Introduction
With the growth of aging population, incidence of
hip joint disease shows an increasing trend. Artificial hip
replacement is a type of reconstructive operation that replaces the
partial or integral damaged hip joint by adopting joint prosthesis
fabricated by artificial simulation to ameliorate and restore the
function of the hip joint, and is one of the major methods in the
treatment of joint diseases in recent years (1–3).
Glutathione S transferases (GSTs) are an important
family of phase II metabolic enzymes in the human body, and family
members include GSTM1, GSTT1, and GSTP1 (4,5). A
previous study (6), showed that GSTs
can catalyze the sulfhydryl group of reduced glutathione to react
the electrophilic compound to increase their water solubility for
excretion, so as to play an important role in detoxification of
carcinogens and metabolism of anticancer drugs. Genetic
polymorphisms of GSTs can alter enzyme activity, thus increasing
the risk of various diseases (6). A
previous study (7) has shown that
the missing genotypes of GSTM1 and GSTT1 can lead to loss of
function of their encoded enzymes. Alteration of A313G (Ile105Val)
on exon 5 of GSTP1 (rs1695) results in decreased thermal stability
and reduced specific catalytic activity of the encoded protein.
Changes in the polymorphisms of the three genes can affect the
metabolism of chemotherapeutic drugs by the cells, resulting in
differences in the effective plasma concentrations of
chemotherapeutic agents, which ultimately leads to differences in
efficacy, toxicity, and prognosis of chemotherapy (8). Currently, GSTs gene polymorphism has
attracted more and more attentions. Previous studies have shown
that glutathione S-transferase M1 (GSTM1) deletion may lead to the
occurrence of some malignant tumors, such as lung cancer (9), liver cancer (10), gastric cancer (11) and nasopharyngeal carcinoma (12) and other tumors. A previous study
(13), has reported that GSTs gene
polymorphisms may lead to reduced antioxidant activity of enzymes,
leading to increased susceptibility to diabetes. Another study
showed that infection rate of diabetic patients is 3 times higher
than that of non-diabetic patients after artificial hip replacement
(14). However, the correlations
between GSTM1 gene deletion and artificial hip replacement are
still controversial. Hence, the present study investigated the
correlation between GSTM1 gene deletion and recovery of patients
undergoing artificial hip replacement.
Materials and methods
Basic data
A total of 241 patients who received artificial hip
replacement in People's Hospital of Rizhao from December 2010 to
October 2016 were enrolled to serve as observation group. Those
patients included 149 males (61.8%) and 92 (38.9%) females, and the
mean age was 65±9.41 years. Eighty healthy people who at the same
period took physical examination in our hospital were selected to
serve as control group. Control group included 41 males (51.25%)
and 39 females (48.75%). There were no statistically significant
differences in sex, age, hypertension, diabetes and smoking history
between two groups (P>0.05) (Table
I). Harris scoring (15), which
includes seven indexes: Pain (44 points), daily activity (14
points), gait (11 points), walking aid (11 points), walking
distance (11 points), deformity (4 points) and the degree of
activity (5 points) was performed with a total of 100 points. Four
grades were set based on the total scores: 100-90, excellent;
89–80, good; 79–70, fair; <70, poor. All participants and their
families signed informed consent. This study was approved by the
Ethics Committee of People's Hospital of Rizhao (Shandong,
China).
 | Table I.Basic data of two groups. |
Table I.
Basic data of two groups.
| Factor | Experimental group
(%) | Control group
(%) | OR (95% CI) | χ2 | P-value |
|---|
| Sex |
|
|
|
|
|
| Male | 149 (61.8) | 41 (51.25) | 1.51 (1.12–4.94) | 0.814 | 0.574 |
|
Female | 92 (38.9) | 39 (48.75) |
|
|
|
| Age (years) |
|
|
|
|
|
| ≥65 | 107 (44.39) | 37 (46.25) | 2.41 (1.71–3.44) | 6.74 | 0.749 |
|
<60 | 134 (55.61) | 43 (53.75) |
|
|
|
| Hypertension |
|
|
|
|
|
| Yes | 170 (70.53) | 33 (41.25) |
|
|
|
| No | 71 (29.47) | 47 (58.75) |
|
|
|
| Diabetes |
|
|
|
|
|
| Yes | 96 (39.83) | 29 (36.25) | 1.88 (1.08–2.98) | 5.41 | 0.766 |
| No | 145 (60.17) | 51 (63.75) |
|
|
|
| Smoking history |
|
|
|
|
|
| Yes | 162 (67.21) | 41 (51.25) | 2.87 (1.74–3.04) | 10.55 | 0.648 |
| No | 79 (32.79) | 39 (48.75) |
|
|
|
| White blood cells
(10×9/l) | 4.49±1.5 | 4.1±1.7 |
| 1.948 | 0.052 |
| Hemoglobin (g/l) | 162.5±26.40 | 169.6±33.00 |
| 1.485 | 0.138 |
| Platelets
(10×9/l) | 132.0±25.14 | 138.0±25.20 |
| 1.849 | 0.065 |
| BMI index
(kg/m3) | 22.51±1.30 | 22.78±1.15 |
| 1.655 | 0.099 |
Instrument and reagents
TRIzol reagent and PCR 2X Taq MasterMix kit was
purchased from Invitrogen; Thermo Fisher Scientific, Inc. (Waltham,
MA, USA). DNA Marker was purchased from Sigma-Aldrich; Merck KGaA
(Darmstadt, Germany). Roche light cycle 480 was purchased from
Roche Diagnostics (Basel, Switzerland).
Follow-up
Patients were followed up once every month within
the first three months after operation, followed by once every
three months for nine months. Hospitalization time, the length of
the use of antibiotics and the condition of infection were analyzed
in deletion group and non-deletion group were recorded. After
discharge from hospital, the patient continued to receive
antithrombotic therapy, such as oral coumarin or aspirin, and the
corresponding training, such as the constriction exercise of the
affected limb, the continuous passive exercise, the training of
joint motion, walking practice and stairs exercises were used to
prevent postoperative complications.
Exclusion and inclusion criteria
Inclusion criteria: Patients received no hormone
drug treatments; patients with normal liver and kidney function;
patients willing to cooperate with researchers. Exclusion: Patients
with rheumatism, rheumatoid arthritis or gonarthritis; patients
with mental illness or physical disability; patients who were not
willing to receive treatment.
Collection of specimens and extraction
of total ribonucleic acid (RNA)
Three milliliters synovial fluid was collected and
transferred into a centrifuge tube, followed by centrifugation at
2,500 × g at 4°C for 10 min. Subsequently, the supernatant was
transferred to a Eppendorf (EP) tube and restored at −80°C. DNA was
extracted according to the instructions of kit, followed by
reservation at −20°C.
Single nucleotide polymorphism
sequencing
GSTM1 genotyping was performed by polymerase chain
reaction-restriction fragment length polymorphism (PCR-RFLP) with
β-globin as the endogenous control. Primer sequence of GSTM1 gene
were: 5′-TACTCAGAGTTTCTGGGGAAGCGGC-3′ (forward) and
5′-ACGGTGGAGGTCAAGGACATCATAG-3′ (reverse); Primer sequences of
endogenous control β-globin were: 5′-GAACCCCAGGGTACAGAGAAAGATC-3′
(forward) and 5′-GGACGAAGGAAGAGTGTCGGAAG-3′ (reverse). PCR reaction
system was 25 µl: 2 µl DNA template, 0.5 mol/l primer, 2×2.0 µl
deoxy-ribonucleoside triphosphate (dNTP), 2.5 µl buffer, 1.5 mol/l
MgCl2 and 1.0 IU TaqDNA. PCR reaction conditions were:
Pre-denaturation at 94°C for 2 min, followed by 35 cycles of 94°C
for 45 sec, 55°C for 50 sec and 72°C for 50 sec, and 72°C for 5
min. Finally, 10 ul PCR product was subjected to electrophoresis by
using 1.5% agarose gel for 45 min, followed by staining with 1.5%
ethidium bromide (EB).
Statistical analysis
Data obtained in the present study were analyzed by
using Statistical Product and Service Solutions (SPSS, Inc.,
Chicago, IL, USA) v.17.0 statistical software. Enumeration data
were compared by Chi-square test. Measurement data were expressed
by mean ± SD. t-test was used for the comparisons between deletion
and non-deletion groups. P<0.05 was considered to indicate a
statistically significant difference.
Results
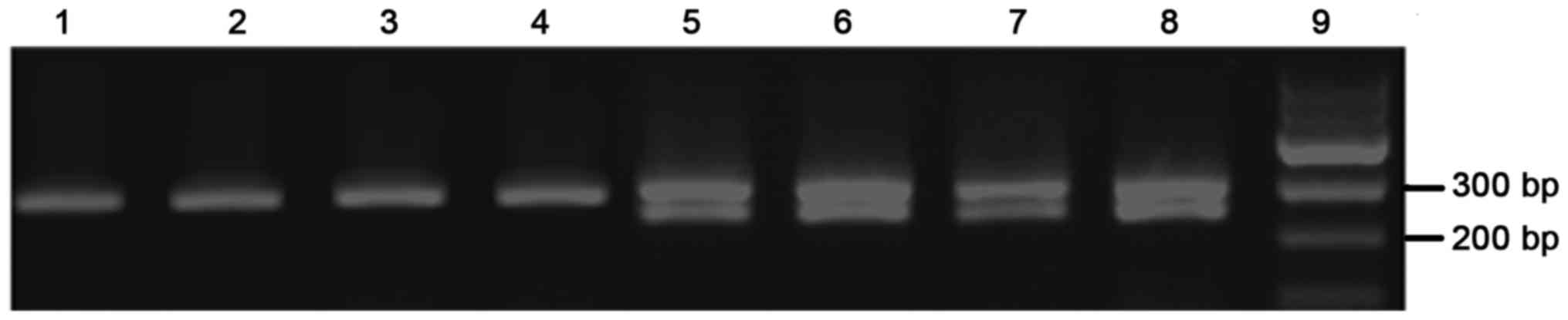
PCR amplification results
Multiplex PCR amplification of GSTM1 was carried to
obtain products with a length of 298, 248 and 207 bp. GSTMl (−)
genotype only showed a band of 298 bp, while GSTM1 (+) showed two
bands after electrophoresis (Fig.
1).
GSTM1 gene polymorphism and recovery
of patients undergoing artificial hip replacement
In the present study, there were 241 patients with
artificial hip joint replacement. Giscontinuous chi-square test
showed that GSTM1 gene deletion type in observation group (67.63%)
was higher than that in control group (41.25%), suggesting that
deletion of GSTM1 gene is related to the poor recovery of patients
undergoing artificial hip replacement (OR=1.51, 95% CI:
1.075–2.023, P<0.05; Table
II).
 | Table II.GSTM1 gene polymorphism and recovery
of patients undergoing artificial hip replacement. |
Table II.
GSTM1 gene polymorphism and recovery
of patients undergoing artificial hip replacement.
| Genotype | Experimental group,
n=241 (%) | Control group, n=80
(%) | OR (95% CI) | χ2 | P-value |
|---|
| GSTM1 |
|
|
|
|
|
| GSTM1
(+) | 78
(32.37) | 47 (58.75) | – |
|
|
| GSTM1
(−) | 163 (67.63) | 33 (41.25) | 1.51
(1.075–2.023) | 0.743 | <0.05 |
Comparison of clinical data between
deletion group and non-deletion group in experimental group
Patients were divided into GSTM1-deletion and
non-GSTM1-deletion groups. we found that there was no difference in
sex, age, hypertension, smoking history, leukocyte, hemoglobin,
platelet, and BMI index between patients in deletion and
non-deletion groups (P>0.05), The number of patients with
diabetes in GSTM1-deletion was more than that in non-GSTM1-deletion
group (P<0.05; Table III).
 | Table III.Comparison of clinical data between
deletion group and non-deletion group in experimental group. |
Table III.
Comparison of clinical data between
deletion group and non-deletion group in experimental group.
| Variables | Deletion (n=163) | Non-deletion
(n=78) | t | P-value |
|---|
| Sex |
|
|
|
|
|
Male | 100 | 49 |
| 0.887 |
|
Female | 63 | 29 |
|
|
| Age (years) |
|
|
|
|
|
≥65 | 75 | 32 |
| 0.491 |
|
<65 | 88 | 46 |
|
|
| Hypertension |
|
|
|
|
|
Yes | 120 | 50 |
| 0.134 |
| No | 43 | 28 |
|
|
| Diabetes |
|
|
|
|
|
Yes | 77 | 19 |
| 0.001 |
| No | 86 | 59 |
|
|
| Smoking
history |
|
|
|
|
|
Yes | 115 | 47 |
| 0.142 |
| No | 48 | 31 |
|
|
| White blood cells
(10×9/l) | 4.84±1.76 | 4.61±1.24 | 1.037 | 0.301 |
| Hemoglobin
(g/l) | 163.39±23.87 | 167.39±25.75 | 1.186 | 0.237 |
| Platelet
(10×9/l) | 126.89±29.12 | 134.29±29.61 | 1.836 | 0.068 |
| BMI index
(kg/m3) | 22.48±1.84 | 22.89±1.06 | 1.827 | 0.069 |
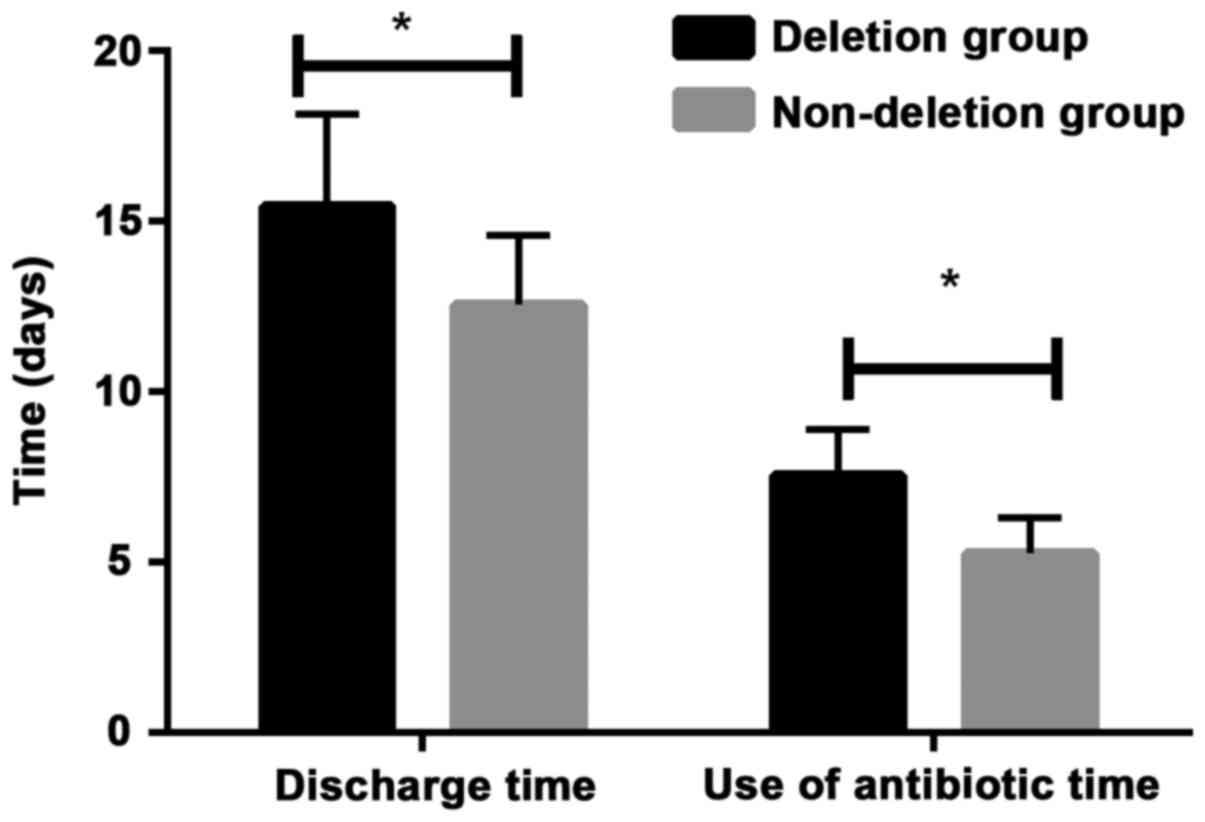
Prognosis of patients
Hospitalization time and the length of the use of
antibiotics were compared between deletion group and non-deletion
group. We found that hospitalization time and the length of the use
of antibiotics were significantly longer in deletion group than in
non-deletion group (P<0.05; Fig.
2). In addition, infection rate of deletion group was
significantly higher than that of non-deletion group (P<0.05;
Table IV).
 | Table IV.Prognosis of patients. |
Table IV.
Prognosis of patients.
| Groups | Infection | Non-infection | P-value |
|---|
| Deletion
(n=78) | 37 (47.44) | 41 (52.56) | 0.048 |
| Non-deletion
(n=163) | 55 (33.74) | 108 (66.26) |
|
Follow-up
Observation group was divided in two groups
including deletion group and non-deletion group, and all patients
were followed up for 12 months. Harris scoring was performed. No
significant differences in Harris scores were found between two
groups on the day of discharge (P>0.05). Harris scores were
significantly lower in deletion group than those in non-deletion
group half year (P=0.004) and one year after discharge (P=0.001;
Table V).
 | Table V.Comparisons of Harris scores. |
Table V.
Comparisons of Harris scores.
| Group | n | Discharge after
operation | Half a year after
discharge | One year after
discharge |
|---|
| GSTM1 gene deletion
type | 163 | 59.41±12.88 | 66.47±10.57 | 71.43±16.94 |
| GSTM1 gene
non-deletion type | 78 | 60.57±14.38 | 70.76±11.67 | 79.12±15.51 |
| t value |
| 6.874 | 8.419 | 9.354 |
| P-value |
| 0.364 | 0.074 | 0.047 |
Discussion
In recent years, with the application of biological
materials and maturation of surgical techniques, artificial hip
replacement technique becomes more and more mature (16,17). At
present, postoperative infection is still the main problem of
artificial hip replacement, and has a great influence on the
recovery of patients (18). Hence,
in order to reduce postoperative complications caused by artificial
hip replacement and improve patient's quality of life, effects of
GSTM1 polymorphism on the recovery of patients underwent artificial
hip replacement was first investigated in the present study.
As an important phase II metabolic enzyme, GSTM1 is
located on the first chromosome, which has detoxificative and cell
protective effects to the human body (19,20). A
large number of studies reported that (21–23)
GSTM1 is associated with the occurrence and prognosis of various
types of cancer, but its involvement in artificial hip replacement
remains unclear. In the present study, PCR-RFLP technology was
adopted to analyze the genotype deletion of GSTM1 gene, so as to
study the recovery of patients undergoing artificial hip
replacement.
Results of this study indicated that the
distribution frequency of deletion type of GSTM1 gene was 41.25% in
control group, which is consistent with the finding in previous
study (24). Among 241 patients
undergoing artificial hip replacement, there were 163 (67.63%)
cases of deletion type of GSTM1 gene. Significant difference in
distribution frequency was found between observation group and
control group (OR=1.51, 95% CI: 1.075–2.023, P<0.05), suggesting
that deletion of GSTM1 gene is correlated with poor recovery.
Studies have shown that the absence of the GSTM1 gene may lead to
the development of diabetes, and the incidence of infection in
patients with diabetes after hip replacement is much higher than
normal, delaying recovery and leading to poor prognosi. We compared
the clinical data between the deletion group and the non-deletion
group. We found that the number patients with diabetes in deletion
group were significantly bigger than that in the non-deletion
group. This also shows that there is a link between the loss of
GSTM1 gene and the prognosis of hip replacement patients. Loss of
GSTM1 gene may cause the development of diabetes, and the risk of
infection in patients with diabetes after hip replacement is much
higher than that in normal people. Therefore, patients were further
divided into GSTM1 gene deletion group and GSTM1 gene non-deletion
group for follow-up study. Harris score revealed that recovery of
patients in GSTM1 gene deletion group was significantly worse
compared with that in GSTM1 gene non-deletion group within one year
after discharge (P<0.05), indicating that GSTM1 gene deletion
may be a risk factor for the delayed recovery in patients underwent
artificial hip replacement. Those results indicate that GSTM1 gene
deletion in patients with hip replacement had an impact on
prognosis. Life safety and health issues are currently the focus of
social attention. Recovery after artificial hip replacement is a
slow and systematic process. Individualized treatment and
rehabilitation can reduce the occurrence of complications after
replacement, thus achieving better recovery effect to improve the
quality of life of patients. This study provided references for the
prediction of recovery of patients with artificial hip
replacement.
It is the first time to make study through combining
GSTM1 gene with artificial hip replacement. This study is hoped to
provide better service for the recovery of patients and clinical
treatment through discussing the relationship between GSTM1 gene
and recovery of patients undergoing artificial hip replacement.
Also an in-depth discussion will be made according to the results
of this study and deeper-seated experiments will be designed
according to the guess of influence mechanism in the future. There
are also limitations in this study, for example, the short period
of the follow-up and small sample size caused by the difficulty in
enrolling healthy volunteers, in which may affects the reliability
of the results. Future studies with bigger sample size are needed
to further confirm the conclusions in the present study.
In conclusion, PCR-RFLP technology is successfully
utilized to analyze GSTM1 genotypes in synovial fluid, and the
results suggest that GSTM1 gene polymorphism is correlated with
recovery of patients undergoing artificial hip replacement. The
present study provided references for postoperative rehabilitation
of patients undergoing artificial hip replacement.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Application
Of Accelerated Rehabilitation Surgical Concept In The Perioperative
Period Of Hip Arthroplasty (project no. 2016ws0387), the Medical
and Health Science And Technology Development Program of Shandong
(grant no. 2016WS0327), and the Fund Of Natural Science of Shandong
(grant no. ZR2014CQ042).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XL and TX conceived and designed the study. XL and
BH were responsible for the collection and analysis of the data. BW
and MQ interpreted the data and drafted the manuscript. XL and BW
revised the manuscript critically for important intellectual
content. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
People's Hospital of Rizhao (Shandong, China). Signed written
informed consent was obtained from the patients and/or
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
van der Pas SL, Nelissen RGHH and Fiocco
M: Patients with staged bilateral total joint arthroplasty in
registries: Immortal time bias and methodological options. J Bone
Joint Surg Am. 99:e822017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Warth LC, Callaghan JJ, Liu SS, Klaassen
AL, Goet DD and Johnston RC: Thirty-five-year results after
Charnley total hip arthroplasty in patients less than fifty years
old: A concise follow-up of previous reports. J Bone Joint Surg Am.
96:1814–1819. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cadossi M, Mazzotti A, Baldini N, Giannini
S and Savarino L: New couplings, old problems: Is there a role for
ceramic-on-metal hip arthroplasty? J Biomed Mater Res B Appl
Biomater. 104:204–209. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Piacentini S, Polimanti R, Porreca F,
Martínez-Labarga C, De Stefano GF and Fuciarelli M: GSTT1 and GSTM1
gene polymorphisms in European and African populations. Mol Biol
Rep. 38:1225–1230. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhang X, Lin J, Wu X, Lin Z, Ning B,
Kadlubar S and Kadlubar FF: Association between GSTM1 copy number,
promoter variants and susceptibility to urinary bladder cancer. Int
J Mol Epidemiol Genet. 3:228–236. 2012.PubMed/NCBI
|
|
6
|
Wang J, Zou L, Huang S, Lu F, Lang X, Han
L, Song Z and Xu Z: Genetic polymorphisms of glutathione
S-transferase genes GSTM1, GSTT1 and risk of coronary heart
disease. Mutagenesis. 25:365–369. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tang ZH, Zhang C, Cheng P, Sun HM, Jin Y,
Chen YJ and Huang F: Glutathione-S-transferase polymorphisms
(GSTM1, GSTT1 and GSTP1) and acute leukemia risk in Asians: A
meta-analysis. Asian Pac J Cancer Prev. 15:2075–2081. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Singh S: Cytoprotective and regulatory
functions of glutathione S-transferases in cancer cell
proliferation and cell death. Cancer Chemother Pharmacol. 75:1–15.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tamaki Y, Arai T, Sugimura H, Sasaki T,
Honda M, Muroi Y, Matsubara Y, Kanno S, Ishikawa M, Hirasawa N and
Hiratsuka M: Association between cancer risk and drug-metabolizing
enzyme gene (CYP2A6, CYP2A13, CYP4B1, SULT1A1, GSTM1, and GSTT1)
polymorphisms in cases of lung cancer in Japan. Drug Metab
Pharmacokinet. 26:516–522. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wang B, Huang G, Wang D, Li A, Xu Z, Dong
R, Zhang D and Zhou W: Null genotypes of GSTM1 and GSTT1 contribute
to hepatocellular carcinoma risk: Evidence from an updated
meta-analysis. J Hepatol. 53:508–518. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
García-González MA, Quintero E, Bujanda L,
Nicolás D, Benito R, Strunk M, Santolaria S, Sopeña F, Badía M,
Hijona E, et al: Relevance of GSTM1, GSTT1, and GSTP1 gene
polymorphisms to gastric cancer susceptibility and phenotype.
Mutagenesis. 27:771–777. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wei Y, Zhou T, Lin H, Sun M, Wang D, Li H
and Li B: Significant associations between GSTM1/GSTT1
polymorphisms and nasopharyngeal cancer risk. Tumor Biol.
34:887–894. 2013. View Article : Google Scholar
|
|
13
|
Raza S, Abbas S, Ahmad A, Ahmed F, Zaidi
Zh and Mahdi F: Association of glutathione-S-transferase (GSTM1 and
GSTT1) and FTO gene polymorphisms with type 2 diabetes mellitus
cases in Northern India. Balkan J Med Genet. 17:47–54. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Van Ness PH, Peduzzi PN and Quagliarello
VJ: Efficacy and effectiveness as aspects of cluster randomized
trials with nursing home residents: Methodological insights from a
pneumonia prevention trial. Contemp Clin Trials. 33:1124–1131.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kalairajah Y, Azurza K, Hulme C, Molloy S
and Drabu KJ: Health outcome measures in the evaluation of total
hip arthroplasties-a comparison between the Harris hip score and
the Oxford hip score. J Arthroplasty. 20:1037–1041. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Urquhart DM, Hanna FS, Brennan SL, Wluka
AE, Leder K, Cameron PA, Graves SE and Cicuttini FM: Incidence and
risk factors for deep surgical site infection after primary total
hip arthroplasty: A systematic review. J Arthroplasty. 25:1216–1222
e1-e3. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bozic KJ, Lau E, Kurtz S, Ong K, Rubash H,
Vail TP and Berry DJ: Patient-related risk factors for
periprosthetic joint infection and postoperative mortality
following total hip arthroplasty in Medicare patients. J Bone Joint
Surg Am. 94:794–800. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Schrama JC, Espehaug B, Hallan G,
Engesaeter LB, Furnes O, Havelin LI and Fevang BT: Risk of revision
for infection in primary total hip and knee arthroplasty in
patients with rheumatoid arthritis compared with osteoarthritis: A
prospective, population-based study on 108,786 hip and knee joint
arthroplasties from the Norwegian Arthroplasty Register. Arthritis
Care Res (Hoboken). 62:473–479. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hashemi M, Eskandari-Nasab E, Fazaeli A,
Taheri M, Rezaei H, Mashhadi M, Arbabi F, Kaykhaei MA, Jahantigh M
and Bahari G: Association between polymorphisms of glutathione
S-transferase genes (GSTM1, GSTP1 and GSTT1) and breast cancer risk
in a sample Iranian population. Biomark Med. 6:797–803. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wang IJ, Guo YL, Lin TJ, Chen PC and Wu
YN: GSTM1, GSTP1, prenatal smoke exposure, and atopic dermatitis.
Ann Allergy Asthma Immunol. 105:124–129. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Abdel Rahman HA, Khorshied MM, Elazzamy HH
and Khorshid OM: The link between genetic polymorphism of
glutathione-S-transferases, GSTM1, and GSTT1 and diffuse large
B-cell lymphoma in Egypt. J Cancer Res Clin Oncol. 138:1363–1368.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Borst L, Buchard A, Rosthøj S, Wesolowska
A, Wehner PS, Wesenberg F, Dalhoff K and Schmiegelow K: Gene dose
effects of GSTM1, GSTT1 and GSTP1 polymorphisms on outcome in
childhood acute lymphoblastic leukemia. J Pediatr Hematol Oncol.
34:38–42. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yang LM, Li XH and Bao CF: Glutathione
S-transferase P1 and DNA polymorphisms influence response to
chemotherapy and prognosis of bone tumors. Asian Pac J Cancer Prev.
13:5883–5886. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Yao ZG, Yong E and Wang HY: The interacted
effects between glutathione S-transferase gene polymorphism and
smoking in lung cancer. Chinese J Med Guide. 14:185–186. 882012.(In
Chinese).
|