Introduction
Osteonecrosis of the femoral head (ONFH) is one of
the most common challenging orthopaedic conditions and poses a
great threat to human health (1,2). ONFH
has a high occurrence rate; in China, an estimated
5,000,000-7,500,000 ONFH patients currently require treatment and
the number of novel cases per year is as high as 150,000-300,000,
and thus, it ranks first among hip joint diseases (3,4). ONFH
frequently occurs in young and middle-aged populations. Without any
timely and effective treatment, ONFH develops to femoral collapse
in ~80% of patients within 1–4 years, ultimately causing severe
damage to the entire hip joint (5–9).
At present, ONFH patients without collapse or with
only mild collapse are primarily subjected to joint preservation.
However, once noticeable femoral collapse occurs, the efficacy of
preservation treatment is greatly decreased. Consequently, patients
must undergo total hip arthroplasty (THA) (8,10,11).
Furthermore, artificial prostheses have a limited service life. For
this reason, most young patients receive repeated THA, which is not
only painful for them but also greatly increases the economic
burden on their family and society (12). Therefore, whether collapse occurs
after ONFH is critically relevant to the prognosis of ONFH and the
guidance of clinical treatment, and accordingly, the prediction of
collapse after ONFH has long been a clinical research focus.
Numerous studies have indicated that whether femoral
collapse occurs after ONFH is associated with the location and size
of the necrosis, as well as with the bone remodelling ability, and
most of the studies that evaluated the Association Research
Circulation Osseous (ARCO) stage, Japanese Investigation Committee
(JIC) type, the sum of the necrotic angles, the proportion of the
necrotic area and the proportion of the proximal sclerotic rim have
indicated that a large necrotic area, necrosis located at the
lateral part of the femoral head and poor bone remodelling ability
after necrosis are risk factors for the collapse of the
osteonecrosis-affected femoral head (13–20).
However, due to the complexity of the issue itself and the
limitations of imaging examination, all of the above studies
predicted the occurrence of the collapse from only one perspective.
The ARCO (21) and Steinberg systems
(22) have been widely applied in
ONFH staging. These systems propose subtypes of ONFH based on its
severity and its characteristics at different stages. However,
their classifications of different subtypes of ONFH primarily focus
on the necrotic area based on imaging features of ONFH at different
stages, without taking the necrotic location into account. Li et
al (23) of the China-Japan
Friendship Hospital (CJFH) proposed a novel typing method based on
the necrotic location and the necrotic area. They postulated that
ONFH may be classified into the medial (M), central (C) and lateral
(L) types, and the L type may be further classified into L1, L2 and
L3; the M and C types have a good prognosis, followed by the L1
type, while the L2 and L3 types have the poorest prognosis. This
typing method may be used for direct demarcation of the necrotic
area and is not influenced by any acetabular anatomical factors.
The method results in smaller errors in predicting collapse
compared with other methods and is therefore more satisfactory than
other methods in clinical practice. However, the CJFH method has
its own limitations. First, it utilizes the medial slice of the
coronal section based on computerized tomography (CT) or magnetic
resonance imaging (MRI). It is generally thought that the medial
slice of the femoral head is the site that bears the maximal
stress. However, the maximal necrotic area may better reflect the
actual ONFH status, as it is the mechanically weak area where
collapse tends to occur. Therefore, the maximal necrotic area may
provide better information for accurate ONFH prognosis prediction.
In most patients with ONFH, the maximal plane of the necrotic focus
is not located at the medial plane, but instead slightly anterior
or posterior (24). Furthermore, the
CJFH method fails to clarify the mechanical foundation and detailed
demarcation of the three-pillar structure. This drawback causes a
degree of randomness in the demarcation of the femoral three-pillar
structure in clinical practice, thereby increasing the uncertainty
of the prediction results.
The structure of bones appears to be adapted to
performing specific functions. While the bone structure determines
what functions the bone is able to perform, the functions also
influence changes in the bone structure, i.e., a change in either
structure or function causes a change in the other to maintain the
balance between them (25–27). According to Wolff's law, bone
trabeculae are not arranged out of order, but rather along the
direction of the primary compression to present an optimal
stress-bearing characteristic (28).
According to this system, the proximal trabeculae of the femoral
head is divided into primary compression trabeculae, secondary
compression trabeculae, primary tensile trabeculae, secondary
tensile trabeculae, and pertrochanteric trabeculae, and the inside
of the femoral head comprises the primary compression trabeculae
and primary tensile trabeculae. A stress test on the proximal
femoral head demonstrated that the stress on the primary tensile
trabeculae was noticeably reduced under a normal physiological
load, whereas the primary compression trabeculae became the primary
stress region (29), suggesting that
the primary compression trabeculae serve as the primary
weight-bearing structure under a normal physiological load and as
the primary mechanical support site, and that the distribution
limits of the compression trabeculae may be regarded as a basis for
three-pillar demarcation. Analysis of the characteristics of the
collapse site in ONFH indicated that the anterolateral part of the
proximal femoral head is the most common site of collapse. This
part of the proximal femoral head contains sparsely distributed
primary compression trabeculae, suggesting an important
weight-bearing role for the compression trabeculae in the femoral
head (30). The application of the
three-pillar theory was first proposed by Herring et al
(31) in 1992 for the typing of
childhood ONFH (i.e., Legg-Calvé-Perthes' disease). According to
this theory, the integrity of the lateral pillar provides an
effective biomechanical shielding effect for the central part of
the femoral head, preventing collapse. If the lateral pillar is
structurally impaired as a result of disease, its shielding effect
disappears and collapse of the femoral head becomes
unavoidable.
In the light of these theories, a previous study by
our group assessed frontal X-ray images of the bilateral hips of
healthy volunteers (32). The
lateral, central and medial pillars were identified from the
intersection points of the lateral and medial rims of the primary
compression trabeculae with the maximum transverse diameter of the
femoral head, and the width ratios of the lateral, central and
medial pillars of the femoral head were then calculated to set a
standard of demarcating the three pillars. The results indicated
that the ratio of the three pillars of the femoral head in terms of
biomechanical weight bearing was ~3:4:3 (32). Based on this result and on the plane
with the maximal ONFH area, the present study proposes a novel
typing method for ONFH, referred to as ABC typing.
Materials and methods
General data
A total of 132 patients (223 hips) with ONFH who
received treatment at Guanganmen Hospital (Beijing, China) from
October 2012 to April 2015 were enrolled in the present study. The
diagnostic criteria were based on the Chinese Experts' Consensus on
the Diagnosis and Treatment of Osteonecrosis of the Femoral Head in
Adults from 2012 (1). Among the
patients, 94 were males and 38 were females. Their age ranged from
18 to 78 years, with a median age of 43 years. In total, 41
patients had ONFH in one hip and 91 in the bilateral hips, and the
median course of the disease was 50 months, ranging from 36 to 147
months. Within the cohort, 45 cases (34.1%) had alcohol-induced
ONFH; 57 cases (43.2%) had steroid-induced ONFH and 30 cases
(22.7%) had idiopathic ONFH. According to the ARCO staging criteria
for ONFH (21), 5 hips were stage I;
79 were stage II, 106 were stage III and 33 were stage IV.
The inclusion criteria for the present study were as
follows: i) Diagnosis of ONFH according to the abovementioned
criteria (1); ii) an ARCO stage of
≥I; iii) patient age of ≥18 years; iv) MRI or CT of both hip joints
available (for patients with an ARCO stage of ≥II); v) a natural
disease course of ≥3 years if no collapse of the femoral head had
occurred; and vi) informed consent provided by the patient.
Patients were excluded from the present study if they met any of
the following criteria: i) Traumatic ONFH or ONFH complicated by
other joint diseases (including bone neoplasms, rheumatoid
arthritis, ankylosing spondylitis, joint tuberculosis or
suppurative arthritis); ii) a severe congenital anomaly in the hip
joint; iii) a history of hip joint surgery; and iv) mental
disorders.
Grouping
An ARCO stage of ≥III was defined as the collapse of
the osteonecrosis-affected femoral. The patients were divided into
a collapse and a non-collapse group.
CT scanning
A Siemens 64-slice dual-source spiral CT (Siemens
AG, Munich, Germany) was used for successive scanning of the
bilateral hip joints along the cross-section. The scanning
parameters were as follows: Voltage, 120 kV; electric current, 60
mA; and slice thickness for bone tissue window scanning, 0.75 mm.
The images obtained were exported in bmp format.
MRI
A GE-signal 1.5 T superconducting nuclear magnetic
resonance analyser (GE Healthcare, Little Chalfont, UK) was
utilized to collect T1-weighted images (T1WI) of the coronal
section of the femoral head. The scanning parameters for T1WI were
as follows: Echo time, 12 msec; repetition time, 560 msec; coil,
USC_S12; number of excitations, 2.00; matrix, 320×256; field of
view, 24; slice thickness, 3.0 mm; and slice interval, 1 mm.
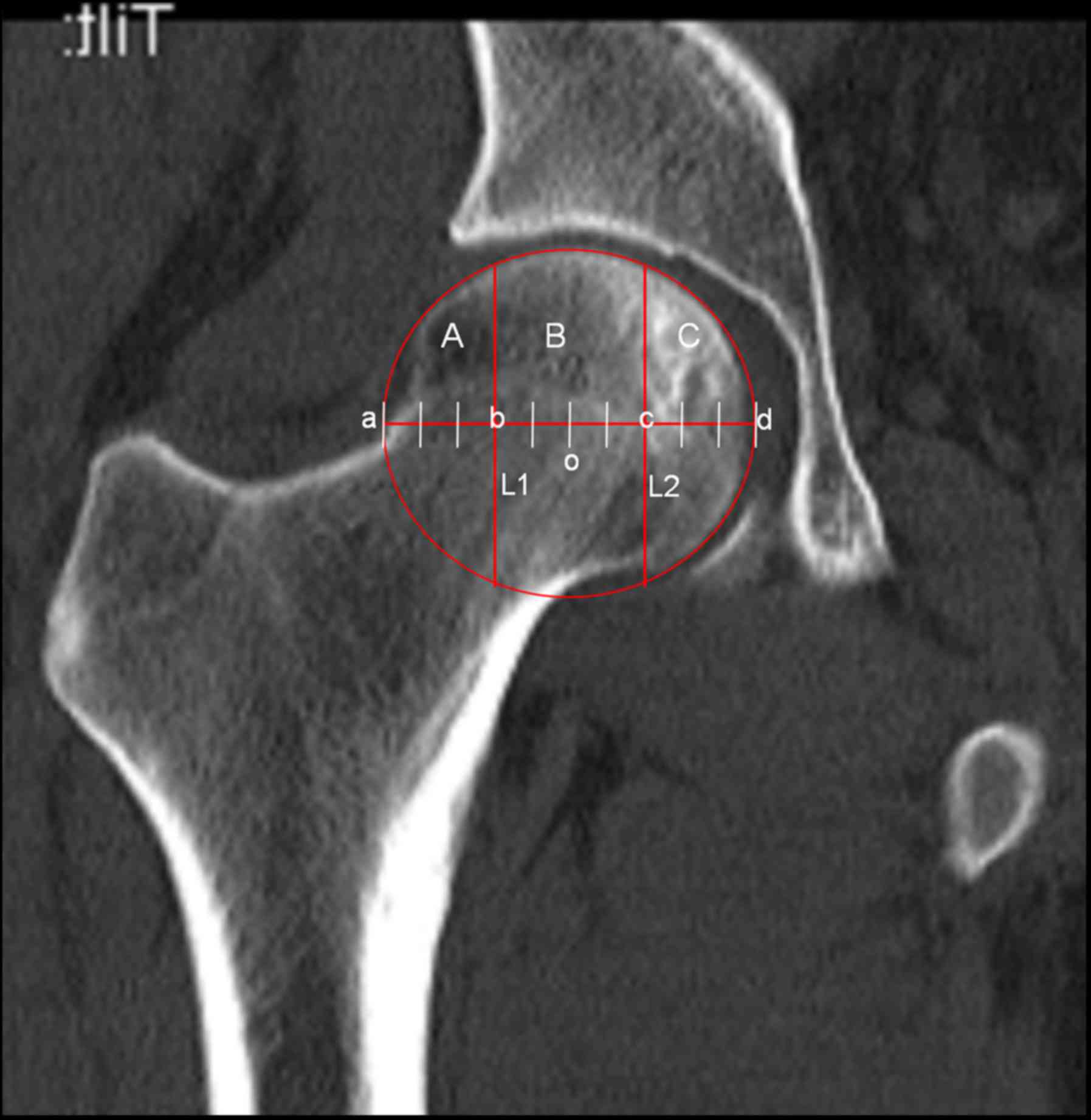
ABC typing method
Based on the three pillars defined by Herring in
Legg-Calvé-Perthes disease (31) and
the measurements and observations of the mechanical distribution
characteristics of bone trabeculae in X-ray images, the coronal
plane of the femoral head was divided into the lateral, central and
medial pillars, which represented 30, 40 and 30% of the total width
of the femoral head, respectively. The detailed demarcation method
was as follows: i) The slice with the maximal necrotic area was
selected from the CT (or MRI T1WI) images for measurement; ii) The
selected image was opened in Computer Aided Design software
(AutoCAD 2012; Autodesk, San Francisco, CA, USA); iii) The femoral
head was regarded as a circle to determine its centre, ‘O’. A
horizontal line was drawn across ‘O’ and the circle was intersected
at the points ‘a’ and ‘d’. The line section ‘ad’ was the maximum
transverse diameter of the femoral head; iv) The vertical lines L1
and L2 were drawn rectangular to the line ‘ad’, with the
intersection points named ‘b’ and ‘c’, respectively, dividing ‘ad’
into ‘ab’, ‘bc’ and ‘cd’ with a length ratio of 3:4:3. The three
sections divided by L1 and L2 corresponded to the three pillars A,
B and C (Fig. 1).
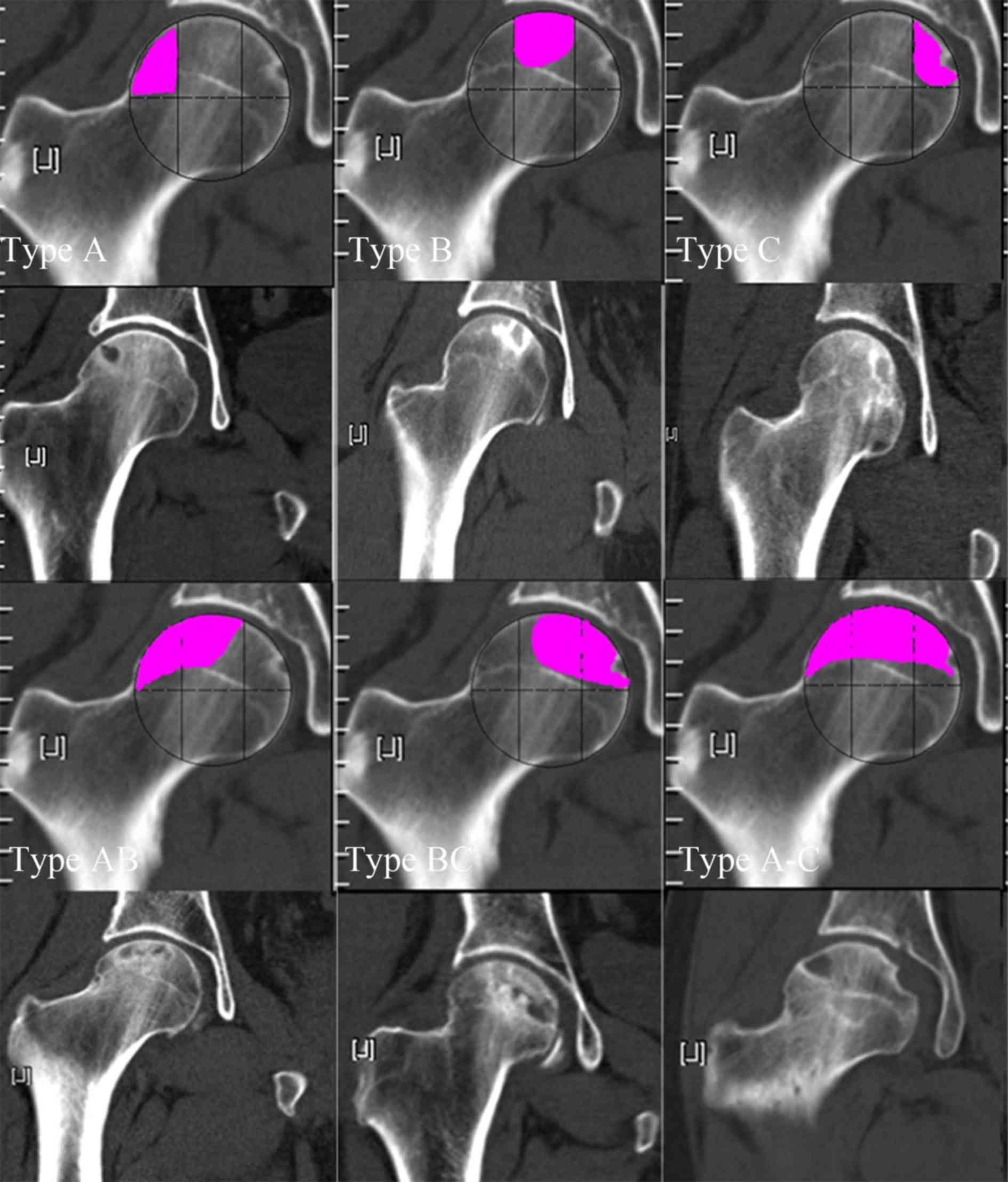
According to the involvement of the three pillars in
the necrotic focus, ONFH was classified into 6 types as follows
(Fig. 2): Type A (lateral)-the
lateral pillar was involved, but the central and medial pillars
were intact; Type B (central)-the central pillar was involved, but
the lateral and medial pillars were intact; Type C (medial)-the
medial pillar was involved, but the central and lateral pillars
were intact; Type AB (lateral double-pillar)-the lateral and
central pillars were involved, but the medial pillar was intact;
Type BC (medial double-pillar)-the central and medial pillars were
involved, but the lateral pillar was intact; Type A-C
(three-pillar)-all pillars were involved.
Collapse risk value assignment
The necrotic area is known to be positively
associated with the risk of collapse (14,17,18,20);
therefore, the involvement of one, two or three pillars was scored
as 1, 2 or 3 points, respectively. Furthermore, the collapse risk
is high when the lateral pillar is involved (23); thus, the involvement of the medial,
central or lateral pillar was assigned 1, 2 or 3 points,
respectively. Based on these methods, the collapse risk was scored
for different ABC types.
The differences in the occurrence of collapse in the
different ABC types of ONFH were examined, and the correlation of
the collapse risk value with the collapse rate was analysed. The
image review, evaluation and scoring were performed by experienced
orthopaedists.
Statistical analysis
Data were processed using SPSS 12.0 software (SPSS,
Inc., Chicago, IL, USA). The differences in the collapse rate among
different ABC types were tested using the chi-square method. The
correlation between the collapse risk value and the collapse rate
was analysed by calculating Spearman's rank correlation
coefficient. All statistical tests were two-sided. P<0.05 was
considered to indicate a statistically significant difference.
Results
Baseline data
The collapse group included 166 hips and the
non-collapse group included 57 hips. In the collapse group, 72
patients were males and 24 were females, and in the non-collapse
group, 22 were males and 14 were females. No significant difference
was observed in the gender ratio between the groups
(χ2=1.38, P=0.24). The average age of the collapse group
was 44±3 years and that of the non-collapse group was 45±4 years.
No significant difference in age was observed between the two
groups (t=−0.93, P=0.35). Finally, the average disease course of
the collapse group was 4.3±1.2 years, and that of the non-collapse
group was 4.0±0.7 years (t=0.98, P=0.33).
Distribution of the ONFH types
The proportions of the A, B, C, AB, BC and A-C types
among the total enrolled cases were 0.9, 9.4, 1.3, 12.1, 9.4 and
66.8%, respectively. These results suggest that ONFH involving only
the lateral or the medial pillar was rare in clinical practice,
whereas the involvement of all three pillars was common (Table I).
 | Table I.ABC typing of the hips with
osteonecrosis of the femoral head (n=223). |
Table I.
ABC typing of the hips with
osteonecrosis of the femoral head (n=223).
| ABC type | n (%) |
|---|
| A | 2 (0.9) |
| B | 21 (9.4) |
| C | 3 (1.3) |
| AB | 27 (12.1) |
| BC | 21 (9.4) |
| A-C | 149 (66.8) |
ABC typing of the collapse and non-collapse groups.
Among the 166 hips in the collapse group, one (0.6%) was type A,
two (1.2%) were type B, 20 (12.1%) were type AB, 11 (6.6%) were
type BC and 132 (79.5%) were type A-C. Among the 57 hips in the
non-collapse group, one (1.9%) was type A, 19 (33.3%) were type B,
three (5.3%) were type C, seven (12.3%) were type AB, 10 (17.5%)
were type BC and 17 (29.8%) were type A-C (Table II). Significant differences were
observed between the two groups regarding all types
(P<0.001).
 | Table II.Comparison of the proportion of hips
with different ABC types of osteonecrosis of the femoral head in
the collapse group (n=166) and the non-collapse group (n=57). |
Table II.
Comparison of the proportion of hips
with different ABC types of osteonecrosis of the femoral head in
the collapse group (n=166) and the non-collapse group (n=57).
| Collapse | A | B | C | AB | BC | A-C |
|---|
| Yes | 1 (0.6) | 2 (1.2) | 0 (0.0) | 20 (12.1) | 11 (6.6) | 132 (79.5) |
| No | 1 (1.9) | 19 (33.3) | 3 (5.3) | 7 (12.3) | 10 (17.5) | 17 (29.8) |
Collapse occurrence in the different
types of ONFH
Among the 223 hips with ONFH, collapse occurred in
50, 9.5, 0.0, 74.1, 52.4 and 88.6% of hips of the type A, B, C, AB,
BC and A-C, respectively (χ2=76.93, P<0.001). For the
different ONFH types, collapse occurred most frequently in the
following order: A-C>AB>BC>A>B>C (Table III).
 | Table III.Collapse rates in the different types
of osteonecrosis of the femoral head. |
Table III.
Collapse rates in the different types
of osteonecrosis of the femoral head.
| ABC type | Hips (n) | Collapses, n
(%) |
|---|
| A | 2 | 1 (50.0) |
| B | 21 | 2 (9.5) |
| C | 3 | 0 (0.0) |
| AB | 27 | 20 (74.1) |
| BC | 21 | 11 (52.4) |
| A-C | 149 | 132 (88.6) |
| Total | 223 | 166 (74.4) |
Pairwise comparison of the collapse occurrence
between the different types of ONFH revealed significant
differences (Table III). However,
as the sample size of certain groups was small (for instance, there
were only 2 cases of type A and 3 cases of type C), the statistical
power may have been low. Therefore, the data were re-analysed
regarding the extent and location of ONFH using a lower number of
categories. Based on the number of pillars involved (i.e., the
necrotic area), the joints were stratified into one-, two- and
three-pillar involvement groups. In addition, according to whether
the necrosis affected the lateral pillar, the joints were
stratified into lateral pillar-involving and non-lateral
pillar-involving groups. The analysis of the merged data revealed
the following: The groups with different numbers of pillars
involved exhibited significant differences (χ2=72.20,
P<0.001), in the following order: The three-pillar group
(88.6%)> the two-pillar group (64.6%)> the one-pillar group
(11.5%; Table IV). Furthermore, the
lateral pillar-involving group and the non-lateral pillar-involving
groups exhibited a significant difference in the collapse rate
(86.0 vs. 28.9%; χ2=61.47, P<0.001; Table V).
 | Table IV.Frequency of collapse of femoral
heads with osteonecrosis stratified by the number of pillars
involved. |
Table IV.
Frequency of collapse of femoral
heads with osteonecrosis stratified by the number of pillars
involved.
| Pillars | Hips (n) | Collapsed femoral
heads, n (%) |
|---|
| 1 | 26 | 3 (11.5) |
| 2 | 48 | 31 (64.6) |
| 3 | 149 | 132 (88.6) |
| Total | 223 | 166 (74.4) |
 | Table V.Proportion of collapsed hips in
patients with osteonecrosis of the femoral head stratified based on
involvement of the lateral pillar. |
Table V.
Proportion of collapsed hips in
patients with osteonecrosis of the femoral head stratified based on
involvement of the lateral pillar.
| Lateral pillar
involvement | Hips (n) | Collapsed femoral
heads, n (%) |
|---|
| Yes | 178 | 153 (86.0) |
| No | 45 | 13 (28.9) |
| Total | 223 | 166 (74.4) |
Correlation between the collapse risk
and the collapse rate
The collapse risk values were assigned according to
the ABC type (i.e., 6 categories) to verify the correlation between
the collapse risk and the collapse rate. The collapse risk was
noticeably correlated with the collapse rate (R=1; Table VI).
 | Table VI.Correlation between the risk of
collapse and the collapse rate. |
Table VI.
Correlation between the risk of
collapse and the collapse rate.
| Item | A | B | C | AB | BC | A-C |
|---|
| Risk value
(score) | 4 | 3 | 2 | 7 | 5 | 9 |
| Collapse rate
(%) | 50 | 9.5 | 0 | 74.1 | 52.4 | 88.6 |
Discussion
The CJFH typing method applied in the present study
is based on the three-pillar theory, considers the necrotic
location and the necrotic area (23), and its proposal has greatly increased
the accuracy of collapse prediction (30). However, this typing method has
certain limitations. First, in clinical practice, a relatively
large proportion of cases suffer from ONFH located in somewhat
anterior or posterior areas, therefore the medial plane is less
likely to reflect the actual necrotic state compared with the
maximal plane (33). Particularly,
for patients with a small necrotic area, the medial plane may not
even reveal the necrotic area (33).
In a previous study by our group, the mechanical distribution of
ONFH was analysed using the finite element method, indicating that
the most noticeable stress concentration was at the border between
the necrotic tissue and the normal tissue, where collapse was most
likely to occur (34). Based on our
experience, using the CT or MRI slice with the maximum ONFH area
for typing has higher practical significance in the clinical
judgement of the prognosis of ONFH. Furthermore, clinicians may
have diverse opinions regarding which CT/MRI slice should be used
as the image of the medial plane of the femoral head (35). As a consequence, selection errors may
occur. By contrast, the slice with the maximum necrotic area is
relatively definite on CT and on MRI, so it is easy to select and
convenient to use, which may increase the accuracy and
repeatability of the clinical application. Therefore, in the
present study, the CT or MRI slice with the maximum coronal
necrotic focus was used for ABC typing to predict the occurrence of
collapse in ONFH. In addition, CJFH typing fails to quantitate how
much of the lateral pillar must be intact to prevent the occurrence
of femoral collapse. Furthermore, CJFH typing does not cover all
ONFH conditions (e.g., when only the lateral pillar or the central
pillar is affected by necrosis), which further limits its clinical
application. Finally, although CJFH typing is based on the
three-pillar theory, it fails to specify detailed demarcation
criteria. In the present study, an ABC typing method was proposed
based on the mechanical distribution characteristics of the bone
trabeculae inside the femoral head, and a detailed approach that
provides criteria for the demarcation of the three-pillar structure
was applied.
The present study indicated that the proportions of
types A, B and C in ONFH were 0.9, 9.4 and 1.3%, respectively,
whereas the proportion of type A-C was as high as 66.8%; these
results indicate that ONFH involving only a single pillar is a rare
clinical phenomenon. By contrast, ONFH involving three pillars is
the most frequent clinical condition, followed by the involvement
of two pillars. The incidence of collapse in types A, B, C, AB, BC
and A-C was 50, 9.5, 0, 74.1, 52.4 and 88.6%, respectively, with an
order, from high to low, of A-C>AB>BC>A>B>C, and the
differences were significant. This result indicates that ABC typing
is able to determine the probability of collapse in ONFH with
different areas/extent of necrotic involvement, thereby offering
value in clinical application. In addition, the present study
indicated that the collapse rate of ONFH involving three pillars
was 88.6%, that of ONFH involving two pillars was 64.6% and that of
ONFH involving one pillar was 11.5%. ONFH involving the lateral
pillar had a collapse rate of 86.0%, which was significantly
different from that for ONFH without lateral pillar involvement.
These results suggest that the size of the necrotic area and
whether the lateral pillar is involved are influential factors
regarding the collapse of the osteonecrosis-affected femoral. In
the present study, the collapse rate of type C ONFH was 0%, and
collapse occurred in only two of the 21 hips (9.5%) with type B
ONFH, which suggests that collapse does not tend to occur in ONFH
with a small necrotic focus that involves only the medial or
central pillar. By contrast, the collapse rates of types A-C and AB
were as high as 88.6 and 74.1%, respectively, which suggests that
collapse is likely to occur in ONFH with a large necrotic size and
ONFH involving the lateral pillar. The present study further
analysed the correlation between the risk value (based on the
number of pillars involved and the involvement location) and the
collapse rate. The Spearman rank test revealed a significant
correlation (R=1), which indicates that ABC typing is
satisfactorily correlated with the collapse risk in ONFH and may be
utilized for prediction of collapse. This result was similar to
results based on JIC typing (19)
and CJFH typing (30). However, the
demarcation method for the three pillars according to the ABC
method proposed in the present study was based on biomechanical
theory, and this newly proposed typing method considers the
anatomical characteristics of the normal femoral head and the
stress distribution characteristics of the bone trabeculae inside
the femoral head; thus, the demarcation criteria for this typing
method are more specific, compared with JIC and CJFH typing.
Furthermore, the ABC typing method utilizes the plane with the
maximum necrotic area for typing, which is different from JIC and
CJFH, and can better reflect the actual ONFH status, thereby
increasing the accuracy of collapse prediction.
Of note, the present study has certain limitations.
First, it was a cross-sectional study, so the accuracy of collapse
prediction remains to be validated by prospective studies.
Furthermore, the ABC typing described in the present study only
considered the necrotic area and the necrotic location, and the
factor of bone remodelling ability after ONFH was excluded. This
exclusion was primarily due to the complexity of the typing issues
and for convenience in clinical practice. In any case, the
combination of these results with those of a previous study by our
group on the sclerotic rim (13) may
further increase the accuracy of collapse prediction in ONFH.
Finally, the sample size of the present study was small. To further
validate the accuracy of the ABC typing method in predicting the
collapse of the osteonecrosis-affected femoral, multicentric
prospective studies with larger sample sizes should be performed in
the future.
In conclusion, the ABC typing method applied in the
present study took the lesion size and location into account, and a
satisfactory correlation with the collapse risk in ONFH was
determined. The ABC method is easy to perform with reproducibility.
The significance of the proposal of this method lies in that the
typing outcomes help determine appropriate treatment protocols
according to the specific risk of collapse and goals of treatment.
In the ABC typing system, types A-C and AB had a poor prognosis,
whereas types B and C had a good prognosis, followed by types BC
and A, which suggests that the occurrence of collapse is associated
with the necrotic area: The larger the necrotic size, the higher
the risk of collapse. Furthermore, collapse occurrence is
associated with the necrotic location: The closer to the lateral
side of the femoral head, the higher the risk of collapse. The
co-existence of a large necrotic area and a lateral necrotic
location increases the collapse risk in ONFH. Based on the type
classification outcomes, the following is suggested: i) For type C
ONFH, special treatment is normally unnecessary as collapse is
generally unlikely to occur in this type, and regular follow-ups
are enough for patients with this condition. ii) Type B has a low
risk of collapse, so that for patients with this type of ONFH,
biological treatment (e.g., stem cell transplantation, circulation
improvement, medication for bone resorption inhibition and bone
formation promotion) may be selected as the major therapeutic
method in clinical practice, whereas lifestyle intervention
measures are not required. iii) The A and BC types have a
considerable risk of collapse, so for patients with these types of
ONFH, lifestyle intervention measures and non-supportive cancellous
bone transplantation, such as those for weight-bearing protection,
reduction of joint load and bone grafting impaction, are necessary
in addition to biological treatment. iv) The A-C and AB types have
a high risk of collapse, and for affected patients, appropriate
therapies for improving biomechanical support (e.g., osteotomy and
grafting of the fibula) are required to prevent the occurrence of
collapse, apart from biological treatment and lifestyle
intervention measures.
Acknowledgements
The authors would like to thank Prof. Fulei Chu from
the Department of Mechanical Engineering (Tsinghua University,
Beijing, China) for assistance in using Auto CAD software.
Funding
No funding was received.
Availability of data and materials
The analyzed data sets generated during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZZ and TY devised the study plan and led the writing
of the article. YuL, XK, and YaL conducted the experiment and
collected the data. SH, HD, and YB conducted the analysis. LX
supervised the whole process, and gave constructive advice and
final approval for the version to be published. The final version
of the manuscript has been read and approved by all authors, and
each author believes that the manuscript represents honest
work.
Ethical approval and consent to
participate
The present study was performed in accordance with
the Declaration of Helsinki. Approval was obtained from the Ethics
Committee of Guanganmen Hospital of the China Academy of Chinese
Medicine Sciences (Beijing, China). Written informed consent was
obtained from all participants.
Patient consent for publication
The patients provided written informed consent for
the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ONFH
|
osteonecrosis of the femoral head
|
|
ARCO
|
association research circulation
osseous
|
|
T1WI
|
T1-weighted imaging
|
References
|
1
|
Zhao DW and Hu YC: Chinese experts'
consensus on the diagnosis and treatment of osteonecrosis of the
femoral head in adults. Orthop Surg. 4:125–130. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Microsurgery Department of the Orthopedics
Branch of the Chinese Medical Doctor Association, : Group from the
Osteonecrosis and Bone Defect Branch of the Chinese Association of
Reparative and Reconstructive Surgery and Microsurgery and
Reconstructive Surgery Group of the Orthopedics Branch of the
Chinese Medical Association: Chinese Guideline for the diagnosis
and treatment of osteonecrosis of the femoral head in adults.
Orthop Surg. 9:3–12. 2017.PubMed/NCBI
|
|
3
|
Wang F and Zhang YH: Advances in research
on the cause and pathological mechanisms of non-traumatic ischemic
necrosis of femoral head. J Pract Diagnosis Ther. 2:121–123.
2007.(In Chinese).
|
|
4
|
Li ZR: Scientific diagnosis and treatment
of osteonecrosis of the femoral head. Chinese J Reparative
Reconstructive Surg. 9:685–686. 2005.
|
|
5
|
Floerkemeier T, Thorey F, Daentzer D,
Lerch M, Klages P, Windhagen H and von Lewinski G: Clinical and
radiological outcome of the treatment of osteonecrosis of the
femoral head using the osteonecrosis intervention implant. Int
Orthop. 35:489–495. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yu T, Zhang Z, Xie L, Ke X and Liu Y: The
influence of traditional Chinese medicine constitutions on the
potential repair capacity after osteonecrosis of the femoral head.
Complement Ther Med. 29:89–93. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Moya-Angeler J, Gianakos AL, Villa JC, Ni
A and Lane JM: Current concepts on osteonecrosis of the femoral
head. World J Orthop. 6:590–601. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mont MA, Cherian JJ, Sierra RJ, Jones LC
and Lieberman JR: Nontraumatic osteonecrosis of the femoral head:
Where do we stand today? A Ten-year update. J Bone Joint Surg Am.
97:1604–1627. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pierce TP, Elmallah RK, Jauregui JJ, Verna
DF and Mont MA: Outcomes of total hip arthroplasty in patients with
osteonecrosis of the femoral head-a current review. Curr Rev
Musculoskelet Med. 8:246–251. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rajpura A, Wright AC and Board TN: Medical
management of osteonecrosis of the hip: A review. Hip Int.
21:385–392. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gillet C, Dalla Valle A, Gaspard N, Spruyt
D, Vertongen P, Lechanteur J, Rigutto S, Dragan ER, Heuschling A,
Gangji V and Rasschaert J: Osteonecrosis of the Femoral head:
Lipotoxicity exacerbation in MSC and modifications of the bone
marrow fluid. Endocrinology. 158:490–502. 2017.PubMed/NCBI
|
|
12
|
Fukushima W, Fujioka M, Kubo T, Tamakoshi
A, Nagai M and Hirota Y: Nationwide epidemiologic survey of
idiopathic osteonecrosis of the femoral head. Clin Orthop Relat
Res. 468:2715–2724. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yu T, Xie L, Zhang Z, Ke X and Liu Y:
Prediction of osteonecrosis collapse of the femoral head based on
the proportion of the proximal sclerotic rim. Int Orthop.
39:1045–1050. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sugano N, Takaoka K, Ohzono K, Matsui M,
Masuhara K and Ono K: Prognostication of nontraumatic avascular
necrosis of the femoral head. Significance of location and size of
the necrotic lesion. Clin Orthop Relat Res. 303:155–164. 1994.
|
|
15
|
Morita D, Hasegawa Y, Okura T, Osawa Y and
Ishiguro N: Long-term outcomes of transtrochanteric rotational
osteotomy for non-traumatic osteonecrosis of the femoral head. Bone
Joint J. 99-B:1–183. 2017. View Article : Google Scholar
|
|
16
|
Koo KH and Kim R: Quantifying the extent
of osteonecrosis of the femoral head. A new method using MRI. J
Bone Joint Surg Br. 77:875–880. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nishii T, Sugano N, Ohzono K, Sakai T,
Sato Y and Yoshikawa H: Significance of lesion size and location in
the prediction of collapse of osteonecrosis of the femoral head: A
new three-dimensional quantification using magnetic resonance
imaging. J Orthop Res. 20:130–136. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kerboul M, Thomine J, Postel M and Merle
DR: The conservative surgical treatment of idiopathic aseptic
necrosis of the femoral head. J Bone Joint Surg Br. 56:291–296.
1974. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Min BW, Song KS, Cho CH, Lee SM and Lee
KJ: Untreated asymptomatic hips in patients with osteonecrosis of
the femoral head. Clin Orthop Relat Res. 466:1087–1092. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hernigou P and Lambotte JC: Volumetric
analysis of osteonecrosis of the femur. Anatomical correlation
using MRI. J Bone Joint Surg Br. 83:672–675. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gardeniers JWM: Report of the Committee of
Staging and Nomenclature. ARCO News Letter. 5(2): 79–82. 1993.
|
|
22
|
Steinberg ME, Hayken GD and Steinberg DR:
A quantitative system for staging avascular necrosis. J Bone Joint
Surg. 77:34–41. 1995. View Article : Google Scholar
|
|
23
|
Li ZR, Liu ZH, Sun W, Shi ZC, Wang BL and
Zhao FC: The classification of osteonecrosis of the femoral head
based on the three pillars structure: China-Japan Friendship
Hospital (CJFH) classification. Chin J Orthop. 6:515–520. 2012.(In
Chinese).
|
|
24
|
Li ZR: Osteonecrosis. The People's Health
Publishing House; Beijing: 2012, View Article : Google Scholar
|
|
25
|
Ahn AC and Grodzinsky AJ: Relevance of
collagen piezoelectricity to ‘Wolff's Law’: A critical review. Med
Eng Phys. 31:733–741. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tsubota K, Suzuki Y, Yamada T, Hojo M,
Makinouchi A and Adachi T: Computer simulation of trabecular
remodeling in human proximal femur using large-scale voxel FE
models: Approach to understanding Wolff's law. J Biomech.
42:1088–1094. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chen JH, Liu C and You L: Boning up on
Wolff's Law: Mechanical regulation of the cells that make and
maintain bone. J Biomech. 43:108–118. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ma XL, Li HT and Ma JX: Biomechanical
properties of principle compressive trabecular bone in proximal
femur. Biome Eng Clin Med. 2:118–122. 2012.(In Chinese).
|
|
29
|
Zhou GQ, Pang ZH, Chen QQ, He W, Chen ZQ,
Chen LL and Li ZQ: Reconstruction of the biomechanical transfer
path of femoral head necrosis: A subject-specific finite element
investigation. Comput Biol Med. 52:96–101. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Li Z, Sun W, Gao F, Liu Z, Shi Z and Wang
B: Comparative evaluation of osteonecrosis of the femoral head
classification: CJFH classification versus JIC classification. J
Hip Surg. 1:44–49. 2017. View Article : Google Scholar
|
|
31
|
Herring JA, Neustadt JB, Williams JJ,
Early JS and Browne RH: The lateral pillar classification of
Legg-Calvé-Perthes disease. J Pediatr Orthop. 12:143–150. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zhang ZN: 3S system-based typing for
osteonecrosis and its relation with Chinese medicine-based
constitution. Dissertation China Acad Chin Med Sci. 2015.(In
Chinese).
|
|
33
|
Zhang ZN, Xie LM and Yu T: Comparative
study on the differentiation of osteonecrosis of femoral head at
different sections based on three pillars structure. Chin J Tradit
Med Traumatol Orthop. 25:28–31. 2017.(In Chinese).
|
|
34
|
Yu T, Xie L and Chu F: A sclerotic rim
provides mechanical support for the femoral head in osteonecrosis.
Orthopedics. 38:e374–e379. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kim YM, Ahn JH, Kang HS and Kim HJ:
Estimation of the extent of osteonecrosis of the femoral head using
MRI. J Bone Joint Surg Br. 80:954–958. 1998. View Article : Google Scholar : PubMed/NCBI
|