Introduction
Severe pneumonia is a common kind of
community-acquired infection in the respiratory department, with
serious conditions, rapid development and long course; it can
easily induce respiratory failure and affect many other organs,
seriously influencing the patient's quality of life (1,2). The
death rate of patients with severe pneumonia is relatively high,
and it is the highest among the infectious diseases, being at
approximately 20–50%; the respiratory functions of patients with
severe pneumonia have been greatly affected due to
high-permeability edema, hyperemia and inflammatory exudation of
lung tissues, as well as increased respiratory secretions (3,4).
Mechanical ventilation is a very important auxiliary means to treat
patients with severe pneumonia; it can effectively ameliorate the
pulmonary ventilation and gas exchange functions of the patients,
but it can seriously affect the sputum expectoration of the
patients and cause dyspnea because its inevitable side-effects may
also further lead to reduced functions of the respiratory tract in
the patients (5,6). Therefore, effective and safe
therapeutic modes are extremely important for symptom improvement
and prognosis of the patients during mechanical ventilation.
The principles of pulmonary rehabilitation therapy
have not been completely elaborated yet; the main functions of the
therapy are to enhance the patients' exercise capacity, improve the
respiratory function reserve and ameliorate the patients'
cardiopulmonary functions. Its advantages are that it can alleviate
the patients' symptoms, relieve and even reverse the progression of
disease and lower the cost of treatment in an effective manner
(7).
In the present study, the effects of comprehensive
pulmonary rehabilitation therapy on the pulmonary functions and
blood gas indexes of 60 patients with severe pneumonia during
mechanical ventilation were observed, so as to investigate the role
of conventional therapy for severe pneumonia assisted by
comprehensive pulmonary rehabilitation therapy. The results are
shown below.
Materials and methods
Clinical data
A total of 120 patients diagnosed with severe
pneumonia in Jining No. 1 People's Hospital (Jining, China) from
May 2013 to May 2015 were selected; the diagnostic criteria were
based on the Guidelines for Diagnosis and Treatment of
Community-Acquired Pneumonia in Chinese Adults (2016 Version). All
the patients were divided into the experimental group (n=60) and
the control group (n=60) through a random number table.
Conventional therapy for severe pneumonia was applied to patients
in both groups, and the experimental group was additionally treated
with comprehensive pulmonary rehabilitation therapy. Patients with
the following conditions were excluded: unstable coronary heart
disease; intermittent myocardial infarction; severe pulmonary
arterial hypertension; serious osteoarthrosis or fracture; mental
disorders or learning disability. This research was approved by the
Ethics Committee of the Jining No. 1 People's Hospital, and
informed consent was signed by the patients or their families.
Therapeutic methods
For the conventional therapy, conventional
anti-infection therapy was adopted. In regards to the pulmonary
rehabilitation therapy, warming-up exercise before training,
respiratory function exercise, respiratory muscle training, health
education, psychological support and nutritional intervention were
performed for the patients by the physicians and the nurses.
Observation indexes
The pulmonary function indexes, blood gas indexes,
Borg index and 6-min walk distance (6MWD) of the two groups of
patients with severe pneumonia were observed before treatment and
at 6 months after treatment, and intra-group and inter-group
comparisons were conducted.
Statistical analysis
Statistical Product and Service Solutions (SPSS)
19.0 software (IBM Corp., Armonk, NY, USA) was used for the
statistical analysis. Comparison between groups was done using
One-way ANOVA test followed by post hoc test (Least Significant
Difference). The measurement data were presented as mean ± SD, and
non-parametric Kolmogorov-Smirnov (K-S) test was performed for the
comparisons between the two groups. P<0.05 indicated a
statistically significant difference.
Results
Basic data
Among the 120 patients with severe pneumonia, there
were 73 males and 47 females, with an average age of 54.5±11.6
years old. The patients were randomly divided into the control
group (n=60) and the experimental group (n=60); in the control
group, there were 32 male patients and 28 female patients, with an
average age of 52.3±9.6 years old; the experimental group consisted
of 41 male patients and 19 female patients, with an average age of
56.7±13.6 years old. There were no remarkable differences in the
basic data, such as sex, weight and age, between the control group
and the experimental group (P>0.05) (Table I).
 | Table I.Comparisons of basic data between the
two groups. |
Table I.
Comparisons of basic data between the
two groups.
|
| Control group
(n=60) | Experimental group
(n=60) | P-value |
|---|
| Age (years) | 52.3±9.6 | 56.7±13.6 | 0.871 |
| Sex, n (%) |
| Male/female | 32 (53.33)/28
(46.67) | 41 (68.33)/19
(31.67) | 0.329 |
| Body temperature | 37.91±0.42 | 37.81±0.53 | 0.891 |
| Weight (kg), n
(%) |
|
| 0.759 |
| <50 | 21 (35.00) | 25 (41.67) |
|
| ≥50 | 39 (65.00) | 35 (58.33) |
|
| Nation, n (%) |
|
| 0.672 |
| Han | 53 (88.33) | 56 (93.33) |
|
| Minority | 7 (11.67) | 4 (6.67) |
|
| Place of residence, n
(%) |
|
| 0.456 |
| City | 40 (66.67) | 46 (76.67) |
|
| Countryside | 20 (33.33) | 14 (23.33) |
|
| C-reactive
protein | 31.64±2.56 | 30.82±2.31 | 0.853 |
| White blood cell
count | 13.21±1.71 | 12.59±1.99 | 0.882 |
Changes in pulmonary function indexes
before treatment and at 6 months after treatment
Before treatment, there were no differences in the
pulmonary function parameters between the two groups (P>0.05);
at 6 months after treatment, as for the comparisons within the
control group, there were differences only in vital capacity (VC)
(1.63±0.21 vs. 2.21±0.32, P=0.021), forced expiratory volume in 1
sec (FEV1) (1.14±0.18 vs. 1.57±0.19, P=0.036) and ratio of FEV1 to
forced vital capacity (FEV1/FVC) (41.22±5.38 vs. 71.15±6.44,
P=0.025), and there were no differences in maximum mid-expiratory
flow (MMEF) (1.15±0.23 vs. 1.32±0.26, P=0.095) and peak expiratory
flow (PEF) (4.11±0.52 vs. 4.54±0.42, P=0.574). For the comparisons
within the experimental group, the VC (1.71±0.31 vs. 2.58±0.72,
P=0.025), FEV1 (1.22±0.24 vs. 2.11±0.32, P=0.036), FEV1/FVC
(39.59±5.01 vs. 82.09±7.13, P=0.014), MMEF (1.14±0.19 vs.
1.81±0.31, P=0.046) and PEF (4.04±0.44 vs. 5.25±0.56, P=0.039) were
different. In terms of inter-group comparison, there were
differences in VC (2.21±0.32 vs. 2.58±0.72, P=0.042), FEV1
(1.57±0.19 vs. 2.11±0.32, P=0.035), FEV1/FVC (71.15±6.44 vs.
82.09±7.13, P=0.036), MMEF (1.32±0.26 vs. 1.81±0.31, P=0.042) and
PEF (4.54±0.42 vs. 5.25±0.56, P=0.039) between the control group
and the experimental group. Conventional therapy assisted by
comprehensive pulmonary rehabilitation therapy has better
improvement effects on the pulmonary functions of patients with
severe pneumonia during mechanical ventilation (Table II).
 | Table II.Changes in pulmonary function
parameters of the two groups of patients before treatment and at 6
months after treatment. |
Table II.
Changes in pulmonary function
parameters of the two groups of patients before treatment and at 6
months after treatment.
|
| Control group
(n=60) | Experimental group
(n=60) | P-value |
|---|
| VC (L) |
| Before
treatment | 1.63±0.21 | 1.71±0.31 | 0.853 |
| After
treatment | 2.21±0.32 | 2.58±0.72 | 0.042 |
| FEV1 (L) |
| Before
treatment | 1.14±0.18 | 1.22±0.24 | 0.862 |
| After
treatment | 1.57±0.19 | 2.11±0.32 | 0.035 |
| FEV1/FVC (%) |
| Before
treatment | 41.22±5.38 | 39.59±5.01 | 0.725 |
| After
treatment | 71.15±6.44 | 82.09±7.13 | 0.036 |
| MMEF (L/sec) |
| Before
treatment | 1.15±0.23 | 1.14±0.19 | 0.987 |
| After
treatment | 1.32±0.26 | 1.81±0.31 | 0.042 |
| PEF (L/sec) |
| Before
treatment | 4.11±0.52 | 4.04±0.44 | 0.902 |
| After
treatment | 4.54±0.42 | 5.25±0.56 | 0.039 |
Changes in blood gas indexes before
treatment and at 6 months after treatment
There were no differences in the blood gas indexes
between the two groups before treatment (P>0.05); as for the
comparisons within the control group at 6 months after treatment,
there were differences in partial pressure of O2
(PaO2) (57.66±6.03 vs. 78.03±6.78, P=0.022) and arterial
partial pressure of carbon dioxide (PaCO2) (67.22±7.48
vs. 51.57±7.96, P=0.035), and there was no difference in arterial
O2 saturation (SaO2) (86.21±4.14 vs.
92.33±3.59, P=0.135). For the comparisons within the experimental
group, the PaO2 (58.26±5.58 vs. 86.21±6.33, P=0.022),
PaCO2 (65.43±7.89 vs. 45.85±7.01, P=0.029) and
SaO2 (88.65±4.22 vs. 95.26±5.02, P=0.035) had
differences. With regard to inter-group comparisons, there were
differences in PaO2 (78.03±6.78 vs. 86.21±6.33, P=0.026)
and PaCO2 (51.57±7.96 vs. 45.85±7.01, P=0.031) between
the control group and the experimental group. Conventional therapy
assisted by comprehensive pulmonary rehabilitation therapy has more
significant improvement effects on PaO2 and
PaCO2 of patients with severe pneumonia during
mechanical ventilation (Table
III).
 | Table III.Changes in blood gas indexes of the
two groups of patients before treatment and at 6 months after
treatment. |
Table III.
Changes in blood gas indexes of the
two groups of patients before treatment and at 6 months after
treatment.
|
| Control group
(n=60) | Experimental group
(n=60) | P-value |
|---|
| PaO2
(mmHg) |
| Before
treatment | 57.66±6.03 | 58.26±5.58 | 0.856 |
| After
treatment | 78.03±6.78 | 86.21±6.33 | 0.026 |
| PaCO2
(mmHg) |
| Before
treatment | 67.22±7.48 | 65.43±7.89 | 0.874 |
| After
treatment | 51.57±7.96 | 45.85±7.01 | 0.031 |
| SaO2
(time/min) |
| Before
treatment | 86.21±4.14 | 88.65±4.22 | 0.816 |
| After
treatment | 92.33±3.59 | 95.26±5.02 | 0.042 |
Changes in Borg index before treatment
and at 6 months after treatment
There was no difference in the Borg index between
the two groups of patients before treatment (P>0.05); at 6
months after treatment, the Borg index (3.58±0.61 vs. 2.09±0.53,
P=0.021) within control group was improved. For intra-group
comparison in experimental group, the Borg index (3.71±0.75 vs.
1.52±0.13, P=0.012) was improved. The Borg index (2.09±0.53 vs.
1.52±0.13, P=0.032) in experimental group was improved more
obviously compared with that in control group (Fig. 1).
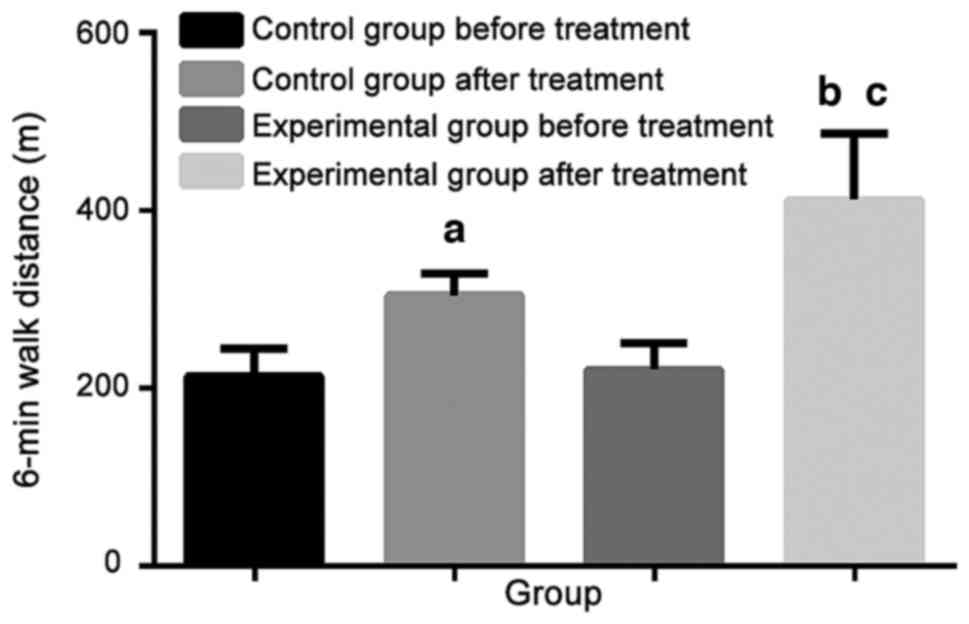
Changes in 6MWD results before
treatment and at 6 months after treatment (m)
Before treatment, there was no difference in the
6MWD between the two groups of patients (P>0.05); at 6 months
after treatment, in the control group, the 6MWD (214.32±31.02 vs.
304.71±24.33, P=0.026) was improved, and in the experimental group,
the 6MWD (221.11±29.59 vs. 412.45±74.77, P=0.012) was also
improved. As for the comparison of the 6MWD (304.71±24.33 vs.
412.45±74.77, P=0.035) between the control group and the
experimental group, the improvement in the experimental group was
more remarkable (Fig. 2).
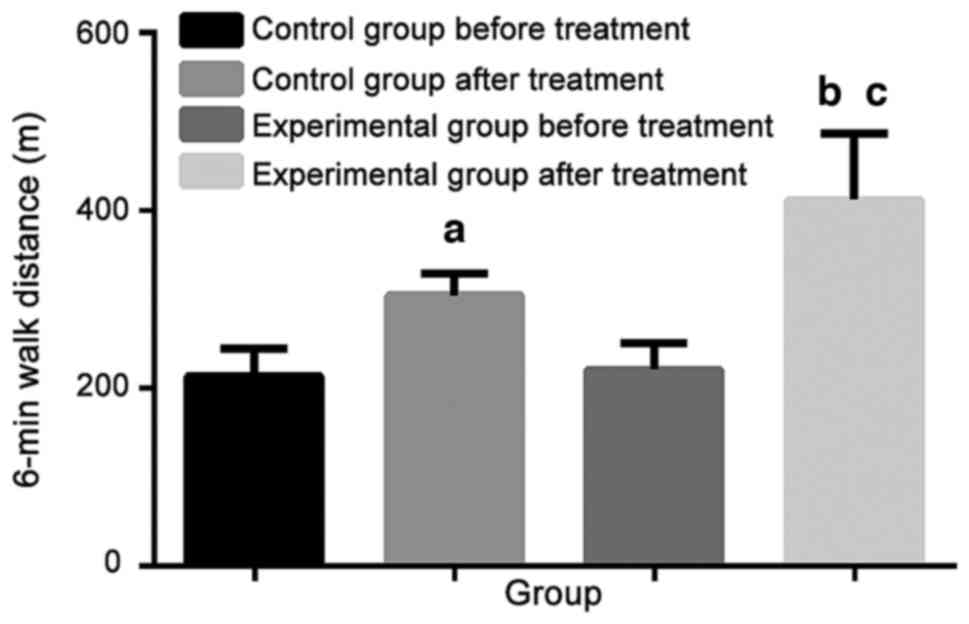 | Figure 2.Comparison of 6MWD results before
treatment and at 6 months after treatment. Before treatment, there
is no difference in the 6MWD between the two groups of patients
(P>0.05); at 6 months after treatment, in the control group, the
6MWD (214.32±31.02 vs. 304.71±24.33, P=0.026) is improved, and in
the experimental group, the 6MWD (221.11±29.59 vs. 412.45±74.77,
P=0.012) is also improved. As for comparison of the 6MWD
(304.71±24.33 vs. 412.45±74.77, P=0.035) between the control group
and the experimental group, the improvement in experimental group
is more remarkable. Compared with control group before treatment,
aP<0.05; Compared with experimental group before
treatment, bP<0.05; Compared with control group after
treatment, cP<0.05. |
Discussion
Bacterial pneumonia is a major complication of
severe pneumonia, and it is a main reason for respiratory failure
of the patients with severe pneumonia; in addition, it can induce
respiratory distress syndrome of the patients and lead to poor
prognosis and even death of the patients with severe pneumonia
(4,8). Mechanical ventilation is an
indispensable support means for treatment of patients with severe
pneumonia, but it is prone to cause lung injury and bacterial
infections, in the patients, which has extremely adverse effects on
the weaning and prognosis of the patients (9,10).
Therefore, the pulmonary rehabilitation therapy was applied in this
study. The pulmonary rehabilitation therapy is an important part of
management of patients with respiratory diseases, and it plays an
active role in improving the patients' pulmonary functions and
immunity (11,12). It was expected that the introduction
of pulmonary rehabilitation therapy could relieve and even reverse
the lung injury and other complications of the patients with severe
pneumonia during mechanical ventilation.
In the present study, the results of conventional
therapy and pulmonary rehabilitation therapy applied to 120
patients with severe pneumonia during mechanical ventilation were
summarized. The duration of this research was 6 months, and
patients with contraindications for pulmonary rehabilitation
therapy were excluded; meanwhile, the approval was obtained from
the ethics committee of the hospital, and the informed consent was
signed by the patients or their families.
It was found through the results of this study that
the pulmonary function indexes of the patients with severe
pneumonia in experimental group who received conventional therapy
assisted by pulmonary rehabilitation therapy were notably better
than those of the patients in control group who received simple
conventional therapy. It proves that pulmonary rehabilitation
therapy is of positive significance to ameliorating the pulmonary
functions of the patients with severe pneumonia during mechanical
ventilation. Pulmonary rehabilitation therapy is a pattern of
combined treatment for patients' exercise capacity, remission of
disease, recovery of pulmonary function and psychology, which
integrates prevention and treatment (13). The results of this study also
revealed that pulmonary rehabilitation therapy effectively improved
the MMEF and PEF and increased the VC and FEV1 of the patients,
thus ameliorating their pulmonary ventilation and gas exchange
functions. Lacasse et al (14) also indicated in their study results
that pulmonary rehabilitation therapy can ameliorate dyspnea and
improve the motor function of the patients in an effective manner.
In this study, the 6MWD of the patients was measured, and the
results showed that the 6MWD of the patients receiving pulmonary
rehabilitation therapy was improved effectively, and the Borg index
was also ameliorated significantly. The improvement of exercise
capacity is crucial to patients' further recovery from the disease,
not only to the enhancement of immunity, but also to the
improvement of information for disease recovery of the patients
(15). However, the results of this
study were partially different from those of McCarthy et al
whose results did not discover that pulmonary rehabilitation
therapy can improve FEV1, which may be caused by different research
objects; in the study of McCarthy et al, patients with
chronic obstructive pulmonary disease were enrolled as the major
research objects. There are few studies on the treatment effect of
pulmonary rehabilitation therapy in severe pneumonia; therefore,
the results of this study are only for reference, and pulmonary
rehabilitation therapy is mainly used to treat chronic pulmonary
diseases (16). Güell et al
(17) conducted a 3-year pulmonary
rehabilitation therapy for patients with severe chronic obstructive
pulmonary disease; it was found that the pulmonary rehabilitation
therapy has treatment effects only in the first 2 years, and that
its effects are not significant any more in 2 years later. It
provides a very important guidance for this study; since the
follow-up was conducted for only 6 months in this research, whether
the pulmonary rehabilitation therapy would be effective in a longer
duration of follow-up still remains unknown, which needs to be
investigated in the future. In addition, the blood gas indexes of
the patients with severe pneumonia were evaluated in this study,
and the results proved that the pulmonary rehabilitation therapy
has remarkable improvement effects on the patients'
PaO2, PaCO2 and SaO2. It was also
reported in the study of Huppmann et al (18) on the pulmonary rehabilitation therapy
for patients with interstitial pneumonia that the therapy can
ameliorate the blood gas indexes in an effective manner. It is
consistent with the results of this research, although the research
objects are different. The pulmonary rehabilitation therapy can
effectively improve the blood gas indexes of patients with chronic
obstructive pulmonary disease in the stable phase (19) and even non-small cell lung cancers
(20); all these have proven that
the pulmonary rehabilitation therapy has improvement effects on the
recovery of pulmonary functions and the exchange capacity between
oxygen and carbon dioxide in the body of the patients.
In conclusion, comprehensive pulmonary
rehabilitation therapy is conducive to improving the pulmonary
functions and blood gas indexes of patients with severe pneumonia
during mechanical ventilation, and it is beneficial to the exchange
capacity between oxygen and carbon dioxide in the body of the
patients.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
WL and XM wrote the manuscript. WL, XW, PZ and XM
were responsible for collecting patient data. XW, QL and LZ
analyzed the patient data. All authors read and approved the final
study.
Ethics approval and consent to
participate
This research was approved by the Ethics Committee
of the Jining No. 1 People's Hospital (Jining, China), and informed
consent was signed by the patients or their families.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ceccato A, Cilloniz C, Ranzani OT,
Menendez R, Agusti C, Gabarrus A, Ferrer M, Sibila O, Niederman MS
and Torres A: Treatment with macrolides and glucocorticosteroids in
severe community-acquired pneumonia: A post-hoc exploratory
analysis of a randomized controlled trial. PLoS One.
12:e01780222017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Feikin DR, Fu W, Park DE, Shi Q, Higdon
MM, Baggett HC, Brooks WA, Knoll Deloria M, Hammitt LL, Howie SRC,
et al: PERCH Study Group: Is higher viral load in the upper
respiratory tract associated with severe pneumonia? Findings From
the PERCH Study. Clin Infect Dis. 64 suppl_3:S337–S346. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Agweyu A, Gathara D, Oliwa J, Muinga N,
Edwards T, Allen E, Maleche-Obimbo E, English M, Aweyo F, Awuonda
B, et al: Severe Pneumonia Study Group: Oral amoxicillin versus
benzyl penicillin for severe pneumonia among kenyan children: A
pragmatic randomized controlled noninferiority trial. Clin Infect
Dis. 60:1216–1224. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tagami T, Matsui H, Horiguchi H, Fushimi K
and Yasunaga H: Recombinant human soluble thrombomodulin and
mortality in severe pneumonia patients with sepsis-associated
disseminated intravascular coagulation: An observational nationwide
study. J Thromb Haemost. 13:31–40. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Patel BK and Hall JB: Perioperative
physiotherapy. Curr Opin Anaesthesiol. 26:152–156. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
McCauley P and Datta D: Management of COPD
patients in the intensive care unit. Crit Care Nurs Clin North Am.
24:419–430. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Spruit MA, Singh SJ, Garvey C, ZuWallack
R, Nici L, Rochester C, Hill K, Holland AE, Lareau SC, Man WD, et
al: ATS/ERS Task Force on Pulmonary Rehabilitation: An official
American Thoracic Society/European Respiratory Society statement:
Key concepts and advances in pulmonary rehabilitation. Am J Respir
Crit Care Med. 188:e13–e64. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ngari MM, Fegan G, Mwangome MK, Ngama MJ,
Mturi N, Scott JAG, Bauni E, Nokes DJ and Berkley JA: Mortality
after inpatient treatment for severe pneumonia in children: A
cohort study. Paediatr Perinat Epidemiol. 31:233–242. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Esteban A, Frutos-Vivar F, Muriel A,
Ferguson ND, Peñuelas O, Abraira V, Raymondos K, Rios F, Nin N,
Apezteguía C, et al: Evolution of mortality over time in patients
receiving mechanical ventilation. Am J Respir Crit Care Med.
188:220–230. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Young D, Harrison DA, Cuthbertson BH,
Rowan K and Collaborators F: TracMan Collaborators: Effect of early
vs late tracheostomy placement on survival in patients receiving
mechanical ventilation: The TracMan randomized trial. JAMA.
309:2121–2129. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Spruit MA, Pitta F, Garvey C, ZuWallack
RL, Roberts CM, Collins EG, Goldstein R, McNamara R, Surpas P,
Atsuyoshi K, et al: ERS Rehabilitation and Chronic Care, and
Physiotherapists Scientific Groups; American Association of
Cardiovascular and Pulmonary Rehabilitation; ATS Pulmonary
Rehabilitation Assembly and the ERS COPD Audit team: Differences in
content and organisational aspects of pulmonary rehabilitation
programmes. Eur Respir J. 43:1326–1337. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ryerson CJ, Cayou C, Topp F, Hilling L,
Camp PG, Wilcox PG, Khalil N, Collard HR and Garvey C: Pulmonary
rehabilitation improves long-term outcomes in interstitial lung
disease: A prospective cohort study. Respir Med. 108:203–210. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Corhay JL, Dang DN, Van Cauwenberge H and
Louis R: Pulmonary rehabilitation and COPD: Providing patients a
good environment for optimizing therapy. Int J Chron Obstruct
Pulmon Dis. 9:27–39. 2014.PubMed/NCBI
|
|
14
|
Lacasse Y, Brosseau L, Milne S, Martin S,
Wong E, Guyatt GH and Goldstein RS: Pulmonary rehabilitation for
chronic obstructive pulmonary disease. Cochrane Database Syst Rev.
88:CD0037932002.
|
|
15
|
Chang G, Meadows ME, Orav EJ and Antin JH:
Mental status changes after hematopoietic stem cell
transplantation. Cancer. 115:4625–4635. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
McCarthy C, Brennan JR, Brown L, Donaghy
D, Jones P, Whelan R, McCormack N, Callanan I, Ryan J and McDonnell
TJ: Use of a care bundle in the emergency department foracute
exacerbations of chronic obstructive pulmonary disease:a
feasibility study. Int J Chron Obstruct Pulmon Dis. 8:605–611.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Güell MR, Cejudo P, Ortega F, Puy MC,
Rodríguez-Trigo G, Pijoan JI, Martinez-Indart L, Gorostiza A, Bdeir
K, Celli B, et al: Benefits of long-term pulmonary rehabilitation
maintenance program in patients with severe chronic obstructive
pulmonary sisease. Three-Year Follow-up. Am J Respir Crit Care Med.
195:622–629. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Huppmann P, Sczepanski B, Boensch M,
Winterkamp S, Schönheit-Kenn U, Neurohr C, Behr J and Kenn K:
Effects of inpatient pulmonary rehabilitation in patients with
interstitial lung disease. Eur Respir J. 42:444–453. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Struik FM, Lacasse Y, Goldstein RS,
Kerstjens HA and Wijkstra PJ: Nocturnal noninvasive positive
pressure ventilation in stable COPD: A systematic review and
individual patient data meta-analysis. Respir Med. 108:329–337.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tokarski S, Tokarska K, Schwarz E,
Obrebska A, Mejer A and Kowalski J: Blood gas analysis, blood
saturation and chosen parameters of spirometric examination in
NSCLC patients undergoing chemotherapy and pulmonary
rehabilitation. Pol Merkur Lekarski. 36:249–253. 2014.PubMed/NCBI
|