Introduction
Tuberculous pleuritis is the pleuritis induced by
the entering of tuberculous bacilli and their metabolites and
autolysates into the pleural cavities of hypersensitive organisms
and is a common disease in clinical practice (1,2). The
tuberculous pleuritis is an acute disease and mainly exhibits two
major symptoms (3), namely, the
local symptom induced by pleural effusion accumulation and the
systemic toxic symptom caused by tuberculosis. Tuberculous
pleuritis belongs to the infectious diseases and its infection
source is tuberculous bacillus (4).
Globally, there are ~2.1 billion individuals infected with the
tuberculous bacillus every year, and most patients were reported in
India and Russia (5). Pulmonary
tuberculosis induced by the tuberculous bacillus is the most common
type, and patients with tuberculous pleuritis account for ~3.0% of
all pulmonary tuberculosis patients (4). Treatment of the tuberculous pleuritis
is not difficult but the treatment period is long and the
recurrence rate is high. Therefore, early diagnosis and treatment
are still critical (6).
Currently, the most common diagnostic method of this
disease is B-mode ultrasound imaging or computed tomography (CT)
examination, but the application of single examination are
challenged by some shortcomings, such as the low accuracy rate and
high rate of misdiagnosis (7). In
this study, a total of 685 cases with tuberculous pleuritis who
were admitted to Yantaishan Hospital (Yantai, China) from January
2012 to August 2016 were selected as the study subjects. Indicators
of the tuberculous pleuritis diagnoses by B-mode ultrasound, CT and
the combined application were analyzed, respectively, to provide
reference and guidance for the clinical diagnoses of the
tuberculous pleuritis.
Patients and methods
Clinical data
A total of 685 patients who were treated in
Yantaishan Hospital from January 2012 to August 2016 and
pathologically diagnosed with tuberculous pleuritis, were selected
to serve as study subjects. Those patients included 399 male cases
and 286 female cases with a mean age of 48.6±12.3 years. Clinical
data of patients including sex, age and hospitalization time were
collected. The study was approved by the Ethics Committee of
Yantaishan Hospital (Yantai, China) and informed consents were
signed by the patients or the guardians.
Methods
All patients underwent CT examination 1–2 weeks
after B-mode ultrasound in Yantaishan Hospital. B-mode ultrasound
diagnosis: Philips EPIQ5 B-mode ultrasound examination instrument
(Philips Healthcare, Amsterdam, The Netherlands) was used. Patients
were fixed in sitting position with both hands raised and the body
slightly bending forward and the examination of the longitudinal
section was started from the area between the 7th and 8th rib of
the posterior axillary lines. The effusion area was reached when no
echoes were detected. Examination was then conducted on the
diagonal plane along the intercostal spaces and the range and
thickness of the effusion were recorded. Pleural thickness of
patients was observed and the range of the liquid anechoic area was
measured to confirm the existence of suspicious echoes. Puncture
fluid was collected under the guidance of B-mode ultrasound if
suspicious echoes existed to conduct further examination. CT
diagnosis: LightSpeed spiral CT examination instrument with 64 rows
and 128 layers (GE Healthcare, Chicago, IL, USA) was used. Patients
were fixed in supine position and the routine 4-mm thick-layer
interval-free scanning was conducted in the area from the scanned
pulmonary apexes to the bilateral costal diaphragmatic angles with
breath-holding. If obvious shaded area could not be recognized,
foregoing scanning could be replaced by 2-mm thin-layer
interval-free scanning or high-resolution computed tomography
(HRCT) scanning. B-mode ultrasound and CT imaging results were
evaluated with reference to the diagnostic standard for the
tuberculous pleuritis established by Porcel (4). With pathological diagnosis with
reference, the diagnostic values of B-mode ultrasound, CT diagnosis
and combined diagnosis were compared. Diagnostic sensitivity =
true-positive number of patients/(number of true-positive patients
+ false-negative patients) ×100%; diagnostic specificity =
true-negative number of patients/(number of false-positive +
true-negative patients) ×100%; diagnostic coincidence = (number of
true-positive + true-negative patients)/total number of patients
×100%; positive predictive value = true-positive number of
patients/(number of true-positive patients + false-positive
patients) ×100%.
Inclusion and exclusion criteria
Inclusion criteria: patients with clinical symptoms
of the tuberculous pleuritis; patients diagnosed with B-mode
ultrasound and CT; patients pathologically diagnosed with
tuberculous pleuritis; patients with positive results of purified
protein derivative (PPD). Exclusion criteria: patients accompanied
with other pulmonary diseases; patients with a history of
cardiopulmonary diseases; patients that suffered from pulmonary
dysfunction; patients transferred to other hospitals during
treatment. All the patients signed an informed consent.
Interpretation of results
All imaging results were reviewed by the 3 senior
imaging physicians of the hospital using a double-blind method.
B-mode ultrasonography usually showed free-style images, and
patients with multiple echo-free areas within the effusion were
diagnosed with tuberculous pleurisy. In CT examination, patients
with free pleural effusion, pleural constriction thickening,
pleural effusion, pleural extensive thickening, adhesion,
calcification, mild to moderate contrast medium injection and CT
value >25 HU were diagnosed with tuberculous pleurisy. In the
combination, patients with positive diagnosis of both examinations
were diagnosed with tuberculous pleurisy.
Statistical analysis
Experimental results were analyzed by Statistical
Product and Service Solutions (SPSS) 22.0 statistical software
[AsiaAnalytics (formerly SPSS China), Shanghai, China]. Enumeration
data are expressed as rate. Intergroup comparisons were made by
χ2 test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Clinical data
Clinical data of patients including sex, age and
hospitalization time are shown in Table
I. Pleural effusion was mainly localized in the right parts and
the amount of yellow pleural effusion was significantly more than
bloody effusion (Table I). The
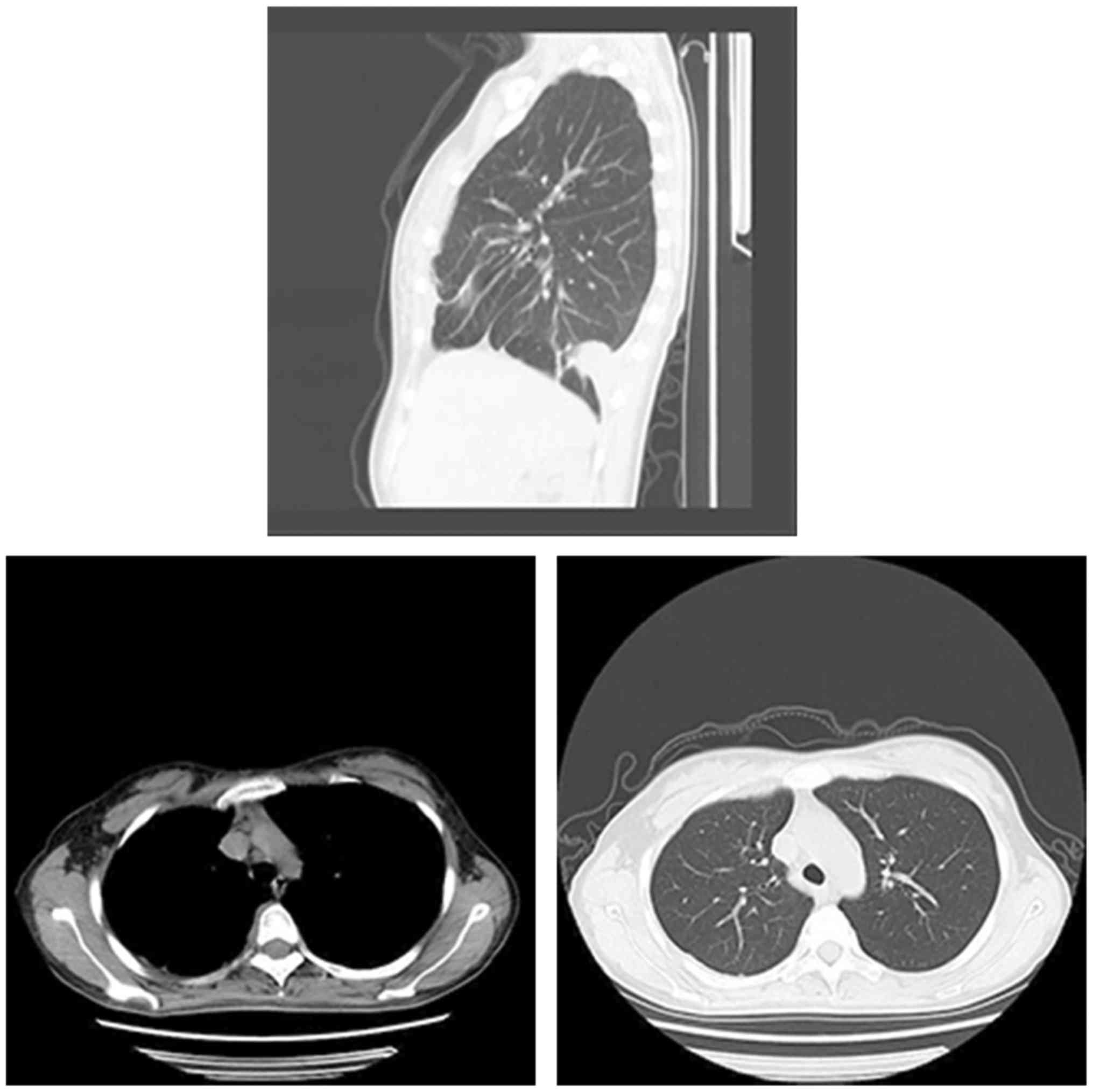
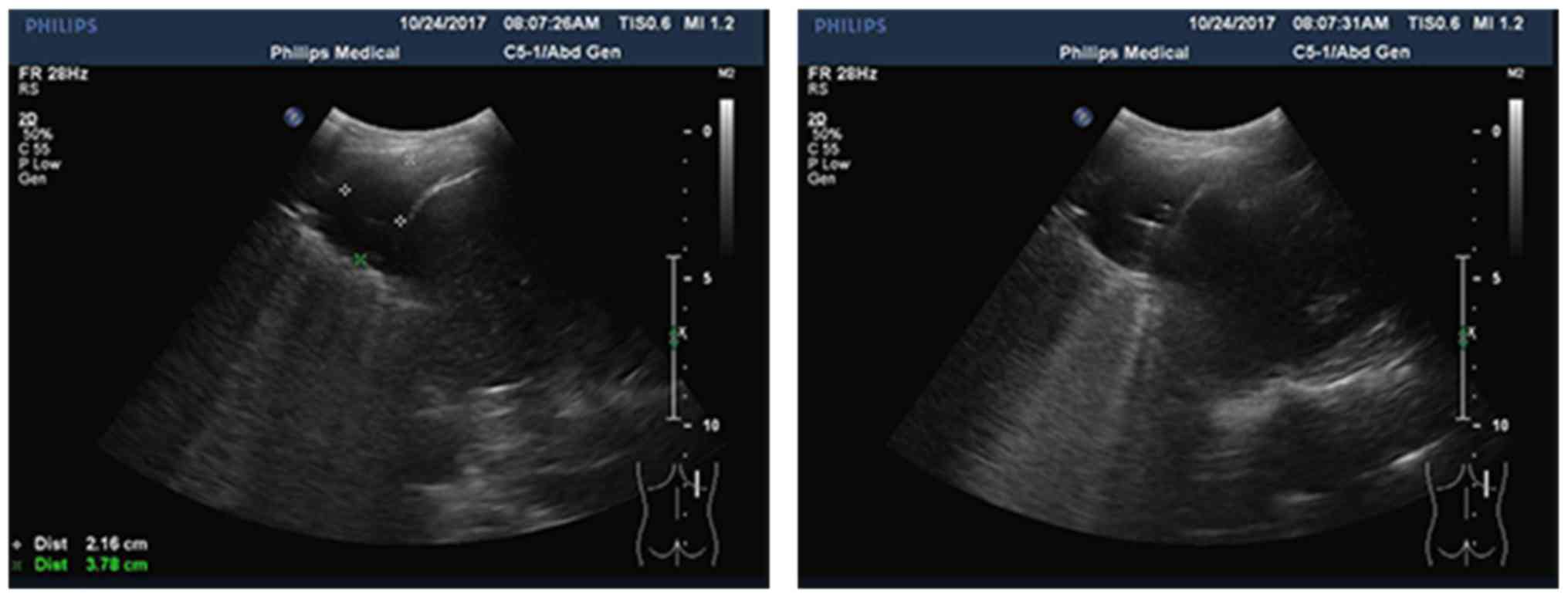
typical CT and ultrasound images are shown in Figs. 1 and 2.
 | Table I.Clinical data of patients (n, %). |
Table I.
Clinical data of patients (n, %).
| Variables | Values |
|---|
| Sex |
|
| Male | 399 (58.2) |
|
Female | 286 (41.8) |
| Age (years) |
|
|
<30 | 428 (62.5) |
| ≥30 | 257 (37.5) |
| Hospitalization time
(h) |
|
|
<10 | 345 (50.4) |
| ≥10 | 340 (49.6) |
| Clinical
symptoms |
|
|
Fever | 272 (39.7) |
| Chest
pain | 178 (26.0) |
| Chest
distress | 156 (22.8) |
|
Dyspnea | 79 (11.5) |
| Residential
location |
|
|
Urban | 386 (56.4) |
|
Rural | 299 (43.6) |
| Distribution of
pleural effusion |
|
| Left | 171 (25.0) |
|
Right | 418 (61.0) |
|
Bilateral | 96 (14.0) |
| Exercise habit |
|
| Yes | 441 (64.4) |
| No | 244 (35.6) |
| Smoking history |
|
| Yes | 496 (72.4) |
| No | 189 (27.6) |
| Color of pleural
effusion |
|
|
Yellow | 562 (82.1) |
|
Bloody | 123 (17.9) |
Diagnostic results
Among 685 patients, there were 574 cases of
tuberculous pleurisy and 111 cases of other types of pleurisy,
including 34 cases of fibrin pleurisy, 57 cases of connective
tissue disease, 18 cases of serofibrin pleurisy and 2 cases of
tumor pleurisy. Further observation showed that the patients with
tuberculous pleurisy had been in contact with the same type of
patients, suggesting that more attention should be paid to the
isolation of infectious diseases. A total of 451 cases of
tuberculous pleurisy were diagnosed by B-mode ultrasound, 501 cases
were diagnosed by CT and 546 cases were diagnosed by B-mode
ultrasound combined with CT (Tables
II–IV).
 | Table II.Tuberculous pleurisy diagnosed by
B-mode ultrasound. |
Table II.
Tuberculous pleurisy diagnosed by
B-mode ultrasound.
| Item | Bacterial culture
(+) | Bacterial culture
(−) | Total |
|---|
| B-mode ultrasound
(+) | 376 | 75 | 451 |
| B-mode ultrasound
(−) | 198 | 36 | 234 |
| Total | 574 | 111 |
 | Table IV.Tuberculous pleurisy diagnosed by
B-mode ultrasound combined with CT. |
Table IV.
Tuberculous pleurisy diagnosed by
B-mode ultrasound combined with CT.
| Item | Bacterial culture
(+) | Bacterial culture
(−) | Total |
|---|
| Combination diagnosis
(+) | 512 | 34 | 546 |
| Combination diagnosis
(−) | 62 | 77 | 139 |
| Total | 574 | 111 |
Differences between B-mode ultrasound
and CT examination
Compared with the findings of CT examination, B-mode
ultrasound examination was less effective concerning the thickening
of the parietal pleura and the combined pericardial effusion. There
were no obvious differences concerning the pleural effusion and
calcification between the results of the two methods (P>0.05)
(Table V).
 | Table V.Imaging diagnostic results of B-mode
ultrasound and CT examinations (n, %). |
Table V.
Imaging diagnostic results of B-mode
ultrasound and CT examinations (n, %).
| Item | B-mode
ultrasound | CT | χ2 | P-value |
|---|
| Pleural effusion | 534 (77.96) | 492 (71.82) | 6.847 | 0.071 |
| Pleural
calcification | 507 (74.01) | 497 (72.55) | 0.373 | 0.068 |
| Parietal pleura
thickening | 19 (2.77) | 149 (21.75) | 114.723 | 0.021 |
| Pericardial
effusion | 41 (5.99) | 86 (12.55) | 17.571 | 0.036 |
Sensitivity and specificity of B-mode
ultrasound, CT and the combined diagnosis
The sensitivity and specificity of the three
diagnostic methods for the tuberculous pleuritis were as follows:
the sensitivity of B-mode ultrasound was 85.51%, the specificity
72.34%, the diagnostic accordance rate 60.15% and the positive
predictive value 83.37%; the sensitivity of CT was 79.69%, the
specificity 83.44%, the diagnostic accordance rate 70.07% and the
positive predictive value 86.83%; the sensitivity of B-mode
ultrasound + CT was 93.81%, the specificity 95.75%, the diagnostic
accordance rate 85.99% and the positive predictive value 93.77%.
The sensitivity, specificity, diagnostic accordance rate and
positive predictive value of the combined diagnosis were increased
compared with those of single examination (P<0.05) (Table VI).
 | Table VI.Sensitivity and specificity of the
three kinds of diagnostic methods (%). |
Table VI.
Sensitivity and specificity of the
three kinds of diagnostic methods (%).
| Item | Sensitivity | Specificity | Diagnostic accordance
rate | Positive predictive
value |
|---|
| B-mode
ultrasound | 85.51 | 72.34 | 60.15 | 83.37 |
| CT | 79.69 | 83.44 | 70.07 | 86.83 |
| B-mode ultrasound +
CT | 93.81 | 95.75 | 85.99 | 93.77 |
| χ2 | 91.031 | 23.964 | 115.673 | 27.530 |
| P-value | 0.0429 | 0.0457 | 0.0305 | 0.0427 |
Discussion
Tuberculous pleuritis is the most common cause of
pleural effusion (8). After
tuberculous bacilli infects pleura, cell-mediated immune response
is induced by the stimulation of the inflammation, leading to a
series of symptoms such as edema and congestion, proliferation of
lymphocytes and the exudation of fibrous proteins on the pleural
surfaces. Under those conditions, capillary permeability is greatly
increased, and a large amount of proteins, blood cells and water is
accumulated in pleural cavities and form the pleural effusion
(9,10). Accumulation of the pleural effusion
causes the decline in absorption ability of visceral pleura and
non-absorbable proteins and celluloses form fibrous moss in pleura.
As a result, the thickening, wrapping and adhesion of the pleura
occurs. In severe cases, the respiratory function is directly
affected, leading to asphyxia (11,12).
According to patients' clinical data, most patients
with tuberculous pleuritis were younger than 30 years old, the
pleural effusion of patients mainly aggregated in the right side
and was mostly yellow effusion. Clinical symptoms mainly included
fever, the incidence among urban residents was higher than that
among rural residents, and higher incidence was observed in smoking
individuals. Possible explanations for these observations are:
young and adult patients are more vulnerable to this disease due to
the stronger response to the infection of tuberculosis bacilli
compared with patients in other age groups (13); urban residents were exposed to
harmful gases (factory emission, vehicle exhaust and passive
smoking) and transmission of the tuberculous pleuritis is easier;
for the smoking patients, nicotine, tar, carbon monoxide and other
harmful gases may destroy the original immune system and the
filtration system of the lungs, thus it is easier for the
tuberculous bacillus to infect the cardio-pulmonary functions
(14,15). The bacteriological culture
examination cannot make the diagnosis to the pleurisy caused by the
non-bacterial pathogen, therefore, the tuberculous pleurisy is
generally excluded and needs to go through many examinations to
confirm the pathological type. Accuracy rates of B-mode ultrasound,
CT examination and the combined diagnosis were compared with the
pathological diagnosis. Results showed that there were basically no
differences in the accuracy between B-mode ultrasound and CT
diagnoses. CT examination is more helpful in the identification of
the thickening of parietal pleura and combined pericardial
effusion. However, the accuracy, specificity and sensitivity of the
combined diagnosis were higher than those of single examination.
B-mode ultrasound diagnosis is the simplest examination method with
high economic effectiveness and CT examination has not been
popularized in the majority of primary hospitals. Therefore, most
patients with tuberculous pleuritis are diagnosed by B-mode
ultrasound. B-mode ultrasound is highly sensitive to pleural
effusion and can accurately localize the effusion. B-mode
ultrasound can be used to accurately estimate effusion location and
volume. In addition, B-mode ultrasound can also be used to guide
the extraction of the puncture fluid from the pleural cavities and
the identification of the thickening of pleura (16). Nevertheless, with B-mode ultrasound
it is hard to detect substantive void, the place communicating with
the pleural cavity, lymph node enlargement and other lesion
conditions in the lungs of the tuberculous pleuritis patients, thus
the specificity is not high. Therefore, the accuracy of B-mode
ultrasound in the diagnosis of tuberculous pleuritis is slightly
lower than that of CT. This is consistent with the findings
reported by Brunetti et al (17). CT examination has the higher density
and spatial resolution and can more accurately show the thickening
of the parietal pleura and pericardial effusion in patients with
tuberculous pleuritis compared with B-mode ultrasound. Moreover, it
can be used to examine the lymphatic vessels and old tuberculous
focus (18). The combined
examination by B-mode ultrasound and CT can compensate the
shortcomings of the two single examinations and improve the
specificity, sensitivity and accuracy.
In this study, clinical data of 685 cases of
tuberculous pleuritis were retrospectively analyzed with the
expectation of providing new insights for the diagnosis of this
disease using B-mode ultrasound and CT. However, there are still
shortcomings. The comparison of the results of B-mode ultrasound
and CT among different age groups and between smokers and
non-smokers were not studied. So, more studies are still
needed.
In conclusion, both B-mode ultrasound and CT can
accurately diagnose tuberculous pleuritis, but the combined
diagnosis by the two methods can compensate the shortcomings of
each technique. Therefore, the combined diagnosis should be
popularized in clinical practice.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
SZ, JZ and YP conceived and designed the study. SZ,
XS and MZ were responsible for the collection and analysis of the
patient data. JZ and HL interpreted the data and drafted the
manuscript. YP revised the manuscript critically for important
intellectual content. All authors read and approved the final
study.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Yantaishan Hospital (Yantai, China). Signed informed consents were
obtained from the patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chakrabarti B and Davies PD: Pleural
tuberculosis. Monaldi Arch Chest Dis. 65:26–33. 2006.PubMed/NCBI
|
|
2
|
Lee JY: Diagnosis and treatment of
extrapulmonary tuberculosis. Tuberc Respir Dis (Seoul). 78:47–55.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Vorster MJ, Allwood BW, Diacon AH and
Koegelenberg CF: Tuberculous pleural effusions: Advances and
controversies. J Thorac Dis. 7:981–991. 2015.PubMed/NCBI
|
|
4
|
Porcel JM: Advances in the diagnosis of
tuberculous pleuritis. Ann Transl Med. 4:2822016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sia JK, Georgieva M and Rengarajan J:
Innate immune defenses in human tuberculosis: An overview of the
interactions between mycobacterium tuberculosis and innate immune
cells. J Immunol Res. 2015:7475432015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chen KY, Feng PH, Chang CC, Chen TT,
Chuang HC, Lee CN, Su CL, Lin LY and Lee KY: Novel biomarker
analysis of pleural effusion enhances differentiation of
tuberculous from malignant pleural effusion. Int J Gen Med.
9:183–189. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dietrich CF, Mathis G, Cui XW, Ignee A,
Hocke M and Hirche TO: Ultrasound of the pleurae and lungs.
Ultrasound Med Biol. 41:351–365. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cao GQ, Li L, Wang YB, Shi ZZ, Fan DY and
Chen HY: Treatment of free-flowing tuberculous pleurisy with
intrapleural urokinase. Int J Tuberc Lung Dis. 19:1395–1400. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Porcel JM, Gasol A, Bielsa S, Civit C,
Light RW and Salud A: Clinical features and survival of lung cancer
patients with pleural effusions. Respirology. 20:654–659. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yousefifard M, Baikpour M, Ghelichkhani P,
Asady H, Shahsavari Nia K, Moghadas Jafari A, Hosseini M and Safari
S: Screening performance characteristic of ultrasonography and
radiography in detection of pleural effusion; a meta-analysis.
Emerg (Tehran). 4:1–10. 2016.PubMed/NCBI
|
|
11
|
Nguyen AH, Miller EJ, Wichman CS, Berim IG
and Agrawal DK: Diagnostic value of tumor antigens in malignant
pleural effusion: A meta-analysis. Transl Res. 166:432–439. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Antonangelo L, Sales RK, Corá AP, Acencio
MM, Teixeira LR and Vargas FS: Pleural fluid tumour markers in
malignant pleural effusion with inconclusive cytologic results.
Curr Oncol. 22:e336–e341. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kahwati LC, Feltner C, Halpern M, Woodell
CL, Boland E, Amick HR, Weber RP and Jonas DE: Primary care
screening and treatment for latent tuberculosis infection in
adults: Evidence report and systematic review for the US preventive
services task force. JAMA. 316:970–983. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Bae KM, Lim SC, Kim HH, Lee WJ, Yun NR,
Kim CM and Kim DM: The relevance of biopsy in tuberculosis patients
without human immunodeficiency virus infection. Am J Trop Med Hyg.
92:636–640. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Manglani RP, Khaja M, Hennessey K and
Kennedy O: Pleural mycobacterium avium complex infection in an
immunocompetent female with no risk factors. Case Rep Pulmonol.
2015:7606142015.PubMed/NCBI
|
|
16
|
Koegelenberg CF, Irusen EM, von
Groote-Bidlingmaier F, Bruwer JW, Batubara EM and Diacon AH: The
utility of ultrasound-guided thoracentesis and pleural biopsy in
undiagnosed pleural exudates. Thorax. 70:995–997. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Brunetti E, Heller T, Richter J,
Kaminstein D, Youkee D, Giordani MT, Goblirsch S and Tamarozzi F:
Application of ultrasonography in the diagnosis of infectious
diseases in resource-limited settings. Curr Infect Dis Rep.
18:62016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Metintas M, Yildirim H, Kaya T, Ak G,
Dundar E, Ozkan R and Metintas S: CT scan-guided Abrams' needle
pleural biopsy versus ultrasound-assisted cutting needle pleural
biopsy for diagnosis in patients with pleural effusion: A
randomized, controlled trial. Respiration. 91:156–163. 2016.
View Article : Google Scholar : PubMed/NCBI
|