregnancy. J Pregnancy.
2012:1059182012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wilson KL, Casey BM, McIntire DD,
Halvorson LM and Cunningham FG: Subclinical thyroid disease and the
incidence of hypertension in pregnancy. Obstet Gynecol.
119:315–320. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Vest AR and Cho LS: Hypertension in
pregnancy. Curr Atheroscler Rep. 16:3952014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mangos GJ, Spaan JJ, Pirabhahar S and
Brown MA: Markers of cardiovascular disease risk after hypertension
in pregnancy. J Hypertens. 30:351–358. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rosengarten D, Blieden LC and Kramer MR:
Pregnancy outcomes in pulmonary arterial hypertension in the modern
management era. Eur Respir J. 40:1304–1305. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lazzarin N, Desideri G, Ferri C, Valensise
H, Gagliardi G, Tiralongo GM and Manfellotto D: Hypertension in
pregnancy and endothelial activation: An emerging risk factor for
cardiovascular disease. Pregnancy Hypertens. 2:393–397. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Shi Y, Pan H, Zhang HZ, Zhao XY, Jin J and
Wang HY: Lipoxin A4 mitigates experimental autoimmune myocarditis
by regulating inflammatory response, NF-κB and PI3K/Akt signaling
pathway in mice. Eur Rev Med Pharmacol Sci. 21:1850–1859.
2017.PubMed/NCBI
|
|
9
|
Al Khaja KA, Sequeira RP, Alkhaja AK and
Damanhori AH: Drug treatment of hypertension in pregnancy: A
critical review of adult guideline recommendations. J Hypertens.
32:454–463. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Perni U, Sison C, Sharma V, Helseth G,
Hawfield A, Suthanthiran M and August P: Angiogenic factors in
superimposed preeclampsia: A longitudinal study of women with
chronic hypertension during pregnancy. Hypertension. 59:740–746.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Graham BB, Chabon J, Kumar R, Kolosionek
E, Gebreab L, Debella E, Edwards M, Diener K, Shade T, Bifeng G, et
al: Protective role of IL-6 in vascular remodeling in
Schistosoma pulmonary hypertension. Am J Respir Cell Mol
Biol. 49:951–959. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Teixeira AA, Quinto BM, Dalboni MA,
Rodrigues CJ and Batista MC: Association of IL-6 polymorphism
−174G/C and metabolic syndrome in hypertensive patients. BioMed Res
Int. 2015:9275892015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Karaman E, Kucuk Urhan M, Bayramoglu A,
Uzun Göçmen S, Ercan S, Guler HI, Kucukkaya Y and Erden S:
Investigation of relationship between IL-6 gene variants and
hypertension in Turkish population. Cytotechnology. 67:947–954.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lukic L, Lalic NM, Rajkovic N, Jotic A,
Lalic K, Milicic T, Seferovic JP, Macesic M and Gajovic JS:
Hypertension in obese type 2 diabetes patients is associated with
increases in insulin resistance and IL-6 cytokine levels: Potential
targets for an efficient preventive intervention. Int J Environ Res
Public Health. 11:3586–3598. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dimas G, Iliadis F, Tegos T, Spiroglou S,
Kanellos I, Karamouzis I, Savopoulos C, Hatzitolios A and Grekas D:
4B.08: Serum levels of TIMP-1 and IL-6 are associated with
hypertension and atherosclerosis in patients with early stages of
chronic kidney disease and type 2 diabetic nephropathy. J
Hypertens. 33 Suppl 1:e552015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Repke JT: Hypertension in pregnancy. I. Md
Med J. 36:473–475. 1987.PubMed/NCBI
|
|
17
|
Murdaca G, Spanò F, Contatore M, Guastalla
A, Penza E, Magnani O and Puppo F: Infection risk associated with
anti-TNF-α agents: A review. Expert Opin Drug Saf. 14:571–582.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ridker PM: From C-reactive protein to
interleukin-6 to interleukin-1: Moving upstream to identify novel
targets for atheroprotection. Circ Res. 118:145–156. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Firoz T, Magee LA, MacDonell K, Payne BA,
Gordon R, Vidler M and von Dadelszen P: Community Level
Interventions for Pre-eclampsia (CLIP) Working Group: Oral
antihypertensive therapy for severe hypertension in pregnancy and
postpartum: A systematic review. BJOG. 121:1210–1220. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Easterling TR: Pharmacological management
of hypertension in pregnancy. Semin Perinatol. 38:487–495. 2014.
View Article : Google Scholar : PubMed/NCBI
|