Introduction
The population growth in senior citizens is a
serious problem worldwide. Accordingly, the increase in prevalence
of hepatic resection is associated with the increasing expectation
of surgery for elderly patients (>65 years) (1). A number of reports have demonstrated
that hepatic resection is acceptable for elderly patients, as the
prognosis and complications of elderly patients following hepatic
resection are similar to those of young patients (2–5).
Conversely, a number of reports have demonstrated that the
complications rate of elderly patients was higher than those of
younger patients due to elderly patients' fragility (6–8).
Therefore, it appeared to be insufficient to evaluate the risk and
indication of surgical intervention by only age. Once postoperative
complications occur, high medical expenses are required due to
prolongation of the hospitalization period and increased use of
drugs. Therefore, prevention and prediction of postoperative
complications are an important issue for the elderly population
receiving surgical treatments. American Society of
Anesthesiologists (ASA) classification, Physical Status
Classification System and Eastern Cooperative Oncology Group (ECOG)
performance status are useful predictors for evaluating the state
of activity in patients prior to surgery (9–13).
However, both systems include subjective factors scored by
estimation; therefore, their accuracy and objectivity are
unclear.
The accelerometer activity meter has received
attention from the general public since its release in 2010 in
developed countries regarding its potential applications in health
care and in rehabilitation (14).
The accelerometer is a device that contains an acceleration sensor,
making it possible to measure calorie consumption while wearing and
has been available to the general public in recent years. An
accelerometer has a distinct difference from a pedometer in that
not only the walking distance but also the exercise intensity such
as sitting time, deskwork time, stair climbing time and bicycle
riding time are measured. Additionally, modern activity meters can
also measure sleeping time and heart rate.
The association between physical activity and
obesity has been evaluated in the field of rehabilitation (15,16). In
addition, a number of reports have demonstrated the association
between activity level and cardiovascular disease (17,18).
Furthermore, physical activity measured by accelerometer was
associated with postoperative outcome, such as duration of
hospitalization and postoperative complications, in cardiovascular
or orthopedic surgery (19,20). However, in abdominal surgery, there
has been no report of the association between complications and
physical activity via accelerometer.
As a novel predictor of postoperative complications,
the present findings suggested that postoperative physical activity
level measured by accelerometer is useful for prediction of
postoperative complications. In the present study, an accelerometer
was used by patients receiving hepatic resection during the
postoperative period, and the association between physical activity
level and postoperative complications was examined.
Patients and methods
Patients
Between August and November 2016, 13 patients (age
range; 58–85 years; males, 10 and females, 3) received hepatic
resection at Shiga University of Medical Science (SUMS) Hospital
(Otsu, Japan). All patients with hepatic resection began a
postoperative diet from postoperative day (POD) 1, and if patients
were able to eat >half of the diet served in POD 3, infusion via
intravenous feeding was ended. If it was less than half amount,
infusion was continued. A total of 1 g cefazolin sodium as an
antibiotic was administered only on the day of surgery every 4 h
during the operation, and it was administered every 8 h following
surgery. In cases where infectious complications occurred
postoperatively, the antibiotics were re-administered based on the
results of various cultures.
Postoperative rehabilitation with the physical
therapist in SUMS Hospital was provided every day from POD 1 for
all patients who underwent abdominal surgery. A total of 12
patients wore the accelerometer to evaluate postoperative physical
activities. One patient was excluded due to complicated sepsis as a
result of venous catheter infection and received intensive
managements from POD 1.
Accelerometer
Lifecorder™ (Suzuken Co., Ltd., Nagoya, Japan) was
used as the accelerometer to evaluate physical activity. The
Lifecorder™ contains an acceleration sensor and can measure the
basal metabolic rate, momentum, number of walks and exercise
intensity by inputting the age, height and weight of the patient.
This accelerometer consists of an acceleration sensor that detects
acceleration, and a computer that calculates basal metabolic rate,
momentum and minute momentum. The momentum is calculated by the
acceleration index (exercise intensity) divided into 10 levels by
the acceleration sensor that recognizes the amplitude and vibration
frequency, multiplied by the body weight. The minute momentum is
calculated as 0.5 in 10 levels. All measurements are made every 4
sec, and the most reliable value is recorded in the device every 2
min. Although division into 10 levels is unique to this model, it
has been confirmed that this is correlated with metabolic
equivalents (21).
Methods
All enrolled patients wore the Lifecorder™ 24 h
daily on the waist from the time of hospitalization until
discharge. The activity level was calculated as total amount of
momentum and minute momentum per day excluded basal metabolic rate
that was expressed as kcal/day. Data from the Lifecorder™ was
analyzed using Lifelyzer 05 Coach™ analysis software (Suzuken Co.,
Ltd.).
Patient background, including age, gender, ASA
classification (9–12), ECOG performance status (13), body mass index, diabetes mellitus,
background liver disease, albumin, alanine aminotransferase,
aspartate aminotransferase, bilirubin, platelet count, prothrombin
activity, white blood cell count, C-reactive protein and
indocyanine green retention rate at 15 min; and operative factors,
including primary disease, tumor size, tumor number, operation
approach, operation method, number of resection, operation time and
bleeding; the degree of physical activity from POD 1 to POD 7;
postoperative course and complications were monitored.
Postoperative complications were defined according to Clavien-Dindo
classification grade II or higher (22). The post-hepatectomy liver failure
(PHLF) was defined according to the definition of the International
Study Group of Liver Surgery (ISGLS) (23). The grade A of PHLF was defined as no
postoperative complication, because it does not affect the
postoperative course. The surgical site infection (SSI) was defined
by Centre for Disease Control and Prevention guidelines (24).
Statistical analysis
Continuous variables were expressed as the mean ±
standard error of the mean. The degree of physical activity up to
the POD 7 was figured and compared for each day with or without
complications. Mann-Whitney U analysis was used for the comparison,
and P<0.05 was considered to indicate a statistically
significant difference. All statistical analyses were performed
with SPSS Statistics 24 (IBM Corp., Armonk, NY, USA).
Results
Patient background
Table I presents
patient characteristics, operative factors and postoperative course
between patients with and without complications. The median
patients' age was 75 and 79 years in the no complication and
complication groups, respectively. The primary diseases were 3
patients with hepatocellular carcinoma (HCC) and 3 patients with
liver metastasis in the no complication group, and 5 patients with
HCC and 1 patient with liver metastasis in the complication group.
In the no complication group, there was 1 patient positive for
hepatitis C (HCV); in contrast, there were 5 HCV patients in the
complication group. The median albumin levels were 3.8 and 4.1 g/dl
in no complication and complication patients, respectively. The
prothrombin activity level was 102% in no complication patients and
92% in complication patients (P=0.05). The alanine aminotransferase
level in no complication patients (23 U/l) was significantly lower
than in complication patients (52 U/l; P=0.04). A total of 3
patients were subjected to partial resection and 3 patients were
subjected to anatomical resection in no complication patients, and
4 patients were subjected to partial resection and 2 patients were
subjected to anatomical resection in complication patients. The ASA
classification and ECOG performance status are indicators of
general condition. All of the no complication patients and 4
complication patients were categorized as class 1 using the ASA
classification, and 2 complication patients were class 2. A total
of 4 and 2 no complication patients were score 0 and 1 in ECOG
performance status, respectively. In contrast, complication
patients included 1 patient with score 2 and 1 patient with score
3. However, there was no statistically significant difference
between the two groups.
 | Table I.Clinical characteristics of the study
patients. |
Table I.
Clinical characteristics of the study
patients.
| Characteristics | Patients without
complication (n=6) | Patients with
complication (n=6) | P-value |
|---|
| Age (years) | 75 (58–81) | 80 (74–85) | 0.09 |
| Gender |
|
|
|
|
Female | 2 (33.3) | 1 (16.7) | >0.99 |
| Male | 4 (66.7) | 5 (83.3) |
|
| ASA
classification |
|
|
|
| 1 | 6 (100.0) | 4 (66.7) | 0.45 |
| 2 | 0 (0.0) | 2 (33.3) |
|
| ECOG performance
status |
|
|
|
| 0 | 4 (66.7) | 2 (33.3) | 0.74 |
| 1 | 2 (33.3) | 2 (33.3) |
|
| 2 | 0 (0.0) | 1 (16.7) |
|
| 3 | 0 (0.0) | 1 (16.7) |
|
| BMI
(kg/m2) | 20.64
(17.85–27.39) | 20.98
(18.03–25.10) | >0.99 |
| Diabetes
mellitus | 2 (33.3) | 1 (16.7) | >0.99 |
| Background liver
disease |
|
|
|
| HCV | 1 (16.7) | 5 (83.3) | 0.08 |
| NBNC | 5 (83.3) | 1 (16.7) |
|
| Albumin (g/dl) | 3.8 (3.4–4.6) | 4.1 (2.1–4.2) | 0.62 |
| ALT (U/l) | 16 (9–26) | 28 (16–83) | 0.07 |
| AST (U/l) | 23 (17–29) | 52 (17–79) | 0.04 |
| Bilirubin
(mg/dl) | 0.6 (0.3–1.2) | 0.5 (0.3–1.1) | 0.63 |
| Platelet count
(×103/µl) | 185 (110–224) | 128 (58–298) | 0.22 |
| Prothrombin
activity (%) | 102 (86–120) | 92 (64–99) | 0.05 |
| White blood count
(×103/µl) | 5.1 (4.0–7.7) | 4.2 (3.3–6.9) | 0.19 |
| CRP (mg/dl) | 0.20
(0.01–0.82) | 0.04
(0.03–0.66) | 0.63 |
| ICGR15 | 9.4 (3.0–21.6) | 13.5
(4.9–44.0) | 0.36 |
| Primary
disease |
|
|
|
| Liver
metastasis | 3 (50.0) | 1 (16.7) | 0.54 |
|
HCC | 3 (50.0) | 5 (83.3) |
|
| Tumor size
(cm) | 2.4 (1.0–3.5) | 2.7 (2.5–5.0) | 0.25 |
| Tumor number |
|
|
|
|
Single | 5 (83.3) | 4 (66.7) | >0.99 |
|
Multiple | 1 (16.7) | 2 (33.3) |
|
| Operation
approach |
|
|
|
|
Open | 2 (33.3) | 3 (50.0) | >0.99 |
|
Laparoscopic | 4 (66.7) | 3 (50.0) |
|
| Operation
method |
|
|
|
| Partial
resection | 3 (50.0) | 4 (66.7) | >0.99 |
|
Anatomical resection | 3 (50.0) | 2 (33.3) |
|
| Number of
resection |
|
|
|
| Initial
resection | 5 (83.3) | 5 (83.3) | >0.99 |
|
Repeated resection | 1 (16.7) | 1 (16.7) |
|
| Operation time
(min) | 212 (86–313) | 241 (95–279) | >0.99 |
| Bleeding (ml) | 10 (10–390) | 292 (10–1,022) | 0.06 |
| PHLF |
|
|
|
| A | 1 (16.7) | 0 (0.0) | >0.99 |
| B | 0 (0.0) | 1 (16.7) |
|
| Negative | 5 (83.3) | 5 (83.3) |
|
|
SSI |
|
|
|
| Positive
(organ/space) | 0 (0.0) | 1 (16.7) | >0.99 |
|
Negative | 6 (100.0) | 5 (83.3) |
|
| Complication |
|
|
|
|
Pneumonia | 0 | 2 (33.3) |
|
|
Refractory pleural
effusion | 0 | 1 (16.7) |
|
| Abscess
formation | 0 | 1 (16.7) |
|
|
Abdominal bleeding | 0 | 1 (16.7) |
|
| Portal
thrombus | 0 | 1 (16.7) |
|
| Hospital stay
(days) | 8 (7–12) | 15 (12–50) | <0.01 |
Complications
Complications occurred in 6 patients with refractory
pleural effusion, intra-abdominal abscess, intra-abdominal bleeding
which required blood transfusion without invasive treatment and
portal thrombus each occurring in 1 patient, and 2 patients
developing pneumonia. The SSI of organ/space occurred in 1 patient
with complication and PHLF occurred in 1 no complication patient
with Grade A and 1 complication patient of Grade B. The median
postoperative hospital stay was 8 and 15 days in no complication
and complication patients, respectively (P<0.01).
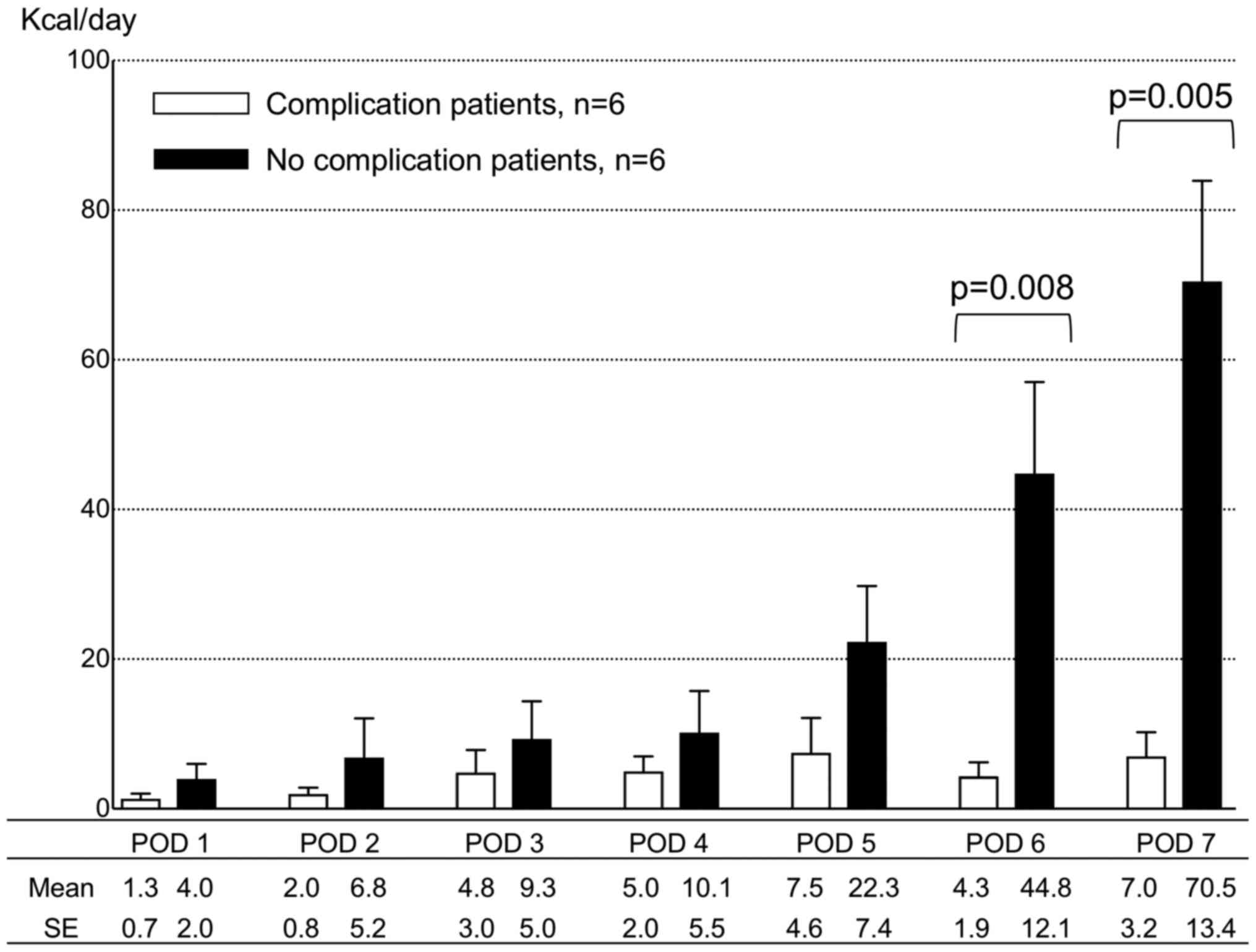
Physical activity level
All 12 patients had their physical activity measured
by accelerometer. Fig. 1 presents a
transitive graph of activity level in patients with and without
complications. Patients with complications exhibited lower physical
activities from POD 1 than patients without complications; however,
there was no statistically significant difference in the physical
activity level between the 2 groups until POD 5. The physical
activity level continuously accelerated in patients without
complication following POD 6. Conversely, patients with
complication did not exhibit increased physical activity levels
following POD 6. Significant differences were observed in physical
activity level following POD 6 between patients with and without
complications (P<0.01).
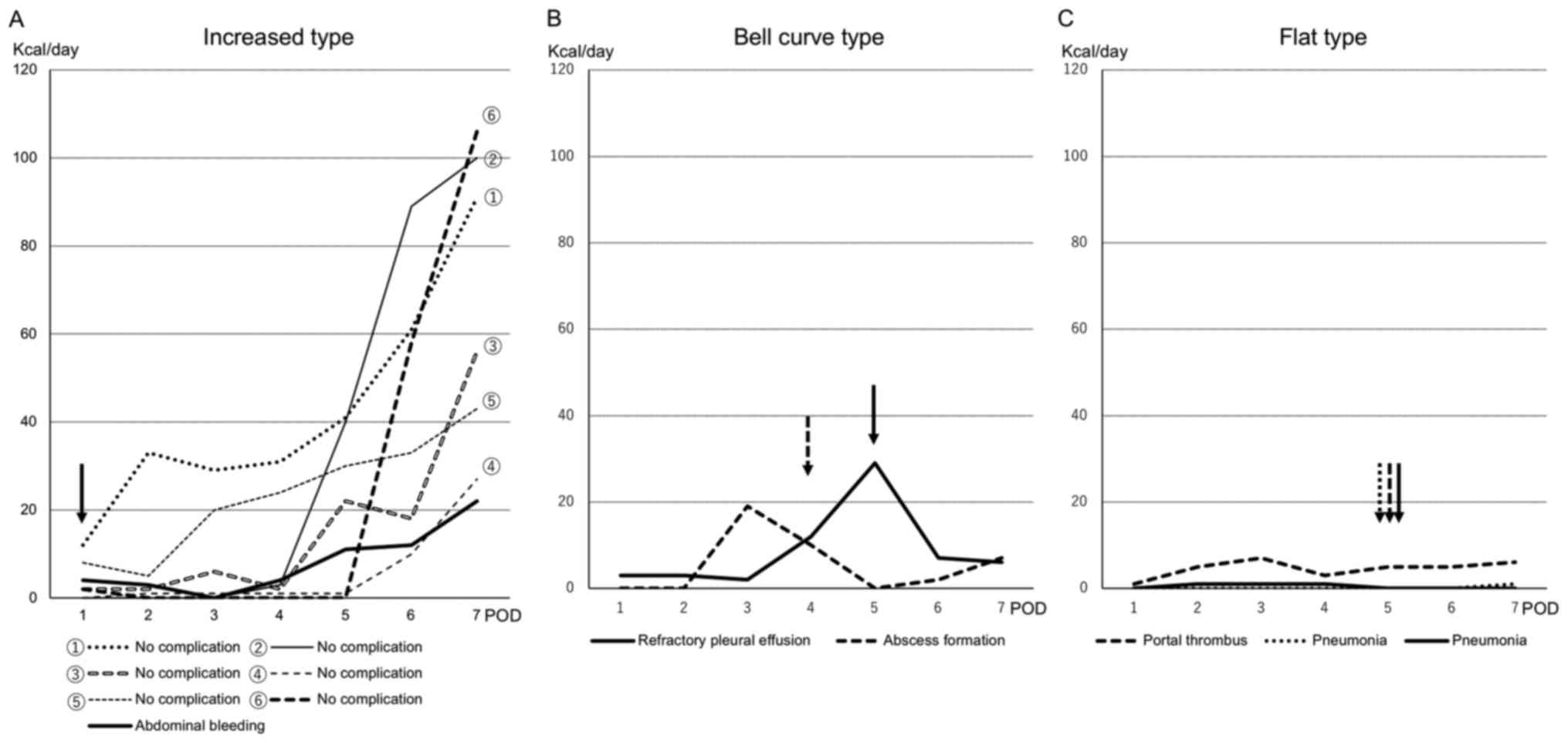
Types of physical activity change
Details of individual activity level are presented
in Fig. 2. The alterations in
patients' physical activity level were divided into 3 types:
Increased type, bell curve type and flat type. The increased type
included 6 patients of normal postoperative course and 1 patient
with postoperative abdominal bleeding at POD 1 (Fig. 2A). The bell curve type included 2
patients with postoperative complications who had intra-abdominal
abscess at POD 5 and refractory pleural effusion at POD 4 (Fig. 2B). The flat type included 2 patients
with pneumonia and 1 patient with portal thrombus at POD 5
(Fig. 2C).
Discussion
Acceleration sensors automatically detect a
patient's number of steps, moving distance, burned calories,
activity time and sleep time. Certain accelerometers can
distinguish the type of exercise (including slow walking, fast
walking, running, desk work and bicycle). In the present study,
patients without complications demonstrated that the physical
activity level gradually increased and quadratic functional
increase was observed until discharge, whereas patients with
complications demonstrated that the physical activity level was
gently decreased in the postoperative course.
The aim of the present study was to evaluate the
usefulness of the accelerometer to predict postoperative
complications following hepatic resection. Although the present
study was preliminary in nature, the change in postoperative
physical activity level following POD 6 demonstrated significant
difference depending on the presence or absence of complications.
The occurrence of postoperative complications observed prior to POD
5 might lead to the decreased physical activity level; therefore,
these findings failed to elucidate whether postoperative physical
activity level measured by accelerometer might predict
postoperative complications. However, 3 representative types of
postoperative physical activity changes were proposed by the
occurrence of postoperative course recorded by accelerometer as a
surrogate marker for postoperative complications.
These 3 types of postoperative physical activity
change were as follows: i) increased type, where a continuous
elevation of physical activity level which may include patients
without complication; ii) bell curve type, where the physical
activity level decreases in the middle period of postoperative
course, which may include postoperative complications such as
abdominal abscess, bile leak, SSI or effusion. In this type, the
physical activities decreased following the occurrence of
complications. The occurrence of complications may influence the
reduction in physical activities. Therefore, if the amount of
physical activity suddenly decreases, complications should be
treated as soon as possible and iii) flat type, where low physical
activity level continues following surgery. The flat type may
include respiratory complications, especially pneumonia. In this
type, the physical activities are never elevated during the
observational period.
Although it is not yet clear due to the small number
of patients, the occurrence of pneumonia may be associated with low
degree of physical activity in the early postoperative period.
Therefore, prevention of pneumonia appeared to require early
upregulation of activity level following surgery (25,26).
The limitations of the present study were the small
sample size, use of a single center and including some young
patients. However, it was demonstrated that the postoperative
physical activity level may be a surrogate marker for postoperative
complications. This provides rationale for larger sample studies by
measuring the postoperative physical activity level. As a future
prospect, via a large size study, it may be possible to conduct
prediction and prevention of complications depending on the
changing pattern of the degree of postoperative physical activity,
and it may be possible to determine the schedule of quantity,
intensity and time of postoperative rehabilitation to tailor
patient management. In addition, it may be possible to demonstrate
whether daily and postoperative activity levels lead to differences
between young and elderly patients, and whether the influence of
the physical activity levels on postoperative complications differs
depending on patient's age via larger sample studies.
Furthermore, it is generally considered that a
greater amount of daily physical activity reduces the likelihood of
postoperative complications. Previously, a number of reports have
demonstrated that a few weeks of a cardiopulmonary rehabilitation
program prior to surgery reduces postoperative complications
(27–29), and a randomized controlled trial is
currently ongoing (30). Therefore,
it is important to elucidate the association between the degree of
daily physical activity prior to operation and postoperative
complications. The authors are currently preparing validation of
the prediction of complications depending on the changing pattern
of postoperative physical activity. In addition, a further study is
planned to clarify the association between preoperative physical
activity and postoperative complications with a larger number of
patients.
In conclusion, the degree of postoperative physical
activity measured using an accelerometer may be strongly associated
with the postoperative complications following hepatic resection.
These findings provide rationale for future studies to evaluate the
association between postoperative physical activity levels using an
accelerometer and postoperative complications using a larger sample
size.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
HI designed the study and wrote the initial draft of
the manuscript. TS and MT contributed to the analysis and
interpretation of data, and assisted in the preparation of the
manuscript. HiM, NK, HaM, TM and SK contributed to the data
collection and interpretation, and critically reviewed the
manuscript. The final version of the manuscript was approved by all
authors.
Ethics approval and consent to
participate
The present study conformed to the Clinical Research
Guidelines and was approved by the Ethics Committee of Shiga
University of Medical Science (approval no. 29-191; Otsu, Japan).
Written informed consent was obtained from all patients or members
of their families prior to surgery.
Patient consent for publication
Written informed consent was obtained from all
patients or members of their families prior to surgery.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ASA classification
|
American Society of Anesthesiologists
Physical Status classification system
|
|
ECOG Performance status
|
Eastern Cooperative Oncology Group
Performance status
|
|
BMI
|
body mass index
|
|
HCV
|
positive of hepatitis C antibody
|
|
NBNC
|
negative of hepatitis B surface
antigen and hepatitis C antibody
|
|
AST
|
aspartate aminotransferase
|
|
ALT
|
alanine aminotransferase
|
|
CRP
|
C-reactive protein
|
|
ICGR15
|
indocyanine green retention rate at 15
min
|
|
HCC
|
hepatocellular carcinoma
|
|
PHLF
|
post-hepatectomy liver failure
|
|
SSI
|
surgical site infection
|
References
|
1
|
Reddy SK, Barbas AS, Turley RS, Gamblin
TC, Geller DA, Marsh JW, Tsung A, Clary BM and Lagoo-Deenadayalan
S: Major liver resection in elderly patients: A multi-institutional
analysis. J Am Coll Surg. 212:787–795. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Poon RT, Fan ST, Lo CM, Liu CL, Ngan H, Ng
IO and Wong J: Hepatocellular carcinoma in the elderly: Results of
surgical and nonsurgical management. Am J Gastroenterol.
94:2460–2466. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wu CC, Chen JT, Ho WL, Yeh DC, Tang JS,
Liu TJ and P'eng FK: Liver resection for hepatocellular carcinoma
in octogenarians. Surgery. 125:332–338. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Shirabe K, Kajiyama K, Harimoto N, Gion T,
Tsujita E, Abe T, Wakiyama S, Nagaie T and Maehara Y: Early outcome
following hepatic resection in patients older than 80 years of age.
World J Surg. 33:1927–1932. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kaibori M, Matsui K, Ishizaki M, Saito T,
Kitade H, Matsui Y and Kwon AH: Hepatic resection for
hepatocellular carcinoma in the elderly. J Surg Oncol. 99:154–160.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mirici-Cappa F, Gramenzi A, Santi V,
Zambruni A, Di Micoli A, Frigerio M, Maraldi F, Di Nolfo MA, Del
Poggio P, Benvegnù L, et al: Treatments for hepatocellular
carcinoma in elderly patients are as effective as in younger
patients: A 20-year multicentre experience. Gut. 59:387–396. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Nanashima A, Abo T, Nonaka T, Fukuoka H,
Hidaka S, Takeshita H, Ichikawa T, Sawai T, Yasutake T, Nakao K and
Nagayasu T: Prognosis of patients with hepatocellular carcinoma
after hepatic resection: Are elderly patients suitable for surgery?
J Surg Oncol. 104:284–291. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nozawa A, Kubo S, Takemura S, Sakata C,
Urata Y, Nishioka T, Kinoshita M, Hamano G, Uenishi T and Suehiro
S: Hepatic resection for hepatocellular carcinoma in super-elderly
patients aged 80 years and older in the first decade of the 21st
century. Surg Today. 45:851–857. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Owens WD, Felts JA and Spitznagel EL Jr:
ASA physical status classifications: A study of consistency of
ratings. Anesthesiology. 49:239–243. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Haynes SR and Lawler PG: An assessment of
the consistency of ASA physical status classification allocation.
Anaesthesia. 50:195–199. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ranta S, Hynynen M and Tammisto T: A
survey of the ASA physical status classification: Significant
variation in allocation among Finnish anaesthesiologists. Acta
Anaesthesiol Scand. 41:629–632. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mak PH, Campbell RC and Irwin MG; American
Society of Anesthesiologists, : The ASA physical status
classification: Inter-observer consistency. American Society of
Anesthesiologists. Anaesth Intensive Care. 30:633–640.
2002.PubMed/NCBI
|
|
13
|
Oken MM, Creech RH, Tormey DC, Horton J,
Davis TE, McFadden ET and Carbone PP: Toxicity and response
criteria of the Eastern Cooperative Oncology Group. Am J Clin
Oncol. 5:649–655. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Westerterp KR: Assessment of physical
activity: A critical appraisal. Eur J Appl Physiol. 105:823–828.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bankoski A, Harris TB, McClain JJ, Brychta
RJ, Caserotti P, Chen KY, Berrigan D, Troiano RP and Koster A:
Sedentary activity associated with metabolic syndrome independent
of physical activity. Diabetes Care. 34:497–503. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Colley RC, Garriguet D, Janssen I, Craig
CL, Clarke J and Tremblay MS: Physical activity of Canadian
children and youth: Accelerometer results from the 2007 to 2009
Canadian Health Measures Survey. Health Rep. 22:15–23.
2011.PubMed/NCBI
|
|
17
|
Healy GN, Matthews CE, Dunstan DW, Winkler
EA and Owen N: Sedentary time and cardio-metabolic biomarkers in US
adults: NHANES 2003–06. Eur Heart J. 32:590–597. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Stamatakis E, Hamer M, Tilling K and
Lawlor DA: Sedentary time in relation to cardio-metabolic risk
factors: Differential associations for self-report vs accelerometry
in working age adults. Int J Epidemiol. 41:1328–1337. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cook DJ, Thompson JE, Prinsen SK, Dearani
JA and Deschamps C: Functional recovery in the elderly after major
surgery: Assessment of mobility recovery using wireless technology.
Ann Thorac Surg. 96:1057–1061. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Harding PA, Holland AE, Hinman RS and
Delany C: Physical activity perceptions and beliefs following total
hip and knee arthroplasty: A qualitative study. Physiother Theory
Pract. 31:107–113. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kumahara H, Schutz Y, Ayabe M, Yoshioka M,
Yoshitake Y, Shindo M, Ishii K and Tanaka H: The use of uniaxial
accelerometry for the assessment of physical-activity-related
energy expenditure: A validation study against whole-body indirect
calorimetry. Br J Nutr. 91:235–243. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Clavien PA, Barkun J, de Oliveira ML,
Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J,
Slankamenac K, Bassi C, et al: The Clavien-Dindo classification of
surgical complications: Five-year experience. Ann Surg.
250:187–196. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Rahbari NN, Garden OJ, Padbury R,
Brooke-Smith M, Crawford M, Adam R, Koch M, Makuuchi M, Dematteo
RP, Christophi C, et al: Posthepatectomy liver failure: A
definition and grading by the International Study Group of Liver
Surgery (ISGLS). Surgery. 149:713–724. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Mangram AJ, Horan TC, Pearson ML, Silver
LC and Jarvis WR: Guideline for prevention of surgical site
infection, 1999. Centers for disease control and prevention (CDC)
hospital infection control practices advisory committee. Am J
Infect Control. 27:97–132; quiz 133–134; discussion 196. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Castelino T, Fiore JF Jr, Niculiseanu P,
Landry T, Augustin B and Feldman LS: The effect of early
mobilization protocols on postoperative outcomes following
abdominal and thoracic surgery: A systematic review. Surgery.
159:991–1003. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Chumillas S, Ponce JL, Delgado F, Viciano
V and Mateu M: Prevention of postoperative pulmonary complications
through respiratory rehabilitation: A controlled clinical study.
Arch Phys Med Rehabil. 79:5–9. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Li C, Carli F, Lee L, Charlebois P, Stein
B, Liberman AS, Kaneva P, Augustin B, Wongyingsinn M, Gamsa A, et
al: Impact of a trimodal prehabilitation program on functional
recovery after colorectal cancer surgery: A pilot study. Surg
Endosc. 27:1072–1082. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Gillis C, Li C, Lee L, Awasthi R, Augustin
B, Gamsa A, Liberman AS, Stein B, Charlebois P, Feldman LS and
Carli F: Prehabilitation versus rehabilitation: A randomized
control trial in patients undergoing colorectal resection for
cancer. Anesthesiology. 121:937–947. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chan KE, Pathak S, Smart NJ, Batchelor N
and Daniels IR: The impact of cardiopulmonary exercise testing on
patients over the age of 80 undergoing elective colorectal cancer
surgery. Colorectal Dis. 18:578–585. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Onerup A, Angenete E, Bock D, Börjesson M,
Olsén Fagevik M, Gillheimer Grybäck E, Skullman S, Thörn SE,
Haglind E and Nilsson H: The effect of pre- and post-operative
physical activity on recovery after colorectal cancer surgery
(PHYSSURG-C): Study protocol for a randomised controlled trial.
Trials. 18:2122017. View Article : Google Scholar : PubMed/NCBI
|