Introduction
Coronary heart disease is a common type of heart
disease with high incidence. More than 20 million people die each
year from cardiovascular disease, of which about 42% die of
coronary heart disease (1). About
50% of people over the age of 50 suffer from coronary heart disease
worldwide (2), and the incidence and
mortality of coronary heart disease are still rising (3). Coronary heart disease has become the
number one killer of human health. Current treatment of coronary
heart disease mainly aims to control the disease, reduce
complications, enhance postoperative care and reduce the number of
treatment. Therefore, early diagnosis and treatment of coronary
heart disease is the key to improve survival (4,5).
At present, diagnosis of coronary heart disease is
mainly based on dyslipidemia (6).
Treatment methods mainly include interventional, surgical and drug
treatments, of which drug treatment is particularly important
(7). Statins are widely used in drug
treatment and show promising therapeutic effects. Statins also play
an important role in secondary prevention of coronary heart disease
(8). Clinical studies have confirmed
that atorvastatin has a satisfactory effect in the treatment of
coronary heart disease (9,10). In addition, therapeutic effect of
angiotensin II receptor blocker (ARB) on coronary heart disease is
also satisfactory. Irbesartan belongs to the ARB, and studies have
shown that high-dose irbesartan can effectively reduce blood
pressure, reduce the degree of carotid atherosclerosis, and relieve
clinical symptoms (11). Type II
secretory phospholipase A2 (sPLA2) is a member of the family of
calcium-dependent phospholipases that is highly expressed in
atherosclerotic lesions, and can affect atherosclerosis and lead to
coronary heart disease (12).
sPLA2-V as a subtype of sPLA2, and has been detected in
atherosclerotic plaques (13). In
the present study, irbesartan and atorvastatin calcium were used
together to investigate their effects on sPLA2-V expression in
myocardium and aorta in rats with coronary heart disease, and to
explore the possible mechanism.
Materials and methods
Experimental animals
One hundred sixty healthy male Wistar rats, 3–4
months old, weighing approximately 200 g, were provided by China
Medical University (Taichung, Taiwan). The rats were kept in cages
with controlled temperature and light cycles (24°C and 12/12 light
cycles) with free access to water and food. The humidity was
60±10%. This study was approved by the Ethics Committee of Jinan
Zhangqiu District Hospital of TCM (Jinan, China).
Drugs and major reagents
Irbesartan was purchased from Jiangsu Hengrui
Medicine Co., Ltd. (state approval no. H20000513; Lianyungang,
China). Atorvastatin calcium was purchased from Beijing Jialin
Pharmaceutical Co., Ltd. (state approval no. H20093819; Beijing,
China). TRIzol and RT-PCR kit were purchased from Sangon Biotech
(Shanghai) Co., Ltd. (Shanghai, China). Total cholesterol (TC),
triglyceride (TG), low-density lipoprotein cholesterol (LDL-C) and
high-density lipoprotein cholesterol (HDL-C) kits (all from Cyttel
Bioscience Inc., Beijing, China). Skim milk powder (BD Biosciences,
San Jose, CA, USA), rabbit anti-rat sPLA2-V polyclonal antibody
(cat no. 16009-1-AP; 1:1,000) and goat anti-rabbit-HRP secondary
polyclonal antibody (cat. no. SA00001-2; 1:800) were purchased from
Wuhan Sanying Biotechnology, Wuhan, China. Protein electrophoresis
buffer, transfer membrane buffer and washing, all from Sangon
Biotech (Shanghai) Co., Ltd.
Model construction
The 160 healthy rats were fed with high-fat diet (2%
cholesterol, 10% lard, 0.5% sodium cholate, 87.3% basal diet) daily
for 6 weeks, followed by intraperitoneal injection of pituitrin at
a dose of 30 U/kg for 3 consecutive days. All rats were subjected
to electrocardiogram and lipids test and 152 rats showed myocardial
ischemia and hyperlipidemia, which are the symptoms of coronary
heart disease, considering the model was constructed
successfully.
Animal grouping and treatment
Rats with coronary heart disease were randomly
divided into 4 groups to receive corresponding treatment, 38 rats
in each group. Rats in irbesartan group were treated with 50
mg/(kg.day) irbesartan through intragastric administration. Rats in
atorvastatin calcium group were given intragastric administration
of atorvastatin calcium at a dose of 10 mg/(kg.day). Rats in
combination group were subjected to intragastric administration of
atorvastatin calcium at a dose of 10 mg/(kg.day) and irbesartan at
a dose of 50 mg/(kg.day), while rats in model groups were given
intragastric administration of normal saline at a dose of 2 ml/day.
Treatment was performed for 12 weeks.
Detection indicators
Collection of specimens
After intragastric administration for 12 weeks, rats
in each group were fasted for 16 h and anesthetized by
intraperitoneal injection of 10% chloral hydrate. Chest was opened,
and heart was punctured to collect blood, followed by
centrifugation at 8,000 × g for 15 min to prepare serum. Heart and
aortic trunk were dissected, and the right apex of left ventricular
myocardium was taken, rinsed with pre-cooling 0.9% saline, and then
placed in 4% paraformaldehyde solution for fixation.
Automatic biochemical analyzer was used to measure
TC, TG, LDL-C, HDL-C and TC/HDL-C according to the instructions of
corresponding kit (Cyttel Bioscience Inc.).
RT-PCR to detect the expression of
sPLA2-V
TRIzol was used to extract total RNA from the apex
and aorta, and cDNA was synthesized by using RNA as template
through reverse transcription according to the instructions of the
kit, and 1 µl of cDNA was used as template in PCR amplification
(Table I). Reaction conditions were:
95°C for 10 min; 95°C for 50 sec, followed by 30 cycles of 56°C for
50 sec and 72°C for 60 sec, and 72°C for 10 min. PCR products were
detected by 1.5% agarose gel electrophoresis. GAPDH was used as
endogenous control to normalize the intensity of each band to
reflect the relative expression level of each gene.
 | Table I.Primer sequences used in PCR
reaction. |
Table I.
Primer sequences used in PCR
reaction.
| Genes | Primers sequence | Length of product
(bp) |
|---|
| sPLA2-V | F:
5′-TCACGCTGGCTTGGTTCCTG-3′ | 320 |
|
| R:
5′-CAATCATGGACTTCAGTTCT-3′ |
|
| GAPDH | F:
5′-TGACTCCACTCACGGCAAATTCAA-3′ | 580 |
|
| R:
5′-CTAGTTGAATGCTTGGATGTACAA-3′ |
|
Detection of sPLA2-V protein
expression
The preserved myocardial and aortic specimens was
mixed with lysis solution (1 ml/100 mg), homogenized on ice, and
then transferred to a centrifuge tube, followed by centrifugation
at 3,000 × g for 8 min to collect supernatant. Protein (20 µg) was
mixed with equal volume of 2X loading buffer and boiled in water
for 5 min, followed by electrophoresis under 100 V until the dye
moved to the lower 1/3 of the gel. Protein was transferred to PVDF
membrane under 110 mA for 2 h. Then membranes were blocked with 5%
skimmed milk powder, followed by incubation with rabbit anti-rat
sPLA2-polyclonal antibody overnight. The next day, membranes were
washed 3 times, 5 min for each time, followed by incubation with
goat anti-rabbit-HRP secondary polyclonal antibody at room
temperature for 1 h. Membranes were then washed 3 times, 5 min for
each time, followed by addition of chemiluminescence substrate.
Signals were detected by gel imager (Thermo Fisher Scientific,
Inc., Waltham, MA, USA).
Statistical analysis
Statistical analysis was performed by using SPSS
17.0 (SPSS, Inc., Chicago, IL, USA). Count data were analyzed by
χ2 test. Measurement data were expressed as the mean ±
SD, and analysis of variance was used for comparisons among
multiple groups and the post-hoc test was Least Significant
Difference test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Comparison of blood lipid indicators
before treatment
Rats were randomly divided into different groups
after model construction. There was no statistical difference in
body weight among groups. Before treatment, no significantly
differences in levels of TC, TG, LDL-C, HDL-C and TC/HDL-C were
found among irbesartan, atorvastatin calcium, combination and model
groups (p>0.05) (Table II).
 | Table II.Comparison of TC, TG, LDL-C, HDL-C and
TC/HDL-C among groups before treatment (mean ± SD). |
Table II.
Comparison of TC, TG, LDL-C, HDL-C and
TC/HDL-C among groups before treatment (mean ± SD).
| Groups (n=38) | Model group | Irbesartan group | Atorvastatin
calcium | Combination
group | F-value | P-value |
|---|
| Weight (g) | 601.52±28.52 | 603.35±30.33 | 603.98±30.15 | 602.82±30.03 | 0.004 | 1.000 |
| TC (mmol/l) | 5.01±1.04 | 5.03±1.12 | 5.05±1.03 | 5.04±1.08 | 0.001 | 0.435 |
| TG (mmol/l) | 2.26±0.26 | 2.27±0.28 | 2.23±0.25 | 2.24±0.28 | 0.014 | 0.996 |
| LDL-C (mmol/l) | 3.09±0.30 | 3.10±0.32 | 3.11±0.33 | 3.08±0.32 | 0.005 | 0.999 |
| HDL-C (mmol/l) | 1.17±0.24 | 1.16±0.22 | 1.13±0.24 | 1.15±0.21 | 0.017 | 0.389 |
| TC/HDL-C
(mmol/l) | 4.40±0.88 | 4.42±0.90 | 4.43±0.93 | 4.40±0.87 | 0.001 | 0.679 |
Comparison of blood lipid indicators
after treatment
Levels of TC, TG, LDL-C, HDL-C and TC/HDL-C in rats
of each group after 12 weeks of treatment were measured by
automatic biochemical analyzer (Table
III). Levels of TC, TG, LDL-C, and TC/HDL-C were significantly
lower in irbesartan, atorvastatin calcium, and combination groups
than those in model group (p<0.05). The decrease is more
significant in combination group than that in irbesartan group or
atorvastatin calcium group (p<0.05), while no significant
difference was found between irbesartan and atorvastatin calcium
groups. Levels of HDL-C were significantly higher in irbesartan,
atorvastatin calcium, and combination groups than in model group
(p<0.05). The increase is more significant in combination group
than in irbesartan or atorvastatin calcium group (p<0.05), while
no significant difference was found between irbesartan and
atorvastatin calcium groups.
 | Table III.Comparison of TC, TG, LDL-C, HDL-C and
TC/HDL-C among groups after treatment (mean ± SD). |
Table III.
Comparison of TC, TG, LDL-C, HDL-C and
TC/HDL-C among groups after treatment (mean ± SD).
| Groups (n=38) | Model group | Irbesartan group | Atorvastatin
calcium | Combination
group | F-value | P-value |
|---|
| TC (mmol/l) | 5.03±1.02 |
4.09±0.15a |
3.80±0.11a |
3.58±0.18b | 4.417 | 0.041 |
| TG (mmol/l) | 2.27±0.28 |
1.90±0.14a |
1.92±0.04a |
1.78±0.15b | 4.373 | 0.043 |
| LDL-C (mmol/l) | 3.21±0.11 |
2.98±0.09a |
2.98±0.15a |
2.54±0.13b | 5.085 | 0.029 |
| HDL-C (mmol/l) | 1.15±0.26 |
1.33±0.25a |
1.32±0.18a |
1.88±0.18b | 6.210 | 0.017 |
| TC/HDL-C
(mmol/l) | 4.43±0.38 |
4.07±0.48a |
3.96±0.34a |
2.98±0.42b | 6.919 | 0.013 |
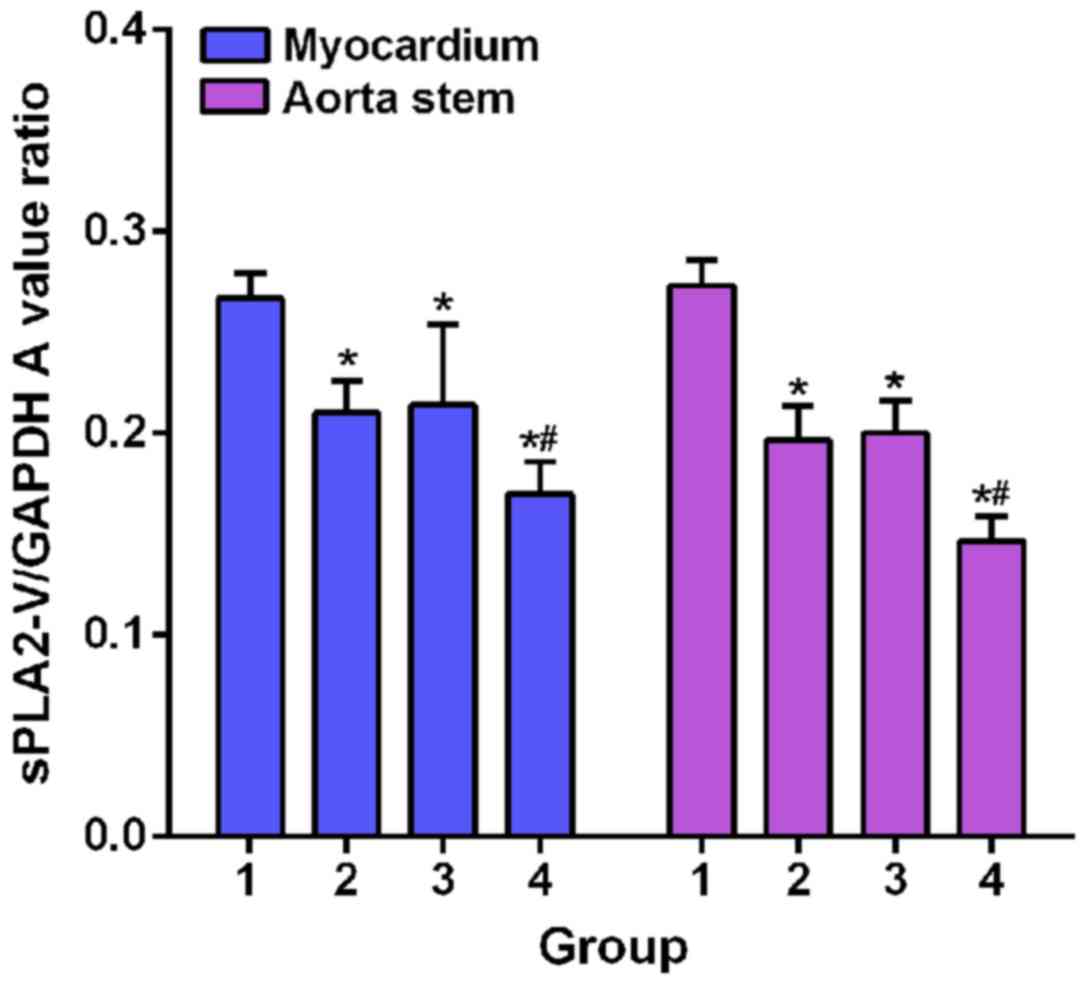
Comparisons of expression level of
PLA2-V mRNA in myocardium and aortic trunk among groups
GAPDH was as an endogenous control. sPLA2-V fragment
was amplified by RT-PCR and analyzed by 1.5% agarose gel
electrophoresis to determine the relative expression of sPLA2-V
mRNA in each sample. After treatment, in 38 rats of irbesartan
group, expression level of sPLA2-V in apex of heart was
significantly decreased in 15 rats, and expression level of sPLA2-V
in aorta was significantly decreased in 11 rats. In atorvastatin
calcium group, expression level of sPLA2-V in apex of heart was
significantly decreased in 19 rats, and expression level of sPLA2-V
in aorta was significantly decreased in 15 rats. In combination
group, expression level of sPLA2-V in apex of heart was
significantly decreased in 30 rats, and expression level of sPLA2-V
in aorta was also significantly decreased in 30 rats (Fig. 1). Expression levels of sPLA2-V mRNA
in apex and aorta were the highest in model group. Expression
levels of sPLA2-V mRNA in apex and aorta of model groups were
significant higher than those of irbesartan, atorvastatin calcium
and combination groups (p<0.05). In addition, expression levels
of sPLA2-V mRNA in apex and aorta of combination group were
significantly lower than those in irbesartan and atorvastatin
calcium groups (p<0.05).
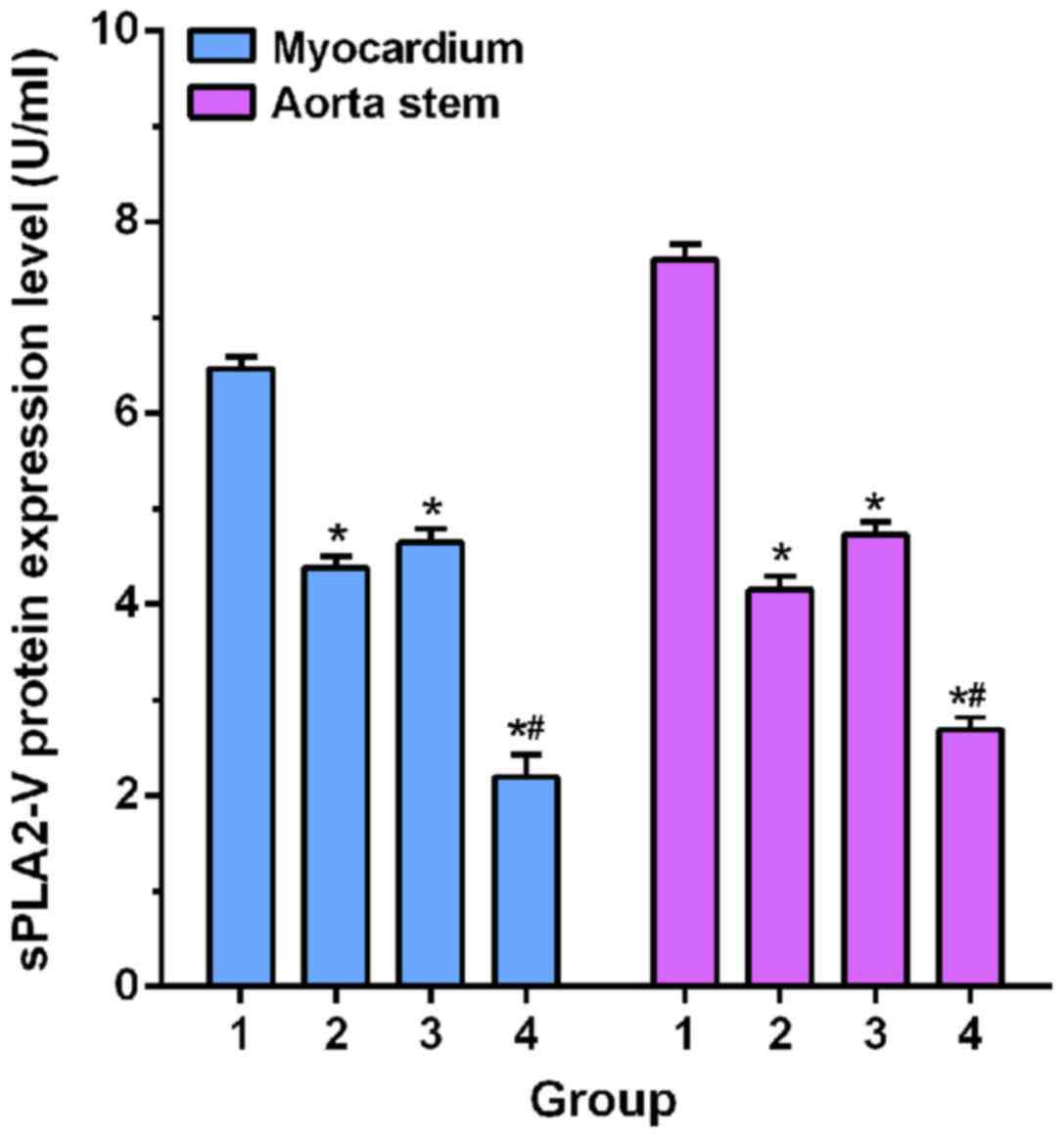
Comparisons of expression level of
PLA2-V protein in myocardium and aortic trunk among groups
Western blot analysis results were shown in Fig. 2. Expression levels of sPLA2-V protein
in apex and aorta of model group were significant higher than those
of irbesartan, atorvastatin calcium and combination groups
(p<0.05). In addition, expression levels of sPLA2-V protein in
apex and aorta of combination group were significantly lower than
those in irbesartan and atorvastatin calcium groups
(p<0.05).
Discussion
Coronary heart disease is a common disease
endangering the health of the elderly, and the incidence is
increasing year by year (14).
Atherosclerosis can lead to organ disease (15). Occurrence of coronary heart disease
may be related to dyslipidemia, genetic, environmental and other
factors (16,17).
At present, dyslipidemia is considered to be the
pathological basis of atherosclerosis. TC and HDL-C play roles of
promoting and inhibiting atherosclerosis respectively. TC/HDL-C
ratio can reflect the balance between atherosclerosis and
anti-atherosclerosis lipoproteins, and the status of cardiovascular
events (18). In this study, Wistar
rat model of coronary heart disease was established to explore the
therapeutic effect of irbesartan and atorvastatin calcium on blood
lipids. Results showed that all blood lipid indexes including TC,
TG, HDL-C, LDL-C and TC/HDL-C were improved in irbesartan,
atorvastatin calcium and combination groups compared with model
group. Compared with irbesartan and atorvastatin calcium groups;
TC, TG, LDL-C and TC/HDL-C decreased significantly, while HDL-C
increased significantly in combination group, indicating that both
irbesartan and atorvastatin calcium can effectively treat coronary
heart disease, and the combined treatment is even better.
Irbesartan can inhibit vasoconstriction, reduce the release of
aldosterone, reduce blood pressure, and effectively treat coronary
heart disease (19). In this study,
irbesartan group also showed significantly improved blood lipid
indexes, which is consistent with previous studies. Atorvastatin
calcium can significantly reduce carotid atherosclerosis plaque in
patients with ischemic attacks and improve blood lipid levels to
achieve effective treatment of coronary heart disease (20). In this study, treatment with
atorvastatin calcium significantly improved lipid indicators and
reduced symptoms of coronary heart disease.
sPLA2-V is a subtype of sPLA2 that is mainly
produced by vascular smooth muscle cells and macrophages. Higher
expression level of sPLA2-V in atherosclerotic plaques than normal
level indicates the risk of coronary heart disease (21). Irbesartan can inhibit atherosclerosis
by reducing sPLA2-V expression (22,23). In
this study, sPLA2-V expression level in irbesartan group was
significantly lower than that in model group, suggesting that
irbesartan may inhibit the expression of sPLA2-V, thereby
inhibiting the progression of atherosclerosis. Ikonomidis and
Michalakeas (24) found that
atorvastatin can reduce serum sPLA2IIa expression levels to achieve
anti-atherosclerotic effect. In addition, irbesartan combined with
revastatin can inhibit the expression of sPLA2-V (25), but the effects on irbesartan combined
with atorvastatin calcium on expression of sPLA2-V remain unknown.
In this study, atorvastatin calcium treatment effectively reduced
sPLA2-V expression level in rats with heart disease, and the
decrease was more significant in combination group than in
irbesartan and atorvastatin calcium groups, while no significant
differences were found between irbesartan and atorvastatin calcium
groups, indicating that irbesartan combined with atorvastatin
calcium is superior to irbesartan or atorvastatin calcium alone in
inhibiting the expression of sPLA2-V.
In conclusion, therapeutic effect of combination of
irbesartan and atorvastatin calcium is better than that of
irbesartan or atorvastatin calcium alone in the treatment of rats
with coronary heart disease. The possible explanation is that the
two drugs can reduce the expression of sPLA2-V in myocardium and
aortic trunk, which in turn relieved atherosclerosis and achieved
better therapeutic effect.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
TL was a major contributor in writing the
manuscript, and designing the methods and the idea of this paper,
and responsible for reviewing. WY participated in the analysis and
discussion of the data, and responsible for the collection of the
data and the follow-up management of the patients. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Jinan Zhangqiu District Hospital of TCM (Jinan, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Wang EY, Dixson J, Schiller NB and Whooley
MA: Causes and predictors of death in patients with coronary heart
disease (from the heart and soul study). Am J Cardiol. 119:27–34.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Woods SE: Primary prevention of coronary
heart disease in women. Should asymptomatic women 50 years of age
take aspirin regularly? Arch Fam Med. 3:361–364. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Menotti A, Puddu PE, Adachi H, Kafatos A,
Tolonen H and Kromhout D: The strength of the multivariable
associations of major risk factors predicting coronary heart
disease mortality is homogeneous across different areas of the
Seven Countries Study during 50-year follow-up. Acta Cardiol.
8:1–7. 2017.
|
|
4
|
Brown JP, Clark AM, Dalal H, Welch K and
Taylor RS: Patient education in the contemporary management of
coronary heart disease. Cochrane Database Syst Rev.
2010:CD0088952010.PubMed/NCBI
|
|
5
|
Lebwohl B, Cao Y, Zong G, Hu FB, Green
PHR, Neugut AI, Rimm EB, Sampson L, Dougherty LW, Giovannucci E, et
al: Long term gluten consumption in adults without celiac disease
and risk of coronary heart disease: Prospective cohort study. BMJ.
357:j18922017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lee JS, Chang PY, Zhang Y, Kizer JR, Best
LG and Howard BV: Triglyceride and HDL-C dyslipidemia and risks of
coronary heart disease and ischemic stroke by glycemic
dysregulation status: The strong heart study. Diabetes Care.
40:529–537. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lu W, Zhu Y, Han Z, Wang X, Wang X and Qiu
C: Drug-coated balloon in combination with bare metal stent
strategy for de novo coronary artery disease: A PRISMA-compliant
meta-analysis of randomized clinical trials. Medicine (Baltimore).
96:e63972017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Serban MC, Muntner P and Rosenson RS:
Reply: Statin intolerance and risk for recurrent myocardial
infarction, Coronary heart disease events, and all-cause mortality.
J Am Coll Cardiol. 70:685–686. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wiklund O, Mattsson-Hultén L, Hurt-Camejo
E and Oscarsson J: Effects of simvastatin and atorvastatin on
inflammation markers in plasma. J Intern Med. 251:338–347. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhao Y, Peng R, Zhao W, Liu Q, Guo Y, Zhao
S and Xu D: Zhibitai and low-dose atorvastatin reduce blood lipids
and inflammation in patients with coronary artery disease. Medicine
(Baltimore). 96:e61042017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ricci F, De Caterina R and Fedorowski A:
Orthostatic hypotension: Epidemiology, prognosis, and treatment. J
Am Coll Cardiol. 66:848–860. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Liu PY, Li YH, Tsai WC, Chao TH, Tsai LM,
Wu HL and Chen JH: Prognostic value and the changes of plasma
levels of secretory type II phospholipase A2 in patients with
coronary artery disease undergoing percutaneous coronary
intervention. Eur Heart J. 24:1824–1832. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Holmes MV, Exeter HJ, Folkersen L, Nelson
CP, Guardiola M, Cooper JA, Sofat R, Boekholdt SM, Khaw KT, Li KW,
et al: CARDIoGRAM Consortium: Novel genetic approach to investigate
the role of plasma secretory phospholipase A2 (sPLA2)-V isoenzyme
in coronary heart disease: Modified Mendelian randomization
analysis using PLA2G5 expression levels. Circ Cardiovasc Genet.
7:144–150. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dickson Vaughan V, Lee CS, Yehle KS, Mola
A, Faulkner KM and Riegel B: Psychometric testing of the Self-Care
of coronary heart disease inventory (SC-CHDI). Res Nurs Health.
40:15–22. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Huang L, Zheng Y, Yuan X, Ma Y, Xie G,
Wang W, Chen H and Shen L: Decreased frequencies and impaired
functions of the CD31+ subpopulation in Treg
cells associated with decreased FoxP3 expression and enhanced Treg
cell defects in patients with coronary heart disease. Clin Exp
Immunol. 187:441–454. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tang SS, Xu S, Cheng J, Cai MY, Chen L,
Liang LL, Yang XL, Chen C, Liu XG and Xiong XD: Two tagSNPs
rs352493 and rs3760908 within SIRT6 gene are associated with the
severity of coronary artery disease in a chinese han population.
Dis Markers. 2016:16280412016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
McLaren JE, Michael DR, Ashlin TG and
Ramji DP: Cytokines, macrophage lipid metabolism and foam cells:
Implications for cardiovascular disease therapy. Prog Lipid Res.
50:331–347. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wu G, Li GB and Dai B: Association of KIF6
variant with lipid level and angiographic coronary artery disease
events risk in the Han Chinese population. Molecules.
17:11269–11280. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ntekim OE, Allard JS, Ngwa JS, Johnson AA,
Castor C, Iyalomhe O, Fungwe TV, Ntekim CC and Obisesan T: Additive
effects of capsaicin oleoresin, irbesartan and amlodipine besylate
on the blood pressure of spontaneously hypertensive rats. J Med
Plants Res. 10:468–478. 2016. View Article : Google Scholar
|
|
20
|
Strupp M: The results support the use of
atorvastatin in elderly patients with recent stroke or TIA.
Neurology. 73:8172009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Xin H, Chen ZY, Lv XB, Liu S, Lian ZX and
Cai SL: Serum secretory phospholipase A2-IIa (sPLA2-IIA) levels in
patients surviving acute myocardial infarction. Eur Rev Med
Pharmacol Sci. 17:999–1004. 2013.PubMed/NCBI
|
|
22
|
Burstein B and Nattel S: Atrial fibrosis:
Mechanisms and clinical relevance in atrial fibrillation. J Am Coll
Cardiol. 51:802–809. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Rivard L and Khairy P: Mechanisms,
clinical significance, and prevention of cognitive impairment in
patients with atrial fibrillation. Can J Cardiol. 33:1556–1564.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ikonomidis I and Michalakeas CA:
Phospholipases in cardiovascular diseaseAdvances in Biochemistry in
Health and Disease: Phospholipases in Health and Disease. Tappia PS
and Dhalla NS: 10. Springer; New York: pp. 73–83. 2014
|
|
25
|
Divchev D, Grothusen C, Luchtefeld M,
Thoenes M, Onono F, Koch R, Drexler H and Schieffer B: Impact of a
combined treatment of angiotensin II type 1 receptor blockade and
3-hydroxy-3-methyl-glutaryl-CoA-reductase inhibition on secretory
phospholipase A2-type IIA and low density lipoprotein oxidation in
patients with coronary artery disease. Eur Heart J. 29:1956–1965.
2008. View Article : Google Scholar : PubMed/NCBI
|