Introduction
Currently, infectious encephalitis belongs to
virosis of the central nervous system and is common in child
patients (1). Bacterium, virus,
fungus and mycoplasma can lead to viral encephalitis with
inflammatory lesions, and the most prevalent encephalitis mainly
consists of viral encephalitis. The child patients' main symptoms
include headache, fever and vomiting, and child patients with
severe viral encephalitis suffer from stress injury (2–4). Stress
response is a kind of non-specific systemic reaction occurring in
organisms, and mild stress response can improve the adaptability of
human body, while excessive stress response exacerbates function
impairment of the human body (5).
Clinical treatment methods for viral encephalitis
have obtained unfavourable effects and mainly aim at clinical
symptoms of child patients. When it is clinically found that the
brain environment disorder of child patients with viral
encephalitis leads to the corresponding changes in
electroencephalograms (EEGs), changes in disease conditions of such
child patients can be analyzed based on changes in EEG. However,
response results of different EEGs vary, and ambulatory
electroencephalogram (AEEG) has higher specificity and diagnostic
value than regular electroencephalogram (REEG) (6–8).
Therefore, this study aims to evaluate the prognosis of child
patients with viral encephalitis through AEEG and REEG.
Patients and methods
Clinical information
Child patients who were primarily diagnosed with
viral encephalitis 3 days after being admitted to Yantaishan
Hospital of Yantai (Yantai, China) from May 2010 to July 2014 were
selected to receive 24 h computed tomography (CT), magnetic
resonance imaging (MRI) and cerebrospinal fluid (CSF) examinations,
and the diagnosis criteria for viral encephalitis were proposed
with reference to literature (5): i)
patients with clinical signs of brain parenchyma damage due to
virus; ii) patients with inflammatory changes in CSF; iii) patients
without space-occupying lesion signs in brain CT and MRI; iv)
patients with nervous system disease, multiple sclerosis
neurological disease, and neurologic demyelinating disease were
excluded. There were 94 child patients with viral encephalitis, in
total. Of them, there were 53 males and 41 females aged 4–11 years
and an average age of 7.40±1.71 years; the disease course lasted
1–3 days with an average of 1.85±0.80 days. They were randomly
divided into the REEG group (n=47) and AEEG group (n=47) by
contrast, and the two groups did not have statistical differences
in the information on age and sex of patients. Families and
guardians of all child patients signed the informed consent. The
study was approved by the Ethics Committee of Yantaishan Hospital
of Yantai.
EEG monitoring
REEG group adopted a 16-lead conventional
electroencephalograph (Dantec Dynamics, Skovlunde, Denmark), and
the electrodes were placed on scalp strictly in accordance with the
international 10–20% system to conduct regular monopolar and
bipolar lead tracing as per 30 min/time. Moreover, the experiment
was induced by coordinating routine eye-closing reaction and
overventilation of patients. The AEEG group used an 8-lead
ambulatory electroencephalograph (NCC, Shanghai, China), and the
electrodes were placed on scalp strictly in accordance with the
international 10–20% system to conduct regular monopolar lead
tracing for 24 h real-time monitoring.
Observation criteria and assessment
indicators
The abnormity rates of different types of EEGs
during hospitalization were identified. First of all, EEG
abnormities were analyzed with reference to Clinical
Electroencephalography (9). The
abnormity degree in this experiment was divided into three levels:
mild, moderate and severe. Mildly abnormal EEG mainly showed α wave
with middle-low amplitude θ wave and extremely few δ waves;
moderately abnormal EEG mainly presented middle-low amplitude θ
wave with active δ wave; severely abnormal EEG exhibited
high-amplitude θ wave and δ wave rhythmic activity. At last, the
hospitalization time, time of EEG restoring to normal and incidence
rates of clinical reoccurrence and sequela were calculated based on
results of different types of electroencephalograph. The prognoses
of child patients with normal and abnormal EEGs in the two groups
were analyzed. Furthermore, the changes in EEG of child patients
were analyzed to evaluate prognoses of child patients and clinical
values.
Statistical analysis
The data obtained in this study were statistically
analyzed with Statistical Product and Service Solutions (SPSS) 19.0
software package (SPSS Inc., Chicago, IL, USA), the measurement
data were expressed as mean ± standard error. The inter-group data
were tested using the Kolmogorov-Smirnov (K-S) method, and the
enumeration data were verified by Chi-square test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Comparison of abnormity rate between
AEEG and REEG
In the REEG group, 25 cases of EEG abnormity were
found with the abnormity rate of 53.2%, while in the AEEG group, 38
cases of EEG abnormity were found with the abnormity rate of 80.9%.
The comparison of abnormity rate between child patients in the REEG
and AEEG groups was statistically significant (P<0.05). The
comparison of abnormity rate between severe child patients in the
two groups was statistically significant (P<0.05). The
comparison of abnormity rates between mild and moderate child
patients in the two groups did not indicate statistical
significance (P>0.05) (Table
I).
 | Table I.Comparison of abnormity rate between
the AEEG and REEG groups. |
Table I.
Comparison of abnormity rate between
the AEEG and REEG groups.
|
| AEEG (n=47) | REEG (n=47) |
|
|
|---|
|
|
|
|
|
|
|---|
| EEG abnormity | n | Abnormity rate
(%) | n | Abnormity rate
(%) | χ2 | P-value |
|---|
| Mild | 7 | 14.9 | 6 | 12.8 | 0.089 | 0.765 |
| Moderate | 11 | 23.4 | 14 | 29.8 | 0.490 | 0.484 |
| Severe | 20 | 42.6 | 5 | 10.6 | 9.889 | 0.002 |
| Total | 38 | 80.9 | 25 | 53.2 | 6.931 | 0.004 |
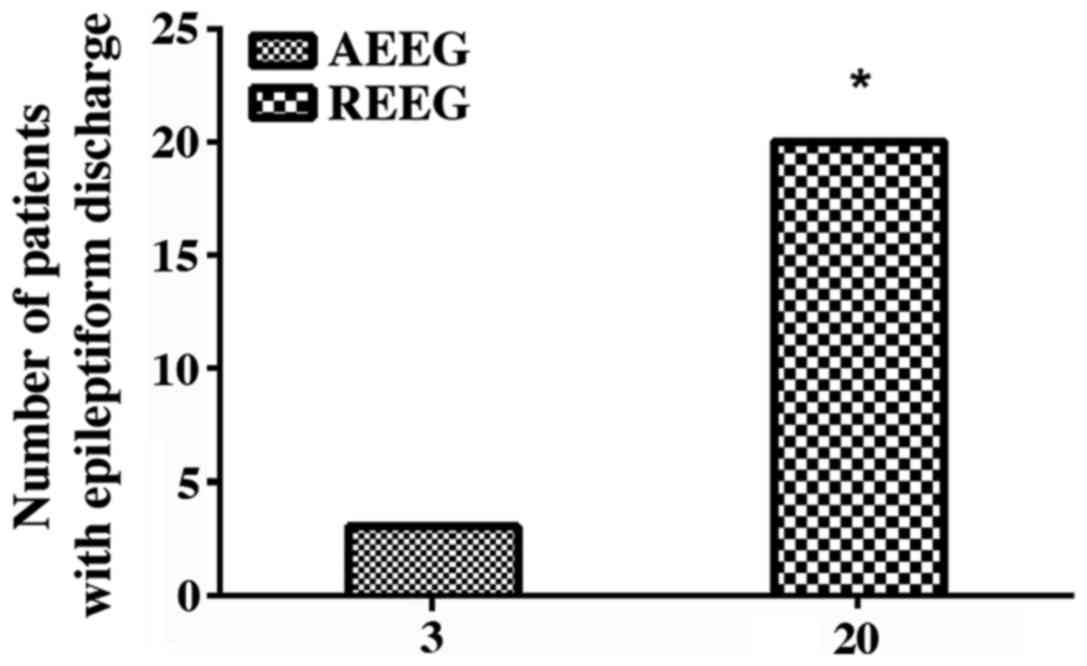
Comparison of epileptiform discharge
between the AEEG and REEG groups
In the REEG group, only 3 child patients with
epileptiform discharge were monitored with the detection rate of
6.4%. In the AEEG group, 20 cases of such child patients were
monitored with the detection rate of 42.6%. According to
statistical analysis, the two methods had a significant difference
(P<0.05) (Fig. 1).
Comparison of clinical indicators of
child patient EEG in the two groups
As the abnormal fluctuation of child patient EEGs
became more significant, the hospitalization time and time of EEG
restoring to normal were increased correspondingly. In the AEEG
group, they were substantially shortened, and statistically
different from those in the REEG group (P<0.001) (Table II).
 | Table II.Comparison of clinical indicators of
child patient EEG in the two groups. |
Table II.
Comparison of clinical indicators of
child patient EEG in the two groups.
| Groups | Abnormity degree of
EEG | AEEG group (d) | F-value | P-value | REEG group (d) | F-value | P-value |
|---|
| Hospitalization
time | Mild | 7.44±3.84 | 12.21 | <0.001 | 9.18±3.51 | 32.65 | <0.001 |
|
| Moderate | 12.61±4.58 |
|
| 17.61±5.14 |
|
|
|
| Severe | 19.17±4.97 |
|
| 26.51±4.21 |
|
|
| Time of EEG
restoring | Mild | 13.45±3.74 | 17.39 | <0.001 | 18.37±4.67 | 4.35 | 0.026 |
| to normal | Moderate | 18.57±4.28 |
|
| 23.49±4.87 |
|
|
|
| Severe | 24.16±5.27 |
|
| 28.67±5.62 |
|
|
Comparison of prognoses among child
patients
According to the study, in the AEEG group, the
incidence rate of severe disease among child patients was 2.1%, and
both incidence rates of clinical reoccurrence and sequela were 0.
By contrast, in the REEG group, these rates were 8.5, 12.7 and
8.5%, respectively. Through comparisons, the two groups had a
statistical difference in the incidence rate of clinical
reoccurrence (P<0.05), rather than in the incidence rates of
severe disease and sequela (P>0.05) (Table III).
 | Table III.Comparison of prognoses among child
patients (n, %). |
Table III.
Comparison of prognoses among child
patients (n, %).
| Groups | n | AEEG | REEG | χ2 | P-value |
|---|
| Incidence rate of
severe disease | 5 | 1 (2.1%) | 4 (8.5%) | 0.845 | 0.361 |
| Incidence rate of
clinical reoccurrence | 6 | 0 | (12.7%) | 4.451 | 0.026 |
| Incidence rate of
sequela | 4 | 0 | (8.5%) | 2.350 | 0.117 |
Discussion
Encephalitis is a nervous functional disorder, and
inflammation tends to occur in immunological diseases,
intoxication, metabolic encephalopathy, cancer, vascular diseases
or viral diseases (10–12). Infectious encephalitis mainly
consists of three types: viral encephalitis, suppurative meningitis
and mycoplasma encephalitis (13).
Viral encephalitis belongs to a kind of inflammation due to the
invasion of virus into brain parenchyma. Patients are infected with
virus and thus, brain parenchyma has virus-induced lesions. As a
result, patients present certain clinical symptoms, such as
headache, nausea and fever (14,15).
EEG detecting, a simple method to monitor brain
functions, can relatively correctly monitor abnormal
electroencephalographic activities and brain damage and help
clinical doctors take the corresponding timely treatment measures
for child patients (16). REEG and
AEEG are the most common clinical instruments, currently and often
used for the auxiliary diagnosis of viral encephalitis (17,18).
REEG has a significant effect on the diagnosis of viral
encephalitis and can timely reflect the moderate and severe
abnormities of child patients, which has an important clinical
significance to viral encephalitis. However, AEEG can more
obviously and accurately detect abnormal discharge due to brain
damage (19). The main reason for
the difficulty in detecting abnormal discharge of patients with
viral encephalitis with REEG is that the monitoring time is short.
On the contrary, AEEG can monitor the changes in brain wave for 24
h, and it is easier to detect the abnormal discharge, effectively
avoiding clinical misdiagnoses and diagnostic errors (20).
It was found in this study that REEG detected 22
normal child patients and 25 abnormal child patients with the
abnormity rate of 53.2%. AEEG detected 9 normal child patients and
38 abnormal child patients with the abnormity rate of 80.9%,
indicating the abnormity rate in the AEEG group is significantly
higher than that in the REEG group (P<0.05). Child patients with
viral encephalitis have continuous and paroxysmal abnormal brain
waves, and abnormal electroencephalographic activities can be
traced better by AEEG for the long monitoring time and continuous
monitoring (21). The REEG group had
a higher detection rate of moderately abnormal child patients, but
lower detection rates of mildly and severely abnormal child
patients. In the AEEG group, the detection rate of severely
abnormal child patients were significantly higher than that of
mildly abnormal child patients. Through comparison, the detection
rate of severely abnormal child patients in the AEEG group was
obviously higher than that in the REEG group (P<0.05). This
fully indicates that two different EEGs have varying detection
rates for encephalitis in different courses. In this study, REEG
cannot more favourably discriminate between mild and moderate child
patients with viral encephalitis and between mild and severe child
patients. In contrast, AEEG can relatively successfully
discriminate severe child patients with viral encephalitis from
moderate and mild ones with a high detection rate. In the REEG
group, 3 child patients with epileptiform discharge were detected
with the detection rate of 6.4%, while in the AEEG group, 20 cases
of epileptiform discharge were detected with the detection rate of
42.6% (P<0.05). Generally, in the position application of
epileptiform discharge, monopolar lead equipment has a better
positioning effect than bipolar one and relatively low amplitude
and distortion degree. The hospitalization time of child patients
and time of EEG restoring to be normal were calculated based on the
study results. The statistical results showed that with the
abnormity degree of EEG deepened, the hospitalization time of child
patients and time of EEG restoring to normal were correspondingly
prolonged. Both the REEG and AEEG groups had differences in the
time of restoring and hospitalization time of child patients
(P<0.05). At last, the prognoses of child patients were
analyzed, and it was found that the comparison of the incidence
rate of clinical reoccurrence between the two groups was
statistically significant (P<0.05). The comparison of incidence
rates of severe disease and sequela between the two groups were not
statistically significant (P>0.05). The abnormity of EEG
reflects the damage degree of child patient brain parenchyma, and
the more abnormal the amplitude of fluctuation is, the more severe
the damage becomes and the larger the opportunity of sequela is. As
the disease conditions of child patients were improved, the
clinical symptoms were correspondingly decreased, and the abnormity
rate of EEG was significantly decreased. Therefore, EEG restoring
to normal can be taken as one of child patient disease condition
improvement indicators (22).
However, the improvement of child patients cannot be confirmed only
based on EEG restoring to normal, and multiple clinical indicators
should be considered to assess disease conditions of child
patients.
There are also certain defects in this study. For
example, whether the medication of child patients before visiting
doctors has an effect on EEG should be confirmed, and a larger
number of samples need analyzing to prove this. Future studies will
be conducted to further verify the conclusion of this study.
In conclusion, EEG can be used for the auxiliary
diagnosis of child patients with viral encephalitis, and AEEG is
superior to REEG, which has higher sensitivity and can be taken as
an indicator for the auxiliary diagnosis of viral encephalitis and
the prognosis of child patients.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YL and CW conceived and designed the study. GZ, CL,
JC and XJ were responsible for the collection and analysis of the
patient data. YL and YW helped with EEG monitoring. YL, GZ and CL
interpreted the data and drafted the manuscript. JC and CW revised
the manuscript critically for important intellectual content. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Yantaishan Hospital of Yantai (Yantai, China). Signed informed
consents were obtained from the parents or guardians of the child
patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Armangue T, Leypoldt F and Dalmau J:
Autoimmune encephalitis as differential diagnosis of infectious
encephalitis. Curr Opin Neurol. 27:361–368. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Adenot M, Frobert E, Blanchard G, Morel B,
Perrot L, Floret D and Javouhey E: Clinical presentation of severe
viral encephalitis with known causative agents in children: A
retrospective study on 16 patients hospitalized in a pediatric
intensive care unit (2008–2011). J Child Neurol. 29:1508–1518.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Daxboeck F, Blacky A, Seidl R, Krause R
and Assadian O: Diagnosis, treatment, and prognosis of
Mycoplasma pneumoniae childhood encephalitis: Systematic
review of 58 cases. J Child Neurol. 19:865–871. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pelkonen T, Sarajuuri A, Rautanen T,
Sinkkonen S and Jero J: Meningoencephalitis and otitis media in a
child with Mycoplasma pneumoniae infection. Acta Otolaryngol
Case Rep. 2:1–4. 2017. View Article : Google Scholar
|
|
5
|
Taba P, Schmutzhard E, Forsberg P, Lutsar
I, Ljøstad U, Mygland Å, Levchenko I, Strle F and Steiner I: EAN
consensus review on prevention, diagnosis and management of
tick-borne encephalitis. Eur J Neurol. 24:1214–e61. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Domingues RB: Treatment of viral
encephalitis. Cent Nerv Syst Agents Med Chem. 9:56–62. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Spencer DC, Sun FT, Brown SN, Jobst BC,
Fountain NB, Wong VS, Mirro EA and Quigg M: Circadian and ultradian
patterns of epileptiform discharges differ by seizure-onset
location during long-term ambulatory intracranial monitoring.
Epilepsia. 57:1495–1502. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Seneviratne U, Mohamed A, Cook M and
D'Souza W: The utility of ambulatory electroencephalography in
routine clinical practice: A critical review. Epilepsy Res.
105:1–12. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kiloh LG, McComas AJ and Osselton JW:
Clinical Electroencephalography. 3rd. Butterworth-Heinemann;
Oxford, UK: 1972
|
|
10
|
Venkatesan A, Tunkel AR, Bloch KC, Lauring
AS, Sejvar J, Bitnun A, Stahl JP, Mailles A, Drebot M, Rupprecht
CE, et al; International Encephalitis Consortium, . Case
definitions, diagnostic algorithms, and priorities in encephalitis:
Consensus statement of the international encephalitis consortium.
Clin Infect Dis. 57:1114–1128. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Armangue T, Leypoldt F and Dalmau J:
Autoimmune encephalitis as differential diagnosis of infectious
encephalitis. Curr Opin Neurol. 27:361–368. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pillai SC, Hacohen Y, Tantsis E, Prelog K,
Merheb V, Kesson A, Barnes E, Gill D, Webster R, Menezes M, et al:
Infectious and autoantibody-associated encephalitis: Clinical
features and long-term outcome. Pediatrics. 135:e974–e984. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Graus F, Titulaer MJ, Balu R, Benseler S,
Bien CG, Cellucci T, Cortese I, Dale RC, Gelfand JM, Geschwind M,
et al: A clinical approach to diagnosis of autoimmune encephalitis.
Lancet Neurol. 15:391–404. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Qian Y, Wong CC, Lai SC, Lin ZH, Zheng WL,
Zhao H, Pan KH, Chen SJ and Si JM: Klebsiella pneumoniae invasive
liver abscess syndrome with purulent meningitis and septic shock: A
case from mainland China. World J Gastroenterol. 22:2861–2866.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kennedy PGE, Quan PL and Lipkin WI: Viral
encephalitis of unknown cause: Current perspective and recent
advances. Viruses. 9:1382017. View
Article : Google Scholar
|
|
16
|
Mohammad SS, Soe SM, Pillai SC, Nosadini
M, Barnes EH, Gill D and Dale RC: Etiological associations and
outcome predictors of acute electroencephalography in childhood
encephalitis. Clin Neurophysiol. 127:3217–3224. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Namekawa K, Mori H, Tabata H, Miyahara H,
Minote M, Nishida A and Shindo K: Extreme delta brush in
electroencephalogram may be nonspecific to the anti-NMDAR
encephalitis. Neurology. 88:2232017.
|
|
18
|
Fangsaad T, Assawabumrungkul S and
Visudtibhan A: Clinical course and long-term outcome in children
with alteration of consciousness underwent continuous EEG
monitoring: A prospective observational study in Thailand. J Clin
Neurosci. 47:93–96. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Qi XK, Liu JG, Li CQ and Ning BO: 27 cases
of atypical viral encephalitis with obvious psychiatric symptom but
negative auxiliary diagnosis. J Neurol Sci. 357:e115–e116. 2015.
View Article : Google Scholar
|
|
20
|
Moeller JJ, Tu B and Bazil CW:
Quantitative and qualitative analysis of ambulatory
electroencephalography during mild traumatic brain injury. Arch
Neurol. 68:1595–1598. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lawley A, Evans S, Manfredonia F and
Cavanna AE: The role of outpatient ambulatory
electroencephalography in the diagnosis and management of adults
with epilepsy or nonepileptic attack disorder: A systematic
literature review. Epilepsy Behav. 53:26–30. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gold JJ, Crawford JR, Glaser C, Sheriff H,
Wang S and Nespeca M: The role of continuous electroencephalography
in childhood encephalitis. Pediatr Neurol. 50:318–323. 2014.
View Article : Google Scholar : PubMed/NCBI
|