Introduction
Clavicle fractures are common in clinics and the
incidence rate is ~2.6–12% of all fractures (1). Allman (2) divided clavicle fractures into three
types: The distal clavicle fracture, the middle clavicle fracture,
and the medial-end clavicle fracture. Among these, medial-end
clavicle fractures are rare and make up only 2–10% (3–6) of all
clavicle fractures; this type of fracture is usually caused by
direct, high-energy injury. The medial-end clavicle fracture is
rare and conservative treatment is generally used in view of the
complex anatomy of the proximal clavicle and the risk of injury to
important neurovascular organs, however, the effect of conservative
treatment is not ideal, which has led to increasing focus on the
potential of surgical treatment. However, there are no unified
recognized standards or specifications for the methods and
materials of internal fixation. In addition, there is no fixation
material specifically designed for medial-end clavicle fractures.
Currently, internal fixators for proximal clavicle fractures
include Kirschner wire, steel wire, screws and various types of
steel plates.
The shape of the inverse distal clavicle anatomic
locking plate is similar to the form of the medial-end clavicle.
The design of double row locking holes in the distal part of the
plate can fix more layers of cortex and strengthen the stability of
fixation. Additionally, the plate can satisfactorily adhere to the
bone through molding. Inspired by this, the present study treated
medial-end clavicle fractures using a method of inversing the
distal clavicle anatomic locking plate. The therapeutic effects
were found to be satisfactory.
Patients and methods
A total of six cases of medial-end clavicle fracture
were treated by the method of inverting the distal clavicle
anatomic locking plate between September 2013 and December 2015 at
the Affiliated Hospital of Shandong University of Traditional
Chinese Medicine (Jinan, China). All patients signed written
informed consent prior to enrolment in the study and the cases
conformed to the surgical indication of a displacement of >1 cm
between the fragment ends. The patient demographics are summarized
in Table I. The patients were
classified based on the Throckmorton type (5). All cases were freshly-closed fractures
and were caused by direct injury. Regular postoperative follow-ups
were performed and the therapeutic efficacy was systematically
evaluated by referencing the Rockwood score standard and the
Disability of the Arm, Shoulder and Han (DASH) score standard
(7,8).
 | Table I.Select patient demographics and
operative outcomes. |
Table I.
Select patient demographics and
operative outcomes.
| Characteristic | n |
|---|
| Total number of
patients | 6 |
| Average age, years
(range) | 46.3±10.6
(24–66) |
| Sex |
|
| Male | 5 |
|
Female | 1 |
| Affected side |
|
| Left | 2 |
|
Right | 4 |
| Throckmorton
type |
|
| Type
A | 1 |
| Type
B | 0 |
| Type
C | 2 |
| Type
D | 3 |
| Type
E | 0 |
| Average length of
follow-up, months (range) | 12.0±2.2 (12–14) |
| Mean fluoroscopic
frequency, (range) | 5 (4–8) |
| Mean operative time,
min (range) | 48.4±6.7 (45–65) |
| Average time to
healed X-ray, months (range) | 3.5 (2.9–6.2) |
| Functional
recovery |
|
|
Excellent | 5 |
| Good | 1 |
|
General | 0 |
| Poor | 0 |
| DASH
score (range) | 8.6±1.2 (7–9) |
When the patients were hospitalized, preoperative
routine examinations were performed. First of all, the relevant
departments were consulted to actively treat medical diseases and
eliminate the contraindication of surgery due to presentation of
coronary heart disease, hypertension or diabetes. Subsequently, the
surgical plan was developed following department discussion, and
antibiotics were administered to patients 30 min prior to surgery.
Finally, surgery was performed for each patient when all these
preparations had been completed.
A circuit nurse performed urethral catheterization
for the patient, and the patient was then placed in the beach chair
position to adequately expose the surgical area following the
successful administration of brachial plexus anesthesia (with local
anesthesia when necessary). The skin, subcutaneous tissue, and
fascia were cut in turn, and the periosteum was finitely stripped
subsequent to making an 8–10 cm skin incision. The incision
accorded to the direction of clavicle centered on the fracture end.
The fracture was reset anatomically, following which the inversely
implanted distal clavicle anatomic locking plate (Jiangsu Hopromed
Co., Ltd., Jiangsu, China; http://www.js-hp.com) was used to fix the broken
fracture end. The plate was carefully shaped based on the different
clavicle forms so it adhered to the surface of the bone without a
gap. The broken fracture end of type D was first fixed using a lag
screw (Jiangsu Hopromed Co., Ltd.). Three locking screws (Jiangsu
Hopromed Co., Ltd.) were placed on the far-end of the fracture and
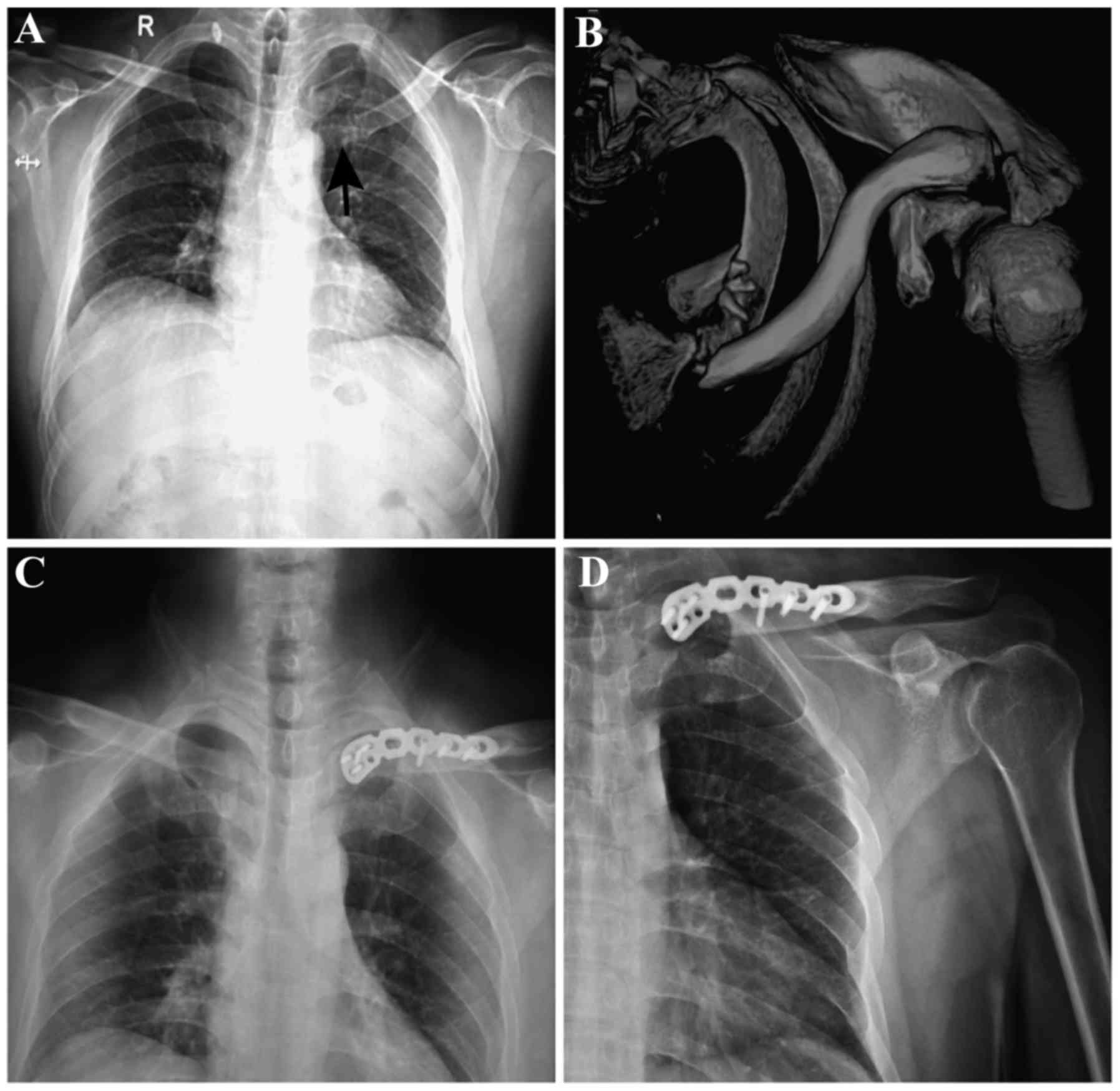
2–3 locking screws were placed on the near-end (Fig. 1A-C). The plate was implanted across
the sternoclavicular joint when there was insufficient space in the
near-end of the fracture to implant 2–3 locking screws. Two locking
screws were placed on the manubrium sterni in order to enhance
firmness and stability in this situation. Care was required to
drill holes and avoid the screws passing through the contralateral
cortex, as the heart, vessels and other important organs are
located in the deep of manubrium sterni. Unstable fracture
fragments were bundled with double surgical sutures, and artificial
bone (Shanghai Anjiu Biotechnology Co., Ltd., Shanghai, China) was
grafted in the bone defection to accelerate fracture healing. An
X-ray examination was performed to appraise the reduction and the
length of the screws. Finally, the incision was closed in the usual
manner.
Postoperatively, all patients were given antibiotics
(Cefotiam, Zhejiang Yongning Pharmaceutical Co., Ltd., Taizhou,
China) only once to prevent infection, and the extremity of the
forearm was immobilized in a sling for 2 weeks. This surgical
method allowed excellent fixation and early mobilization under the
guidance of the doctor. Patients gradually performed exercises
using the elbow, wrist and hand as comfort would allow. After 4
weeks, the patients began to activate the shoulder in all
directions and progressively increased the range. Normal
activities, including sports and weight-bearing exercises, were not
allowed until fracture union had been completed. Postoperative
follow-up was periodically performed to evaluate the shoulder
function and observe complications including incision infection,
nerve vascular injury, chest injury and nonunion. A final
assessment of shoulder function was assessed based on the Rockwood
score standard and DASH score standard. The Rockwood score ranges
between 0 and 15 with values 13–15 representing excellent, 10–12
representing good, 7–9 representing general, and <7 representing
poor. The DASH score ranges between 0 and 100 with a higher score
indicating a higher level of functional disability.
The institutional review boards and ethics
committees of the Affiliated Hospital of Shandong University of
Traditional Chinese Medicine approved the present study. All six
patients provided consent for the publication of the present
report.
Results
In the six cases, none of the patients had their
sternoclavicular joint fixed; it was preferable to avoid fixing the
sternoclavicular joint, if possible, as it is a fretting joint. The
six patients received a postoperative follow-up, which ranged
between 10 and 14 months with an average of 12 months. Osseous
healing and functional recovery were observed (Fig. 1D) without incision infection, nerve
vascular injury, chest injury, nonunion or other complications.
According to the Rockwood and DASH score standards, evaluation of
the curative effect showed that five cases were ‘excellent’ and one
case was ‘good’, with an associated rate for achieving good or
excellent outcomes of 100%. All of the DASH scores were <10 and
the average score was 8.6±1.2.
Discussion
The medial-end clavicle fracture is a relatively
rare injury and accounts for only 2–10% of all clavicle fractures.
Throckmorton and Kuhn (5) divided
medial-end clavicle fractures into five types: Type A (transverse
fracture), type B (oblique intra-articular fracture), type C
(oblique extra-articular fracture), type D (comminuted fracture),
and type E (avulsion fracture). These fractures have traditionally
been treated conservatively to avoid damage to the deep tissues
during surgery, including the brachial plexus, subclavian vein,
axillary vein, and apex pulmonis. However, conservative treatment
of these fractures can lead to serious complications, including
nonunion, malunion, and functional disability (9). With continuous improvement at the
clinical level, surgical methods, including open reduction and
internal fixation, partial claviculectomy, and fusion of the
sternoclavicular joints, have been reported in the available
literature (3,5,10,11). Due
to the high rate of the postoperative complications, partial
claviculectomy and fusion of the sternoclavicular joints have
gradually been avoided. By contrast, open reduction and internal
fixation have been considered to be the preferred method (12). However, there are no unified
recognized standards or specifications for the methods and
materials of the internal fixation. In addition, there is no
fixation material specifically designed for medial-end clavicle
fractures.
Bartonícek et al (13) reported that they obtained a good
curative effect by using cerclage wires to treat five cases, and
used the visual analogue scale score and the DASH score to evaluate
the effects. In another study, Oe et al concluded that the
locking T-plate and DCP plate were effective (14). They treated 10 medial-end clavicle
fractures and all patients gained osseous healing without
complications. Correa et al (15) showed that using a reconstruction
plate to treat medial-end clavicle fractures made it possible to
obtain satisfactory clinical effects. Sidhu et al, Ding
et al and Sloan et al used clavicular hook plates and
contralateral lateral clavicle locking plates to treat medial-end
clavicle fractures (4,16,17). All
achieved good effects on postoperative follow-up. These materials
for internal fixation were effective, however, the sample size was
small and no control study was designed in these clinical reports.
In addition, the fixed strength and stability of the T-plate are
relatively poor and it is easy to cause stress concentration around
the sternoclavicular joint, causing plate fracture. The clavicular
hook plate has poor ability to resist distortion and it is easy to
penetrate through the sternum; the hook penetrating through the
sternum will damage the internal organs. The fixation strength of
Kirschner wire and cerclage wire are too weak to fix fractures. In
addition, full exposure in the surgical field is required when
using reconstruction plate to treat fractures, and the plate is too
difficult to shape. Accordingly, the reconstruction plate may
damage the blood supply and extend surgery time.
In the present study, six cases of medial-end
clavicle fractures were treated using a method of inverting the
distal clavicle anatomic locking plate, and satisfactory clinical
effects were obtained. It is important to pay attention to the
following points during surgery: Firstly, adequate locking screws
require placement on the far-end and near-end of the fracture to
ensure stability; the plate is implanted across the
sternoclavicular joint when there is insufficient space in the
near-end of the fracture to implant 2–3 locking screws; 1–2 locking
screws are placed on the manubrium sterni in order to enhance
firmness and stability in this particular situation; care is
required in drilling holes and to avoid the screws passing through
the contralateral cortex as the heart, vessels and other important
organs are located in the deep of manubrium sterni. Secondly, the
broken fracture end of type C and type D fractures require fixation
using a lag screw, with unstable fracture fragments bundled with
double surgical sutures. These methods can increase the strength of
the fixation and promote fracture healing. Thirdly, it is
recommended that artificial bone is grafted in the bone defection
to accelerate fracture healing. Finally, it is necessary to remove
this plate as soon as possible following fracture healing in order
to avoid fracture and reject reaction of plate.
In conclusion, the clinical effect of the treatment
of medial-end clavicle fractures using the method of inverting the
distal clavicle anatomic locking plate was reliable and the
functional recovery of patients was good. However the sample size
was small and no control study was designed in the present report
to support the conclusion, therefore, the results only provide a
reference for the treatment. It is necessary to design a specific
locking plate for medial-end clavicle fractures. Therefore, this
method is worthy of further promotion, and the development of a
specific locking plate for medial-end clavicle fracture is
required.
Acknowledgements
The authors thank Ms. Xiaodi Li, Nanjing University
of Traditional Chinese Medicine (Nanjing, China) for her linguistic
advice.
Funding
Not applicable.
Availability of data and materials
The datasets used and/or analysed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
W-PX and Y-KZ performed the postoperative follow-up
and were major contributors in writing the manuscript. R-XB guided
the design and implementation of the surgery. Y-HC analysed and
interpreted the data. S-LW and H-HX took part in the surgery and
processed the images in the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The institutional review boards and ethics
committees of the Affiliated Hospital of Shandong University of
Traditional Chinese Medicine (Nanjing, China) approved the present
study.
Patient consent for publication
All six patients provided consent for the
publication of the present report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kihlström C, Möller M, Lönn K and Wolf O:
Clavicle fractures: Epidemiology, classification and treatment of
2422 fractures in the Swedish Fracture Register; an observational
study. BMC Musculoskelet Disord. 18:822017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Allman FL Jr: Fractures and ligamentous
injuries of the clavicle and its articulation. J Bone Joint Surg
Am. 49:774–784. 1967. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Smelt J, Khakha RS, Harrison-Phipps K,
Richards A and Bille A: An isolated traumatic medial third
clavicular fracture requiring surgical fixation. Ann Thorac Surg.
103:e297–e298. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sidhu VS, Hermans D and Duckworth DG: The
operative outcomes of displaced medial-end clavicle fractures. J
Shoulder Elbow Surg. 24:1728–1734. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Throckmorton T and Kuhn JE: Fractures of
the medial end of the clavicle. J Shoulder Elbow Surg. 16:49–54.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vander Meijden OA, Gaskill TR and Millett
PJ: Treatment of clavicle fractures: Current concepts review. J
Shoulder Elbow Surg. 21:423–429. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shetty SK, Chandran R, Ballal A, Mathias
LJ, Hegde A and Shetty A: To operate or not to operate the
mid-shaft fractures of the clavicle: A comparative study of
functional outcomes of the two methods of management. J Clin Diagn
Res. 11:RC01–RC03. 2017.
|
|
8
|
Rockwood CA Jr, Groh GI, Wirth MA and
Grassi FA: Resection arthroplasty of the sternoclavicular joint. J
Bone Joint Surg Am. 79:387–393. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Poggetti A, Novi M, Rosati M, Battistini
P, Parchi P and Lisanti M: Unusual medial-end clavicle fracture
combined with double disruption of the superior shoulder suspensory
complex (SSSC): A case report in triathlon Athlete. J Orthop Case
Rep. 6:19–21. 2016.PubMed/NCBI
|
|
10
|
Bourghli A and Fabre A: Proximal end
clavicle fracture from a parachute jumping injury. Orthop Traumatol
Surg Res. 98:238–241. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Teng HG and Liu AL: Partial claviculectomy
after non-union of proximal clavicle fracture. BMJ Case Rep.
2013(pii): bcr20130088742013.PubMed/NCBI
|
|
12
|
Koch MJ and Wells L: Proximal clavicle
physeal fracture with posterior displacement: Diagnosis, treatment,
and prevention. Orthopedics. 35:e108–e111. 2012.PubMed/NCBI
|
|
13
|
Bartonícek J, Fric V and Pacovsk V:
Displaced fractures of the medial end of the clavicle: Report of
five cases. J Orthop Trauma. 24:e31–e35. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Oe K, Gaul L, Hierholzer C, Woltmann A,
Miwa M, Kurosaka M and Buehren V: Operative management of
periarticular medial clavicle fractures: Report of 10 cases. J
Trauma. 72:E1–E7. 2012.
|
|
15
|
Correa MC, Gonçalves LB, Vilela JC, Leonel
IL, Costa LP and de Andrade RP: Extra-articular fracture of the
medial end of the clavicle associated with type IV
acromioclavicular dislocation: Case report. Rev Bras Orthop.
46:596–601. 2011. View Article : Google Scholar
|
|
16
|
Ding M, Ni J, Hu J and Song D: Rare
complication of clavicular hook plate: Clavicle fracture at the
medial end of the plate. J Shoulder Elbow Surg. 20:e18–e20. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sloan AG, Howcroft D and Wykes PR:
Operative treatment of medial clavicle fractures: an alternative
suigicle technique. Injury Extra. 39:270–272. 2008. View Article : Google Scholar
|