Introduction
Acinetobacter baumannii is an opportunistic
pathogen that can cause a broad array of infections including
pneumonia, skin and soft tissue infection, meningitis, urinary
tract infection and blood stream infection, especially in
immunocompromised patients (1). This
ubiquitous organism can be detected in a wide range of
environments, including hospitals and other care facilities, and
can survive for a prolonged period of time on both biotic and
abiotic surfaces (2). A.
baumannii has been designated as a ‘red alert’ human pathogen
due to its extensive antimicrobial resistance (3). Bacterial strains can be classified as
multidrug-resistant (MDR), extensively drug-resistant (XDR) and
pandrug-resistant (PDR). XDR is defined as non-susceptibility to at
least one agent in all but two or fewer antimicrobial categories
(4). Therefore, treatment options
for XDR-A. baumannii infections are limited. When one agent
is routinely used in clinical practice, the susceptibility of A.
baumannii to this drug may markedly decrease (5,6). Given
unpredictable or suboptimal pharmacodynamics and concerns of
resistance emerging along with therapy, antimicrobial combinations
may provide improved treatment options (7). Therefore, a search for novel agents and
their efficient combinations is required. In the present study, the
in vitro antimicrobial activity of sitafloxacin, a new
fluoroquinolone, and the combined effect of sitafloxacin and
sulbactam were detected against clinical isolates of XDR-A.
baumannii.
Materials and methods
Bacterial isolates
XDR-A. baumannii strains were isolated from
clinical specimens collected in three tertiary hospitals affiliated
to Shandong University (Qilu Hospital, Jinan Central Hospital and
Shandong Provincial Qianfoshan Hospital; all in Jinan, China) from
November 2014 to December 2015. For patients from whom A.
baumannii strains were isolated more than once, only one strain
from each patient was included. VITEK® 2 microbial
analysis instruments were used to identify the XDR-A.
baumannii isolates (bioMérieux, Inc., Marcy l'Etoile, France).
The Kirby-Bauer method (8) was
applied to re-evaluate the strains to meet the criteria for
XDR-A. baumannii (4). As a
result, a total of 50 strains were included, of which 36 strains
were from sputum, 5 from lavages, 3 from blood, 3 from skin wounds
or surgical incisions of skin, 2 from cerebrospinal fluid and 1
from urine. ATCC 25922 and ATCC 27853 were used as quality controls
(American Type Culture Collection, Manassas, VA, USA). The Ethics
Committee of Qilu Hospital of Shandong University approved the
present study (approval no. KYLL-2017-612). All patients provided
written informed consent.
Broth microdilution assay
Mueller-Hinton (MH) powder was purchased from Thermo
Fisher Scientific, Inc. and dissolved according to the
manufacturer's protocol. Isolated colonies of A. baumannii
strains were maintained in 10 ml fresh MH broth and shaken in a
thermo-incubator at 37°C overnight. Suspensions with a turbidity
that matched the 0.5 McFarland standard [1.5×108
colony-forming unit (CFU)/ml] were further diluted to obtain the
final bacterial counts of 2–8×105 CFU/ml. Sitafloxacin
and sulbactam were obtained from Beijing Biodee Biotechnology Co.,
Ltd. (Beijing, China). To determine minimum inhibitory
concentration (MIC) values, broth microdilution method was carried
out as described in Clinical and Laboratory Standards Institute
(CLSI) guidelines (9).
Susceptibility was also determined for each isolate using these
criteria. The serially diluted drugs were at concentrations of 128,
64, 32, 16, 8, 4, 2, 1, 0.5, 0.25, 0.125 and 0 µg/ml. When MICs
were higher than 128 µg/ml, drug arrays of 256, 128, 64, 32, 16, 8,
4, 2, 1, 0.5, 0.25 and 0 µg/ml were further prepared. Following the
addition of bacterial suspensions, 96-well plates were incubated
overnight in ambient atmosphere at 37°C. MIC values were determined
by the concentrations of drugs at which bacterial growth was
visibly inhibited.
Microdilution checkerboard assay
Following determination of MICs of sulbactam and
sitafloxacin for each strain, another set of dilution series was
prepared for the two agents: 8X MIC, 4X MIC, 2X MIC, 1X MIC, 0.5X
MIC, 0.25X MIC, 0.125X MIC and 0 µg/ml. Sitafloxacin was added by
column, while sulbactam was added by row in 96-well plates.
Bacterial suspensions at concentrations of 2–8×105
CFU/ml were subsequently added and incubated overnight at 37°C.
Fractional inhibitory concentration index (FICI) values were
calculated as follows: FICI=MIC value of sulbactam combined with
sitafloxacin/MIC value of sulbactam applied alone + MIC value of
sitafloxacin combined with sulbactam/MIC value of sitafloxacin
applied alone. FICI values were interpreted as follows: ≤0.5,
synergy; >0.5 to <1, partial synergy; 1, addition; >1 to
<4, indifference; and ≥4, antagonism (10). The above steps were performed in
triplicate and average values were used as the final results. The
software we used in this study was Excel 2010 (Microsoft
Corporation, Redmond, WA, USA).
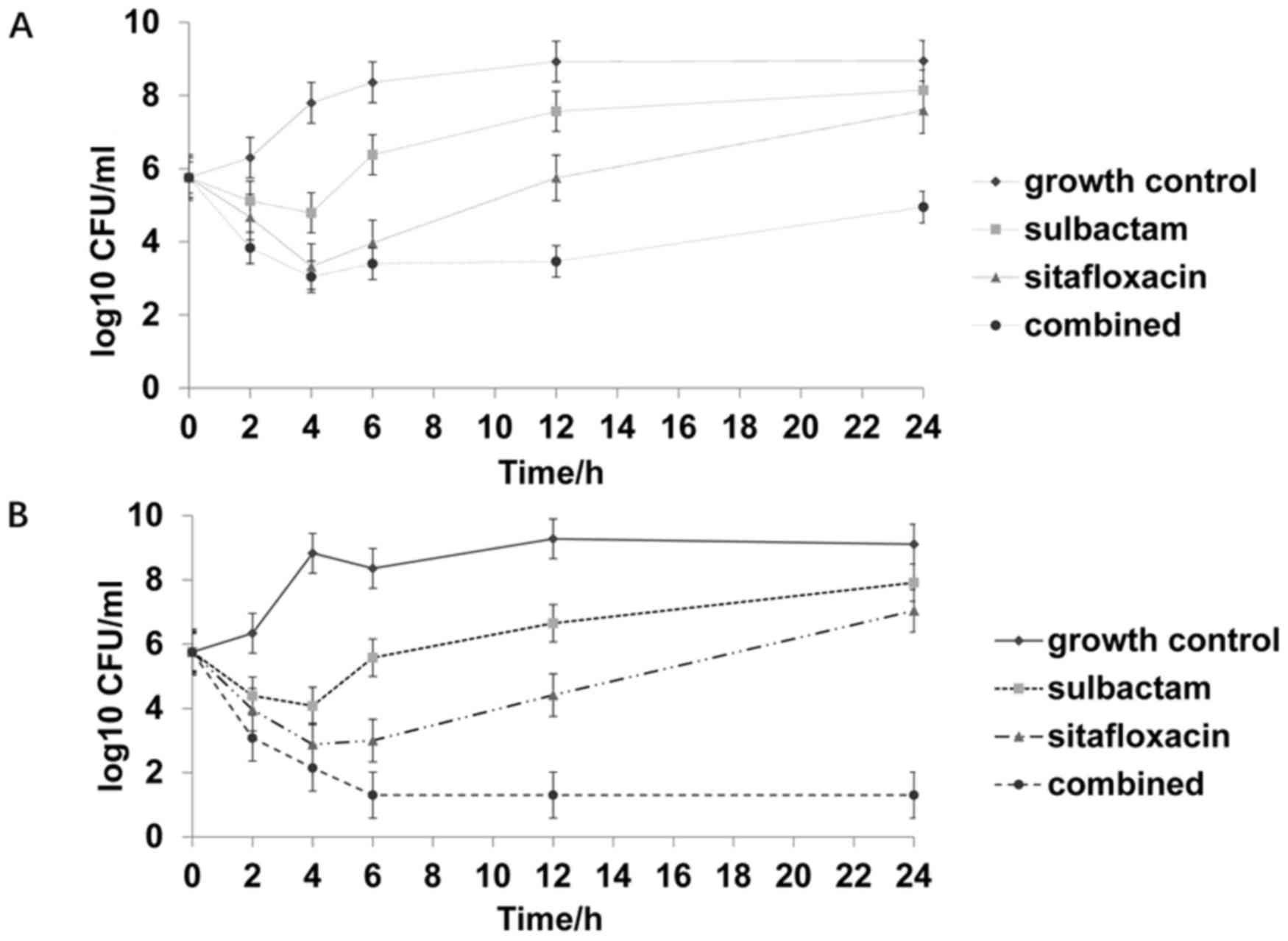
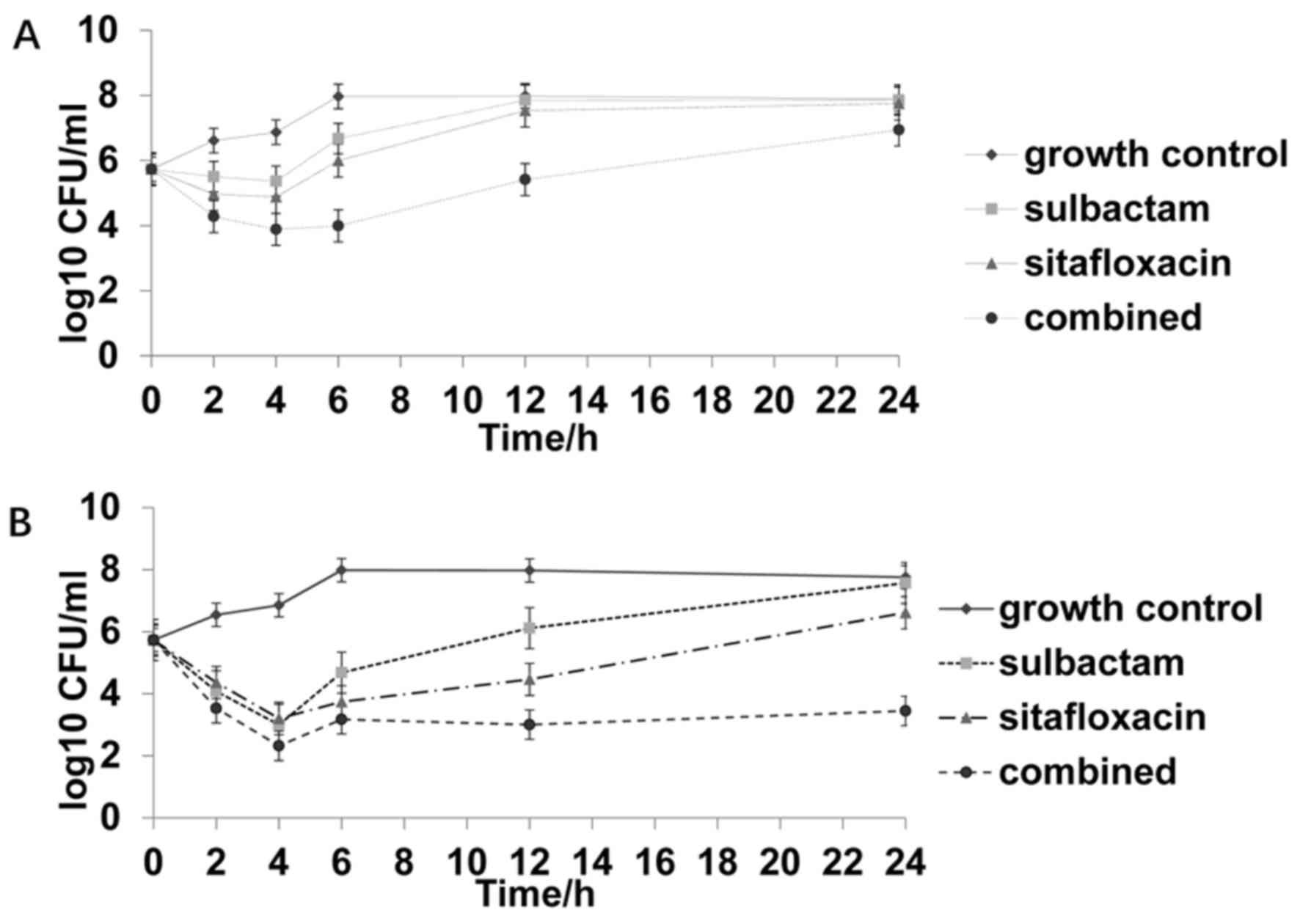
Time-kill assay
Time-kill assay was conducted for four
representative strains with different susceptibilities to
sitafloxacin and sulbactam. Bacterial suspensions were prepared
following the aforementioned steps and turbidity was adjusted
respectively. Thereafter, drugs alone or in combination were added
into the suspensions and incubated at 37°C. Time-kill curves for
individual or combined sulbactam and sitafloxacin were plotted at
0.5X MIC and 1X MIC, respectively. Drug concentrations were
selected according to MIC levels instead of a fixed concentration
and the four representative strains were different from each other
in their susceptibilities towards the two agents. 1X MIC were
chosen to guarantee the antimicrobial activity, while 0.5X MIC were
chosen to see whether synergistic effects could be achieved at
sub-MIC levels. Samples were removed at 0, 1, 2, 4, 6, 12 and 24 h.
Aliquots (100 µl) were serially diluted with cold and sterile PBS.
Bacterial counts were determined by plating three spots of 10 µl of
appropriate dilutions (1:100) on MH agar plates and incubation at
35°C for 18–24 h. Time-kill curves were subsequently constructed by
plotting the mean colony counts (log10 CFU/ml) vs time. The
bactericidal activities of drug combination were defined as a 3
log10 CFU/ml (99.9%) reduction compared with the most efficient
drug at 24 h. Synergy was defined as a 2 log10 CFU/ml decrease
between the combination and the most active agent alone at 24 h
(11). The drug combination was
considered to be antagonistic with a ≥2 log10 increase in counts.
In addition, the combination was considered to be indifferent if
there was a <2 log10 increase or decrease in colony count
compared with the most active drug alone. The experiment was
performed in duplicate to ensure reproducibility. The experiment
was continued for >24 h.
Results
Combined use of sitafloxacin and
sulbactam exhibits an increased inhibitory effect on XDR-A.
baumannii strains compared with the individual use of either
To test the effects of sitafloxacin and sulbactam
against the XDR-A. baumannii strains, MICs and
susceptibility rates were determined. Given that CLSI breakpoints
are not reported for sitafloxacin, CLSI breakpoints for other
fluoroquinolones were used to assess the susceptibility of
pathogens to sitafloxacin. Isolates with MICs of sitafloxacin ≤2
mg/l were provisionally considered to be susceptible to
sitafloxacin (12). CLSI breakpoints
were not available for the use of sulbactam alone, and, therefore,
breakpoints of ampicilin/sulbactam against Acinetobacter spp
(susceptible, ≤8/4 µg/ml; intermediate, 16/8 µg/ml; and resistant,
≥32/16 µg/ml) were used as interpretation criteria instead
(13). The data indicated that the
lowest concentration of the antibiotic at which 50% of the isolates
were inhibited (MIC50) and the lowest concentration of
the antibiotic at which 90% of the isolates were inhibited
(MIC90) for sitafloxacin decreased and the
susceptibility rates increased when the drug was combined with
sulbactam. Similarly, the MIC50 and MIC90 for
sulbactam decreased and the susceptibility rates increased when it
was combined with sitafloxacin (Table
I). MIC values were determined by the concentrations of drugs
at which bacterial growth was completely inhibited. The results
suggested that the combined use of sitafloxacin and sulbactam
exhibited a greater inhibitory effect on XDR-A. baumannii
strains compared with the individual use of either.
 | Table I.MIC values of sitafloxacin and
sulbactam against XDR-A. baumannii isolates. |
Table I.
MIC values of sitafloxacin and
sulbactam against XDR-A. baumannii isolates.
| Antimicrobial
agent | MIC range
(µg/ml) | MIC50
(µg/ml) | MIC90
(µg/ml) | Rate of
susceptibility (%) |
|---|
| Sitafloxacin |
|
|
|
|
|
Alone | 0.125–16 | 1 | 2 | 92 |
|
Combined | 0.016–8 | 0.5 | 2 | 96 |
| Sulbactam |
|
|
|
|
|
Alone | 2–256 | 32 | 64 | 16 |
|
Combined | 0.016–64 | 8 | 32 | 48 |
Sitafloxacin and sulbactam induce a
synergistic or partial synergistic effect on the majority of the 50
strains
To further examine the inhibitory effect of
sitafloxacin and sulbactam against XDR-A. baumannii strains,
FICI was calculated. The data indicated that sitafloxacin and
sulbactam induced a synergistic effect in 16% of the 50 strains. In
addition, sitafloxacin and sulbactam induced a partial synergistic
effect on 50% of the 50 strains. Importantly, sitafloxacin and
sulbactam exhibited no antagonistic effect on any strain (Table II). The results indicated that
sitafloxacin and sulbactam exhibited synergistic or partial
synergistic effects on the majority of the 50 strains.
 | Table II.Distribution of FICI values for the
combination of sitafloxacin and sulbactam against XDR-A.
baumannii isolates. |
Table II.
Distribution of FICI values for the
combination of sitafloxacin and sulbactam against XDR-A.
baumannii isolates.
|
Sulbactam/sitafloxacin | Synergy (FICI
≤0.5) | Partial synergy
(FICI 0.5–1) | Addition (FICI
1) | Indifference (FICI
1–4) | Antagonism (FICI
≥4) |
|---|
| Number of
isolates | 8 | 25 | 8 | 9 | 0 |
| Rate | 16% | 50% | 16% | 18% | 0 |
Majority of the 50 isolates are not
susceptible to sulbactam and are susceptible to sitafloxacin
According to the susceptibility status of the 50
isolates to sulbactam and sitafloxacin, they were divided into the
following four groups: i) Susceptible to both sulbactam and
sitafloxacin (SS); ii) non-susceptible to sulbactam and susceptible
to sitafloxacin (NS); iii) susceptible to sulbactam and
non-susceptible to sitafloxacin (SN); and iv) non-susceptible to
either sulbactam or sitafloxacin (NN). The data indicated that
isolates in the SS group accounted for 14% of all strains, those in
the NS group accounted for 78%, those in the SN group accounted for
2% and those in the NN group accounted for 6% (Table III). The results suggested that the
majority of the 50 isolates were not susceptible to sulbactam and
were susceptible to sitafloxacin.
 | Table III.Distribution of strains susceptible
and non-susceptible to sitafloxacin and sulbactam. |
Table III.
Distribution of strains susceptible
and non-susceptible to sitafloxacin and sulbactam.
|
| Sulbactam |
|---|
|
|
|
|---|
| Number of
isolates | Susceptible |
Non-susceptible |
|---|
| Sitafloxacin |
|
|
|
Susceptible | 7 (14%) | 39 (78%) |
|
Non-susceptible | 1 (2%) | 3 (6%) |
Combined use of sitafloxacin and
sulbactam at the concentration of 1X MIC exhibits bactericidal
activity against all four isolates at 24 h, and synergistic effect
on the four selected isolates
To conduct the time-kill studies, four
representative strains were randomly selected from the four groups
shown in Table III, respectively.
Sulbactam and sitafloxacin displayed a synergistic effect on the
strain selected from the SS group, with a FICI value of 0.375.
Sulbactam and sitafloxacin had FICI values of 0.75 and 0.675 for
strains selected from the NS and SN groups, respectively.
Furthermore, sulbactam and sitafloxacin had an FICI value of 1.5
for the strain selected from the NN group. Time-kill curves for
individual or combined use of sulbactam and sitafloxacin were
plotted at 0.5X MIC and 1X MIC, respectively. Time-kill assays
indicated that sitafloxacin exhibited a rapid bacteriostatic effect
at the concentration of 1X MIC, regardless of the susceptibility
status of the four isolates. Combined use of sitafloxacin and
sulbactam at the concentration of 0.5X MIC exhibited a bactericidal
effect for the strains from the SS and NS groups, and synergistic
effect for all strains but that from NN group. Furthermore,
combined use of sitafloxacin and sulbactam at the concentration of
1X MIC exhibited bactericidal activity, and synergistic effect
against all four isolates at 24 h regardless of the susceptibility
status (Figs. 1–4; Table
IV). Combined use of sitafloxacin and sulbactam at the
concentration of 1X MIC completely removed the strains from SS and
NS groups with no regrowth after 24 h.
 | Table IV.Results of time-kill assay for the
four strains under different drug concentrations. |
Table IV.
Results of time-kill assay for the
four strains under different drug concentrations.
| Results | Strains under a
drug concentration of 0.5X MIC | Strains under a
drug concentration of 1X MIC |
|---|
| Bactericidal
activities |
| SS, NS, SN, NN |
| Synergy | SS, NS, SN |
|
| Indifferent | NN |
|
Discussion
A. baumannii is one of the most common causes
of nosocomial infection in Asia (8).
The risk factors of A. baumannii infection include long stay
in hospital or intensive care unit, mechanical ventilation,
invasive operation, antibiotic exposure, multiple infections,
diabetes and COPD (14). A.
baumannii can form biofilms, which can survive in various
implants (catheterization, endotracheal intubation and deep vein
catheterization) for a long time (15). Patients often merge with basic
diseases, multiple infections or invasive operations. Their
immunity is weak and requires longer treatment time compared with
other infectious diseases. Therefore, the clinical treatment of
A. baumannii infection is usually longer. Chinese experts
recommend combination therapy for the treatment of drug resistant
A. baumannii (16). This
pathogen harbors multiple resistance mechanisms and reduces
therapeutic choices to a limited set of active antibiotics
(16). With the rise of MDR, XDR and
PDR strains globally (17–20), there is a requirement for the
development of safe and effective therapeutic strategies.
Fluoroquinolones have a broad-spectrum antimicrobial activity and
are commonly used in clinical practice (21). At present, the majority of nosocomial
isolates of A. baumannii are resistant to fluoroquinolones
(22–24), and, therefore, fluoroquinolones are
not ideal for the empirical treatment of A.
baumannii-associated infections. A new fluoroquinolone
antibiotic, sitafloxacin, has demonstrated a good in vitro
activity against pathogens that are resistant to other
fluoroquinolones (25,26). Sitafloxacin has been reported to
exhibit acceptable antimicrobial effects against
carbapenem-resistant A. baumannii and the respective
susceptibility rates were 91.4 and 58.9% according to two separate
reports (12,27). Sulbactam exhibits affinities for
penicillin-binding proteins and inhibits bacterial cell wall
synthesis (28,29). Sulbactam is active against A.
baumannii and has been clinically used for infections caused by
this organism (30). In addition,
sulbactam exhibits synergistic effects with other antibiotics
(31).
In the present study, sitafloxacin induced a
promising antimicrobial activity against XDR-A. baumannii
with a susceptibility rate of 92%. Furthermore, combined use of
sitafloxacin with sulbactam resulted in a susceptibility rate of
96%. Sitafloxacin and sulbactam exhibited synergistic effects in
16% of the 50 strains. In addition, sitafloxacin and sulbactam have
shown partial synergistic effect on 50% of strains. None of the
strains exhibited antagonistic effects. However, Odds (32) proposed alternative criteria for
interpretation of FICI values. The authors suggested that
researchers submitting research articles containing FICI data
should interpret synergy as FICI ≤0.5, antagonism as FICI >4.0
and no interaction as FICI >0.5–4.0. Additionally, these authors
argued that their proposed criteria would encourage conservative
interpretation of results (32).
According to the suggestions by Odds (32), sitafloxacin and sulbactam exhibited
no interaction in 84% of XDR-A. baumannii strains included
in the present study. The time-kill assay was performed to further
investigate the bactericidal activity of the two drugs and their
combination (33,34).
Time-kill assays performed in the present study
indicated that sitafloxacin induced a rapid bacteriostatic effect
at the concentration of 1X MIC, regardless of the susceptibility
status of the four isolates. Combined use of sitafloxacin and
sulbactam at the concentration of 0.5X MIC only exhibited
bactericidal effects for the strains susceptible to sitafloxacin.
In addition, combined use of sitafloxacin and sulbactam at the
concentration of 1X MIC exhibited bactericidal activity against all
four isolates at 24 h. The strains from the SS and NS groups were
completely removed with no regrowth after 24 h when sitafloxacin
and sulbactam are combined at the concentration of 1X MIC. Combined
use of sitafloxacin and sulbactam at the concentration of 0.5X MIC
exhibited a synergistic effect for all strains except for the NN
group strain. In addition, synergistic effect was achieved for all
four isolates, regardless of the susceptibility status, when both
drugs are used at the concentration of 1X MIC. The results of the
present study indicated that the combination of sitafloxacin and
sulbactam was more efficient at eliminating isolates that were
susceptible to sitafloxacin compared with isolates that were
non-susceptible to sitafloxacin.
Sitafloxacin and sulbactam combination could be a
promising alternative treatment for XDR- A. baumannii
infection. However, in vitro experimental results do not
necessarily correspond with clinical efficacy (35), which may be the result of the
metabolism of the agents and the discordant redistribution of
different agents in target tissues (24). Still, in vitro experiments
provide a convenient way to screen compounds to propose
combinations that could be synergistic in vivo.
In conclusion, the present study indicated that
sulbactam enhanced the bactericidal activity of sitafloxacin and
this combination revealed synergistic or partial synergistic effect
in the majority of cases. For strains that were non-susceptible to
sitafloxacin, the bactericidal activities of the combination of
sitafloxacin and sulbactam were impaired at a concentration that is
lower than its MIC. However, this impairment was overcome by
increasing the concentration to 1X MIC. In future investigations,
insights should be gained into the clinical impact of the
combination of sitafloxacin and sulbactam, and the possible
benefits associated with the application of this combination.
Acknowledgements
The authors wish to thank their department and
research team for their help and dedication.
Funding
The present study was supported by the 2015
Scientific Medicine Development Fund of Shandong Province (grant
no. 2015WS0290).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
The final version of the manuscript has been read
and approved by all authors, and each author believes that the
manuscript represents honest work. NX, GW and QX collaborated to
design the study. NX, GW, YL, XD and FC were responsible for
performing experiments. NX, GW and YL analyzed the data. All
authors collaborated to interpret results and develop the
manuscript.
Ethics approval and consent to
participate
All procedures performed in the current study were
approved by the Ethics Committee of Shandong University (Jinan,
China). Written informed consent was obtained from all patients or
their families.
Patient consent for publication
Written informed consents for publication of any
associated data and accompanying images were obtained from all
patients or their parents, guardians or next of kin.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lee K, Yong D, Jeong SH and Chong Y:
Multidrug-resistant acinetobacter spp.: Increasingly problematic
nosocomial pathogens. Yonsei Med J. 52:879–891. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Peleg AY, Seifert H and Paterson DL:
Acinetobacter baumannii: Emergence of a successful pathogen. Clin
Microbiol Rev. 21:538–582. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cerqueira GM and Peleg AY: Insights into
Acinetobacter baumannii pathogenicity. IUBMB Life. 63:1055–1060.
2011. View
Article : Google Scholar : PubMed/NCBI
|
|
4
|
Magiorakos AP, Srinivasan A, Carey RB,
Carmeli Y, Falagas ME, Giske CG, Harbarth S, Hindler JF, Kahlmeter
G, Olsson-Liljequist B, et al: Multidrug-resistant, extensively
drug-resistant and pandrug-resistant bacteria: An international
expert proposal for interim standard definitions for acquired
resistance. Clin Microbiol Infect. 18:268–281. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Corbella X, Montero A, Pujol M, Domínguez
MA, Ayats J, Argerich MJ, Garrigosa F, Ariza J and Gudiol F:
Emergence and rapid spread of carbapenem resistance during a large
and sustained hospital outbreak of multiresistant Acinetobacter
baumannii. J Clin Microbiol. 38:4086–4095. 2000.PubMed/NCBI
|
|
6
|
Viehman JA, Nguyen MH and Doi Y: Treatment
options for carbapenem-resistant and extensively drug-resistant
Acinetobacter baumannii infections. Drugs. 74:1315–1333. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chen Q, Li X, Zhou H, Jiang Y, Chen Y, Hua
X and Yu Y: Decreased susceptibility to tigecycline in
Acinetobacter baumannii mediated by a mutation in trm encoding
sam-dependent methyltransferase. J Antimicrob Chemother. 69:72–76.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Clinical and Laboratory Standards
Institute, . Performance Standards for Antimicrobial Susceptibility
Testing; Twenty-Fifth Informational Supplement. CLSI document
M100-S25. Clinical and Laboratory Standards Institute; Wayne, PA:
2015
|
|
9
|
Sader HS, Flamm RK and Jones RN:
Antimicrobial activity of daptomycin tested against gram-positive
pathogens collected in europe, latin america, and selected
countries in the asia-pacific region (2011). Diagn Microbiol Infect
Dis. 75:417–422. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ji J, Du X, Chen Y, Fu Y, Wang H and Yu Y:
In vitro activity of sulbactam in combination with imipenem,
meropenem, panipenem or cefoperazone against clinical isolates of
Acinetobacter baumannii. Int J Antimicrob Agents. 41:400–401. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Vidaillac C, Benichou L and Duval RE: In
vitro synergy of colistin combinations against colistin-resistant
Acinetobacter baumanniiPseudomonas aeruginosa, and klebsiella
pneumoniae isolates. Antimicrob Agents Chemother. 56:4856–4861.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Huang YS, Wang JT, Sheng WH, Chuang YC and
Chang SC: Comparative in vitro activity of sitafloxacin against
bacteremic isolates of carbapenem resistant Acinetobacter baumannii
complex. J Microbiol Immunol Infect. 48:545–551. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chung DR, Song JH, Kim SH, Thamlikitkul V,
Huang SG, Wang H, So TM, Yasin RM, Hsueh PR, Carlos CC, et al: High
prevalence of multidrug-resistant nonfermenters in
hospital-acquired pneumonia in asia. Am J Respir Crit Care Med.
184:1409–1417. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Munoz-price LS and Weinstein RA:
Acinetobacter infection. N Engl J Med. 358:1271–1281. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Djeribi R, Bouchloukh W, Jouenne T and
Menaa B: Characterization of bacterial biofilms formed on urinary
catheters. Am J Infect Control. 40:854–859. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Doi Y, Murray GL and Peleg AY:
Acinetobacter baumannii: Evolution of antimicrobial resistance -
treatment options. Semin Respir Crit Care Med. 36:85–98. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Dijkshoorn L, Nemec A and Seifert H: An
increasing threat in hospitals: Multidrug-resistant Acinetobacter
baumannii. Nat Rev Microbiol. 5:939–951. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Potron A, Poirel L and Nordmann P:
Emerging broad-spectrum resistance in Pseudomonas aeruginosa and
Acinetobacter baumannii Mechanisms and epidemiology. Int J
Antimicrob Agents. 45:568–585. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Göttig S, Gruber TM, Higgins PG, Wachsmuth
M, Seifert H and Kempf VA: Detection of pan drug-resistant
Acinetobacter baumannii in germany. J Antimicrob Chemother.
69:2578–2579. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Karah N, Haldorsen B, Hermansen NO, Tveten
Y, Ragnhildstveit E, Skutlaberg DH, Tofteland S, Sundsfjord A and
Samuelsen Ø: Emergence of OXA-carbapenemase- and 16S rRNA
methylase-producing international clones of Acinetobacter baumannii
in norway. J Med Microbiol. 60:515–521. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sharma PC, Jain A and Jain S:
Fluoroquinolone antibacterials: A review on chemistry, microbiology
and therapeutic prospects. Acta Pol Pharm. 66:587–604.
2009.PubMed/NCBI
|
|
22
|
Krzyściak P, Chmielarczyk A, Pobiega M,
Romaniszyn D and Wójkowska-Mach J: Acinetobacter baumannii isolated
from hospital-acquired infection: Biofilm production and drug
susceptibility. APMIS. 125:1017–1026. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Saroj SD, Clemmer KM, Bonomo RA and Rather
PN: Novel mechanism for fluoroquinolone resistance in Acinetobacter
baumannii. Antimicrob Agents Chemother. 56:4955–4957. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Grochowalska A, Kozioå-Montewka M and
Sobieszczańska A: Analysis of Acinetobacter baumannii resistance
patterns in patients with chronic obstructive pulmonary disease
(copd) in terms of choice of effective empiric antibiotic therapy.
Ann Agric Environ Med. 24:307–311. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Keating GM: Sitafloxacin: In bacterial
infections. Drugs. 71:731–744. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Deguchi T, Yasuda M, Kawamura T, Nakano M,
Ozeki S, Kanematsu E, Nishino Y and Kawada Y: Improved
antimicrobial activity of DU-6859a, a new fluoroquinolone, against
quinolone-resistant klebsiella pneumoniae and enterobacter cloacae
isolates with alterations in GyrA and ParC proteins. Antimicrob
Agents Chemother. 41:2544–2546. 1997.PubMed/NCBI
|
|
27
|
Thamlikitkul V and Tiengrim S: In vitro
activity of sitafloxacin against carbapenem-resistant Acinetobacter
baumannii. Int J Antimicrob Agents. 42:284–285. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Rafailidis PI, Ioannidou EN and Falagas
ME: Ampicillin/sulbactam: Current status in severe bacterial
infections. Drugs. 67:1829–1849. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Penwell WF, Shapiro AB, Giacobbe RA, Gu
RF, Gao N, Thresher J, McLaughlin RE, Huband MD, DeJonge BL, Ehmann
DE and Miller AA: Molecular mechanisms of sulbactam antibacterial
activity and resistance determinants in Acinetobacter baumannii.
Antimicrob Agents Chemother. 59:1680–1689. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Urban C, Go E, Mariano N and Rahal JJ:
Interaction of sulbactam, clavulanic acid and tazobactam with
penicillin-binding proteins of imipenem-resistant and -susceptible
acinetobacter baumannii. FEMS Microbiol Lett. 125:193–197. 1995.
View Article : Google Scholar
|
|
31
|
Poulikakos P, Tansarli GS and Falagas ME:
Combination antibiotic treatment versus monotherapy for
multidrug-resistant, extensively drug-resistant, and
pandrug-resistant acinetobacter infections: A systematic review.
Eur J Clin Microbiol Infect Dis. 33:1675–1685. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Odds FC: Synergy, antagonism, and what the
chequerboard puts between them. J Antimicrob Chemother. 52:12003.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Nageeb W, Metwally L, Kamel M and Zakaria
S: In vitro antimicrobial synergy studies of carbapenem-resistant
Acinetobacter baumannii isolated from intensive care units of a
tertiary care hospital in egypt. J Infect Public Health. 8:593–602.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Phee LM, Betts JW, Bharathan B and Wareham
DW: Colistin and fusidic acid, a novel potent synergistic
combination for treatment of multidrug-resistant Acinetobacter
baumannii infections. Antimicrob Agents Chemother. 59:4544–4550.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Simsek F, Gedik H, Yildirmak MT, Iris NE,
Türkmen A, Ersoy A, Ersöz M and Gücüyener A: Colistin against
colistin-only-susceptible Acinetobacter baumannii-related
infections: Monotherapy or combination therapy? Indian J Med
Microbiol. 30:448–452. 2012. View Article : Google Scholar : PubMed/NCBI
|